Abstract
Influenza virus hemagglutinin consists of a highly variable and immunodominant head domain and a more conserved but immunosubdominant stalk domain. We introduced seven N-linked glycosylation sites in the hemagglutinin head domain to shield the immunodominant antigenic sites. The hyperglycosylated hemagglutinin enhanced stalk-directed seroreactivity while dampening the head response in immunized mice. Upon influenza virus challenge, mice vaccinated with the hyperglycosylated hemagglutinin were better protected against morbidity and mortality than mice receiving the wild-type hemagglutinin.
TEXT
Currently, most influenza virus vaccines consist of a combination of three or four seasonal virus strains predicted to circulate in the following season. Influenza virus hemagglutinin (HA) and neuraminidase are the most abundant viral glycoproteins on the surface of the virus. Antibodies elicited by conventional vaccines target primarily the immunodominant globular head domain of HA (1–3). These antibodies generally bind four antigenic sites proximal to the receptor binding site (4, 5), and they neutralize the virus by obstructing its binding to the receptor on the cell surface. The antigenic regions are highly variable, and current vaccines therefore offer limited protection against drifted strains or other HA subtypes.
Recently, broadly neutralizing antibodies have been described that are reactive against a wide variety of strains or subtypes (6–13). Many of these antibodies target the stalk domain of HA, which is more conserved than the highly variable head domain. These antibodies do not block virus attachment but rather inhibit the conformational changes required for membrane fusion, block the cleavage of HA to HA1 and HA2, or prevent the egress of new virions from the plasma membrane of the infected cell (6–8, 10, 12). It has been proposed that a vaccine capable of eliciting high titers of stalk-directed antibodies could confer broader protection than current vaccines and therefore eliminate the need for annual vaccination (14, 15). Such a vaccine could also offer protection against emerging pandemic strains of influenza.
We aimed to redirect the immune response away from the immunodominant and variable head domain in order to focus the immune response on the conserved stalk domain. To this end, we constructed an HA with a hyperglycosylated globular head domain. We hypothesized that by masking the antigenic sites in the globular head with carbohydrates, we could suppress the immune response to the globular head domain and redirect the immune response toward the more conserved stalk domain.
The number of glycosylation sites in the globular head domain of HA has increased over time (16–18). It was shown that the addition of glycosylation in the head domain prevents the binding of monoclonal antibodies (19) or antisera raised against less glycosylated HAs (18, 20) and decreased the need for other escape substitutions in the antigenic sites during antigenic drift (17, 21). These studies suggest that the introduction of additional glycosylation sites in the globular head of the HA alters its antigenicity. Therefore, hyperglycosylation of the HA globular head may be a good way to redirect the antibody response toward the conserved stalk domain.
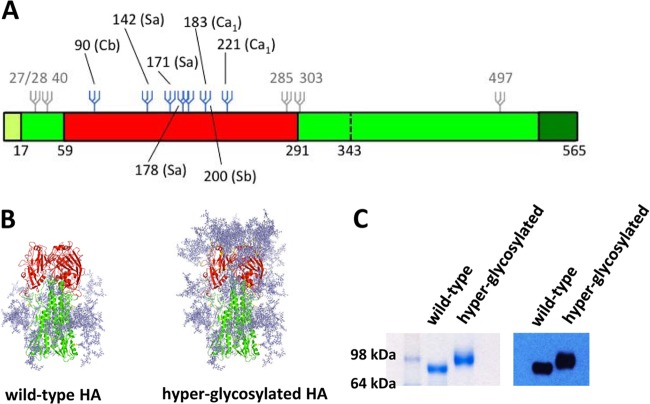
Using site-directed mutagenesis (primer sequences available upon request), we introduced seven N-linked glycosylation sites in the immunodominant antigenic sites of the HA head domain (4) (Fig. 1). We used the HA of A/Puerto Rico/8/34 virus (PR/8) as our model, because the PR/8 HA contains very few glycosylation sites. Only one of the naturally occurring glycans is situated in the head domain, although it does not seem to cover any of the antigenic sites. Glycans were introduced at the Ca, Cb, Sa, and Sb antigenic sites (Fig. 1A and B). Nearly all N-linked glycosylation sites within different H1 hemagglutinins appear in just two of the four antigenic sites, being Cb (e.g., glycan at position 90) and Sa (e.g., positions 142, 171, and 178), or outside the classical antigenic sites (e.g., positions 71 and 104) (20, 22). Four of the seven introduced glycosylation sites of the hyperglycosylated HA correspond to naturally occurring glycosylation in antigenic sites Cb and Sa (positions 90, 142, 171, and 178). To shield the other two antigenic sites, glycosylation sites were introduced in the antigenic sites Ca and Sb based on the HA structure and, when possible, using existing Asn residues.
