Abstract
Background
Preventing obesity requires maintenance of healthy eating behaviors over time. Food labels and strategies that increase visibility and convenience of healthy foods (choice architecture) promote healthier choices, but long-term effectiveness is unknown.
Purpose
Assess effectiveness of traffic-light labeling and choice architecture cafeteria intervention over 24 months.
Design
Longitudinal pre–post cohort follow-up study between December 2009 and February 2012. Data were analyzed in 2012.
Setting/participants
Large hospital cafeteria with mean of 6511 transactions daily. Cafeteria sales were analyzed for: (1) all cafeteria customers and (2) longitudinal cohort of 2285 hospital employees who used the cafeteria regularly.
Intervention
After 3-month baseline period, cafeteria items were labeled green (healthy), yellow (less healthy) or red (unhealthy) and rearranged to make healthy items more accessible.
Main outcome measures
Proportion of cafeteria sales that were green or red during each 3-month period from baseline to 24 months. Changes in 12- and 24-month sales were compared to baseline for all transactions and transactions by the employee cohort.
Results
The proportion of sales of red items decreased from 24% at baseline to 20% at 24 months (p<0.001), and green sales increased from 41% to 46% (p<0.001). Red beverages decreased from 26% of beverage sales at baseline to 17% at 24 months (p<0.001); green beverages increased from 52% to 60% (p<0.001). Similar patterns were observed for the cohort of employees, with largest change for red beverages (23% to 14%, p<0.001).
Conclusions
A traffic-light and choice architecture cafeteria intervention resulted in sustained healthier choices over 2 years, suggesting food environment interventions can promote long-term changes in population eating behaviors.
Introduction
The rising prevalence of overweight and obesity is now a major health concern in the U.S. and worldwide.1,2 Easily accessible, low cost, energy-dense food contributes to high calorie diets and weight gain.3,4 Although individual-level interventions can result in large weight changes among small groups of patients, efforts to prevent obesity at the population level will require changes in the food environment that promote healthy, lower calorie foods and discourage unhealthy, energy-dense foods.3,4
Several factors contribute to unhealthy eating patterns, including lack of knowledge,5,6 automatic or habitual choice processes,7,8 and preference for convenience.9–11 All of these factors can be addressed in the context of the food environment. Nutrition labeling on food packages addresses knowledge by providing detailed information about the nutritional and caloric content of a food, but many nutrition labels require a high level of literacy and numeracy to interpret.12 Simpler labeling schemes, such as traffic lights that identify healthy items as “green” and unhealthy items as “red,” have demonstrated effectiveness for promoting healthier choices in studies with either brief exposure conditions or short-term follow up.13–18 “Nudging strategies” that target automatic processes and preferences for convenience can manipulate the food environment to promote healthier choices.7 Some studies have demonstrated that small changes in the food environment, including choice architecture interventions to make healthy items more visible and convenient, can result in better food choices, but these studies have demonstrated only short-term change after a brief exposure to the intervention.9,10,13,14,19,20
It is critical to evaluate the long-term effectiveness of food environment interventions in order to develop effective health policies and programs for obesity prevention. A simulation modeling study of a traffic-light intervention demonstrated that if small changes in energy consumption were sustained at a population level over time, the intervention would be effective for both weight reduction and cost savings.21 However, it is currently unknown if food labeling and environment interventions can produce durable changes in healthy food choices or if individuals revert back to unhealthy eating patterns.
It has been previously demonstrated that a traffic-light labeling and choice architecture intervention in a large hospital cafeteria was effective for promoting healthy food and beverage choices over 6 months among all cafeteria patrons and among hospital employees.13,14 The objective of the current study was to evaluate whether the increase in sales of healthier items was maintained over the 24 months following implementation of the intervention by comparing sales at 12 and 24 months to a baseline period prior to the labeling. Outcomes were analyzed for: (1) purchases of all cafeteria patrons to determine the effectiveness of the intervention for a broad population of infrequent and frequent cafeteria users and (2) purchases of a cohort of 2285 employees who regularly visited the cafeteria from baseline through the end of 24-month follow-up to determine the effectiveness of the intervention for customers who had repeated exposure.
Methods
This study was approved by the Partners Healthcare Institutional Review Board.
