Abstract
The association of metastatic breast cancer presenting as thrombocytopenia and anaemia is demonstrated in the following case of a 79-year-old woman. Her main symptoms were abdominal pain, altered bowel habit and weight loss. Without a clear causative pathology, she underwent a CT scan which demonstrated multiple sclerotic bone lesions. With a raised CA15-3 and strong oestrogen receptor positivity on immunohistochemistry on a trephine bone marrow biopsy, a diagnosis of metastatic lobular breast cancer was made. Interestingly, only a small breast mass was noted on mammography. The patient was managed conservatively and initiated on supportive therapy. This case report summarises the varying presentation of bone marrow suppression secondary to metastatic infiltration, especially in the absence of classical symptoms associated with primary solid tumour. Accurate bone marrow analysis is also vital in establishing the final diagnosis.
Background
The presence of isolated anaemia and thrombocytopenia with an asymptomatic breast lump is an interesting and unusual presentation of metastatic breast cancer. Indeed, the case was on the background of a likely neoplastic lesion and raised tumour markers.
Case presentation
A 79-year-old woman was admitted to the acute surgical team with a 2-week history of central abdominal pain and loose bowel motions. These symptoms were associated with a 3-month duration of anorexia, decreased appetite and general malaise resulting in an approximate weight loss of 20–64 kg. Mobility was significantly reduced due to widespread back pain. Her medical history included ischaemic heart disease, chronic kidney disease, gastro-oesophageal reflux disease and a previous appendicectomy. Her regular prescribed medications were amlodipine, aspirin, bisoprolol, furosemide, lisinopril, nicorandil, omeprazole and simvastatin. There was no alteration in medication including dosages for over 12 months. She was a life-long non-smoker and consumed alcohol in moderation. Examination was unremarkable apart from a discrete left 1 cm axillary mass that was non-tender and non-mobile under the skin.
Investigations