FIG 1.
Covering antigenic sites of HA with N-linked glycosylation. (A) Schematic of the influenza HA and the position of introduced glycans. The signal peptide is shown in light green, the head and stalk domain of the ectodomain in red and green, respectively, and the transmembrane and cytoplasmic domains are depicted in dark green. Glycans indicated in gray are present in the wild-type HA. Additional glycans in the hyperglycosylated HA are depicted in blue. (B) Modeling of introduced glycans on the crystal structure of the PR/8 HA (PDB 1RU7). Original and additional glycans were modeled on the crystal structure of the PR/8 HA using GlyProt (37) and drawn using PyMol (DeLano Scientific). Because of modeling limitations, only 6 out of the 7 added potential N-linked glycans are present on the hyperglycosylated HA model. (C) The ectodomain of the wild-type HA and the hyperglycosylated HA containing the T4-foldon trimerization domain and a His tag were expressed in 293T cells, and purified glycoproteins were run on an SDS-PAGE polyacrylamide gel under denaturing and reducing conditions. A clear increase in molecular weight is present for the hyperglycosylated HA compared to the wild-type HA, indicating the presence of additional glycosylation.
The wild-type and mutant genes for full-length and soluble HA with the addition of a trimerization domain and His tag were cloned into the pCAGGS expression vector (23) for transient transfection into mammalian cells using linear polyethylenimine (Polysciences) (24). The hyperglycosylated HA expressed to levels similar to those of the wild-type HA glycoprotein. An increase in molecular weight as demonstrated by SDS-PAGE analysis with subsequent Coomassie staining and Western blot analysis confirms that additional glycans are expressed on the surface of the hyperglycosylated proteins (Fig. 1C). However, because of limitations of the resolution of standard SDS-PAGE gels and expected variation in glycosylation site usage and glycan chain heterogeneity (25–27), it is not possible to determine whether each of the newly created glycosylation sites is efficiently glycosylated.
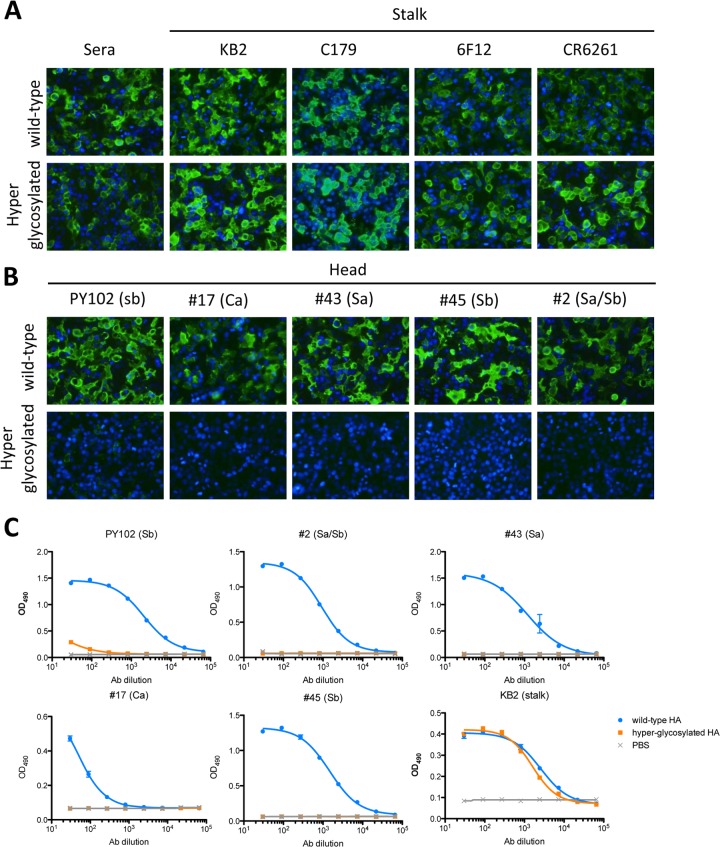