Study Design
This is a longitudinal follow-up study from December 2009 through February 2012 in the main cafeteria at Massachusetts General Hospital (MGH) in Boston, Massachusetts. Baseline cafeteria sales data were collected from December 2009 through February 2010, followed by the cafeteria intervention starting in March 2010. Initial data analyses to compare sales during the first 6 months of the intervention to the 3 month baseline period have been reported.13,14 The current study evaluates the effectiveness of the cafeteria intervention after 24 months of follow-up.
Setting and Participants
Massachusetts General Hospital is a 907-bed teaching hospital. The hospital has one main cafeteria and four smaller on-site cafeterias. The cafeterias are operated by the hospital’s nutrition and food services, and no outside food vendors are located on campus. The main cafeteria serves hospital employees, patients, and visitors 7 days a week between the hours of 6:30 am and 8:00 pm. Hospital employees have the option of paying for cafeteria purchases by direct payroll deduction using a “platinum plate” card. During the study period, 7431 employees used a platinum plate card at least once to pay for purchases in the main cafeteria. To assess the effect of the intervention on employees with frequent long-term exposure to the cafeteria, employee platinum plate users who made a purchase in the cafeteria at least three times during each 3-month period from baseline to the end of follow up were included in the study cohort. This cohort was identified retrospectively from sales data at the end of the 24-month follow-up period.
Cafeteria Intervention
After collecting baseline sales data for 3 months, labeling and choice architecture changes were implemented in the cafeteria sequentially and are described in detail elsewhere.13,14 The changes for the labeling and choice architecture intervention were made as permanent changes to the cafeteria. Briefly, the traffic-light food labeling system was based on the 2005 U.S. Department of Agriculture My Pyramid recommendations,22 and every item in the cafeteria was labeled as red, yellow, or green based on three positive criteria (fruit/vegetable, whole grain, and lean protein/low-fat dairy as the main ingredient) and two negative criteria (saturated fat and caloric content). Items with more positive than negative criteria were green, items with equal positive and negative criteria were yellow, and items with more negative than positive criteria were red. The only exceptions were bottled water and diet beverages with 0 calories; they were labeled green despite having no positive criteria. The new labeling system in the cafeteria was promoted to hospital employees and visitors, and permanent signage and menu board changes accompanied the labels.
Choice architecture changes were implemented 3 months after introduction of the traffic-light labels. Cafeteria items were rearranged to make some of the green items more visible and convenient for purchase and some red items less visible. Examples of choice architecture changes included: rearranging items in the beverage and sandwich refrigerators to put all the green items at eye level; placing baskets of bottled water throughout the cafeteria; and providing pre-packaged salads next to the pizza counter. There were no significant changes in the food or beverage items offered in the cafeteria during the entire study period.
Outcomes
Sales data from the cash registers were used to track purchases throughout the study. For analyses of all cafeteria purchases, the dependent variables were binary indicators of whether a food item was labeled green/not green, yellow/not yellow, or red/not red. For the employee cohort, the outcomes were the proportions of cafeteria items purchased by each employee at baseline and at 12- and 24-month follow-up that were labeled green, yellow, or red. Each color proportion was a separate outcome. Purchases of cold beverages, which represented approximately 20% of total cafeteria sales at baseline, were assessed separately. To assess the impact of the intervention on overall cafeteria revenue, mean daily cafeteria sales, mean daily transactions, and mean dollars spent per transaction were calculated for each 3-month period. For employees using platinum plate cards, purchases were linked to sociodemographic data from human resources files. Data were available on employee age, gender, job type, and self-reported race/ethnicity (white, black, Asian, or Latino). Human resources data did not provide information on race and ethnicity separately. Job types were aggregated into five categories that roughly correlated with increasing education attainment: service workers (manual and/or unskilled laborers); support staff; technicians (e.g., radiology technicians, respiratory therapists); professionals (e.g., occupational therapists, pharmacists); and management/clinicians (e.g., hospital managers, physicians, nurses). Education was inconsistently reported by employees. For those who did report their education, 90% of service workers had a high school education or less, and 83% of professionals and management/clinicians had a bachelor’s degree or higher.
