Abstract
The lateral positioning used for the lateral suboccipital surgical approach is associated with various pathophysiologic complications. Strategies to avoid complications including an excessive load on the cervical vertebra and countermeasures against pressure ulcer development are needed. We retrospectively investigated positioning-related complications in 71 patients with cerebellopontine angle lesions undergoing surgery in our department between January 2003 and December 2010 using the lateral suboccipital approach. One patient postoperatively developed rhabdomyolysis, and another presented with transient peroneal nerve palsy on the unaffected side. Stage I and II pressure ulcers were noted in 22 and 12 patients, respectively, although neither stage III nor more severe pressure ulcers occurred. No patients experienced cervical vertebra and spinal cord impairments, brachial plexus palsy, or ulnar nerve palsy associated with rotation and flexion of the neck. Strategies to prevent positioning-related complications, associated with lateral positioning for the lateral suboccipital surgical approach, include the following: atraumatic fixation of the neck focusing on jugular venous perfusion and airway pressure, trunk rotation, and sufficient relief of weightbearing and protection of nerves including the peripheral nerves of all four extremities.
Keywords: lateral suboccipital approach, positioning-related complications, pressure ulcer, cerebellopontine angle tumor
Introduction
With the lateral positioning used for surgery via the lateral suboccipital approach, patients must be monitored for various pathophysiologic complications because lesions may develop at the cerebellopontine angle, in which several important structures are located close to each other. To perform surgery in a comfortable posture in consideration of the microscopic visual axis, it is necessary to establish a lateral position that alleviates venous perfusion pressure elevation and increased airway pressure, allowing the cerebellum to be retracted easily. Adjusting the head position within various angles and the accommodation of various body weights, to prevent excessive force on the cervical vertebra and increased skin pressure from the operation table and its attachments, are also essential.
We retrospectively investigated positioning-related complications associated with the lateral suboccipital approach. We report technical points as well as describing the devices we use to avoid these complications.
Patients and Methods
Positioning-related complications following surgery using the lateral suboccipital approach were retrospectively investigated in 71 patients with cerebellopontine angle lesions who underwent operations at our department between January 2003 and December 2010 (Table 1). Seven patients underwent staged surgeries. The present analysis is based on the first surgery. Pressure ulcer severity was evaluated using the National Pressure Ulcer Advisory Panel classification.
Table 1. Characteristics of 71 patients.
| Parameter | No./Value |
|---|---|
| No. of patients | 71 |
| Male-to-female ratio | 28:43 |
| Age, y, median (range) | 57 (16–81) |
| Operative duration, min, median (range) | 608 (210–1060) |
| Body weight, kg, median (range) | 57.2 (39.6–97.8) |
| Disease | |
| Schwannoma | 26 |
| VS | 23 |
| JFS | 2 |
| TS | 1 |
| CPA MN | 16 |
| HFS/TGN | 13 |
| Others | 16 |
Abbreviations: VS, vestibular schwannoma; JFS, jugular foramen schwannoma; TS, trigeminal schwannoma; CPA, cerebellopontine angle; MN, meningioma; HFS, hemifacial spasm; TGN, trigeminal neuralgia.
We briefly introduce our methods for establishing suitable lateral positions. Patients are first placed in the supine position, and then in a lateral position with the trunk rotated 30 to 60 degrees toward the unaffected side. The patient's head is then rotated toward the unaffected side, maintaining the vertex down and neck flexion position, and suitably fixed for surgical approaches dependent on the locations and sizes of lesions. We clinically determine the safe limits of the range of rotation and flexion, that is, those not causing neurologic symptoms, by positioning the neck in the outpatient clinic and at the bedside in all patients. To prevent jugular venous obstruction and elevation of tracheal tube cuff pressure, an approximately two-finger breadth space is always secured between the mandible and clavicle.