Immunofluorescence microscopy showed good binding by conformational antibodies to the stalk domain of the hyperglycosylated HA (7, 11, 28, 29), suggesting that the stalk domain is properly folded (Fig. 2A). On the other hand, antibodies targeting the antigenic sites at the globular head domain of the PR/8 HA did not bind the hyperglycosylated HA (Fig. 2B), suggesting effective shielding of the antigenic sites. This was further confirmed by enzyme-linked immunosorbent assay (ELISA) binding studies (Fig. 2C), showing no binding of five different head-directed antibodies to purified soluble hyperglycosylated HA, while the binding of stalk-directed antibody KB2 was not affected. It is most likely that this loss of binding is caused by the presence of a glycan, though we cannot exclude the effect of the mutation “introducing” the glycosylation site on the binding of these antibodies.
FIG 2.
Hyperglycosylated HA expresses well at the surface of transfected mammalian cells and is able to bind stalk antibodies. Plasmids encoding wild-type or hyperglycosylated full-length HA were transfected into 293T cells. The HA was stained 24 h posttransfection with PR8 antiserum or stalk-directed antibodies KB2 (28), C179 (29), 6F12 (11), and CR6261 (7) (A) or head-directed antibodies PY102 (38), 17, 43, 45, and 2 (B). Monoclonal antibodies 17, 43, 45, and 2 were generated for this research as described before (11). The indicated binding epitope at the PR/8 HA was mapped using escape studies in eggs for each newly generated HA head antibody as described previously (4). Binding of stalk-directed antibodies to the hyperglycosylated HA is not changed compared to that of the wild-type HA. In contrast, introduction of glycosylation sites in the antigenic sites of the globular head domain of the HA abrogated binding of head-directed antibodies. (C) Binding of five different head-directed antibodies to purified, soluble HA was tested in ELISAs. Head-directed antibodies did not bind to hyperglycosylated HA, while binding of stalk-directed antibody KB2 was not affected.
Soluble wild-type and hyperglycosylated HA proteins containing a T4-foldon trimerization domain and His tag were expressed in 293T (ATCC CRL-11268) cells upon transient transfection and purified using Ni-nitrilotriacetic acid (NTA) beads (Qiagen) as described previously (30). A mammalian expression system was chosen because mammalian cells utilize large complex glycans, in contrast to other expression systems like insect cells (25). Naive 6- to 8-week-old BALB/c mice were vaccinated intramuscularly with 10 μg of protein adjuvanted with 5 μg of poly(I·C) (Invivogen) three times in 3- to 4-week intervals. Serum samples were collected 3 weeks after the second and third immunizations. All mouse experiments were performed under the guidelines of the Icahn School of Medicine at Mount Sinai Institutional Animal Care and Use Committee (permit LA09-00266).
