Abstract
Alpha-adrenoceptor antagonists (alpha-blockers) are widely prescribed to treat lower urinary tract symptoms (LUTS) in men but fail to ameliorate LUTS sufficiently, especially the storage symptoms related to frequency, urgency and nocturia. We performed a meta-analysis of randomised controlled trials (RCTs) comparing an alpha-blocker plus muscarinic antagonist with an alpha-blocker alone in male LUTS patients who were treated with alpha-blocker prior to randomisation. The review contained six randomised controlled trials (RCTs) that included a total of 2,208 male patients who were randomised to receive alpha-blocker plus muscarinic antagonist or alpha-blocker alone. The add-on group experienced significantly greater improvement in both total IPSS (International Prostate Symptom Score) and storage IPSS. Adverse events (AEs) were commonly experienced by both groups (41.6 vs. 33.3%) though they were not severe. Our meta-analysis indicated that muscarinic antagonists as add-on therapy alleviate LUTS, especially storage symptoms. The add-on therapy demonstrated safety and tolerability comparable with alpha-blocker monotherapy in male with LUTS.
Lower urinary tract symptoms (LUTS) are a major health problem and are prevalent in men aged >45 years1,2,3. The constellation of LUTS in men comprises storage symptoms, including overactive bladder (OAB), voiding symptoms and post-micturition symptoms4. Traditionally, LUTS in men were attributed to benign prostatic hyperplasia (BPH) and were considered synonymous with BPH. It is estimated that approximatively 917 million men worldwide suffered from BPH/LUTS in 20085, and these symptoms significantly affect the daily lives of sufferers.
Alpha-blockers targeting the prostate are widely prescribed to treat LUTS associated with BPH. However, because storage symptoms and voiding symptoms coexist frequently, the treatment of LUTS is still complicated in men1. And it is not fully understood whether storage symptoms may develop secondarily to benign prostatic obstruction (BPO) in male patients6. Moreover, in some alpha-blocker-treated LUTS patients, some storage symptoms, such as frequency and urgency, may persist6,7. Thus, medication targeting the prostate alone is not sufficient for treating LUTS, and drugs targeting the bladder, rather than the prostate, could be added to the management of LUTS, given that the bladder is another contributor to LUTS patients in men8,9. Muscarinic antagonists, the first-line pharmacotherapy for OAB symptoms, are proved efficient in alleviating storage symptoms in male LUTS. However, the use of muscarinic antagonists in these patients has been limited by physicians considering the theoretical threat of increasing post-void residual (PVR) or acute urinary retention (AUR). This systematic review focuses on the efficacy and safety of muscarinic antagonist as an add-on therapy for men with LUTS who still suffer storage symptoms after treatment with alpha-blocker.
Results
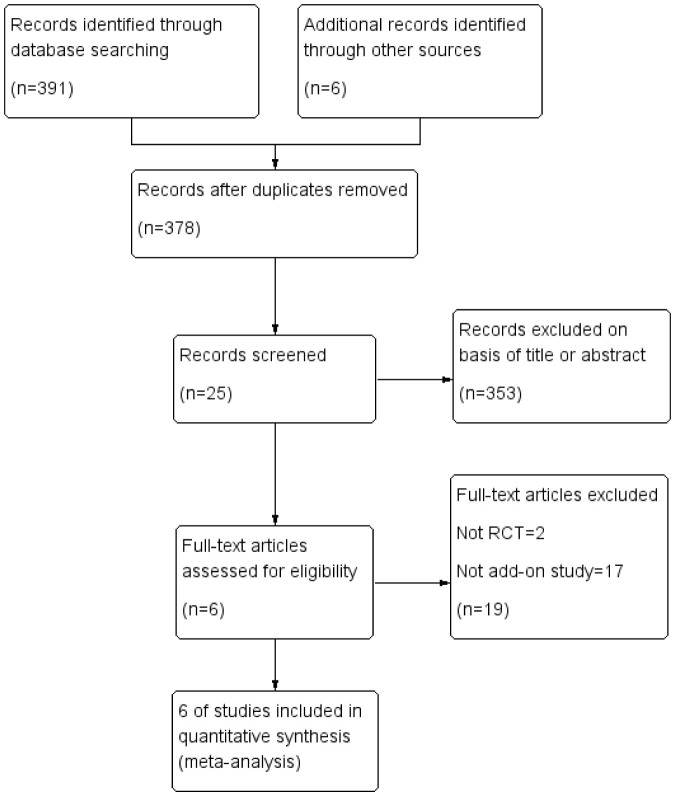
The search strategy initially yielded 391 studies, and six additional studies were identified through other sources; 378 records remained after duplicate deletion (Figure 1). Of these, 353 papers were excluded on basis of the title or the abstract for irrelevance to the topic, and 19 papers were excluded after reading the full-text. Thus, data from a total of 6 published clinical trials were included in this systematic review. Overall, 2,224 male patients were randomised to the intervention group (n = 1221) or control group (n = 1003).
