ABSTRACT
BACKGROUND
Patient activation is linked to better health outcomes and lower rates of health service utilization. The role of patient activation in the rate of hospital readmission within 30 days of hospital discharge has not been examined.
METHODS
A secondary analysis using data from the Project RED-LIT randomized controlled trial conducted at an urban safety net hospital. Data from 695 English-speaking general medical inpatient subjects were analyzed. We used an adapted, eight-item version of the validated Patient Activation Measure (PAM). Total scores were categorized, according to standardized methods, as one of four PAM levels of activation: Level 1 (lowest activation) through Level 4 (highest activation). The primary outcome measure was total 30-day post-discharge hospital utilization, defined as total emergency department (ED) visits plus hospital readmissions including observation stays. Poisson regression was used to control for confounding.
RESULTS
Of the 695 subjects, 67 (9.6 %) were PAM Level 1, 123 (17.7 %) were Level 2, 193 (27.8 %) were Level 3, and 312 (44.9 %) were Level 4. Compared with highly activated patients (PAM Level 4), a higher rate of 30-day post-discharge hospital utilization was observed for patients at lower levels of activation (PAM Level 1, incident rate ratio [IRR] 1.75, 95 % CI,1.18 to 2.60) and (PAM Level 2, IRR 1.50, 95 % CI 1.06 to 2.13). The rate of returning to the hospital among patients at PAM Level 3 was not statistically different than patients with PAM Level 4 (IRR 1.30, 95 % CI, 0.94 to 1.80). The rate ratio for PAM Level 1 was also higher compared with Level 4 for ED use alone (1.68(1.07 to 2.63)) and for hospital readmissions alone (1.93 [1.22 to 3.06]).
CONCLUSION
Hospitalized adult medical patients in an urban academic safety net hospital with lower levels of Patient Activation had a higher rate of post-discharge 30-day hospital utilization.
KEY WORDS: patient activation, readmission
INTRODUCTION
Hospital utilization (readmissions and emergency department visits) in the 30 days after hospital discharge is common and costly. In 2004, the rate of 30-day hospital readmissions among Medicare recipients was approximately 20 %, costing an estimated $17.4 billion.1 Including emergency department visits in post-discharge acute care use estimates increases utilization rates by as much as one-third.2,3 Unfortunately, a significant portion of this utilization may be unneeded. We found that approximately one-third of the hospital utilization events following discharge could be avoided with an intervention that improves clinician, patient, and family preparation for care transitions.4 Given the significant potential cost savings for even a modest impact on unnecessary readmissions during care transitions, it is not surprising that widespread efforts are underway to identify and address modifiable factors contributing to 30-day hospital utilization.
Our research, and the work of others, has identified several key risk factors for early unplanned hospital reutilization, including depression, low health literacy, male gender, advanced age, complex medication regimens and taking certain high risk medications.5–9 Collectively, the research suggests that a successful care transition depends on the patient’s ability to manage their discharge care plan upon returning home. The knowledge, skills, confidence and inclination to assume responsibility for managing one’s health and healthcare needs is often referred to as patient activation.10 Hibbard et al. developed the patient activation measure (PAM) to evaluate patient activation, its influence on health behaviors, and its response to supportive interventions.10 This research demonstrates that activated patients are more likely to obtain preventive care, maintain healthy lifestyle behaviors and experience a range of improved health outcomes than patients with low levels of activation.11,12
According to Hibbard and colleagues, patient activation is comprised of specific domains of attitudes, knowledge and skills patients require for disease self-management. This includes the belief that patients should engage in self-managing care, collaborating with providers, and maintaining their health. The activated patient should possess the knowledge and skills to: 1) self-manage symptoms/problems; 2) engage in activities that maintain functioning and reduce health declines; 3) be involved in shared decision making and collaboration with providers; and 4) navigate the health care system and access high quality care. Patients’ supportive care needs vary by activation level, and interventions should be tailored to target the appropriate knowledge and skill gaps.