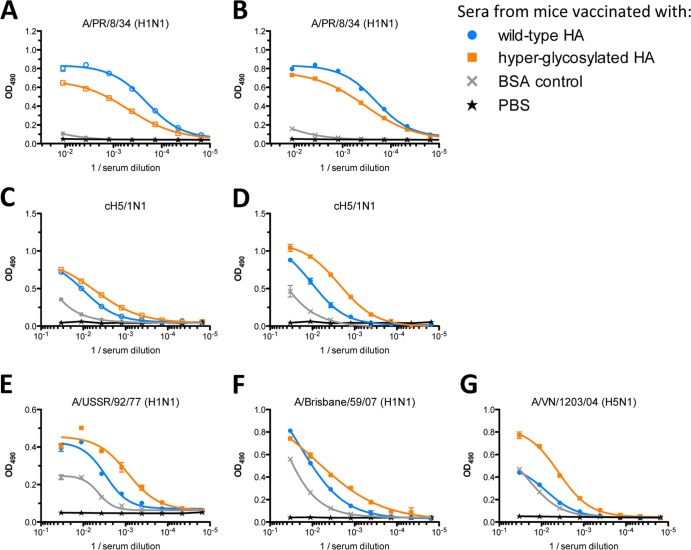
Seroreactivity induced by either wild-type HA or the hyperglycosylated variant was analyzed by ELISA against purified influenza viruses as described previously (31, 32). First, reactivity to the parental strain, PR/8, was tested. Mice vaccinated with wild-type HA elicited higher titers of antibodies than hyperglycosylated HA, which was especially apparent after two immunizations (Fig. 3A and B). After three immunizations, the difference in reactivity to PR/8 was less apparent. This could be the result of boosting epitopes on the head that are not shielded efficiently by the introduced glycans or due to an increase in stalk antibodies. To assay binding to the stalk domain without interference from head reactivity, we made use of the chimeric HAs that were recently developed in our lab (32, 33). The chimeric HAs used in the described experiments contain the stalk of PR/8 HA (H1) with the head domain of an exotic HA subtype to which no cross-reactivity is expected, like H9 or H5. Thus, chimeric HAs with a PR/8 stalk and an H9 or H5 head are named cH9/1 and cH5/1, respectively. Observed seroreactivity to these chimeric HAs induced by our immunization strategy is therefore solely directed toward the H1 stalk domain, as the mice are naive to both H9 and H5 subtype HAs. Here, we demonstrate that the seroreactivity to the stalk is higher upon vaccination with the hyperglycosylated HA than in mice vaccinated with the wild-type HA. After two immunizations, the difference was 3-fold, while the difference increased to almost 9-fold after three immunizations (Fig. 3C and D). Thus, the enhanced seroreactivity to the stalk domain is accompanied by a dampened response to the globular head domain, suggesting that the introduction of glycans to shield immunodominant epitopes is an effective way to alter the antigenicity of the influenza virus HA.
FIG 3.
Immunization of mice with the hyperglycosylated HA induces high titers of stalk-directed antibodies against distinct seasonal H1N1 and pandemic H5N1 viruses. Sera originating from mice vaccinated with the wild-type or hyperglycosylated HAs were assayed by ELISA for reactivity against purified viruses: A/Puerto Rico/8/34, cH5/1, A/USSR/92/77, A/Brisbane/59/07, and A/Vietnam/1203/04. Sera originating from mice vaccinated with the hyperglycosylated HA were less reactive to virus containing the full-length PR/8 HA compared to mice vaccinated with the wild-type HA after two (A) and three (B) immunizations. In contrast, seroreactivity to a virus bearing the cH5/1 HA, which consists of a subtype H5 head domain and the PR/8 stalk domain, was higher for sera originating from mice vaccinated with the hyperglycosylated HA than in mice vaccinated with the wild-type HA. This difference in reactivity was observed after two immunizations (C) and became more apparent after three immunizations (D). The seroreactivity to distinct H1N1 viruses (E, F) and an H5N1 virus (G) was also enhanced in mice vaccinated with the hyperglycosylated HA compared to that in mice immunized with the wild-type HA.
To further determine whether immunization with the hyperglycosylated HA increased the breadth of the antibody response, heterologous seroreactivity was tested against two distinct H1N1 strains, A/USSR/92/77 and A/Brisbane/59/07 (Fig. 3E and F). ELISAs show superior reactivity of sera from hyperglycosylated HA-vaccinated mice to these H1N1 viruses compared to that of the wild-type HA-vaccinated mice. In addition, enhanced reactivity was also detected against a low-pathogenic variant of a pandemic human H5N1 strain, A/Vietnam/1203/04 (Fig. 3G). Together, these analyses show that hyperglycosylated HA is able to elicit a robust heterologous and heterosubtypic response directed against the stalk of HA while reducing the immune response to the globular head compared to wild-type HA.
