Abstract
Based on the amyloid hypothesis, controlling β-amyloid protein (Aβ) accumulation is supposed to suppress downstream pathological events, tau accumulation, neurodegeneration and cognitive decline. However, in recent clinical trials, Aβ removal or reducing Aβ production has shown limited efficacy. Moreover, while active immunisation with Aβ resulted in the clearance of Aβ, it did not prevent tau pathology or neurodegeneration. This prompts the concern that it might be too late to employ Aβ targeting therapies once tau mediated neurodegeneration has occurred. Therefore, it is timely and very important to develop tau directed therapies. The pathomechanisms of tau mediated neurodegeneration are unclear but hyperphosphorylation, oligomerisation, fibrillisation and propagation of tau pathology have been proposed as the likely pathological processes that induce loss of function or gain of toxic function of tau, causing neurodegeneration. Here we review the strategies for tau directed treatments based on recent progress in research on tau and our understanding of the pathomechanisms of tau mediated neurodegeneration.
INTRODUCTION
Alzheimer’s disease (AD) is the most common cause of dementia, contributing to up to 70% of dementia cases. As the global population ages, nearly 35.6 million people worldwide are estimated to be living with dementia, and the number of people with dementia is predicted to double by 2030 (65.7 million) and more than triple by 2050 (115.4 million) if effective disease modifying therapies are not developed.1 Current therapies for AD only provide symptomatic relief, either by temporarily improving symptoms above baseline or by delaying cognitive decline. Thus disease modifying therapies based on the pathomechanisms of AD are a central focus of AD drug discovery.
AD has two pathological hallmarks: senile plaques (SPs), consisting of β-amyloid protein (Aβ), and neurofibrillary tangles (NFTs), consisting of tau protein. Mutations in the amyloid precursor protein (APP) gene that lead to excess production or reduced clearance of Aβ in the brain, and mutations in the genes encoding protease subunits (ie, presenilin (PS) 1 and 2, involved in cleavage of APP to generate amyloidogenic Aβ peptides) induce AD in an autosomal dominant manner. Therefore, abnormal accumulation of Aβ is speculated to be the most important and disease specific pathomechanism involved in the initiation of the multiple pathological steps leading to Aβ oligomerisation, abnormal tau aggregation, synaptic dysfunction, cell death and brain shrinkage. This assumption is widely accepted as the amyloid hypothesis of AD.2 The results of clinicopathological studies and recent clinical studies using biomarkers, including amyloid positron emission tomography (PET), 2-[18 F]-fluoro-2-deoxy-D-glucose (FDG)-PET, CSF analysis of Aβ and tau/p-tau, and MRI support the amyloid hypothesis. Neocortical SPs appear in the preclinical phase more than 10 years earlier than neocortical NFTs, and NFT expansion accompanies cognitive decline.3–5
This hypothesis has been further supported by a recent cross sectional analysis study looking at families with autosomal dominant AD. By using the participant’s age and their parent’s age at symptom onset, researchers estimated the years from expected symptom onset of AD. They could then determine the relative order and magnitude of pathophysiological changes associated with AD,6 although it is still uncertain whether sporadic AD has a similar pathophysiological process to inherited AD. However, other studies indicate that tau pathology appears at a younger age than SPs7 and most recently Braak and Del Tredici,8 and Elobeid et al9 demonstrated tau positive pathology in cases less than 30 years of age. Based on these data, they propose that tau pathology begins to deposit in the locus coeruleus and then spreads from there to other brainstem nuclei and to the entorhinal cortex (EC), perhaps by direct cell to cell transmission. This has led to an alternative hypothesis that subcortical tangle pathology before SP formation represents the earliest stages of tau pathology in sporadic AD (figure 1).7–10 However, other interpretations cannot be excluded, such as this tau pathology is merely an insignificant alternation related to aging, or that soluble oligomeric Aβ accumulation precedes this early tau pathology.
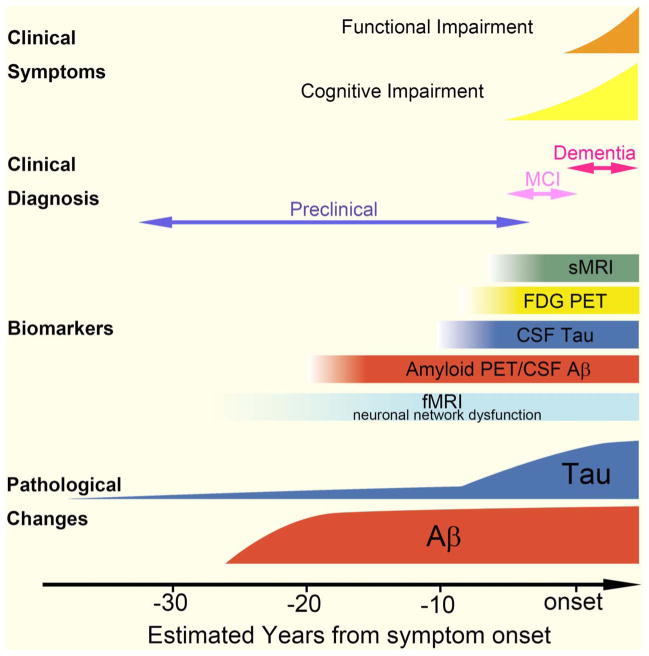
Figure 1.