Statistical Analysis
Weekend and holiday sales are excluded from all reported statistics. Holiday sales included the period between December 24 and the first business day following New Year’s Day, a time when the cafeteria has less business. Statistical analyses focused on purchases in the initial 3-month baseline period compared to the 3-month periods at 12- and 24-month follow-up. Hypothesis testing for analyses of all cafeteria purchases used logistic regression to assess changes in the likelihood of purchasing items labeled with a specific color from baseline to each follow-up period adjusting for day of the week and clustering by period. Analyses of the employee cohort’s purchases used linear regression with employee-specific random effects to account for the non-independence of employees’ purchases over time. The random effects models controlled for employee age, gender, full-/part-time work status, race, and job type. The 1.7% of employees missing any sociodemographic data were excluded from the analysis. To assess whether changes in purchasing varied by race or ethnicity, time by race interaction terms were created and assessed for joint significance. All analyses were conducted in 2012 using Stata 12.1.
Results
From December 2009 through February 2012 (3-month baseline period followed by 24-month follow-up period), there was a daily mean of 16,834 items sold in the cafeteria, including 3444 cold beverages, and a mean of 6511 transactions. During the entire 27 months of the study, 2285 employees met inclusion criteria of making at least 3 transactions during each 3-month period, and among this cohort, the mean number of transactions per employee per period was 32. The mean age of employees was 43 years, and 73% were female. Employees self-identified their race as white (75%), Asian (7%), black (10%), or Latino (8%). Employees were categorized into the following job types: service workers (8%), support staff (12%), technicians (9%), professionals (14%), and management/clinicians (58%).
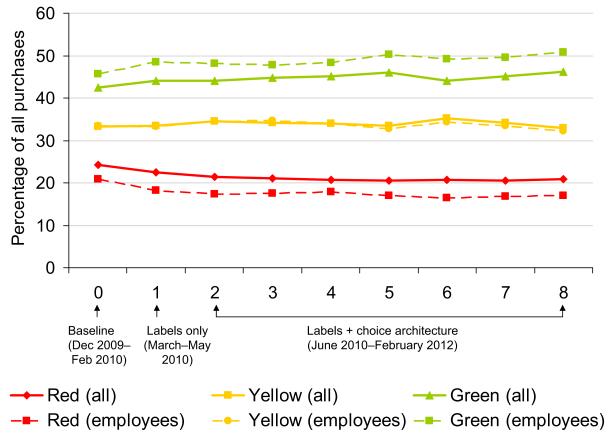
Figure 1 shows the proportion of green, yellow, and red purchases for all cafeteria customers and for the cohort of regular employee customers from December 2009 through February 2012. For all cafeteria purchases, the proportion of red items decreased from 24% of all purchases during the baseline period to 21% at 12 months and remained 21% at 24-month follow-up (p<0.001 for both compared to baseline). Green items increased from 41% at baseline to 45% at 12 months and 46% at 24 months (p <0.001 for both compared to baseline). Figure 2 shows the proportion of green, yellow, and red beverage purchases for all cafeteria customers and for the cohort of regular employee customers. For all cafeteria customers, the proportion of red beverages decreased from 27% at baseline to 17% at 12 months and 18% at 24 months (p <0.001 for both), and green beverages increased from 52% of all beverage purchase at baseline to 59% at 12 months and 60% at 24 months (p <0.001 for both). Changes in green and red purchases at 12 and 24 months for the employee cohort in Figures 1 and 2 were similar to all cafeteria customers. Table 1 shows the absolute percentages of green, yellow, and red purchases by the cohort of employees at baseline and at 12- and 24-month follow up as well as the relative percent change from baseline to 24-month follow-up. The largest changes occurred for red items, with the sales of all red items decreasing by 20% and red beverages decreasing by 39%. A sensitivity analysis to determine if frequency of cafeteria use affected purchasing patterns demonstrated that frequent users (at least 10 purchases every 3-month period) and less frequent users (no purchase requirement) had similar changes in green and red purchases over the entire 2-year follow-up (data not shown).
Figure 1.
Purchases by (1) all customers and (2) a cohort of regular employee customers, from baseline to 24 months following implementation of the cafeteria intervention.
Note: Each number 0–8 on the X axis represents a 3-month period of time.
Figure 2.
Beverage purchases by (1) all customers and (2) a cohort of regular employee customers, from baseline to 24 months following implementation of the cafeteria intervention.
Note: Each number 0–8 on the X axis represents a 3-month period of time.
Table 1.