Figure 1. Study selection process.
Table 1 shows the characteristics of the included studies. All of the selected trials were randomised controlled trials (RCTs) and reported in English. Before the randomisation, all male patients in the included studies were treated with alpha-blocker. Among the 6 included trials, subjects were treated with tamsulosin in 4 studies14,15,16,17 and terazosin in 1 study18 and the last study19 did not describe the treatment in detail. Of the 6 trials, the patients of the intervention group in 316,18,19 were randomised to receive tolterodine, and solifenacin was used as an add-on therapy in 214,15. Oxybutynin was used in only one trial17. The methodological quality of the trials was assessed using the Jadad scoring system: four trials scored more than 2 points, the remaining two scored 2 points each. The scores indicate four papers were high quality and two were moderate quality studies. A summary of the included trials is shown in Table 2.
Table 1. Characteristics of included studies.
| Participants | ||||||||
|---|---|---|---|---|---|---|---|---|
| Trials | Designs | Jadad Score | Total | Intervention group | Control group | Agent used, comparison group and duration | Treated with alpha-blocker before randomization | Outcome measures |
| Athanasopoulos [16] | RCT | 2 | 50 | 25 | 25 | tamsulosin 0.4 mg/day plus tolterodine 4 mg/day versus tamsulosin 0.4 mg/day for 3 months | tamsulosin 0.4 mg/day for 1 week | Qmax, PVR, maximum detrusor pressure during micturition, MCC, QOL, VFC, maximum unstable contraction pressure |
| Yang [18] | RCT | 2 | 69 | 33 | 36 | terazosin 2 mg/day plus tolterodine 4 mg/day versus terazosin 2 mg/day for 6 weeks | terazosin 2 mg/day for 1 week | Qmax, PVR, IPSS total, IPSS storage, IPSS voiding |
| MacDiarmid [17] | RCT | 3 | 418 | 209 | 209 | tamsulosin 0.4 mg/day plus oxybutynin 10 mg/day versus tamsulosin 0.4 mg/day plus placebo for 12 weeks | tamsulosin 0.4 mg/day for 4 weeks | Qmax, PVR, IPSS total, IPSS storage, QOL components of IPSS, SPI, AEs |
| Chapple [19] | RCT | 4 | 652 | 329 | 323 | alpha-blocker plus tolterodine 4 mg/day versus alpha-blocker plus placebo for 12 weeks | alpha-blocker for 1 month | Qmax, PVR, micturitions per 24 h, daytime micturitions, nocturnal micturitions, urgency episodes per 24 h, daytime urgency, nocturnal urgency, UUI episodes per 24 h, OABSS, AEs |
| Yamaguchi [14] | RCT | 4 | 638 | 210/213 | 215 | tamsulosin 0.2 mg/day plus solifenacin 2.5 mg versus tamsulosin 0.2 mg/day plus solifenacin 5.0 mg/day versus tamsulosin 0.2 mg/day plus placebo | tamsulosin for 6 weeks | Qmax, PVR, nocturia episodes, IPSS total, IPSS storage, IPSS voiding, IPSS post micturition symptom score, QOL components of IPSS, micturitions per 24 h, urgency episodes per 24 h, urgency incontinence episodes per 24 h, OABSS, AEs |
| Kaplan [15] | RCT | 4 | 397 | 202 | 195 | tamsulosin 0.4 mg/day plus solifenacin 5 mg/day versus tamsulosin 0.4 mg/day plus placebo | tamsulosin 0.4 mg/day for 4 weeks | PVR, IPSS total, IPSS storage, IPSS voiding, QOL scores, micturitions per 24 h, urgency episodes per 24 h, UPS, PPBC, AEs |
RCT, randomized controlled trial; Qmax, maximum urinary flow rate; PVR, post-void residual; MCC, maximum cystometric capacity; QOL, quality of life; VFC, volume at first contraction; IPSS, International Prostate Symptom Score; SPI, Symptom Problem Index; AEs, adverse events; UUI, urgency urinary incontinence; OABSS, Overactive Bladder Symptom Scores; UPS, Urgency Perception Scale; PPBC, Patient Perception of Bladder Condition.