On admission, initial investigations revealed a significant normocytic anaemia and thrombocytopenia (haemoglobin 71 g/L, mean cell volume 86.7 fL, white cell count 6.2×109/L, neutrophils 2.4×109/L, lymphocytes 3.1×109/L, monocytes 0.5×109/L, eosinophils 0.1×109/L, basophils 0.1×109/L, nucleated red blood cells (NRBCs) 0.63×109/L, mean corpuscular haemoglobin 29.1 pg and platelet 32×109/L).
A peripheral blood film showed a leucoerythroblastic picture with red cell anisocytosis, tear drop poikilocytes, NRBCs and left shifted neutrophils. There was no hypochromia or macrocytosis to suggest a nutritional deficiency.
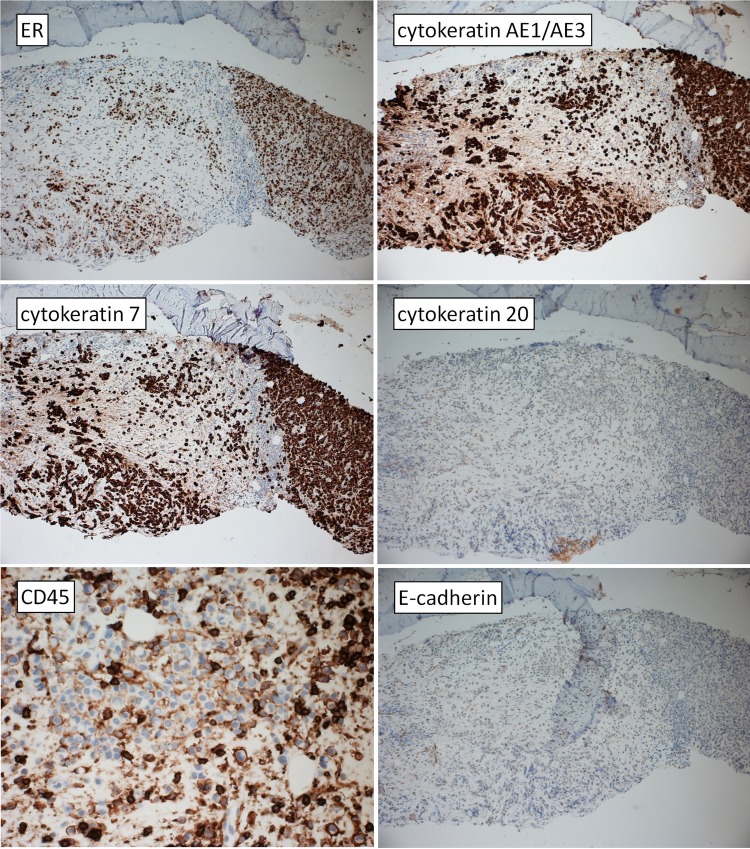
The coagulation screen (prothrombin time 10.7 s and activated partial thromboplastin time 26.8 s), direct Coombs’ test (negative), inflammatory markers (C reactive protein 7.5 mg/L) and liver function tests (albumin 36 g/L, bilirubin 20 μmol/L, alkaline phosphatase 120 U/L and alanine transaminase 34 U/L) were normal. However, tumour markers (carcinoembryonic antigen 1087 μg/L CA-199 179 U/mL and CA-153 4234 U/mL) were grossly abnormal. With the concern of an underlying malignant pathology, a CT scan of the thorax, abdomen and pelvis was performed revealing multiple sclerotic foci (figure 1) in the thoracic, lumbar spine and pelvis. In addition, there was left axillary lymphadenopathy extending from the axillary tail of the breast into the axilla (figure 2). In light of the deranged haematological parameters, a bone marrow examination was undertaken. Attempts to obtain a bone marrow aspirate were unsuccessful leading to a dry tap. A trephine biopsy was obtained, showing areas of widespread fibrosis (WHO grade 3) and osteosclerosis (figure 3) and infiltration of non-haematological cells. Such cells exhibited a signet ring appearance, pale cytoplasm and cytoplasmic inclusions (figure 4). Immunohistochemistry studies (figure 5) showed positive epithelial markers in particular pan cytokeratin AE1/AE3 with differential expression of cytokeratin 7 rather than cytokeratin 20. Epithelial membrane antigen was also positive. Oestrogen receptor was strongly positive, but negative for thyroid transcription factor-1 (TTF-1), CD45 and E-cadherin. Malignant infiltration of the bone marrow was hence identified with a phenotype consistent with metastatic lobular carcinoma of the breast.
Figure 1.
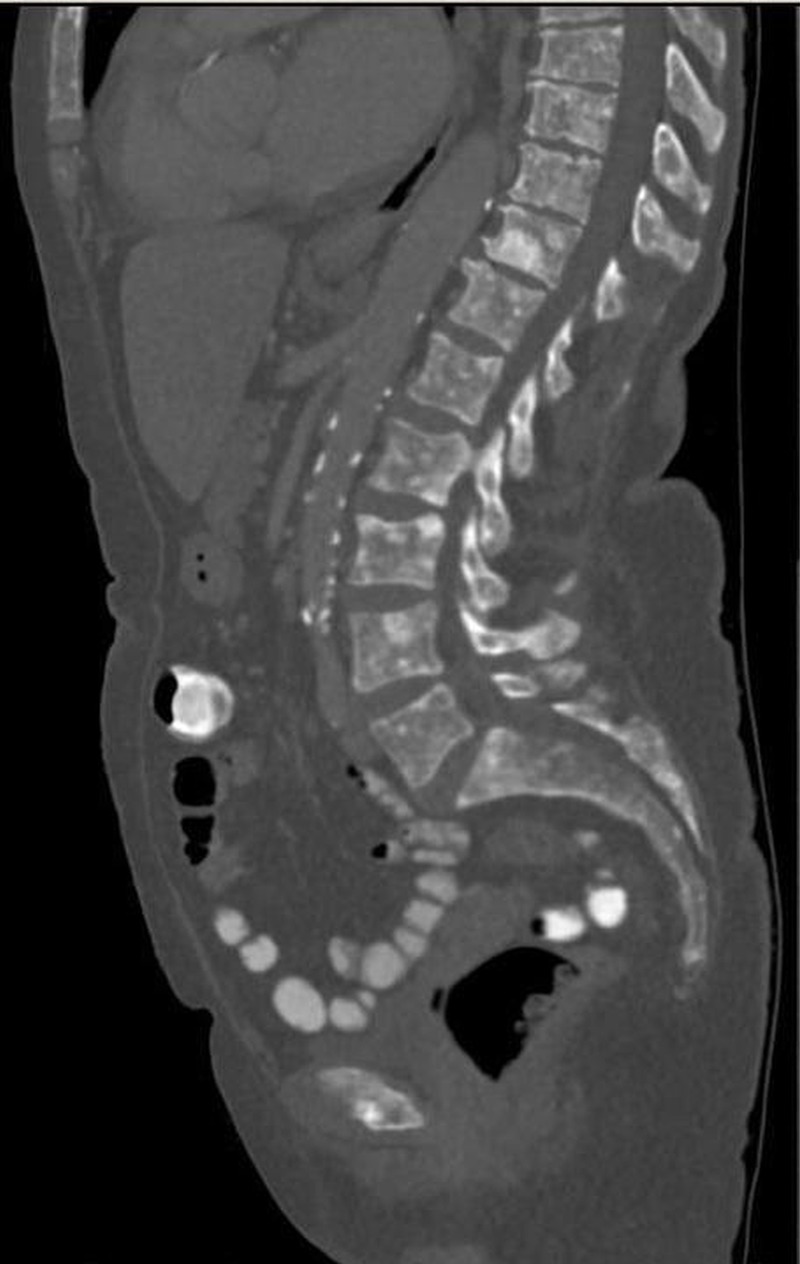
CT scan (sagittal plane) showing diffuse sclerotic lesions within the skeleton.