Cafeteria purchases of red and green-labeled items by the cohort of employees at baseline and follow-up
| Baseline (no intervention) (Dec. 2009–Feb. 2010) |
12-month follow- up (Dec. 2010–Feb. 2011) |
24-month follow-up (Dec. 2011–Feb. 2012) |
|||
|---|---|---|---|---|---|
| Proportionc of Purchases, % |
Proportionc of Purchases, % |
Proportionc of purchases, % |
Relative change from baseline, % |
p value |
|
| All cafeteria purchasesa |
|||||
| Red | 20 | 16 | 16 | −20 | <0.001 |
| Yellow | 34 | 33 | 32 | −4 | <0.001 |
| Green | 46 | 50 | 52 | 12 | <0.001 |
| Beverage purchasesb |
|||||
| Red | 23 | 14 | 14 | −39 | <0.001 |
| Yellow | 17 | 22 | 20 | 16 | <0.001 |
| Green | 60 | 64 | 66 | 10 | <0.001 |
Proportions in table may not add to 100% due to rounding
Proportions are of all cafeteria purchases.
Proportions are of all cold beverage purchases.
Adjusted for employee age, gender, race, job type, and full/part-time work status.
Table 2 shows the absolute percentages and relative percent changes during follow up for beverage purchases of employees by race/ethnicity and job type. At 24-month follow-up, purchases of green beverages increased and red beverages decreased compared to baseline for employees from all racial/ethnic backgrounds and from all job types. Similar but slightly smaller changes were observed for all purchases, and analyses of employee purchases by age and gender did not demonstrate any important differences (data not shown).
Table 2.
Beverages purchases at baseline and follow-up by race/ethnicity and job category for the cohort of employees
| Baseline (no intervention) (Dec 2009–Feb 2010) |
12-month follow-up (Dec 2010– Feb 2011) |
24-month follow-up (Dec 2011–Feb 2012) |
|||
|---|---|---|---|---|---|
| Proportion of beverage purchases, % |
Proportion of beverage purchases, % |
Proportion of beverage purchases, % |
Relative change from baseline, % |
p value |
|
| RED BEVERAGES | |||||
| Race/ethnicitya | |||||
| White | 20 | 12 | 12 | −42 | <0.001 |
| Asian | 27 | 13 | 16 | −42 | <0.001 |
| Latino | 30 | 22 | 20 | −31 | <0.001 |
| Black | 32 | 22 | 23 | −29 | <0.001 |
| Job categoryb | |||||
| Management/clinician | 21 | 12 | 12 | −44 | <0.001 |
| Professionals | 21 | 14 | 14 | −35 | <0.001 |
| Technicians | 26 | 15 | 17 | −34 | <0.001 |
| Support staff | 29 | 20 | 18 | −38 | <0.001 |
| Service workers | 29 | 23 | 22 | −23 | <0.001 |
|
GREEN
BEVERAGES |
|||||
| Race/ethnicitya | |||||
| White | 64 | 69 | 69 | 9 | <0.001 |
| Asian | 50 | 53 | 59 | 18 | 0.002 |
| Latino | 48 | 50 | 57 | 17 | 0.001 |
| Black | 48 | 48 | 54 | 13 | 0.005 |
| Job categoryb | |||||
| Management/clinician | 57 | 62 | 62 | 9 | <0.001 |
| Professionals | 56 | 62 | 62 | 11 | 0.002 |
| Technicians | 47 | 51 | 56 | 21 | <0.001 |
| Support staff | 48 | 51 | 57 | 17 | <0.001 |
| Service workers | 47 | 46 | 52 | 11 | 0.04 |
Proportions in table may not add to 100% due to rounding
All numbers adjusted for job type, age, gender, and full/part–time work status.
All numbers adjusted for race, age, gender, and full/part–time work status.
Table 3 shows the overall cafeteria sales and transactions at baseline and 12- and 24-month follow-up. Overall cafeteria sales, including beverage sales, were stable over the 2-year period, with significant, but relatively small, increases.
Table 3.
Cafeteria transactions and revenue at baseline and follow–up
| Baseline (no intervention) (Dec 2009–Feb 2010) |
12–month follow–up (Dec 2010–Feb 2011) |
24–month follow–up (Dec 2011–Feb 2012) |
p–value for 24 months compared to baseline |
|
|---|---|---|---|---|
| Number of daily transactions (mean) |
6,511 | 7,136 | 6,688 | 0.004 |
| Overall daily cafeteria revenue (mean) |
$31,289 | $34,631 | $32,647 | <0.001 |
| Daily beverage revenue (mean) |
$4,350 | $4,860 | $4,489 | 0.007 |
| Amount spent per transaction (mean) |
$4.81 | $4.85 | $4.88 | <0.001 |
Discussion
This is the first study to evaluate the long-term effectiveness of a food labeling intervention to promote healthier choices. This study analyzed objective sales data over time rather than relying on cross-sectional customer surveys and self-reported purchasing behavior, and found that a traffic-light labeling and choice architecture intervention in a large hospital cafeteria resulted in sustained improvements in healthy food and beverage choices over 2 years, including among a longitudinal cohort of hospital employees from diverse backgrounds. These results suggest that simple food environment interventions can play a major role in public health policies to reduce obesity.