Results
There were 28 male and 43 female patients with an average age of 57 years (range: 16–81 years). The mean duration of surgery was 608 minutes (10 hours and 8 minutes; range: 3 hours and 30 minutes to 17 hours and 40 minutes). The lesions were schwannoma in 26 cases (vestibular 23, jugular foramen 2, and trigeminal 1), cerebellopontine angle meningioma in 16, microvascular decompression for facial spasm and trigeminal neuralgia in 13, and others in 16 (Table 1). None of these cases showed impairment of jugular venous perfusion or failure of cerebellar retraction due to pressure elevation in the airway. A young male patient developed rhabdomyolysis, and another presented with transient peroneal nerve palsy on the unaffected side after surgery due to insufficient protection of the lateral knee region on the unaffected side. Stage I and II pressure ulcers were noted in the axilla and lateral thoracic region after surgery in 22 and 12 patients, respectively; however, none of our patients developed stage III or higher severe pressure ulcers (Fig. 1). No patients showed cervical vertebra and spinal cord impairments, brachial plexus palsy, or ulnar nerve palsy associated with rotation and flexion of the neck (Table 2).
Fig. 1.

This photograph shows a pressure ulcer that developed on the chest of the unaffected side after surgery via the lateral suboccipital approach (National Pressure Ulcer Advisory Panel stage I).
Table 2. Complications related to the lateral position.
| Complication | No. |
|---|---|
| Rhabdomyolysis | 1 |
| Deep peroneal nerve palsy | 1 |
| Pressure ulcera | |
| Stage I | 22 |
| Stage II | 12 |
National Pressure Ulcer Advisory Panel classification.
To identify factors involved in postoperative pressure ulcer formation, gender, age, operative duration, and body weight were compared in the 71 surgical patients between those with postoperative pressure ulcers on the trunk (ulcer group: UG) and those without (no ulcer group: NUG). Gender was analyzed as a factor using the chi-square test, and age, operative duration, and body weight were analyzed using the Student t test. The incidence of pressure ulcers on the trunk did not differ significantly between men and women; nor was there a significant age-related difference. The mean operative duration was 714 minutes (11 hours and 54 minutes) in the UG and 510 minutes (8 hours and 30 minutes) in the NUG, showing a significantly longer duration of surgery in the UG (p < 0.05 by Student t test). Mean body weight was 60 kg in the UG and 55 kg in the NUG, thus significantly greater in the former (p < 0.05 by Student t test) (Table 3).
Table 3. Factors related to pressure ulcer development.
| UG | NUG | p value | |
|---|---|---|---|
| No. of patients (%) | 34 (48) | 37 (52) | |
| Male-to-female ratio | 15:19 | 13:24 | NSa |
| Age, y, median (range) | 56 (31–76) | 58(16–81) | NSb |
| Operative duration, min, median (range) | 714 (305–1060) | 510 (210–940) | <0.05b |
| Body weight, kg, median (range) | 60 (41–98) | 55 (40–76) | <0.05b |
Abbreviations: UG, ulcer group; NUG, no ulcer group; NS, not significant.
Assessed by chi-square test.
Assessed by Student t test.
Discussion
Positioning is more variable and complicated in neurosurgery than in general surgery. Even a tiny alteration in a patient's position can markedly influence cerebral retraction and the operator's posture, ultimately having an impact on the surgical outcome. Positioning-related complications often depend on pathophysiologic states caused by complex positioning requirements, and sufficient attention should be paid to avoiding these complications.
The lateral position is frequently used in neurosurgery mainly for cerebellopontine angle tumors, such as vestibular schwannoma and meningioma, and microvascular decompression for facial spasm and trigeminal neuralgia. The lateral position is more variable and complex than the simple supine and prone positions, and modifications include the park-bench position,1 2 3 three-quarter prone position,4 and prone oblique position.5 Because the location and size of lesions, physical structure, and mobility of the cervical vertebra vary among patients, selection of the optimal position for each case is essential.