Figure 2.

CT scan (transverse plane) with axillary lymphadenopathy.
Figure 3.
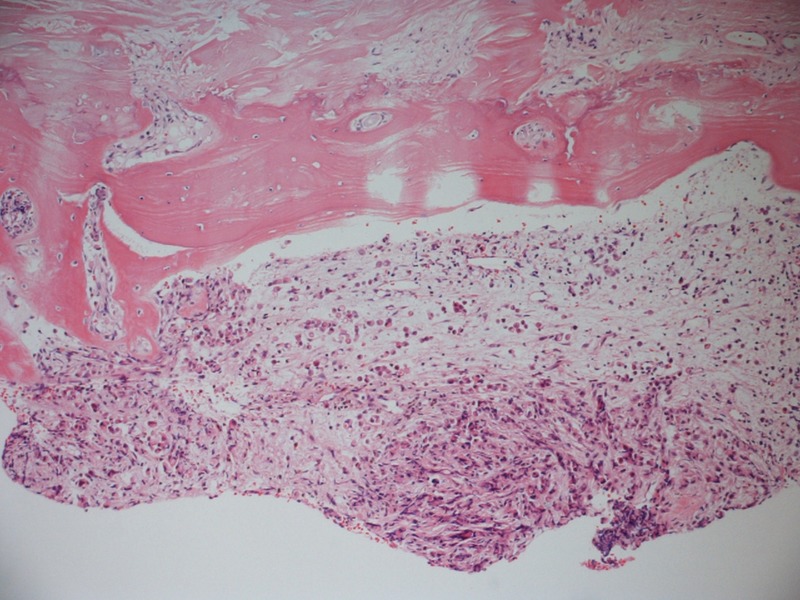
Trephine bone marrow histology with fibrosis and osteosclerosis with infiltration of non-haematological cells (H&E ×100).
Figure 4.
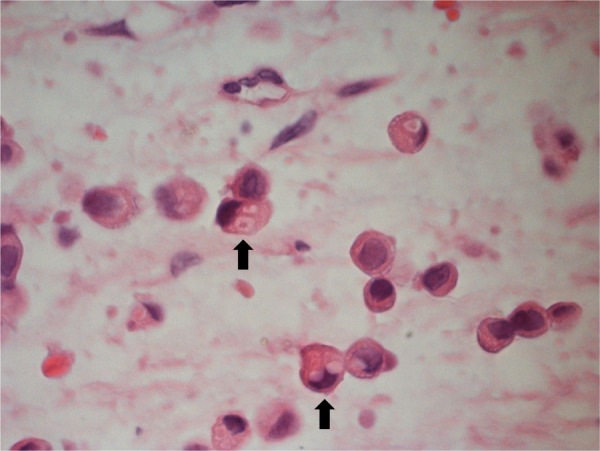
Non-haematological infiltration in trephine bone marrow displaying a signet ring appearance, pale cytoplasm and cytoplasmic inclusions (H&E ×1000).
Figure 5.
Immunohistochemistry of trephine bone marrow: ER+/cytokeratin AE1/AE3+/cytokeratin 7+/cytokeratin 20−/CD45−/E-cadherin. ER, oestrogen receptor.
A mammogram (figure 6) confirmed an irregular asymmetric left breast mass measuring 3 cm in all fields. Lipogenic reaction was also noted.
Figure 6.
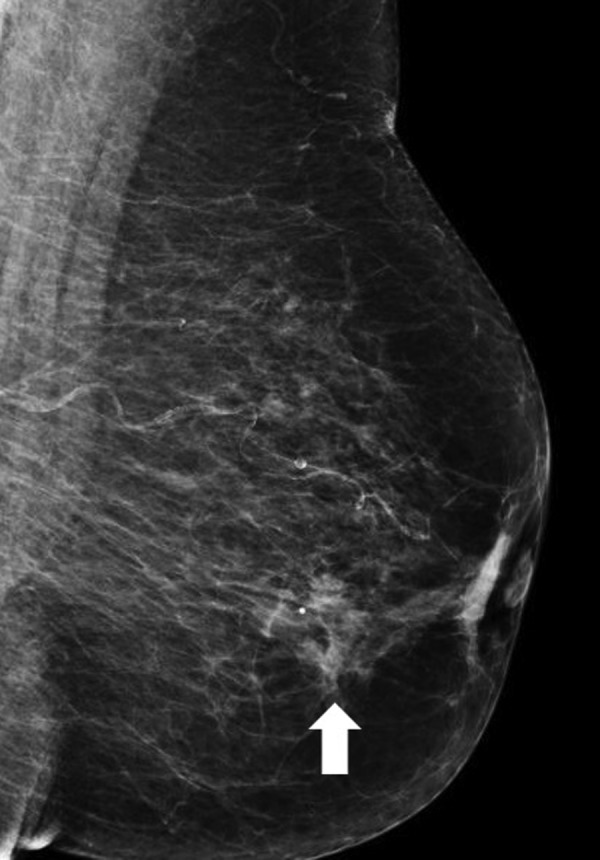
A small irregular mass in mammogram of the left breast.