In the hospital transition setting, a safe and effective hospital discharge is reliant on the patient’s activation level—that is, the ability to carry out what is frequently a complex treatment plan requiring disease self-management skills and the ability to seek and obtain healthcare in a timely and appropriate manner. It is conceivable then that for a patient without these skills (i.e., low patient activation) an acute event requiring hospitalization could be sufficiently debilitating to undermine the patient’s ability to learn and carry out important self-care duties in the post-discharge setting, resulting in an increased risk of an unplanned return to the hospital. While there have been both prospective and cross-sectional studies associating lower activation scores with higher risk of hospitalization,13–15 there have been no studies linking the activation score with readmissions or with 30-day unplanned readmissions. One Australian study did find higher readmission rates among patients categorized as frequent utilizers of hospital services compared with similar patients with chronic disease self-management support, suggesting a role for patient activation in reducing avoidable readmissions.16 This continues to be an important knowledge gap. Whereas initial hospitalization may be attributable to an acute illness or exacerbation of chronic disease, 30-day readmissions or ED visits are infrequently linked to the original cause of admission and are believed to often be a complication or failure of the discharge plan. While some suggest that readmission within 30 days of an index admission is a marker for poor quality or coordination of patient care, evidence points to patient activation or patient engagement in self-care behaviors as another root cause of early hospital reutilization. Certainly, a proportion of the avoidable 30-day readmissions are likely related to modifiable patient factors such as health literacy and other factors related conceptually to patient activation.
Evidence shows that patient activation is a modifiable attribute and that effective interventions can increase patient activation and improve health outcomes and reduce health service costs. For example, one study by Hibbard et al. examined the impact of a health coaching intervention to enhance patient activation among a cohort of patients with diabetes; intervention subjects had increased patient activation and improved clinical parameters.11 Measuring a patient’s activation level before discharge may present an opportunity for healthcare providers to target discharge education and preparation to meet the individual’s needs in a more effective and cost-efficient approach. In the current study, we examine patient activation in relation to post-discharge hospital reutilization in order to determine whether a low patient activation score is associated with an increased rate of 30-day hospital utilization following discharge. This is a potentially important target, as low or early stage patient activation can be enhanced with tailored interventions, and may represent an opportunity to decrease avoidable 30-day post-discharge hospital utilization.
METHODS
The data used for the analysis of the relationship between patient activation and unplanned hospital utilization was gathered from Project RED-LIT I and RED-LIT II, entitled, “A Randomized Controlled Trial (RCT) to Reduce Cardiopulmonary Rehospitalization.” This was a two-armed intervention trial conducted from October 2008 to October 2010 on the medical in-patient service at Boston Medical Center, an urban safety net hospital in Boston, to improve patient education and safety in the transition between hospital and home with a primary goal of reducing 30-day hospital readmission. (NHLBI 1 R01 HL081307-01). This trial explored the effectiveness of an innovative patient-education and self-management technology system—the embodied conversational agent—compared to usual care on reducing early re-hospitalization for patients with chronic cardiopulmonary diseases and limited health literacy. Potential participants were excluded if they had been admitted from a skilled nursing facility or other hospital, admitted for a planned hospitalization, on hospital precautions, on suicide watch, or were deaf or blind. Of the 802 participants in the RED-LIT trials, complete data was available on 695 participants for this analysis.
Outcome Variables
The primary outcome variable for this study was the sum of all unplanned utilization events of hospital services within 30 days of the index discharge. This included hospital admission, observation stays (which were categorized as hospital readmission), and emergency department (ED) visits. We also analyzed hospital readmissions and ED visits separately as secondary outcome variables. Outcome data were collected from the Boston Medical Center electronic medical records or were self-reported during a follow-up telephone call to subjects 30 days after discharge. ED visits or readmissions to outside hospitals were identified by patient self-report only and were not independently confirmed. Utilization events to Boston Medical Center (BMC) as well as other hospitals and EDs were included.