The head is fixed, paying attention to the degrees of rotation toward the unaffected side (contralateral rotation), vertex down, and neck flexion. During surgery for vestibular schwannoma, the microscopic visual axes can change within a broad range from the brainstem side to the petrous bone surface, from the lower cranial nerves to the tentorial side. Such maneuvers continuously expose important structures. To minimize traction of the cerebellum induced by a forced posture for surgeons, the degrees of head rotation and vertex down should be adequate. The look-through method is useful and frequently used in our department, in which the intraoperative microscopic visual axis assumed from the head position and lesion is confirmed using magnetic resonance imaging look-through film. The occipital bone surface is covered by thick occipital muscles and physiologically located in a deep region. Adding anteflexion to the head position renders the occipital bone surface (particularly the foramen magnum) accessible at a shallow site, facilitating craniotomy.
Head fixation for the lateral suboccipital approach is complex, and rotation and flexion of the neck may result in an excessive force load on the neck and cervical vertebra in many cases. In addition to preoperative imaging screening for cervical vertebral hernia and cervical spondylosis, it is necessary to identify safe limits of rotation and flexion that do not cause neurologic symptoms by positioning the neck in the outpatient clinic and at the bedside. Excess flexion and rotation of the neck unfortunately can produce cervical rotation–associated vertebral arterial obstruction (latent bow hunter's syndrome) and salivary gland obstruction–induced acute sialadenitis.1 6 We do not use the supine position with the head turned to the opposite side because neck rotation could be excessive in this position. When jugular vein perfusion is impaired and pressure in the airway rises due to a passive force loaded onto the neck, cerebellar retraction becomes insufficient, necessitating intraoperative traction of the cerebellum that may subsequently cause cerebellar contusion and congestive brain infarction. To obtain sufficient venous perfusion, we always secure an approximately two-finger breadth space between the mandible and clavicle. To prevent elevation of tracheal tube cuff pressure due to rotation and flexion of the neck and rising pressure in the airway due to kinking of the tube, cooperation with anesthesiologists is important.
Because weightbearing deviates toward one side in the lateral position, modifications to protect and remove weightbearing on the upper and lower limbs on the unaffected side (underside) are necessary. In regions with a shallow distribution and low mobility of peripheral nerves, pressure on a local region for a prolonged period can cause peripheral neuropathy. To use the lateral position, it is necessary to understand the anatomical distribution of the brachial plexus and the ulnar and peroneal nerves (Fig. 2). The brachial plexus distributes directly below the humeral head in the shoulder joint, and its mobility is limited by the humeral head. When traction of the shoulder on the unaffected side toward the caudal side is added to lateral bending of the head toward the healthy side, the brachial plexus is compressed, which may cause brachial plexus impairment after surgery. The ulnar nerve is on the medial side of the elbow and passes through the cubital tunnel in the humeral epicondylar region. Because the cubital tunnel is narrow, and neuropathy is readily induced by compression of this tunnel, direct contact of the medial elbow on the unaffected side with the bed and fixation devices for a prolonged period should be avoided.7 The common peroneal nerve in the leg distributes to the lateral side of the peroneal head and bifurcates to the superficial and deep peroneal nerves and the tibial nerve. Since the skin is thin and mobility is minimal on the lateral side of the popliteal fossa, attention should be paid to sufficient protection of and non-weightbearing on this region of the healthy leg. We experienced a case of postoperative peroneal nerve palsy on the unaffected side that required 6 months to resolve. Decompression and protection of the lateral region of the popliteal fossa must be performed very carefully.
Fig. 2.