Chronological relationships among pathology, clinical symptoms and biomarkers. Based on biomarker studies, β-amyloid protein (Aβ) accumulation appears to start ~20 years before the onset of dementia. Amyloid positron emission tomography (PET) or a decrease in Aβ1–42 levels in CSF may indicate Aβ accumulation in the brain, even in preclinical Alzheimer’s disease (AD). Neocortical tau pathology correlates closely with the timing of symptom onset. But, as discussed in the text, these findings need to be reconciled with reports by Braak and colleagues7,8 that tau pathology is seen in the brain prior to Aβ pathology, while functional MRI (fMRI) abnormalities may be the earliest biomarker to change in the preclinical phase of AD.11–14 FDG, 2-[18 F]-fluoro-2-deoxy-D-glucose; MCI, mild cognitive impairment.
Aβ biomarker (amyloid PET, Aβ1–42 in CSF) abnormalities precede synaptic dysfunction (FDG-PET) and tau biomarker (tau/p-tau in CSF) abnormalities, followed by brain structural changes (structural MRI) and, finally, cognitive decline (figure 1). However, other studies suggest that functional MRI, which indicates neuronal hyperconnectivity or hypoconnectivity, may show abnormalities before amyloid biomarkers become abnormal, thereby suggesting this may be the earliest biomarker to change in preclinical AD (figure 1).11–14 According to the amyloid cascade hypothesis, pharmacological agents that reduce brain Aβ content are supposed to act as effective drugs against AD; several different candidate drugs of this type have been developed. However, clinical trials directed at increasing the clearance or decreasing production of Aβ, which are at different stages of development, have been largely disappointing. Active immunisation with Aβ (AN1792) resulted in impressive clearance of SPs from the brain, as confirmed by pathological examination, but did not prevent progressive cognitive decline, NFT formation or neurodegeneration.15 Moreover, neither tarenflurbil16 nor semagacestat (http://files.shareholder.com/downloads/LLY/1921397628x0x395879/54b1f68f-c7b8-4c04-87d1-8c609c21f6f7/LLY_News_2010_8_17_Product.pdf), which act to decrease the production of Aβ, showed any clinical benefits. Most recently, the results on the phase III clinical trials of passive immunisations against Aβ (bapineuzumab and ?solane-zumab) were announced (http://www.pfizer.com/news/press_releases/pfizer_press_release.jsp?guid=20120806006130en&source=RSS_2011&page=1; http://newsroom.lilly.com/releasedetail.cfm?releaseid=702211). None of these clinical trials proved significant efficacy of the primary endpoints, although the potential efficacy was not completely denied.
These observations have challenged the assumption that Aβ induces tau mediated neurodegeneration, and the work of Braak et al7,8,17 are consistent with the view that tau pathology emerges autonomously and independently from Aβ, and tau pathology may be the more proximal cause of neurodegeneration in AD. This view is supported by findings in AD mouse models: Aβ immunotherapy in 3×Tg-AD (PS1 (M146V), APP (Swe) and tau (P301L)) mice resulted in a reduction in extracellular SPs and intracellular Aβ accumulation and led to the clearance of less phosphorylated tau pathology; however, hyperphosphorylated tau aggregates were unaffected by Aβ antibody treatment.18 Additionally, reduction of both soluble Aβ and tau levels, but not a reduction of soluble Aβ levels alone, ameliorated cognitive decline.19 Therefore, Aβ targeting therapies might exert preventive effects in the preclinical or very early clinical stages of AD, but once cognitive decline appears in association with accumulations of tau pathology, then tau targeting drugs might be necessary for disease modification (figure 1).