Differential diagnosis
In any case of thrombocytopenia, the microangiopathic haemolytic anaemias should be sought to avoid delay in their prompt management. The blood morphology and baseline blood tests as well as the clinical picture were not consistent with this group of conditions, hence other causes were considered. Leucoerythroblastosis can indicate bone marrow infiltration or severe induced bone marrow stress, for example by overwhelming sepsis or inflammation. In this case, the absence of clinical signs of the former suggests that bone marrow infiltration to be the cause, which was later confirmed on trephine biopsy. Drug-induced thrombocytopenia was unlikely as no alterations in the patient's medications were noted.
Treatment
Increasing red cell transfusion dependency was noted throughout her hospital stay with no significant bleeding events. In light of the widespread nature of the disease and poor performance status, a palliative approach was taken with instigation of letrozole (2.5 mg/day) initially and subsequently denosumab (120 mg/m2/day), a monoclonal antibody utilised in the treatment of osteoporosis by its action to inhibit receptor activator of nuclear factor κ B ligand. This was complemented with calcium and vitamin D supplementation.
An axillary/breast biopsy or fine-needle aspiration cytology was not undertaken as it was deemed unsafe in the presence of refractory thrombocytopenia and not alter management.
Outcome and follow-up
The patient was reviewed by the community palliative care team 3 weeks postdischarge with good effect of the prescribed therapy. At 4 months after her initial diagnosis, she continued with denosumab therapy requiring red cell and platelet transfusion on a monthly basis.
Discussion
Invasive lobular carcinoma (ILC) represents 5–15% of breast cancers.1 2 The association of metastatic cancer with bone marrow infiltration and pancytopenia is well established with an approximate incidence of 80%.3 ILC has been reported to metastasise more commonly to meninges, bone marrow, peritoneum and liver.4 5 This case correlates with autopsy studies where substantial metastatic spread had remained clinically undetected,4 5 especially involvement of the peritoneum and abdominal organs in patients with ILC. Bone marrow micrometastases are associated with later distant metastases but not with locoregional recurrence.3 There are no published data on the incidence of bone marrow infiltration in ILC.
Interestingly, the peripheral blood findings are usually unremarkable in patients with metastatic marrow infiltration where anaemia and leucocytosis are often present. However, leucoerythroblastic reactions, noted in patients with carcinomas of the breast, lung or prostate, should prompt further investigation if deemed appropriate.
Malignancy must be appreciated in the presence of low haematological markers in elderly patients. Guided by the peripheral blood smear, this case highlights that bone marrow examination with appropriate and accurate immunohistochemical techniques is invaluable in establishing the diagnosis of patients presenting with cytopenias. Thus, physicians should be aware of the importance of a structured approach that includes correlation with an accurate clinical history and examination, relevant radiological investigations and peripheral blood and bone marrow histology.
Learning points.
Causes of peripheral blood cytopenias in the elderly are varied, but morphological clues like leucoerythroblastosis can help narrow down differential diagnoses.
Immunohistochemistry can corroborate the histological diagnosis, indicate the likely primary site and aid definitive targeted therapy.
Occult metastatic spread in invasive lobular carcinoma is well established.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Sastre-Garau X, Jouve M, Asselain B, et al. Infiltrating lobular carcinoma of the breast. Clinicopathological analysis of 975 cases with reference to data on conservative therapy and metastatic patterns. Cancer 1996;77:113. [DOI] [PubMed] [Google Scholar]
- 2.Rakha EA, El-Sayed ME, Menon S, et al. Histologic grading is an independent prognostic factor in invasive lobular carcinoma of the breast. Breast Cancer Res Treat 2008;111:121. [DOI] [PubMed] [Google Scholar]
- 3.Cummings MC. Occult metastases in breast cancer. In: Cancer forum. Cancer Council Australia, 2003:95–6 [Google Scholar]
- 4.Harris M, Howell A, Chrissohou M, et al. A comparison of the metastatic pattern of infiltrating lobular carcinoma and infiltrating duct carcinoma of the breast. Br J Cancer 1984;50:23–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixon AR, Ellis IO, Elston CW, et al. A comparison of the clinical patterns of invasive lobular and ductal carcinomas of the breast. Br J Cancer 1991;63:634–5 [DOI] [PMC free article] [PubMed] [Google Scholar]