The food industry has opposed various nutrition and menu labeling strategies, arguing that there is scientific uncertainty regarding the effectiveness of labeling policies.23 Indeed, previous research has provided some mixed results regarding calorie labeling in the U.S.17,24–29 However, these observational studies are cross-sectional in design and subject to confounding. There is evidence from experimental studies that demonstrate short-term effectiveness of labeling, and research suggests that traffic-light labels are particularly effective for changing behavior.13–16,18,30 A major gap in the evidence for food labeling is whether individuals will continue to make healthier choices over time or whether they develop “fatigue” for the labels and revert to previous unhealthy choices. These results strongly support a sustained effect of a food environment intervention utilizing traffic-light labels, particularly among the longitudinal cohort of employees who visited the cafeteria frequently. These effects were consistent among employees of all racial/ethnic and job type subgroups, demonstrating that the intervention was effective for individuals from diverse cultural and educational backgrounds.
A second aspect of this cafeteria intervention was choice architecture. The results of this study were unable to separate out the effects of the labeling and the choice architecture since both interventions were incorporated into the cafeteria as permanent changes. In the initial 6 months of the intervention, the largest changes in red and green purchases occurred when the labels were implemented, but sequentially adding choice architecture further decreased red sales and increased green sales.13,14 In the current study, purchases of the red and green items remained remarkably stable over the 18 months following the addition of the choice architecture intervention to the labels.
Although the details of these labeling criteria and product placement interventions may be debated, the results clearly demonstrate that individuals exposed to food labeling and environmental interventions will change their behavior to make healthier choices over an extended period of time. The intervention effect was strongest for beverages, with a 39% reduction in purchase of unhealthy beverages by employees over 2 years. Sugar-sweetened beverages are associated with obesity, diabetes, cardiovascular disease, and other chronic diseases.31–34 Reducing consumption of sugar-sweetened beverages on a daily basis is associated with weight loss35 and therefore can help prevent obesity-related metabolic disease. Point-of-purchase interventions that discourage sugar-sweetened beverages are likely to have a considerable impact on excess calorie consumption in the population.
The food industry can play an important role in addressing the obesity epidemic without compromising their success and profit. Despite labeling both healthy and unhealthy foods and beverages in this study, overall cafeteria sales revenue and daily transaction counts showed that the business remained robust throughout the study period. These results are consistent with other preliminary data showing that food companies and restaurants that offered low-calorie and healthier food choices had stronger sales growth between 2006 and 2011 than companies and restaurants that did not offer these options.36
This study does have limitations. The intervention was conducted at one hospital cafeteria in an urban setting in the U.S., and the findings may not be generalizable to all settings. This was a longitudinal study that did not have a control site. However, analyses of employees were based on within-person changes in purchasing and were not vulnerable to the biases associated with a changing population, and purchasing patterns for all analyses showed consistent patterns over the 2-year period.
The results of this study provide strong evidence that a simple traffic-light labeling and choice architecture intervention can improve healthy food and beverage choices of a diverse population over a sustained period of time. Cumulative small changes in eating behaviors across the population could lead to substantial reductions in the prevalence of obesity and obesity-related diseases. In the future, collaboration between public health officials, policymakers, and the food industry has potential to promote healthier population eating behaviors without compromising individual choice or business success.
Acknowledgments
We would like to thank Susan J. Barraclough, MS, RD, the Director of Nutrition and Food Services at Massachusetts General Hospital for her leadership, support, and oversight of the implementation and maintenance of the cafeteria intervention.
