A 36-year-old man with a history of substance abuse was admitted for two days of fever, cough, and confusion. Aside from dental caries, which had worsened due to methamphetamine use, he had no medical history. On examination, he was febrile to 101.0 °F and stuporous with horizontal nystagmus. Laboratory data revealed a leukocytosis of 29,500 cells/mm3 and a negative HIV screen.
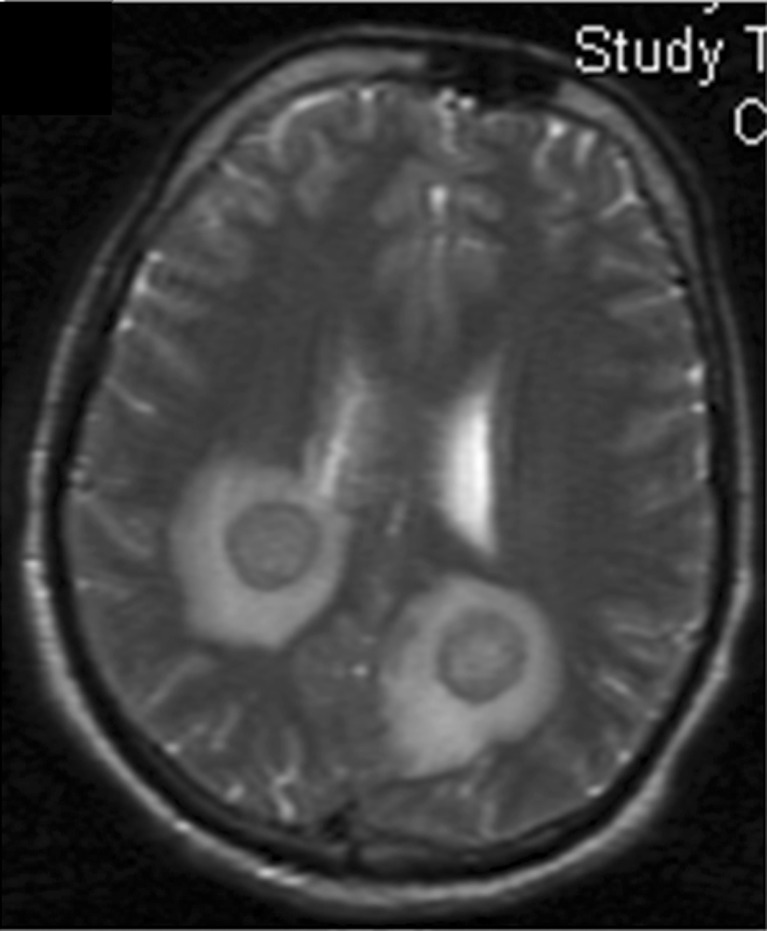
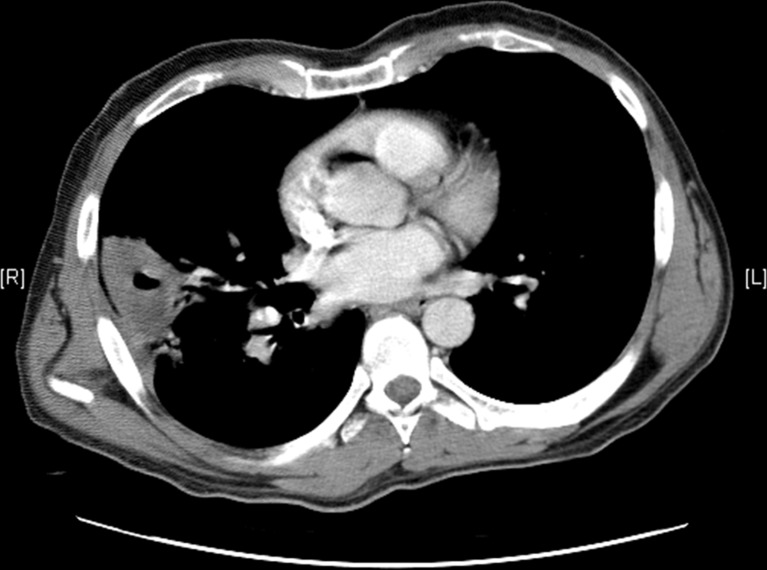
Gadolinium-contrasted magnetic resonance imaging (MRI) of the brain showed two ring-enhancing lesions in the parieto-occipital cortex (Fig. 1), and computed tomography (CT) scan of the chest revealed a cavitary, right lower lobe lung mass (Fig. 2). A CT-guided core biopsy of the lung mass demonstrated inflammatory debris histologically, with culture yielding Streptococcus intermedius.
Figure 1.
T2-weighted, gadolinium-contrasted MRI of the brain revealing two 2.0 cm ring-enhancing lesions in the parieto-occipital cortex bilaterally with associated vasogenic edema.
Figure 2.
CT of the chest indicating a 5.5 cm, cavitary right lower lobe lung mass.
Oral anaerobes and microaerophilic streptococci are common isolates of concomitant brain-lung abscesses where poor dentition and aspiration underlie pathogenesis.1 Such infections begin with pneumonia, followed by hematogenous seeding of the cerebral cortex, leading to multiple abscesses in a middle cerebral artery distribution. In contrast, solitary brain abscesses of the frontal lobe develop as a result of sinusitis or odontogenic infection.2 Successful treatment of brain abscesses usually requires surgical drainage and antimicrobial chemotherapy.3 The patient underwent stereotactic drainage of both brain abscesses and a course of intravenous antibiotic therapy.
Acknowledgements
The authors would like to thank Adam Solesby for his assistance with the digital imagery in the case. The authors have not received any funding or benefits from industry or elsewhere to support this work.
Conflict of Interest
The authors report no conflicts of interest.
REFERENCES
- 1.Khatib R, Ramanathan J, Baran J., Jr Streptococcus intermedius: A cause of lobar pneumonia with meningitis and brain abscesses. Clin Infect Dis. 2000;30(2):396–397. doi: 10.1086/313672. [DOI] [PubMed] [Google Scholar]
- 2.Mathisen GE, Johnson JP. Brain abscess. Clin Infect Dis. 1997;25(4):763–779. doi: 10.1086/515541. [DOI] [PubMed] [Google Scholar]
- 3.Mandell GL, Douglas RG, Bennett JE, Dolin R. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 7. New York: Elsevier/Churchill Livingstone; 2010. [Google Scholar]