Table 2. A summary of the main outcomes of included studies.
| Yamaguchi [14] | Yamaguchi [14] | ||||||
|---|---|---|---|---|---|---|---|
| Outcome | Athanasopoulos [16] | Yang [18] | MacDiarmid [17] | Chapple [19] | (SOL: 2.5 mg) | (SOL: 5.0 mg) | Kaplan [15] |
| Qmax, mL/s | +1.32 vs +1.16 | +0.8 vs +0.7 | −0.2 vs +0.1 | −0.2 vs +0.8 | −0.74 vs −0.13 | −0.66 vs −0.13 | NR |
| Change, P | NS | NS | NS | NS | NS | NS | NR |
| PVR, mL | −4.20 vs −8.2 | −3.9 vs −0.7 | +18.2 vs +7.8 | +13.6 vs +1.0 | +13.19 vs +5.92 | +22.59 vs +5.92 | +0.02 vs −13.5 |
| Change, P | NS | NS | up, 0.02 | up, 0.023 | up, 0.029 | up, <0.001 | NS |
| IPSS total | NR | −5 vs −1.2 | −6.9 vs −5.2 | −4.6 vs −4.3 | −3.5 vs −3.1 | −3.1 vs −3.1 | −5.38 vs −4.90 |
| Change, P | NR | down, <0.001 | down, 0.006 | NS | NS | NS | NS |
| IPSS storage | NR | −4 vs −1 | −3.7 vs −2.4 | −2.6 vs −2.1 | −2.3 vs −1.8 | −2.4 vs −1.8 | −2.80 vs −2.33 |
| Change, P | NR | down, <0.001 | down, <0.001 | down, 0.037 | down, 0.022 | down, 0.011 | NS |
| IPSS voiding | NR | −1.07 vs −0.2 | NR | −2.1 vs −2.0 | −0.9 vs −0.9 | −0.4 vs −0.9 | −2.54 vs −2.59 |
| Change, P | NR | NS | NR | NS | NS | NS | NS |
| Micturitions per 24 h | NR | NR | NR | −1.8 vs −1.2 | −1.27 vs −0.22 | −1.06 vs −0.22 | −1.05 vs −0.67 |
| Change, P | NR | NR | NR | down, <0.01 | down, <0.001 | down, <0.001 | NS |
| Urgency Episodes per 24 h | NR | NR | NR | −2.9 vs −1.8 | −2.18 vs −1.93 | −2.36 vs −1.93 | −2.18 vs −1.10 |
| Change, P | NR | NR | NR | down, ≤0.001 | NS | down, 0.049 | down, <0.001 |
Qmax, maximum urinary flow rate; NS, not significant; NR, not reported; PVR, post-void residual; IPSS, International Prostate Symptom Score.
Change: change in intervention group vs change in control group; P: P < 0.05 considered as statistical significance between groups, P ≥ 0.05 considered as NS.
The study by Athanasopoulos16 recruited 50 men aged 50–80 years with urodynamically proven mild or moderate bladder outlet obstruction (BOO) and concomitant detrusor instability. Before randomisation, all male patients were treated with 0.4 mg tamsulosin per day for 1 week. Subsequently, 25 of those patients (control group) continued to be treated with tamsulosin only and the other patients (intervention group) received an additional 2 mg tolterodine twice daily. Given that a placebo was not used, the effectiveness of blinding was poor, which may have affected the outcomes in both groups. After 3 months of treatment, a significant improvement was reported in the maximum cystometric capacity (MCC), volume at first contraction (VFC) and maximum unstable contraction both groups. The maximum urinary flow rate (Qmax) and post-void residual (PVR) were not significantly different between the control group and the intervention group. In this study, data reported by the authors were presented as the mean ± SEM. Thus, we performed a corresponding conversion for the SEM. However, the SD was very low due to the number of enrolled subjects in the trial.
Yang et al.18 reported on 69 male LUTS patients who still suffered storage symptoms after treatment with terazosin at a dose of 2 mg once daily for 1 week. Thirty-six patients in the control group continued to receive 2 mg terazosin per day, and 33 patients in the intervention group received 2 mg terazosin per day plus 4 mg tolterodine per day. After 6 weeks, all patients completed the International Prostate Symptom Score (IPSS) questionnaire. Yang discovered that the reduction in the total IPSS and storage IPSS of the intervention arm was significantly greater than that of control arm. For Qmax (maximum urinary flow rate) and PVR (post-void residual), there were no significant differences between the groups after a 6-week treatment. In Yang's study, the control group was treated with only terazosin and blinding was not mentioned, which may affect the assessment of the data quality. However, the overall quality was assessed as acceptable, and the data were extracted for analysis.
In MacDiarmid's study17, 418 patients were included after the 4 weeks of treatment with tamsulosin (0.4 mg once daily). The patients were administered either 0.4 mg tamsulosin per day plus 10 mg oxybutynin per day or the same dose of tamsulosin plus placebo. At 12 weeks, analysis of the total IPSS and storage IPSS revealed an advantage for patients treated with oxybutynin compared with the placebo group. There were no significant differences between oxybutynin and placebo with respect to the Qmax throughout the study, and the treatment with oxybutynin resulted in an increase in PVR at week 12 compared with placebo.