This research is supported by the Robert Wood Johnson Foundation’s Pioneer Portfolio and the Donaghue Foundation through the grant, “Applying Behavioral Economics to Perplexing Health and Health Care Challenges.” Dr. Thorndike is supported by the NIH/National Heart Lung and Blood institute grant K23 HL93221. Neither the NIH nor the Robert Wood Johnson and Donaghue Foundations had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
No other financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Finucane MM, Stevens GA, Cowan MJ, et al. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Body Mass Index). National, regional, and global trends in body-mass index since 1980: Systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377(9765):557–67. doi: 10.1016/S0140-6736(10)62037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang YC, McPherson K, Marsh T, Gortmaker SL, Brown M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011;378(9793):815–25. doi: 10.1016/S0140-6736(11)60814-3. [DOI] [PubMed] [Google Scholar]
- 3.Swinburn BA, Sacks G, Hall KD, et al. The global obesity pandemic: Shaped by global drivers and local environments. Lancet. 2011;378(9793):804–14. doi: 10.1016/S0140-6736(11)60813-1. [DOI] [PubMed] [Google Scholar]
- 4.Gortmaker SL, Swinburn BA, Levy D, et al. Changing the future of obesity: Science, policy, and action. Lancet. 2011;378(9793):838–47. doi: 10.1016/S0140-6736(11)60815-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krukowski RA, Harvey-Berino J, Kolodinsky J, Narsana RT, Desisto TP. Consumers may not use or understand calorie labeling in restaurants. J Am Diet Assoc. 2006;106(6):917–20. doi: 10.1016/j.jada.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 6.Elbel B. Consumer estimation of recommended and actual calories at fast food restaurants. Obesity (Silver Spring) 2011;19(10):1971–8. doi: 10.1038/oby.2011.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marteau TM, Hollands GJ, Fletcher PC. Changing human behavior to prevent disease: The importance of targeting automatic processes. Science. 2012;337(6101):1492–5. doi: 10.1126/science.1226918. [DOI] [PubMed] [Google Scholar]
- 8.Wansink B, Just DR, Payne CR. Mindless eating and healthy heuristics for the irrational. American Economic Review: Papers & Proceedings. 2009;99(2):165–9. doi: 10.1257/aer.99.2.165. [DOI] [PubMed] [Google Scholar]
- 9.Rozin P, Scott S, Dingley M, Urbanek JK, Jiang H, Kaltenbach M. Nudge to nobesity I: Minor changes in accessibility decrease food intake. Judgment and Decision Making. 2011 Jun;6(4):323–32. [Google Scholar]
- 10.Dayan E, Bar-Hillel M. Nudge to nobesity II: Menu positions influence food orders. Judgment and Decision Making. 2011 Jun;6(4):333–42. [Google Scholar]
- 11.Schwartz J, Riis J, Elbel B, Ariely D. Inviting consumers to downsize fast-food portions significantly reduces calorie consumption. Health Aff (Millwood) 2012;31(2):399–407. doi: 10.1377/hlthaff.2011.0224. [DOI] [PubMed] [Google Scholar]
- 12.Rothman RL, Housam R, Weiss H, et al. Patient understanding of food labels: The role of literacy and numeracy. Am J Prev Med. 2006;31(5):391–8. doi: 10.1016/j.amepre.2006.07.025. [DOI] [PubMed] [Google Scholar]
- 13.Thorndike AN, Sonnenberg L, Riis J, Barraclough S, Levy DE. A 2-phase labeling and choice architecture intervention to improve healthy food and beverage choices. Am J Public Health. 2012;102(3):527–33. doi: 10.2105/AJPH.2011.300391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy DE, Riis J, Sonnenberg LM, Barraclough SJ, Thorndike AN. Food choices of minority and low-income employees: A cafeteria intervention. Am J Prev Med. 2012;43(3):240–8. doi: 10.1016/j.amepre.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borgmeier I, Westenhoefer J. Impact of different food label formats on healthiness evaluation and food choice of consumers: A randomized-controlled study. BMC Public Health. 2009;9:184. doi: 10.1186/1471-2458-9-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly B, Hughes C, Chapman K, et al. Consumer testing of the acceptability and effectiveness of front-of-pack food labelling systems for the Australian grocery market. Health Promot Internation. 2009;24(2):120–9. doi: 10.1093/heapro/dap012. [DOI] [PubMed] [Google Scholar]