We hypothesized that the enhanced stalk reactivity induced by the hyperglycosylated vaccine construct would result in improved in vivo efficacy against viral infection. To test this hypothesis, mice were infected with 20 mouse median lethal doses (mLD50) of a “7 + 1” reassortant PR/8 virus expressing cH9/1 (32, 34) 4 weeks after the final boost. In addition to mice immunized with either the hyperglycosylated or wild-type HA, control animals vaccinated with bovine serum albumin (BSA) adjuvanted with poly(I·C) were included. Because the mice were naive to the H9 head and all other viral gene products, any observed protection should be attributed solely to the response specific to the HA stalk domain. Weight loss was monitored daily for 14 days after challenge, and animals that lost 20% or more of their initial body weight were scored as dead and euthanized. As shown in Fig. 4A, mice vaccinated with the hyperglycosylated HA lost minimal weight compared to the control animals. Mice vaccinated with wild-type HA lost significantly more weight and began succumbing to infection at day five postinfection. Thus, mice vaccinated with the hyperglycosylated HA were better protected against morbidity (weight loss; Fig. 4A) and mortality (survival; Fig. 4B) than mice vaccinated with the wild-type HA on the basis of enhanced reactivity to the HA stalk. In addition to virus neutralization (11, 34), other mechanisms of action for broadly reactive stalk-directed antibodies, including antibody-dependent cellular cytotoxicity (35) and complement-dependent lysis (36), may have contributed to the in vivo protection observed in our animal experiments.
FIG 4.
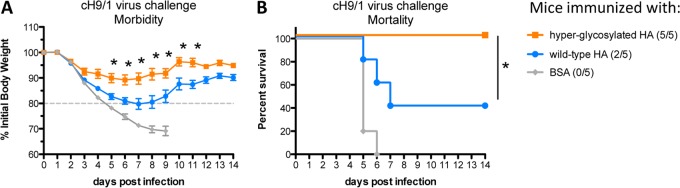
Mice immunized with the hyperglycosylated HA show protection against morbidity and mortality upon challenge with a cH9/1 virus. (A) Mice (n = 5) were challenged with 20 mLD50 of a virus containing the cH9/1 HA and weighed daily. Vaccination with the hyperglycosylated HA protected mice better from morbidity as measured by weight loss (A) and mortality (B) compared to mice vaccinated with the wild-type HA. Significant differences between the hyperglycosylated HA and the wild-type HA-vaccinated mice were observed at the indicated points. Statistical significance for weight curves was calculated using multiple unpaired t tests correcting for multiple comparisons with the Holm-Sidak method (*, P < 0.001; Prism version 6.0b; GraphPad Software). Statistical significance for the Kaplan-Meier survival curve was calculated with the Mantel-Cox test (*, P < 0.05; Prism version 6.0b; GraphPad Software).
Here, we demonstrate that immunization with the hyperglycosylated HA protein induces higher titers of stalk-directed antibodies, while dampening the immune response to the globular head domain, than immunization with the wild-type HA. The induced humoral immune response is broadly cross-reactive to distinct H1N1 viruses and to a pandemic human H5N1 strain. The hyperglycosylated HA-immunized animals were better protected against a lethal viral infection, solely on the basis of HA stalk-directed immunity, than animals immunized with the wild-type HA. The data suggest that shielding immunodominant epitopes at the antigenic sites shifts the head/stalk antibody balance toward the conserved stalk domain.
ACKNOWLEDGMENTS
We gratefully acknowledge Chen Wang for technical assistance and Matthew Miller and Gene Tan for critical readings of the manuscript.
This work was partially supported by NIH program project grant 1P01AI097092-01A1 and by PATH.