Chapple et al.19 reported an RCT recruiting 652 male patients aged greater than 40 years. All patients suffered from OAB symptoms and had taken a stable dose of alpha-blocker for more than 1 month as a treatment for LUTS. The most frequently used alpha-blocker in his study was tamsulosin, and the other alpha-blockers such as alfuzosin, doxazosin and terazosin were also used by enrolled subjects. Although different medications were used in the included patients, no contrast was mentioned for the efficacy of the different alpha-blockers or the different doses. Three hundred and twenty-nine male LUTS patients in the intervention arm were treated with alpha-blocker plus 4 mg tolterodine per day, and 323 patients in the control arm were treated with the same alpha-blocker plus placebo. For 24-h micturition and 24-h urgency episodes, greater reductions were discovered in the intervention arm. The intervention arm demonstrated a significantly greater improvement in storage IPSS scores. However, there were no significant differences between the two groups in changes in total IPSS scores. Although the difference in the mean increase in PVR between the groups was statistically significant, this increase was not considered to be clinically meaningful. There were no statistically significant differences in Qmax between the two groups.
Yamaguchi et al.14 recruited 638 patients aged greater than 50 years with LUTS and residual OAB symptoms despite treatment with tamsulosin for ≥6 weeks. The patients were randomised to receive 0.2 mg tamsulosin plus 5.0 mg solifenacin, 0.2 mg tamsulosin plus 2.5 mg solifenacin or the same dose of tamsulosin plus placebo. After 12 weeks of double-blind treatment, both treatment arms had significantly better improvements in storage IPSS and 24-h micturitions than the placebo arm. However, there was no improvement in the total IPSS. There was a statistically significant reduction in the mean change in urgency episodes when using the standard dose of 5 mg solifenacin compared with placebo. However, there were no statistically significant differences between the 2.5 mg solifenacin treatment arm and the placebo arm.
In Kaplan's study15, patients were randomised to two groups after taking 0.4 mg tamsulosin per day for 4 weeks. The intervention group consisted of 202 patients who were treated with 0.4 mg tamsulosin plus 5 mg solifenacin, and the control group consisted of 195 patients who were treated with the same dose of solifenacin plus placebo. After 12 weeks of treatment, a statistically significant reduction in the number of 24-h urgency episodes observed between the two groups. However, the differences in PVR, total IPSS, storage IPSS, voiding IPSS and 24-h micturitions between the groups were not statistically significant.
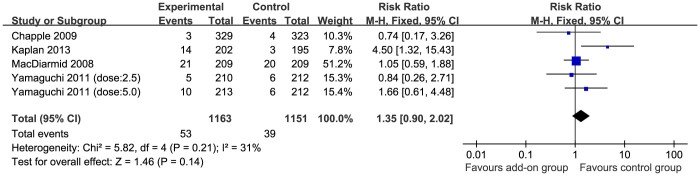
Data on Qmax and PVR were extracted for Forest plot from five studies14,16,17,18,19 that involved a total of 1827 subjects (Figure 2 and Figure 3). However, the results of meta-analysis revealed that no significant association exist between the use of muscarinic antagonists and the improvement in Qmax (MD = 0.04; 95%CI, −0.43–0.51; p = 0.85).The meta-analysis of the data in Figure 3 indicated a tendency towards an increase in PVR when treated with muscarinic antagonists (MD = 10.35; 95%CI, 6.59–14.11; p < 0.00001). For subjective outcomes, although the only validated scoring system for assessing LUTS was IPSS, only 4 trials14,16,17,18 reported total IPSS and storage IPSS. Of these 4 papers, only 217,18 described the outcomes as the mean ± SD. LUTS were significantly ameliorated in the intervention group when assessed by total IPSS (Figure 4; MD = −2.37; 95%CI, −3.50–−1.23; p < 0.0001), and the corresponding change was also identified in storage IPSS (Figure 5; MD = −1.65; 95%CI, −3.00–−0.31; p = 0.02). Almost all these studies except for Athanasopoulos's16 and Yang's18 reported AEs and discontinuation rates. Approximately 44.2% of subjects in the add-on group reported side effects. However, 37.8% of subjects allocated to the placebo group also reported adverse effects. Among all those studies, the most common adverse event was dry mouth, and other side effects such as constipation and dizziness also occurred in both groups. Figure 6 indicates that the overall RR was 1.17 (95%CI, 1.06–1.29; p = 0.002). The discontinuation rates were higher in the intervention arm compared with 3.4% patient withdrawal in the placebo arm; regardless, the differences between the groups were not statistically significant (Figure 7; overall RR = 1.35; 95%CI, 0.90–2.02; p = 0.14).
Figure 2. Fixed effect model of the mean differences (MDs) with 95% confidence intervals (CIs) of maximum urinary flow rate (Qmax).