- 17.Roberto CA, Larsen PD, Agnew H, Baik J, Brownell KD. Evaluating the impact of menu labeling on food choices and intake. Am J Public Health. 2010;100(2):312–8. doi: 10.2105/AJPH.2009.160226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hawley KL, Roberto CA, Bragg MA, Liu PJ, Schwartz MB, Brownell KD. The science of front-of-package food labels. Public Health Nutr. 2013;16(3):430–9. doi: 10.1017/S1368980012000754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Downs JS, Loewenstein G, Wisdom J. Strategies for promoting healthier food choices. American Economic Review: Papers & Proceedings. 2009;99:159–64. doi: 10.1257/aer.99.2.159. [DOI] [PubMed] [Google Scholar]
- 20.Skov LR, Lourenco S, Hansen GL, Mikkelsen BE, Schofield C. Choice architecture as a means to change eating behaviour in self-service settings: A systematic review. Obes Rev. 2013;14:187–96. doi: 10.1111/j.1467-789X.2012.01054.x. [DOI] [PubMed] [Google Scholar]
- 21.Sacks G, Veerman JL, Moodie M, Swinburn B. ‘Traffic-light’ nutrition labelling and ‘junk-food’ tax: A modelled comparison of cost-effectiveness for obesity prevention. Int J Obes (Lond) 2011;35(7):1001–9. doi: 10.1038/ijo.2010.228. [DOI] [PubMed] [Google Scholar]
- 22.United States Department of Agriculture [Updated 2005. June 11];Dietary guidelines for Americans. 2009 www.mypyramid.gov/guidelines/index.html.
- 23.Ludwig DS, Brownell KD. Public health action amid scientific uncertainty: The case of restaurant calorie labeling regulations. JAMA. 2009;302(4):434–5. doi: 10.1001/jama.2009.1045. [DOI] [PubMed] [Google Scholar]
- 24.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int J Behav Nutr Phys Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bassett MT, Dumanovsky T, Huang C, et al. Purchasing behavior and calorie information at fast-food chains in New York City, 2007. Am J Public Health. 2008;98(8):1457–9. doi: 10.2105/AJPH.2008.135020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pulos E, Leng K. Evaluation of a voluntary menu-labeling program in full-service restaurants. Am J Public Health. 2010;100(6):1035–9. doi: 10.2105/AJPH.2009.174839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: a first look at the effects on low-income people in New York City. Health Aff (Millwood) 2009;28(6):w1110–21. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 28.Dumanovsky T, Huang CY, Nonas CA, Matte TD, Bassett MT, Silver LD. Changes in energy content of lunchtime purchases from fast food restaurants after introduction of calorie labelling: cross sectional customer surveys. BMJ. 2011;343:4464. doi: 10.1136/bmj.d4464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finkelstein EA, Strombotne KL, Chan NL, Krieger J. Mandatory menu labeling in one fast-food chain in King County, Washington. Am J Prev Med. 2011;40:122–7. doi: 10.1016/j.amepre.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 30.Roberto CA, Bragg MA, Schwartz MB, et al. Facts up front versus traffic light food labels: a randomized controlled trial. Am J Prev Med. 2012;43(2):134–41. doi: 10.1016/j.amepre.2012.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Brownell KD, Farley T, Willett WC, et al. The public health and economic benefits of taxing sugar-sweetened beverages. N Engl J Med. 2009;361(16):1599–1605. doi: 10.1056/NEJMhpr0905723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bleich SN, Wang YC, Wang Y, Gortmaker SL. Increasing consumption of sugar-sweetened beverages among U.S. adults: 1988–1994 to 1999–2004. Am J Clin Nutr. 2009;89(1):372–81. doi: 10.3945/ajcn.2008.26883. [DOI] [PubMed] [Google Scholar]
- 33.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation. 2010;121(11):1356–64. doi: 10.1161/CIRCULATIONAHA.109.876185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Malik VS, Popkin BM, Bray GA, Després JP, Willett WC, Hu FB. Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis. Diabetes Care. 2010;33:2477–83. doi: 10.2337/dc10-1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen L, Appel LJ, Loria C, et al. Reduction in consumption of sugar-sweetened beverages is associated with weight loss: The PREMIER trial. Am J Clin Nutr. 2009;89(5):1299–1306. doi: 10.3945/ajcn.2008.27240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cardello H, Wolfson J, Yufera-Leitch M, Warren L, Spitz M. Better-for-you foods: An opportunity to improve public health and increase food industry profits. Hudson Institute; Washington DC: [April 8, 2013]. Mar, 2013. www.hudson.org/files/publications/better_for_you_combinedFINAL.pdf. [Google Scholar]