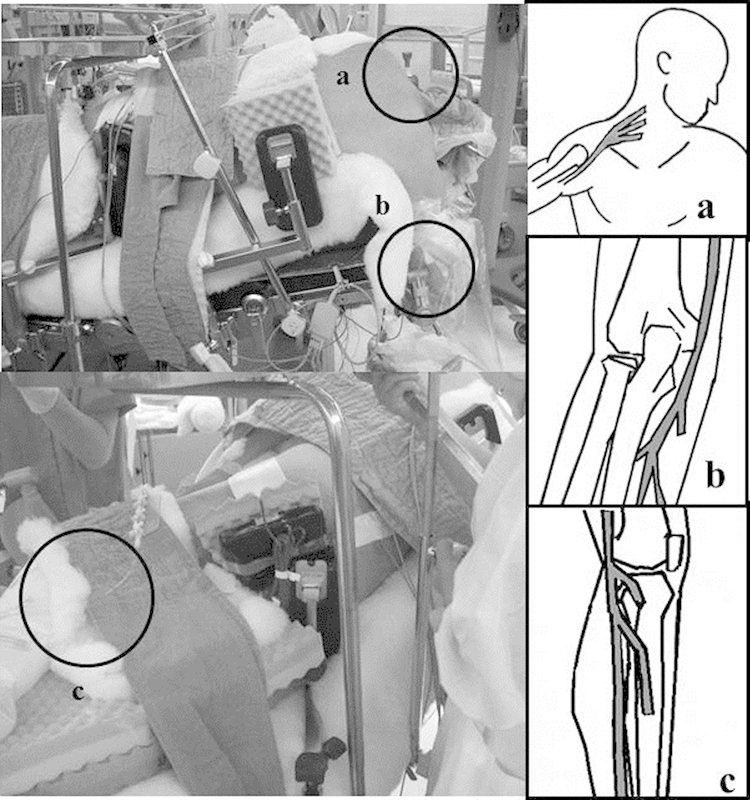
These drawings and photographs show the weak points of peripheral nerves that are easily affected while the patient is in the lateral position. (A) Brachial plexus, (B) ulnar nerve, (C) peroneal nerve.
Stage I or II pressure ulcers on the trunk developed after surgery in 34 patients (48% of 71 patients). Local pressure increases as the trunk skin area in contact with the bed decreases, as compared with the supine and prone positions, increasing the incidence of pressure ulcers. Particularly, pressure ulcers in the axilla over the precordia directly cause postoperative pain and dyspnea, markedly reducing the patient's activities of daily living. Comparisons between the UG and NUG revealed operative duration and body weight to be possible risk factors for pressure ulcers related to surgery conducted with the patient in a lateral position. Countermeasures against pressure ulcers, based on the physiques and surgical procedures of individual patients, are essential. We experienced a rare case in which rhabdomyolysis developed despite no superficial skin injury being present in a nonobese young man (body mass index: 18.9). It may have been due to intraoperative hypotensive anesthesia-induced muscular ischemia and factors related to drugs such as propofol. It is necessary to fully recognize the risks associated with hypotensive anesthesia, dehydration, and drugs, in addition to the patient's physique and the duration of surgery.
The body pressure distribution on the skin in contact with the bed in the lateral position was analyzed using various parameters from the viewpoint of pressure ulcer prevention and peripheral nerve protection using an ErgoCheck (ABW, Hamburg, Germany) (Fig. 3). The local contact pressure was concentrated in the axillary region and great trochanter in all lateral positions, and the pressure could be dispersed and reduced using a low resilience type of foam. The skin contact area was widened and local pressure was dispersed by rotating the trunk forward. The local pressure on the axillary region was markedly reduced, by 59%, from 116.6 to 48.2 mm Hg (Fig. 4), demonstrating that trunk rotation is a suitable maneuver for the prevention of pressure ulcers. It is also useful to secure a favorable space for surgery of the lateral occipital bone surface because the shoulder, as an obstacle, can be avoided when the trunk is rotated forward.
Fig. 3.

(A) ErgoCheck measuring system (ABW, Hamburg, Germany). (B) Photograph of local body pressure measurements taken with the patient in the lateral position.
Fig. 4.