MOLECULAR MECHANISMS OF TAU MEDIATED NEURODEGENERATION
Tau protein is a member of a large family of microtubule associated proteins that are involved in microtubule (MT) assembly and stabilisation; therefore, tau protein plays an important role in maintaining appropriate neuron morphology and intercellular transport with motor proteins. Tau proteins are predominantly expressed in neurons, but they are also expressed in lower quantities in astrocytes and oligodendrocytes. In the adult human brain, six tau isoforms are produced from a single gene on chromosome 17q21 by alternative mRNA splicing.20,21 The six isoforms differ from each other by the presence or absence of one or more of three distinctive inserts encoded by exons 2, 3 and 10. Exons 9–12 in the tau gene encode four MT binding motifs, which are imperfect repeats of 31 or 32 amino acids in the carboxy terminal half of the tau molecule, and alternative splicing of exon 10 generates tau protein isoforms with three or four MT binding repeats. In the normal adult human brain, similar levels of three and four MT binding repeat tau isoforms are expressed.22 However, several tauopathies exhibit an imbalance in tau isoform accumulation: progressive supranuclear palsy (PSP), corticobasal degeneration (CBD) and argyrophilic grain disease show selective four repeat tau accumulation, while Pick’s disease shows selective three repeat tau accumulation. Under normal physiological conditions, the balance of phosphorylation and dephosphorylation of tau coordinates tau attachment to and detachment from MTs, where it has a role in maintaining MT stability and in the trafficking of cargoes along the axon.23 Thus loss of normal function of tau protein induces structural and functional impairments of MTs. Also, because neuronal processes (dendrites and axons) extend over long distances, profound adverse effects may occur at distal parts of neurons, such as synapses (figure 2).
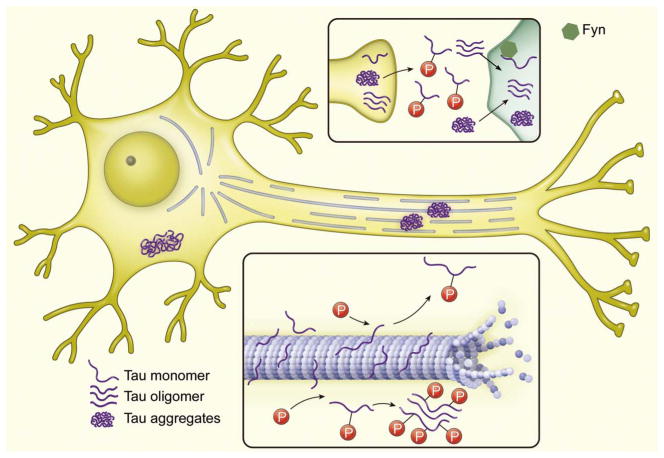
Figure 2.
Schematic presentation of tau mediated neurodegeneration. Phosphorylation and dephosphorylation of tau control the attachment and detachment of tau from microtubules (MT). Hyperphosphorylation of tau induces disassembly of MTs, causing axonal transport insufficiency. Unbound tau self-aggregates into oligomers or aggregates. Tau aggregates in axons or dendrites congest axonal transport. Tau pathology is transmitted synaptically. An interaction between Fyn and tau induces synaptic dysfunction.
The most compelling causes of dysfunctional tau in tauopathies are the abnormal hyperphosphorylation of this protein and mutations that impair the binding of tau to MTs.24 Hyperphosphorylation decreases the ability of tau to bind to MTs, resulting in an abnormal increase in the levels of unbound tau. It is likely that higher cytosolic concentrations of tau increase the likelihood that oligomers and aggregates will form (figure 2). Tau can self-aggregate into filaments through its MT binding repeat, which have a β sheet structure. The molecular mechanism by which tau phosphorylation may lead to aggregation is still unclear, although it is presumed that hyperphosphorylation precedes tau aggregation by a series of studies.25 However, the flanking regions, especially the region amino terminal to the repeat region, inhibit self-aggregation of tau. In the abnormal hyperphosphorylation that occurs in AD and other tauopathies, this inhibition might be diminished, resulting in tau self-assembling into filaments.26 Interestingly, observations of tangles and the activation of caspases in living tau transgenic (Tg) mice (rTg4510) using in vivo multiphoton imaging suggest that caspase activation precedes NFT formation, and it was proposed that tau, which had been truncated as a result of caspase cleavage, recruited normal tau causing it to misfold and form tangles.27 An immunoelectron microscopic study, by contrast, demonstrated that caspase cleaved tau was a minimal component of NFTs in rTg4510 mice.28 However, it is still unclear whether NFTs themselves are toxic, and whether or not truncation of tau is an important early pathological step promoting oligomerisation and fibrillisation.