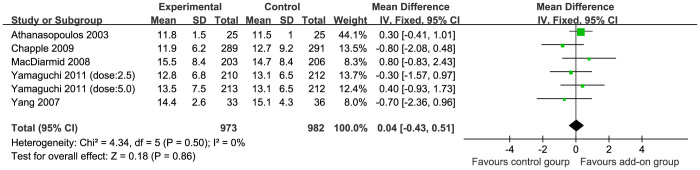
Figure 3. Fixed effect model of the mean differences (MDs) with 95% confidence intervals (CIs) of post-void residual (PVR).
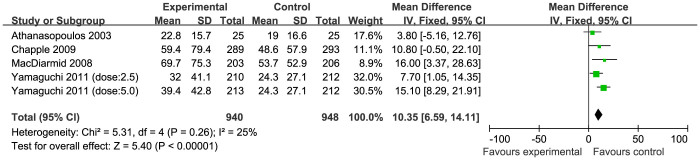
Figure 4. Fixed effect model of the mean differences (MDs) with 95% confidence intervals (CIs) of total International Prostate Symptom Score (IPSS).
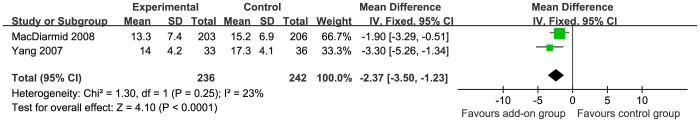
Figure 5. Random effect model of the mean differences (MDs) with 95% confidence intervals (CIs) of storage International Prostate Symptom Score (IPSS).
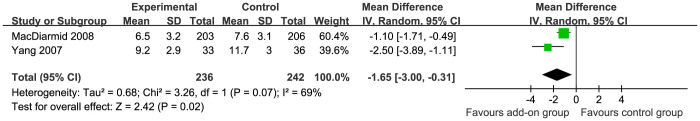
Figure 6. Fixed effect model of the risk ratios (RRs) with 95% confidence intervals (CIs) of adverse events (AEs).
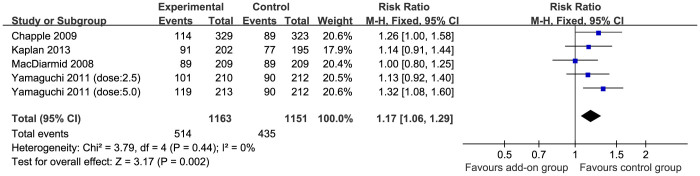
Figure 7. Fixed effect model of the risk ratios (RRs) with 95% confidence intervals (CIs) of discontinuation rates.
Cochrane risk of bias tool was used to assess all included trials. All trials in this meta-analysis clearly described the sequence generation process and the concealment of allocation prior to assignment. Almost all included trials except for Athanasopoulos's16 and Yang's18 were judged to have low risk of bias in blinding of participants/personnel and outcome assessment. 3 trials16,17,18 were hard to permit judgement of “low risk” or “high risk” for insufficient reporting of attrition. Figure 8 indicates the authors' judgements on each risk of bias domain for each trial.
Figure 8. Risk of bias assessment for randomized controlled trials.
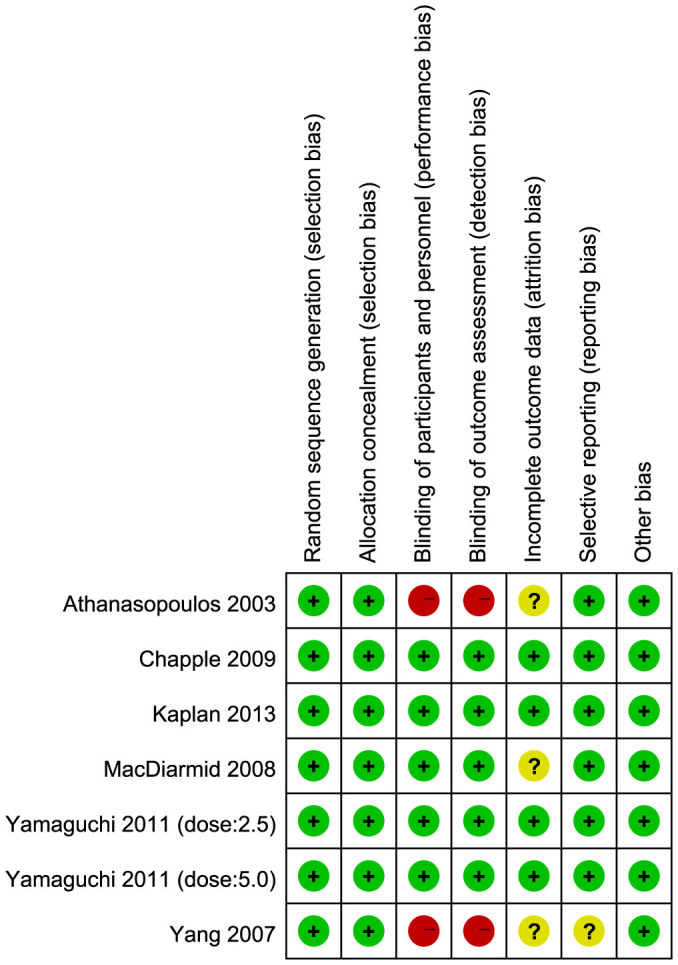
+ indicates low risk of bias, − indicates high risk of bias, and ? indicates unclear risk of bias.