Primary Independent Variable
Patient activation was assessed at baseline during the index hospitalization using an abbreviated eight-item version of the validated 13-item Patient Activation Measure (PAM) (see Table 1). Developed using Rasch psychometric methods analysis, PAM is an interval-level, unidimensional, Guttman-like measure.10,11 The PAM 13 has been validated in various healthcare settings such as hospital and ambulatory settings and for diverse patient populations such as occupational health, diabetes patients and multiple sclerosis patients.10,17–19 We derived the adapted PAM tool from these original validation data using estimated individual item discrimination parameters (unpublished data). The adapted tool was only administered at baseline during the index hospitalization. The PAM assesses an individual’s level of knowledge, confidence and skill to manage one’s health and healthcare. A set of responses is scored per protocol and categorized based on four possible activation levels. According to research using the PAM tool, patient activation is classified as: Level 1 (patients tend to be overwhelmed and unprepared to play an active role in their own health); Level 2 (patients lack knowledge and confidence for self-management); Level 3 (patients are beginning to take action, but lack confidence and skill to support some behavior changes); and Level 4 (patients have adopted many of the behaviors to support their health, but may not be able to maintain them in the face of life stressors).
Table 1.
Patient Activation Measure
| 1) | When all is said and done, I am the person who is responsible for taking care of my health |
| 2) | Taking an active role in my own health care is the most important thing that affects my health |
| 3) | I am confident that I can tell whether I need to go to the doctor or whether I can take care of a health problem on my own |
| 4) | I am confident that I can follow through on medical treatments I may need to do at home |
| 5) | I have been able to maintain (keep up with) lifestyle changes, like eating right or exercising |
| 6) | I know how to prevent problems with my health |
| 7) | I am confident I can figure out solutions when new problems arise with my health |
| 8) | I am confident that I can maintain lifestyle changes, like eating right and exercising, even during times of stress |
The PAM score was calculated based on participant responses to a scale of 0 (lowest activation) to 100 (highest activation), consistent with the procedure PAM 13. The continuous score was converted to the ordinal four-category variable, reflecting the four stages of activation. Stage 1 = PAM score of 47.0 or lower; Stage 2 = PAM score of 47.1 to 55.1; Stage 3 = PAM score of 55.2 to 67.0; Stage 4 = PAM score of 67.0 and above
Statistical Analysis
The demographic and background health characteristics of the participants were stratified by the four levels of PAM. Chi-square tests were used to identify potential confounders of the relationship between patient activation and 30-day hospital reutilization. Potential covariates for multivariable analyses included age in years, Charlson comorbidity index, gender (male versus female), insurance (Free Care, Medicaid, Medicare, or private insurance), income (unknown/refused to answer, no income–$19,999, $20,000–$39,999, $40,000 or more), marital status (single/single with partner, divorced/separated/widowed, or married), education (less than high school, high school diploma or equivalent, more than high school), race (Black, Hispanic, White or Other), employment (disabled/injured, retired, unemployed, or employed [part or full time]), homelessness in the 6 months prior to the index admission (yes versus no), having a primary care physician (yes versus no), symptoms of depression measured with the PHQ-9 (≥ 10 severe, 5–9 moderate, 1–4 mild), health literacy measured with the Rapid Assessment of Adult Literacy in Medicine (REALM, grade 6 and below, grade 7 to 8, grade 9 and above), frequent utilizer status (0–2 versus > 2 admissions in the 6 months prior to the index admission), and REDLIT treatment group (intervention versus control).
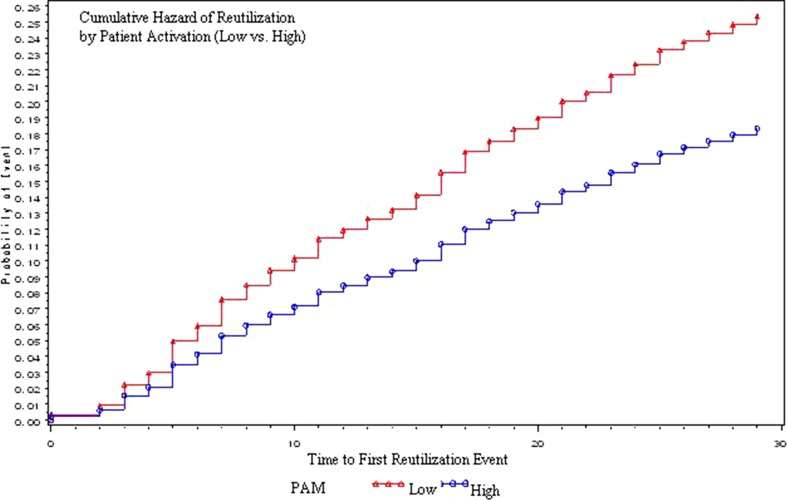
Multiple stepwise selection processes were utilized to construct the Poisson models for the primary and secondary outcomes. First, simple Poisson models were run only including the categorical PAM as the independent variable of interest and each one of the other predictors individually to see whether the associations with the outcomes were significant at α < 0.20, controlling for patient activation. This identified the potentially significant predictors. Poisson models were then constructed. From these models, manual forward stepwise selection processes were conducted to build the final Poisson models. Two-sided tests with p values < 0.05 were used to judge significance. The analyses were conducted in SAS 9.1.20 In addition, we evaluated a Kaplan–Meier hazard curve to capture the hazard of the first readmission to either the hospital or the ED within 30 days of discharge, stratified by activation level (Levels 1 and 2 [low] versus Levels 3 and 4 [high]).