Footnotes
Published ahead of print 23 October 2013
REFERENCES
- 1.Margine I, Hai R, Albrecht RA, Obermoser G, Harrod AC, Banchereau J, Palucka K, Garcia-Sastre A, Palese P, Treanor JJ, Krammer F. 2013. H3N2 influenza virus infection induces broadly reactive hemagglutinin stalk antibodies in humans and mice. J. Virol. 87:4728–4737. 10.1128/JVI.03509-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sui J, Sheehan J, Hwang WC, Bankston LA, Burchett SK, Huang CY, Liddington RC, Beigel JH, Marasco WA. 2011. Wide prevalence of heterosubtypic broadly neutralizing human anti-influenza A antibodies. Clin. Infect. Dis. 52:1003–1009. 10.1093/cid/cir121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wrammert J, Smith K, Miller J, Langley WA, Kokko K, Larsen C, Zheng NY, Mays I, Garman L, Helms C, James J, Air GM, Capra JD, Ahmed R, Wilson PC. 2008. Rapid cloning of high-affinity human monoclonal antibodies against influenza virus. Nature 453:667–671. 10.1038/nature06890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caton AJ, Brownlee GG, Yewdell JW, Gerhard W. 1982. The antigenic structure of the influenza virus A/PR/8/34 hemagglutinin (H1 subtype). Cell 31:417–427. 10.1016/0092-8674(82)90135-0 [DOI] [PubMed] [Google Scholar]
- 5.Wiley DC, Wilson IA, Skehel JJ. 1981. Structural identification of the antibody-binding sites of Hong Kong influenza haemagglutinin and their involvement in antigenic variation. Nature 289:373–378. 10.1038/289373a0 [DOI] [PubMed] [Google Scholar]
- 6.Dreyfus C, Laursen NS, Kwaks T, Zuijdgeest D, Khayat R, Ekiert DC, Lee JH, Metlagel Z, Bujny MV, Jongeneelen M, van der Vlugt R, Lamrani M, Korse HJ, Geelen E, Sahin O, Sieuwerts M, Brakenhoff JP, Vogels R, Li OT, Poon LL, Peiris M, Koudstaal W, Ward AB, Wilson IA, Goudsmit J, Friesen RH. 2012. Highly conserved protective epitopes on influenza B viruses. Science 337:1343–1348. 10.1126/science.1222908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ekiert DC, Bhabha G, Elsliger MA, Friesen RH, Jongeneelen M, Throsby M, Goudsmit J, Wilson IA. 2009. Antibody recognition of a highly conserved influenza virus epitope. Science 324:246–251. 10.1126/science.1171491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ekiert DC, Friesen RH, Bhabha G, Kwaks T, Jongeneelen M, Yu W, Ophorst C, Cox F, Korse HJ, Brandenburg B, Vogels R, Brakenhoff JP, Kompier R, Koldijk MH, Cornelissen LA, Poon LL, Peiris M, Koudstaal W, Wilson IA, Goudsmit J. 2011. A highly conserved neutralizing epitope on group 2 influenza A viruses. Science 333:843–850. 10.1126/science.1204839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friesen RH, Koudstaal W, Koldijk MH, Weverling GJ, Brakenhoff JP, Lenting PJ, Stittelaar KJ, Osterhaus AD, Kompier R, Goudsmit J. 2010. New class of monoclonal antibodies against severe influenza: prophylactic and therapeutic efficacy in ferrets. PLoS One 5:e9106. 10.1371/journal.pone.0009106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sui J, Hwang WC, Perez S, Wei G, Aird D, Chen LM, Santelli E, Stec B, Cadwell G, Ali M, Wan H, Murakami A, Yammanuru A, Han T, Cox NJ, Bankston LA, Donis RO, Liddington RC, Marasco WA. 2009. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat. Struct. Mol. Biol. 16:265–273. 10.1038/nsmb.1566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan GS, Krammer F, Eggink D, Kongchanagul A, Moran TM, Palese P. 2012. A pan-H1 anti-hemagglutinin monoclonal antibody with potent broad-spectrum efficacy in vivo. J. Virol. 86:6179–6188. 10.1128/JVI.00469-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Throsby M, van den Brink E, Jongeneelen M, Poon LL, Alard P, Cornelissen L, Bakker A, Cox F, van Deventer E, Guan Y, Cinatl J, ter Meulen J, Lasters I, Carsetti R, Peiris M, de Kruif J, Goudsmit J. 2008. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+ memory B cells. PLoS One 3:e3942. 10.1371/journal.pone.0003942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang TT, Tan GS, Hai R, Pica N, Petersen E, Moran TM, Palese P. 2010. Broadly protective monoclonal antibodies against H3 influenza viruses following sequential immunization with different hemagglutinins. PLoS Pathog. 6:e1000796. 10.1371/journal.ppat.1000796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nabel GJ, Fauci AS. 2010. Induction of unnatural immunity: prospects for a broadly protective universal influenza vaccine. Nat. Med. 16:1389–1391. 10.1038/nm1210-1389 [DOI] [PubMed] [Google Scholar]
- 15.Palese P, Wang TT. 2011. Why do influenza virus subtypes die out? A hypothesis. mBio 2(5):e00150–11. 10.1128/mBio.00150-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Das SR, Puigbo P, Hensley SE, Hurt DE, Bennink JR, Yewdell JW. 2010. Glycosylation focuses sequence variation in the influenza A virus H1 hemagglutinin globular domain. PLoS Pathog. 6:e1001211. 10.1371/journal.ppat.1001211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kobayashi Y, Suzuki Y. 2012. Evidence for N-glycan shielding of antigenic sites during evolution of human influenza A virus hemagglutinin. J. Virol. 86:3446–3451. 10.1128/JVI.06147-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medina RA, Stertz S, Manicassamy B, Zimmermann P, Sun X, Albrecht RA, Uusi-Kerttula H, Zagordi O, Belshe RB, Frey SE, Tumpey TM, Garcia-Sastre A. 2013. Glycosylations in the globular head of the hemagglutinin protein modulate the virulence and antigenic properties of the H1N1 influenza viruses. Sci. Transl. Med. 5:187ra70. 10.1126/scitranslmed.3005996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skehel JJ, Stevens DJ, Daniels RS, Douglas AR, Knossow M, Wilson IA, Wiley DC. 1984. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc. Natl. Acad. Sci. U. S. A. 81:1779–1783. 10.1073/pnas.81.6.1779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wei CJ, Boyington JC, Dai K, Houser KV, Pearce MB, Kong WP, Yang ZY, Tumpey TM, Nabel GJ. 2010. Cross-neutralization of 1918 and 2009 influenza viruses: role of glycans in viral evolution and vaccine design. Sci. Transl. Med. 2:24ra21. 10.1126/scitranslmed.3000799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki Y. 2011. Positive selection for gains of N-linked glycosylation sites in hemagglutinin during evolution of H3N2 human influenza A virus. Genes Genet. Syst. 86:287–294. 10.1266/ggs.86.287 [DOI] [PubMed] [Google Scholar]
- 22.Das SR, Hensley SE, David A, Schmidt L, Gibbs JS, Puigbo P, Ince WL, Bennink JR, Yewdell JW. 2011. Fitness costs limit influenza A virus hemagglutinin glycosylation as an immune evasion strategy. Proc. Natl. Acad. Sci. U. S. A. 108:E1417–E1422. 10.1073/pnas.1108754108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Niwa H, Yamamura K, Miyazaki J. 1991. Efficient selection for high-expression transfectants with a novel eukaryotic vector. Gene 108:193–199. 10.1016/0378-1119(91)90434-D [DOI] [PubMed] [Google Scholar]
- 24.Kirschner M, Monrose V, Paluch M, Techodamrongsin N, Rethwilm A, Moore JP. 2006. The production of cleaved, trimeric human immunodeficiency virus type 1 (HIV-1) envelope glycoprotein vaccine antigens and infectious pseudoviruses using linear polyethylenimine as a transfection reagent. Protein Expr. Purif. 48:61–68. 10.1016/j.pep.2006.02.017 [DOI] [PubMed] [Google Scholar]