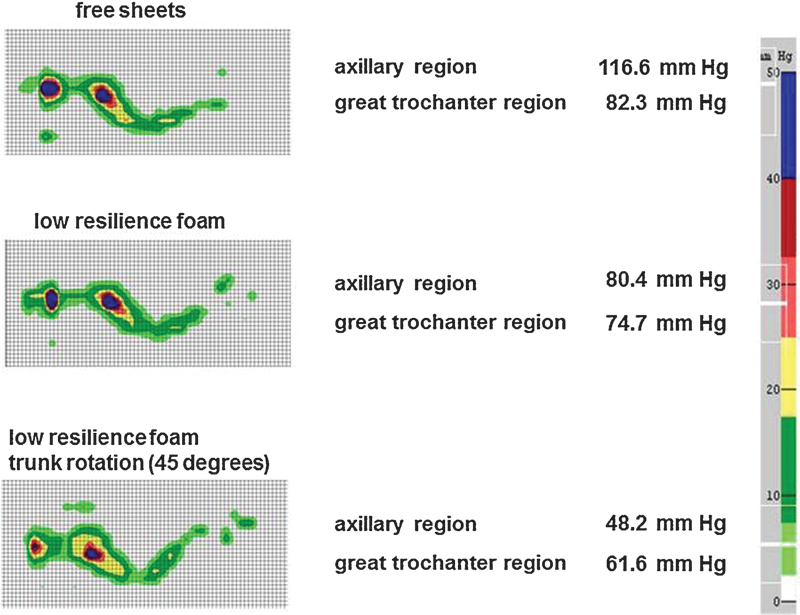
Local body pressure measurements in the lateral position show that local body pressure decreased when the trunk was rotated and when a low resilience type of foam was used.
We are currently trying to prevent pressure ulcers of the lateral thoracic region using a viscoelastic type of foam (Fig. 5). The previous low resilience foam was too soft, so the axillary region was crushed by weightbearing that interfered with sufficient body pressure dispersion. This disadvantage is reduced with the currently used material. The density of the viscoelastic foam is higher than that of the previous low resilience foam, showing a rubber-like viscosity, which ameliorated crushing of the axillary region and sufficiently dispersed body pressure by widely supporting not only the axilla but also the low back region. We used this foam for the four most recently performed surgeries, and none of these cases developed pressure ulcers. The use of this foam will be among the items examined in our future efforts to reduce postoperative complications.
Fig. 5.

Photograph of the new device made of viscoelastic foam (asterisk) and low resilience foam (double asterisk) (Cape Co., Yokosuka, Japan).
Conclusion
Fixation of the head in the lateral position used for the lateral suboccipital approach causes a variety of pathophysiologic conditions, leading to excess loads on the trunk and the neck. Positioning-related complications can potentially be minimized by atraumatic fixation of the neck taking jugular venous perfusion and airway pressure into account, trunk rotation, and placement of the patients in a stable position that sufficiently protects nerves including the peripheral nerves of the extremities.
References
- 1.Kim L J, Klopfenstein J D, Feiz-Erfan I, Zubay G P, Spetzler R F. Postoperative acute sialadenitis after skull base surgery. Skull Base. 2008;18(2):129–134. doi: 10.1055/s-2007-991110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.St-Arnaud D Paquin M J Safe positioning for neurosurgical patients Can Oper Room Nurs J 20092747–11., 16, 18–19 passim [PubMed] [Google Scholar]
- 3.Toung T J, McPherson R W, Ahn H, Donham R T, Alano J, Long D. Pneumocephalus: effects of patient position on the incidence and location of aerocele after posterior fossa and upper cervical cord surgery. Anesth Analg. 1986;65(1):65–70. [PubMed] [Google Scholar]
- 4.Ausman J I, Malik G M, Dujovny M, Mann R. Three-quarter prone approach to the pineal-tentorial region. Surg Neurol. 1988;29(4):298–306. doi: 10.1016/0090-3019(88)90161-9. [DOI] [PubMed] [Google Scholar]
- 5.Kikuta K I Miyamoto S Kataoka H Satow T Yamada K Hashimoto N Use of the prone oblique position in surgery for posterior fossa lesions Acta Neurochir (Wien) 2004146101119–1124.; discussion 1124 [DOI] [PubMed] [Google Scholar]
- 6.Singha S K, Chatterjee N. Postoperative sialadenitis following retromastoid suboccipital craniectomy for posterior fossa tumor. J Anesth. 2009;23(4):591–593. doi: 10.1007/s00540-009-0807-7. [DOI] [PubMed] [Google Scholar]
- 7.Winfree C J Kline D G Intraoperative positioning nerve injuries Surg Neurol 20056315–18.; discussion 18 [DOI] [PubMed] [Google Scholar]