RESULTS
Of the 695 participants, 67 (10 %) were at Level 1, 122 (18 %) were at Level 2, 193 (28 %) were at Level 3, and 312 (45 %) were at Level 4 (Table 2). Participants were on average 48 years of age, more than half reported black race, and the sample was evenly split between males and females. The majority (75 %) of the participants had Medicare, Medicaid, or Free Care, and 47 % of participants reported income below $40,000 annually. Of the 168 (24 %) with a post-discharge hospital service utilization within 30 days of the index admission, 123 (18 %) had one event and 45 (6 %) had at least two events. In bivariate analyses, we detected significant associations between patient activation and years of education (p value = 0.01), employment status (p value = 0.02), health literacy level (p value < 0.01) and depressive symptom level (p value < 0.01). Patients with low PAM scores (Levels 1 and 2) were more likely to have low health literacy, have completed fewer years of education, be disabled or retired, and have a higher level of depressive symptoms.
Table 2.
Baseline Characteristics
| Levels of PAM | Total (n = 695) |
p value | |||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||||
| Frequency (Column %) | (n = 67) | (n = 123) | (n = 193) | (n = 312) | |||
| Age in years: mean (SD) | 49.4 (12.7) | 49.0 (13.1) | 48.2 (14.8) | 48.6 (13.6) | 48.7 (14.0) | 0.93 | |
| Charlson comorbidity index: mean(SD) | 1.9 (1.9) | 1.9 (2.0) | 1.9 (2.4) | 1.7 (2.1) | 1.8 (2.2) | 0.87 | |
| Gender | Female | 32 (48) | 63 (52) | 96 (50) | 158 (51) | 349 (50) | 0.96 |
| Insurance | Free Care* | 13 (19) | 18 (15) | 29 (15) | 62 (20) | 122 (17) | 0.78 |
| Medicaid | 29 (43) | 57 (46) | 79 (40) | 125 (40) | 290 (42) | ||
| Medicare | 8 (12) | 13 (11) | 31 (16) | 38 (12) | 90 (13) | ||
| Private | 17 (25) | 35 (28) | 54 (28) | 87 (28) | 193 (28) | ||
| Income | No income – 19,999 | 23 (34) | 53 (43) | 72 (37) | 93 (30) | 241 (35) | 0.24 |
| 20,000–39,999 | 9 (13) | 12 (10) | 21 (11) | 43 (14) | 85 (12) | ||
| 40,000 and above | 6 (9) | 14 (11) | 31 (16) | 54 (17) | 105 (15) | ||
| Marital status | Single/Single with Partner | 37 (55) | 52 (42) | 99 (51) | 157 (50) | 345 (50) | 0.42 |
| Divorced/Separated/Widowed | 20 (30) | 38 (31) | 53 (27) | 80 (26) | 191 (27) | ||
| Married | 10 (15) | 31 (25) | 37 (19) | 73 (23) | 151 (22) | ||
| Education | Less than High School | 18 (27) | 32 (26) | 36 (19) | 61 (20) | 147 (21) | 0.01 |
| High School or Equivalent | 34 (51) | 43 (35) | 89 (46) | 113 (36) | 279 (40) | ||
| More than High School | 15 (22) | 48 (39) | 68 (35) | 138 (44) | 269 (39) | ||
| Race | Non-Hispanic Black | 33 (49) | 66 (54) | 99 (51) | 166 (53) | 364 (52) | 0.85 |
| Hispanic | 6 (9) | 16 (13) | 28 (15) | 31 (10) | 81 (12) | ||
| Other | 4 (6) | 5 (4) | 12 (6) | 22 (7) | 44 (6) | ||
| Non-Hispanic White | 24 (36) | 35 (28) | 54 (28) | 93 (30) | 206 (30) | ||
| Employment status | Disabled/Injured | 26 (39) | 37 (31) | 52 (28) | 74 (24) | 189 (28) | 0.02 |