Discussion
To the best of our knowledge, this study is the first systematic review with a meta-analysis of the efficacy and safety of muscarinic antagonist as add-on therapy for male LUTS. Six RCTs of muscarinic antagonists (including tolterodine, solifenacin and oxybutynin) tested in a total of 2,224 male patients with LUTS were included.
Several medications for the treatment of male LUTS are available: alpha-blockers, muscarinic antagonists, 5α-reductase inhibitors and phosphodiesterase type 5 inhibitors10,11. Traditionally, in adult men, LUTS were attributed to benign prostatic enlargement, and the contraction of the prostate is mediated mainly by α1A-adrenoceptors8,12. Thus, of these drugs, alpha-blockers are the most widely used class of medications for the treatment of LUTS. However, storage symptoms persist in some patients treated with alpha-blocker. Therefore, targeting the prostatic smooth muscle alone is not sufficient to relieve LUTS.
Muscarinic receptors include M1, M2, M3, M4 and M5. Of these subtypes, M1 receptors are mainly located in the brain (cortex and hippocampus), glands and sympathetic ganglia. The M4 receptors are located in basal forebrain and striatum, and the M5 receptors are located in substantia nigra. The subtypes M2 and M3 are most predominant in the human bladder13. Although M2 receptors predominate in the bladder, the subtype M3 receptors are primarily responsible for bladder contraction11,13. Based on the theory that inhibiting muscarinic receptors can reduce smooth muscle cell contractions and the sensory threshold of the bladder, muscarinic antagonists are used to treat storage symptoms such as urgency and frequency. However, this blocking activity in turn may decrease the bladder's ability to contract.
Our review of published data from six randomised trials indicated that muscarinic antagonists as add-on therapy yielded better results than placebo although Qmax in the intervention group was not significantly different compared to the control group. The most pragmatic assessment of the efficacy for LUTS is to measure symptom scores20. The total IPSS was significantly improved by treating with muscarinic antagonists, and the storage IPSS also decreased in the intervention arm. Almost all published data indicated that the mean changes in both 24-micturiations episodes and 24-urgency episodes were significantly reduced in the add-on group.
Nearly half (44.2%) of the participants treated with alpha-blocker plus muscarinic antagonist reported an adverse effect. However, the incidence of AEs was also high (37.8%) in alpha-blocker plus placebo. Such a similar incidence of AEs between groups suggests that the AEs may be caused by the alpha-blocker. The most common side effect reported in the intervention group was dry mouth, suggesting that muscarinic antagonists affected the salivary glands. A higher incidence of AUR was expected in the add-on group given the increased PVR. However, instances of AUR were seldom reported, and the incidence of urinary retention (UR) was also low. Other AEs included constipation and dizziness. Of these AEs, UR may have been the main cause for discontinuation. Most of the adverse events were mild or moderate, and the overall safety profile of these agents was generally deemed acceptable.
All of the included studies were RCTs, and the qualities of these RCTs were assessed by the Jadad scoring system. Seven pre-specified criteria were used to evaluate bias, such as selection bias, performance bias, detection bias, attrition bias and reporting bias. Overall, all six studies in this meta-analysis had a fairly low risk of bias. The duration of the six trials varied from 6 weeks to 12 weeks. There was no clear data to determine what the duration of the treatment should be and whether the efficacy and the safety of add-on group were sustainable during long-term therapy. Thus, more data on long-term treatment should be collected in the future to identify the sustained efficacy and safety. Of the six trials included, the patients in two15,19 were required to have less than 10 ng/mL PSA; the patients were required to have less than 4 ng/mL PSA in both Yang's study18 and MacDiarmid's study17; and the two remaining trials did not indicate PSA level requirements. However, we did not analyse the influence of the different serum PSA levels on the data. All indicated above are limitations in our systematic review.