- 25.de Vries RP, Smit CH, de Bruin E, Rigter A, de Vries E, Cornelissen LA, Eggink D, Chung NP, Moore JP, Sanders RW, Hokke CH, Koopmans M, Rottier PJ, de Haan CA. 2012. Glycan-dependent immunogenicity of recombinant soluble trimeric hemagglutinin. J. Virol. 86:11735–11744. 10.1128/JVI.01084-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Depetris RS, Julien JP, Khayat R, Lee JH, Pejchal R, Katpally U, Cocco N, Kachare M, Massi E, David KB, Cupo A, Marozsan AJ, Olson WC, Ward AB, Wilson IA, Sanders RW, Moore JP. 2012. Partial enzymatic deglycosylation preserves the structure of cleaved recombinant HIV-1 envelope glycoprotein trimers. J. Biol. Chem. 287:24239–24254. 10.1074/jbc.M112.371898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mir-Shekari SY, Ashford DA, Harvey DJ, Dwek RA, Schulze IT. 1997. The glycosylation of the influenza A virus hemagglutinin by mammalian cells. A site-specific study. J. Biol. Chem. 272:4027–4036 [DOI] [PubMed] [Google Scholar]
- 28.Heaton NS, Leyva-Grado VH, Tan GS, Eggink D, Hai R, Palese P. 2013. In vivo bioluminescent imaging of influenza a virus infection and characterization of novel cross-protective monoclonal antibodies. J. Virol. 87:8272–8281. 10.1128/JVI.00969-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smirnov YA, Lipatov AS, Gitelman AK, Okuno Y, Van Beek R, Osterhaus AD, Claas EC. 1999. An epitope shared by the hemagglutinins of H1, H2, H5, and H6 subtypes of influenza A virus. Acta Virol. 43:237–244 [PubMed] [Google Scholar]
- 30.Krammer F, Margine I, Tan GS, Pica N, Krause JC, Palese P. 2012. A carboxy-terminal trimerization domain stabilizes conformational epitopes on the stalk domain of soluble recombinant hemagglutinin substrates. PLoS One 7:e43603. 10.1371/journal.pone.0043603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Goff PH, Krammer F, Hai R, Seibert CW, Margine I, Garcia-Sastre A, Palese P. 2013. Induction of cross-reactive antibodies to novel H7N9 influenza virus by recombinant Newcastle disease virus expressing a North American lineage H7 subtype hemagglutinin. J. Virol. 87:8235–8240. 10.1128/JVI.01085-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hai R, Krammer F, Tan GS, Pica N, Eggink D, Maamary J, Margine I, Albrecht RA, Palese P. 2012. Influenza viruses expressing chimeric hemagglutinins: globular head and stalk domains derived from different subtypes. J. Virol. 86:5774–5781. 10.1128/JVI.00137-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pica N, Hai R, Krammer F, Wang TT, Maamary J, Eggink D, Tan GS, Krause JC, Moran T, Stein CR, Banach D, Wrammert J, Belshe RB, Garcia-Sastre A, Palese P. 2012. Hemagglutinin stalk antibodies elicited by the 2009 pandemic influenza virus as a mechanism for the extinction of seasonal H1N1 viruses. Proc. Natl. Acad. Sci. U. S. A. 109:2573–2578. 10.1073/pnas.1200039109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krammer F, Pica N, Hai R, Margine I, Palese P. 2013. Chimeric hemagglutinin influenza virus vaccine constructs elicit broadly protective stalk-specific antibodies. J. Virol. 87:6542–6550. 10.1128/JVI.00641-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jegaskanda S, Job ER, Kramski M, Laurie K, Isitman G, de Rose R, Winnall WR, Stratov I, Brooks AG, Reading PC, Kent SJ. 2013. Cross-reactive influenza-specific antibody-dependent cellular cytotoxicity antibodies in the absence of neutralizing antibodies. J. Immunol. 190:1837–1848. 10.4049/jimmunol.1201574 [DOI] [PubMed] [Google Scholar]
- 36.Terajima M, Cruz J, Co MD, Lee JH, Kaur K, Wrammert J, Wilson PC, Ennis FA. 2011. Complement-dependent lysis of influenza a virus-infected cells by broadly cross-reactive human monoclonal antibodies. J. Virol. 85:13463–13467. 10.1128/JVI.05193-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bohne-Lang A, von der Lieth CW. 2005. GlyProt: in silico glycosylation of proteins. Nucleic Acids Res. 33:W214–W219. 10.1093/nar/gki385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dinca L, Neuwirth S, Schulman J, Bona C. 1993. Induction of antihemagglutinin antibodies by polyclonal antiidiotype antibodies. Viral Immunol. 6:75–84. 10.1089/vim.1993.6.75 [DOI] [PubMed] [Google Scholar]