| Retired | 12 (18) | 12 (10) | 23 (12) | 43 (14) | 90 (13) | ||
| Unemployed | 17 (26) | 36 (30) | 54 (29) | 70 (23) | 177 (26) | ||
| Employed (Part or Full Time) | 11 (17) | 35 (29) | 58 (31) | 122 (39) | 226 (33) | ||
| Been homeless | Yes | 14 (21) | 17 (14) | 30 (16) | 33 (11) | 94 (14) | 0.11 |
| Has PCP | Yes | 56 (84) | 104 (85) | 157 (81) | 258 (83) | 575 (83) | 0.90 |
| Depressive symptoms† | Severe | 18 (27) | 28 (23) | 27 (14) | 26 (8) | 99 (14) | < 0.01 |
| Moderate | 6 (9) | 14 (12) | 12 (6) | 16 (5) | 48 (7) | ||
| Mild | 43 (64) | 79 (65) | 151 (79) | 269 (87) | 542 (78) | ||
| REALM category | Grade 6 and below (0–44) | 10 (16) | 19 (17) | 36 (19) | 28 (9) | 93 (14) | < 0.01 |
| Grade 7 to 8 (45–60) | 14 (23) | 40 (35) | 46 (25) | 75 (25) | 175 (26) | ||
| Grade 9 and above (61–66) | 37 (61) | 56 (49) | 103 (56) | 201 (66) | 397 (60) | ||
| Frequent utilizer‡ | No | 32 (48) | 54 (44) | 74 (38) | 117 (42) | 277 (40) | 0.32 |
| REDLIT treatment group | Intervention | 31 (46) | 55 (45) | 99 (52) | 157 (50) | 342 (49) | 0.61 |
Not all column % add up to 100 % due to missing data
PCP primary care provider; REALM rapid estimate for adult literacy in medicine
*Free Care is a Massachusetts state program for uninsured patients
†Determined by using the Patient Health Questionnaire-9, a nine-item, four-point Likert scale, standard scoring algorithm to screen for major and minor depression
‡Frequent utilizer defined as an individual with two or more hospital visits within 6 months prior to the index admission
Unadjusted Poisson regression analyses showed a dose effect of PAM score on 30-day hospital reutilization risk. Specifically, we found that compared to participants with the highest PAM scores, participants with the lowest PAM scores (Level 1) have 2.27 times the risk of reutilization within 30 days (95 % CI 1.56 to 3.30, p value < 0.001), those at Level 2 have 1.78 times the reutilization risk (95 % CI 1.28 to 2.49, p value < 0.001), and those at Level 3 have 1.42 times the reutilization risk (95 % CI 1.04 to 1.95, p value = 0.03). The adjusted Poisson regression analyses are shown in Table 3. After controlling for potential confounders, the association between PAM and 30-day hospital reutilization remained significant. Compared to patients with the highest level of activation (Level 4), those with PAM Level 1 have 1.75 times the rate of reutilization within 30 days (95 % CI 1.18 to 2.60, p < 0.001), those at Level 2 have a 1.50 times higher rate (95 % CI 1.06 to 2.13, p < 0.001), and those at Level 3 have a 1.30 times higher rate of reutilization (95 % CI 0.94 to 2.13, p = 0.03). The associations between PAM and the secondary outcomes (30-day rehospitalization, and 30-day return to the ED) were also statistically significant (Table 4). In addition, the Kaplan–Meyer hazard curve (Fig. 1) exhibits a higher hazard for reutilization for participants with lower levels of activation (Level 1 and 2) versus higher levels of activation (Level 3 and 4), p value < 0.05.