Based on the data available, muscarinic antagonist as an add-on therapy for patients with previous alpha-blocker treatment yielded better results than the control group in terms of the total IPSS, storage IPSS, 24-h micturitions and 24-h urgency episodes. There are also side effects (most often dry mouth) in groups treated with alpha-blocker plus muscarinic antagonist, and increased PVR is more likely to occur in these groups. Thus, we recommend that male patients with persistent LUTS after alpha-blocker treatment take the muscarinic antagonist as an add-on therapy to alleviate the storage symptoms. In addition, PVR should be measured during the treatment to assess the increase in PVR or the incidence of UR.
Methods
Design and search strategy
All relevant randomised controlled trials that involved at least one study arm using a muscarinic antagonist drug and included male LUTS patients still suffering from storage symptoms after alpha-blocker treatment were identified for this systematic review and meta-analysis. A comprehensive database search was performed by Li J and Shi Q independently. The following databases were searched: Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE (via PubMed) and EMBASE. Additional articles or abstracts were retrieved via hyperlinks and by manually scrutinising the reference lists of the selected papers and other relevant publications from the American Urological Association (AUA), European Association of Urology (EAU), and International Continence Society (ICS) between 2008 and 2013. There was no restriction on the language of the publication. The following search terms were used to identify any relevant studies: “muscarinic antagonist or antimuscarinic or anticholinergic or tolterodine or oxybutynin or propiverine or solifenacin” and “alpha-blocker or adrenergic alpha-1 receptor antagonist or doxazosin or alfuzosin or terazosin or tamsulosin or naftopidil” and “lower urinary tract symptoms or LUTS or benign prostatic hyperplasia or BPH” and “randomised controlled trial or RCT” and “human” and “male”.
Study selection and data extraction
Two investigators evaluated all the potentially eligible studies independently without prior consideration of the results. The following criteria were used for study selection: (1) the study was a randomised controlled trial (RCT), (2) the patients were males and were required to have a history of LUTS, and (3) the patients were treated with alpha-blocker before randomisation. Studies were excluded if: (1) the studies were not RCTs, (2) the articles reported on neurogenic LUTS or LUTS in women/children, (3) the patients had a history of prostatic surgery or history of prostate cancer, (4) the patients were treated before randomisation with other medications other than alpha-blockers, and (5) the studies included other interventions except for muscarinic antagonists.
Data extraction was performed independently by two reviewers and then cross checked. Any discrepancy was resolved by author Han P. For each included study. The following information was extracted: the first author, year of publication, study design and relevant outcome data. The primary outcome measure was IPSS (through completing the IPSS questionnaire: included total IPSS and storage IPSS) and the secondary outcomes included Qmax (assessed by uroflowmetry), PVR (measured by ultrasound), micturitions per 24 h, urgency episodes per 24 h, adverse events and discontinuation rates. We tried to contact all corresponding authors for the missing data. The quality of the included trials was assessed using the Jadad scoring system21, which is used to evaluate studies based on randomisation, blinding, description of withdrawals and dropouts22. A study with a Jadad score of ≥3 was considered to be a high-quality study23. Any disagreements that could not be reconciled by discussion were considered by Han P or by Wei Q. Two authors, Li J and Shi Q, used the Cochrane risk of bias tool to assess all included studies. The following seven quality parameters were considered: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting and (7) other bias. These criteria for a judgement of low, high or unclear risk of bias for each item were used to describe the bias. Data from the included trials were processed as described in the Cochrane Reviewers' handbook24.
Statistical analysis
Statistical analyses were conducted by Review Manager, version 5.1.0 (Cochrane Collaboration, Oxford, UK). I2 statistic was used to assess heterogeneity in study results. The Mantel-Haenszel chi-squared test for heterogeneity was performed. I2 values < 25% were considered to indicate no heterogeneity; 25%–50% was considered as moderate heterogeneity; 50%–75% was considered as large heterogeneity and >50% was considered to indicate extreme heterogeneity25. A fixed effect was used for calculations in the absence of evidence of heterogeneity; otherwise, a random effects model was applied. We reported the risk ratio (RR) for dichotomous data and weighted mean differences (WMD) for continuous data, accompanied by 95% confidence intervals (CI). A p value < 0.05 was considered statistically significant.
Author Contributions
H.P. and W.Q. have contributed to the conception and design of the study, and the critical revision of the article. L.J. and S.Q. searched and selected the studies, analyzed the data, prepared figures 1–8 and drafted the article. B.Y., P.C. and T.Y. participated in the acquisition of data and statistical analysis. Y.H. and W.Y. participated in the interpretation of data.
