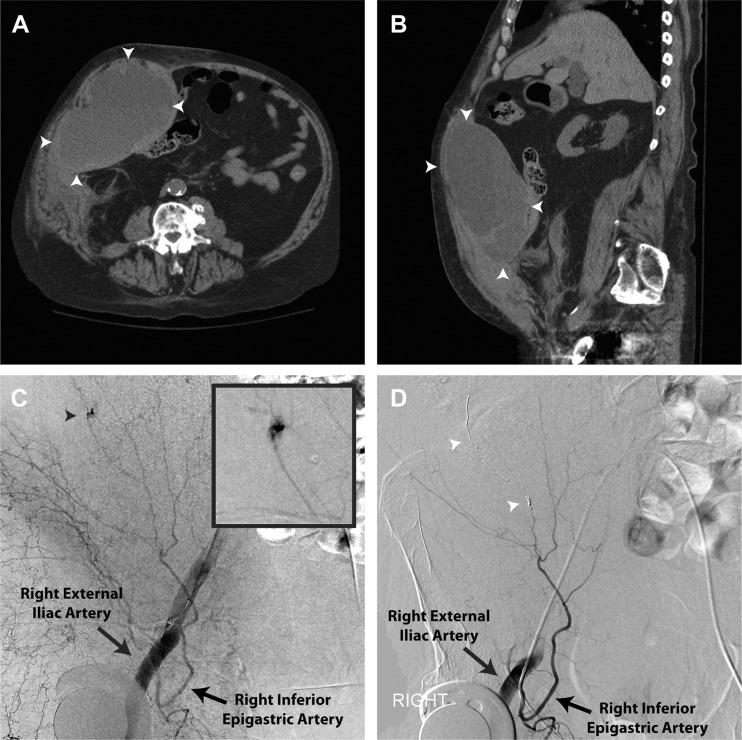
A75-year-old man with multiple myeloma and history of pulmonary embolism on warfarin anticoagulation presented with three days of worsening abdominal pain after a fall. His exam demonstrated a tender, unilateral abdominal mass that remained palpable with tensing of the rectus sheath (Fothergill’s sign).1 Initial hemoglobin was 5.7 g/dL, platelets 47,000/mm3, and INR 1.74. Computed tomography revealed a large right-sided rectus sheath hematoma (Figs. 1A, B). Blood products were administered and anticoagulation was reversed. However, repeat hemoglobin was 4.9 g/dL. Emergent angiography identified a hemorrhaging branch of the right inferior epigastric artery (Fig. 1C, black arrowhead and inset). One linear and two short coils were deployed achieving hemostasis (Fig. 1D, white arrowheads). Surgical evacuation was performed three days later due to overlying skin necrosis. He recovered without further incident and was discharged without anticoagulation.
Figure 1.
Embolization of a large rectus sheath hematoma.
Rectus sheath hematoma is an uncommon complication of anticoagulant therapy and usually self-tamponades. Conservative management includes anticoagulant reversal, fluids, and transfusion, if needed. Invasive measures are indicated if bleeding persists and compromises hemodynamic stability. Historically, surgical evacuation with vessel ligation was performed; however, percutaneous arterial embolization is a safe, effective, and less invasive alternative.2
REFERENCES
- 1.Osinbowale O, Bartholomew JR. Rectus sheath hematoma. Vasc Med. 2008;13:275–9. doi: 10.1177/1358863X08094767. [DOI] [PubMed] [Google Scholar]
- 2.Rimola J, Perendreu J, Falcó J, Fortuño JR, Massuet A, Branera J. Percutaneous arterial embolization in the management of rectus sheath hematoma. AJR Am J Roentgenol. 2007;188(6):W497–502. doi: 10.2214/AJR.06.0861. [DOI] [PubMed] [Google Scholar]