Table 3.
Multivariable Poisson Regression Model for the Primary Outcome
| 30-day reutilization* | Categories | IRR (95 % CI) |
|---|---|---|
| PAM | Level 1 | 1.75 (1.18 to 2.60) |
| Level 2 | 1.50 (1.06 to 2.13) | |
| Level 3 | 1.30 (0.94 to 1.80) | |
| Level 4 | Ref | |
| Employment | Disabled/Injured | 1.27 (0.87 to 1.85) |
| Retired | 1.05 (0.59 to 1.88) | |
| Unemployed | 0.92 (0.63 to 1.34) | |
| Employed (Part to Full Time) | Ref | |
| Depressive symptoms† | Moderate to Severe | 1.53 (1.00 to 2.33) |
| Mild Depression | 1.54 (1.11 to 2.13) | |
| No Depression | Ref | |
| Gender | Female | 0.82 (0.63 to 1.05) |
| Male | Ref | |
| Race | Black | 0.82 (0.61 to 1.09) |
| Hispanic | 1.04 (0.68 to 1.60) | |
| Other | 0.86 (0.48 to 1.52) | |
| White | Ref | |
| Frequent utilizer‡ | Yes | 1.94 (1.49 to 2.53) |
| No | Ref |
IRR incidence rate ratio
Adjusted for age, Charlson comorbidity index, insurance, and education
*Defined as the sum of emergency department visits plus rehospitalizations. An emergency department visit that leads to a rehospitalization is counted only as a rehospitalization
†Determined by using the Patient Health Questionnaire-9, a nine-item, four-point Likert scale, standard scoring algorithm to screen for major and minor depression
‡Frequent utilizer defined as an individual with two or more hospital visits within 6 months prior to the index admission
Table 4.
Multivariable Poisson Regression Models for Secondary Outcomes
| 30-day rehospitalization | 30-day return to the ED† | ||
|---|---|---|---|
| Categories | IRR (95 % CI)* | IRR (95 % CI) | |
| PAM | Level 1 | 1.93 (1.22 to 3.06) | 1.68 (1.07 to 2.63) |
| Level 2 | 1.70 (1.14 to 2.55) | 1.33 (0.89 to 1.98) | |
| Level 3 | 1.50 (1.03 to 2.19) | 1.19 (0.82 to 1.74) | |
| Level 4 | Ref | Ref | |
| Employment | Disabled/Injured | 1.81 (1.16 to 2.82) | 1.11 (0.72 to 1.71) |
| Retired | 1.11 (0.59 to 2.08) | 1.01 (0.48 to 2.11) | |
| Unemployed | 0.92 (0.56 to 1.51) | 0.93 (0.62 to 1.39) | |
| Employed (Part to Full Time) | Ref | Ref | |
| Depressive symptoms | Moderate to Severe | 2.08 (1.32 to 3.28) | |
| Mild Depression | 1.89 (1.31 to 2.71) | ||
| No Depression | Ref | ||
| Gender | Female | 0.88 (0.65 to 1.18) | 0.75 (0.56 to 1.00) |
| Male | Ref | Ref | |
| Race | Black | 0.58 (0.42 to 0.81) | 0.99 (0.70 to 1.39) |
| Hispanic | 0.75 (0.45 to 1.26) | 1.27 (0.78 to 2.06) | |
| Other | 0.56 (0.28 to 1.13) | 1.06 (0.56 to 2.02) | |
| White | Ref | Ref | |
| Frequent utilizer | Yes | 2.32 (1.7 to 3.17) | 1.71 (1.26 to 2.32) |
| No | Ref | Ref |
Rehospitalization model adjusted for RED-LIT intervention group, age, Charlson comorbidity index, and insurance
*Deviance scaled
†Return to ED model adjusted for age, Charlson comorbidity index, insurance, and education
Figure 1.
Cumulative hazard curve.
DISCUSSION
Our results suggest that patients with low activation have nearly twice the risk of 30-day post-discharge hospital service utilization compared with patients with higher activation. This is an important finding suggesting a new strategy for identifying patients at risk for unplanned return to hospital following discharge and an opportunity for intervention.