Acknowledgments
This work was collectively supported by grant (National Natural Science Foundation of China (No.30901484 and No.81270841)), and Science & Technology Pillar Program from Science & Technology Department of Sichuan Province (2013SZ0034). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- Irwin D. E. et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50, 1306–1315 (2006). [DOI] [PubMed] [Google Scholar]
- Rosen R. et al. Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7). Eur Urol 44, 637–649 (2003). [DOI] [PubMed] [Google Scholar]
- Sexton C. C. et al. The overlap of storage, voiding and postmicturition symptoms and implications for treatment seeking in the USA, UK and Sweden: EpiLUTS. BJU Int 103 Suppl 3, 12–23 (2009). [DOI] [PubMed] [Google Scholar]
- Abrams P. et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61, 37–49 (2003). [DOI] [PubMed] [Google Scholar]
- Irwin D. E., Kopp Z. S., Agatep B., Milsom I. & Abrams P. Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 108, 1132–1138 (2011). [DOI] [PubMed] [Google Scholar]
- Chapple C. R. & Roehrborn C. G. A shifted paradigm for the further understanding, evaluation, and treatment of lower urinary tract symptoms in men: focus on the bladder. Eur Urol 49, 651–658 (2006). [DOI] [PubMed] [Google Scholar]
- Lemack G. E. Defining the role of overactive bladder treatments in men with lower urinary tract symptoms. Nat Clin Pract Urol 4, 174–175 (2007). [DOI] [PubMed] [Google Scholar]
- Füllhase C. et al. Systematic review of combination drug therapy for non-neurogenic male lower urinary tract symptoms. Eur Urol 64, 228–243 (2013). [DOI] [PubMed] [Google Scholar]
- Roosen A. et al. A refocus on the bladder as the originator of storage lower urinary tract symptoms: a systematic review of the latest literature. Eur Urol 56, 810–820 (2009). [DOI] [PubMed] [Google Scholar]
- Oelke M. et al. EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64, 118–140 (2013). [DOI] [PubMed] [Google Scholar]
- McVary K. T. et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 185, 1793–1803 (2011). [DOI] [PubMed] [Google Scholar]
- Michel M. C. & Vrydag W. Aplha1-, alpha2- and beta-adrenoceptors in the urinary bladder, urethra and prostate. Br J Pharmacol 147 Suppl 2, S88–119 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caulfield M. & Birdsall N. International Union of Pharmacology. XVII. Classification of muscarinic acetylcholine receptors. Pharmacol Rev 50, 279–290 (1998). [PubMed] [Google Scholar]
- Yamaguchi O. et al. Solifenacin as add-on therapy for overactive bladder symptoms in men treated for lower urinary tract symptoms-ASSIT, Randomized Controlled Study. Urology 78, 126–133 (2011). [DOI] [PubMed] [Google Scholar]
- Kaplan S., McCammon K., Fincher R., Fakhoury A. & He W. Safety and tolerability of solifenacin add-on therapy to α-blocker treated men with residual urgency and frequency. J Urol 189 Suppl 1, S129–134 (2013). [DOI] [PubMed] [Google Scholar]
- Athanasopoulos A. et al. Combination treatment with an α-blocker plus an anticholinergic for bladder outlet obstruction: a prospective, randomized, controlled study. J Urol 169, 2253–2256 (2003). [DOI] [PubMed] [Google Scholar]
- MacDiarmid S. A. et al. Efficacy and safety of extended-release oxybutynin in combination with tamsulosin for treatment of lower urinary tract symptoms in men: randomized, double-blind, placebo-controlled study. Mayo Clin Proc 83, 1002–1010 (2008). [DOI] [PubMed] [Google Scholar]
- Yang Y. et al. Efficacy and safety of combined therapy with terazosin and tolterodine for patients with lower urinary tract symptoms associated with benign prostatic hyperplasia: a prospective study. Chin Med J 120, 370–374 (2007). [PubMed] [Google Scholar]
- Chapple C. et al. Tolterodine treatment improves storage symptoms suggestive of overactive bladder in men treated with α-blockers. Eur Urol 56, 534–543 (2009). [DOI] [PubMed] [Google Scholar]
- Blake-James B. T., Rashidian A., Ikeda Y. & Emberton M. The role of anticholinergics in men with lower urinary tract symptoms suggestive of benign prostatic hyperplasia: a systematic review and meta-analysis. BJU Int 99, 85–96 (2007). [DOI] [PubMed] [Google Scholar]
- Jadad A. R. et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials 17, 1–12 (1996). [DOI] [PubMed] [Google Scholar]
- Altman D. G. & Schulz K. F. Statistics notes: Concealing treatment allocation in randomised trials. BMJ 323, 446–447 (2001). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D. et al. Does quality of reports of randomized trials affect estimates of intervention efficacy reported in meta-analyses? Lancet 352, 609–613 (1998). [DOI] [PubMed] [Google Scholar]
- Higgins J. & Green S. Cochrane Handbook For Systematic Reviews Of Interventions 5.1.0 (The Nordic Cochrane Centre, Copenhagen, 2011). [Google Scholar]
- Higgins J. P., Thompson S. G., Deeks J. J. & Altman D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]