Screening for risk factors associated with poor health outcomes is only warranted when a positive screen is actionable and when taking action holds the promise of improving the patient’s course. Patient activation clearly meets these criteria. It is a modifiable risk factor for readmission and may be more modifiable than other risk factors for reutilization, such as male gender, homelessness, or depression. Low patient activation has been shown to be amenable to intervention in some contexts.21 Potentially screening for patient activation could not only identify patients at risk for readmission, but more importantly, help discharge planners develop tailored and cost-effective tiered intervention plans based on the individual’s activation level, to prepare patients for a safe and effective discharge that reduces the risk for readmission or ED visits.
Hospitals in 25 states are now using the Patient Activation Measure to tailor the type and amount of support they provide to patients during their hospitalization and in the post-discharge period. A key way that hospitals and transition care teams are using the PAM is to segment patient populations based both on disease burden and ability to self-manage (PAM score). This strategy allows hospitals to spend more time with patients who have low levels of activation during their hospital stay, helping them prepare for the post-hospital period and then providing them with more support after they leave the hospital. Thus, the hospitals can be more targeted in the way they use their resources, giving more time and attention to patients who need it and less intensive support to those who have more self-management skills.
There are several limitations to our study. First, study subjects were recruited from an urban safety net hospital, so our results may be less generalizable to non-urban, non-safety net hospitals. Second, reutilization events outside of BMC were collected through medical record review and subject self-report. Not all events could be independently confirmed; however, 91 % of events were confirmed by review of the BMC electronic medical record. Third, examination of the role of income in the relationships examined in this paper was limited by the narrow distribution of income in our cohort and by the fact that this analysis was conducted in Massachusetts. The existence of near universal insurance in Massachusetts during the period of data collection may limit the generalizability of our results. However, with the upcoming implementation of the Affordable Care Act, the levels of access to health care services currently available in Massachusetts may become more similar nationally. Future research on the role of income on the relationship between patient activation and health services utilization is warranted in our changing health care landscape. Nonetheless, our finding that low patient activation is associated with higher readmission and ED visits suggests that simply having greater access to health services is not sufficient to reduce avoidable readmissions. Indeed, available resources need to be tailored to the patient’s individual needs and activation level in order to be effectively deployed.
Lastly, our adapted patient activation measure, PAM-8, has not been fully tested for reliability and validity. Still our findings indicate strong predictive power for identifying patients at risk of early readmission or ED use, and warrant further investigation of the role of patient activation in the care transitions setting. Finally, this is a secondary analysis of an existing data set. Therefore, some unaccounted, residual confounding is possible in our results. For example, we were unable to account fully for the potential influence of caregiver involvement or social support. Future research including PAM data collection among caregivers is warranted. However, we have included a number of patient-level variables in our analysis, allowing us to control for many potentially important confounders.
CONCLUSION
Patients with a low level of activation are at risk for early unplanned hospital utilization. As hospitals move into an era where they will face financial penalties for higher readmission rates, understanding the factors that lead to unnecessary readmissions is a priority. Using the measurement of patient activation as a predictor of hospital reutilization can provide hospitals with a way to effectively target their efforts in preventing readmissions. Randomized trials are needed to demonstrate that interventions targeting patient activation are effective in reducing avoidable readmissions.
Acknowledgements
Dr. Mitchell is supported by a mentored clinical scientist award from the Agency for Healthcare Research and Quality (1K08HS019771-01). The REDLIT trial was funded by the National Heart Lung and Blood Institute (NHLBI 1 R01 HL081307-01).
Conflict of Interest
No authors have any conflict of interest to report. Dr. Mitchell is a non-product speaker on health behavior counseling for MERCK & Co.
REFERENCES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Steiner C, Barrett M, Hunter K. Hospital Readmissions and Multiple Emergency Department Visits, in Selected States, 2006–2007: Statistical Brief #90. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet] Rockville: Agency for Health Care Policy and Research (US); 2010. [PubMed] [Google Scholar]
- 3.Rising KL, White LF, Fernandez WG, Boutwell AE. Emergency department visits after hospital discharge: a missing part of the equation. Ann Emerg Med. 2013. [DOI] [PubMed]
- 4.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell SE, Paasche-Orlow MK, Forsythe SR, Chetty VK, O’Donnell JK, Greenwald JL, et al. Post-discharge hospital utilization among adult medical inpatients with depressive symptoms. J Hosp Med. 2010;5(7):378–384. doi: 10.1002/jhm.673. [DOI] [PubMed] [Google Scholar]
- 6.Mitchell SE, Sadikova E, Jack BW, Paasche-Orlow MK. Health literacy and 30-day post-discharge hospital utilization. J Health Commun. 2012;17(Suppl 3):325–338. doi: 10.1080/10810730.2012.715233. [DOI] [PubMed] [Google Scholar]
- 7.Marcantonio ER, McKean S, Goldfinger M, Kleefield S, Yurkofsky M, Brennan TA. Factors associated with unplanned hospital readmission among patients 65 years of age and older in a Medicare managed care plan. Am J Med. 1999;107(1):13–17. doi: 10.1016/S0002-9343(99)00159-X. [DOI] [PubMed] [Google Scholar]
- 8.Woz S, Mitchell S, Hesko C, Paasche-Orlow M, Greenwald J, Chetty VK, et al. Gender as risk factor for 30 days post-discharge hospital utilisation: a secondary data analysis. BMJ Open. 2012;2(2):e000428. doi: 10.1136/bmjopen-2011-000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei NJ, Wexler D, Nathan DM, Grant RW. Intensification of diabetes medication and risk for 30-day readmission. Diabet Med. 2012. [DOI] [PMC free article] [PubMed]
- 10.Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res. 2004;39(4 Pt 1):1005–1026. doi: 10.1111/j.1475-6773.2004.00269.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hibbard JH, Tusler M. Assessing activation stage and employing a “next steps” approach to supporting patient self-management. J Ambul Care Manage. 2007;30(1):2–8. doi: 10.1097/00004479-200701000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Parchman ML, Zeber JE, Palmer RF. Participatory decision making, patient activation, medication adherence, and intermediate clinical outcomes in type 2 diabetes: a STARNet study. Ann Fam Med. 2010;8(5):410–417. doi: 10.1370/afm.1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Begum N, Donald M, Ozolins IZ, Dower J. Hospital admissions, emergency department utilization and patient activation for self-management among people with diabetes. Diabetes Res Clin Pract. 2011;93(2):260–267. doi: 10.1016/j.diabres.2011.05.031. [DOI] [PubMed] [Google Scholar]
- 14.Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27(5):520–526. doi: 10.1007/s11606-011-1931-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Remmers C, Hibbard J, Mosen DM, Wagenfield M, Hoye RE, Jones C. Is patient activation associated with future health outcomes and healthcare utilization among patients with diabetes? J Ambul Care Manage. 2009;32(4):320–327. doi: 10.1097/JAC.0b013e3181ba6e77. [DOI] [PubMed] [Google Scholar]
- 16.Kirby SE. An Exploration of the Reasons for Frequent Readmission in Patients with Chronic Disease: Activation from Frequent Flyers to Self-Management. University of New South Whales; 2012.
- 17.Stepleman L, Rutter MC, Hibbard J, Johns L, Wright D, Hughes M. Validation of the patient activation measure in a multiple sclerosis clinic sample and implications for care. Disabil Rehabil. 2010;32(19):1558–1567. doi: 10.3109/09638280903567885. [DOI] [PubMed] [Google Scholar]
- 18.Fowles JB, Terry P, Xi M, Hibbard J, Bloom CT, Harvey L. Measuring self-management of patients’ and employees’ health: further validation of the Patient Activation Measure (PAM) based on its relation to employee characteristics. Patient Educ Couns. 2009;77(1):116–122. doi: 10.1016/j.pec.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Med Care. 2005;43(5):436–444. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 20.SAS Institute I. SAS 9.1.3 Help and Documentation. 2000–2004.
- 21.Deen D, Lu WH, Rothstein D, Santana L, Gold MR. Asking questions: the effect of a brief intervention in community health centers on patient activation. Patient Educ Couns. 2011;84(2):257–260. doi: 10.1016/j.pec.2010.07.026. [DOI] [PubMed] [Google Scholar]