Several recent studies have demonstrated that extracellular tau aggregates contribute to the propagation of tau pathology. Recombinant tau fibrils29 or paired helical filaments (PHFs) from AD brain,30 when added to the culture medium, can be taken up by cells and induce fibrillisation of cytoplasmic tau, and the induced aggregates can be transferred between cells in a co-culture system.29,31 In vivo, injection of brain extracts from mutant P301S tau expressing mice into the brains of wild-type (WT) tau expressing mice induces assembly of WT human tau into filaments and spreading of tau pathology to neighbouring brain regions.32 Recently, two similar papers on the propagation of tau pathology from the EC to other areas along neuronal networks were published.33,34 The authors of these papers used bigenic mice expressing P301L mutant human tau, primarily directed to be expressed in the superficial layers of the medial EC, and to a lesser extent in the lateral EC and pre- and para-subiculum. They showed propagation of tau pathology anterogradely along a neural network from the EC to the dentate gyrus, and then the CA1 and CA3 areas, indicating that tau pathology might spread trans-synaptically (figure 2). Interestingly, tau aggregates consisted of both human and mouse tau, indicating that human mutant tau seeded mouse tau aggregation.33
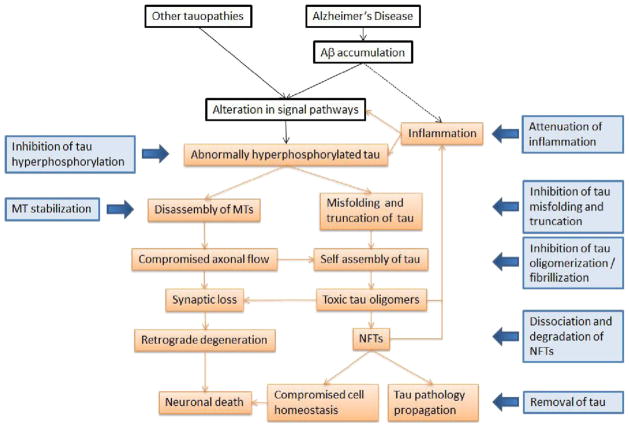
The presumed molecular mechanisms underlying tau mediated neurodegeneration and possible therapeutic targets are summarised in figures 2 and 3.
Figure 3.
Therapeutic targets for possible pathomechanisms in tauopathies. Aβ, β-amyloid protein; MT, microtubules; NFT, neurofibrillary tangle.
THERAPEUTIC STRATEGIES FOR TAU MEDIATED NEURODEGENERATION
MT stabilisation
Post-translational modifications on tau, including phosphorylation, glycosylation, nitration and acetylation, and changes in the ratio of three to four repeat tau, all of which are observed in AD and/or related tauopathies, should compromise the normal physiological function of tau. The most important function of tau is to assemble and stabilise MTs. Hyperphosphorylation of tau induces a reduction in the ability of tau to bind MTs which, together with the sequestration of tau into NFTs and neuritic tau pathology thereby depleting functional tau, can cause MT instability and disassembly, culminating in impaired axonal transport. Impaired axonal transport and decreased MT density are observed particularly in the early stage of AD.35,36 A tauopathy mouse model expressing T44 human WT tau showed tau hyperphosphorylation, neuronal tau accumulation, decreased MT density, reduced fast axonal transport and axonal spheroids, which indicate impaired axonal transport.37 When this tauopathy mouse model was treated with the MT stabilising drug paclitaxel, which is used for cancer treatment, mice showed a significant improvement in fast axonal transport and MT density compared with vehicle treated mice. Furthermore, their motor function markedly improved.38 However, paclitaxel has poor blood–brain barrier permeability, making it unsuitable for the treatment of human tauopathies.
A similar MT stabilising drug, epothilone D, demonstrates a favourable pharmacokinetic and pharmacodynamic profile. Epothilone D treatment reduced forebrain tau pathology and increased hippocampal neuronal integrity, with no dose limiting side effects, in tauopathy model mice (PS19).39,40 Another study indicated that treatment with a very low dose of BMS-241027 (identical to epothilone D) improved cognitive function and tau pathology in rTg4510 tau Tg mice.41 These data reveal that brain penetrant MT stabilising drugs hold promise for the treatment of AD and related tauopathies, and that epothilone D could be a good candidate for a clinical trial. Phase I clinical trials for mild AD to evaluate the safety, tolerability and effect of epothilone D on CSF biomarker have started (http://clinicaltrials.gov/ct2/show/NCT01492374).
Another MT stabilising drug is davunetide (also referred to as NAP and AL-108) which is an octapeptide derived from activity dependent neuroprotective protein.42 Intranasal administration of davunetide is undergoing phase II clinical trials for the treatment of tauopathies, including PSP, frontotemporal dementia and parkinsonism linked to chromosome 17 (FTDP-17), CBD and progressive non-fluent aphasia (http://www.clinicaltrials.gov/ct2/show/NCT01056965). The main pharmacological action of davunetide is thought to be stabilisation of MTs in neurons,43 although the drug has other pleiotrophic effects and does not directly affect the polymerisation or dynamics of reconstituted neural MTs.44
Inhibition of tau phosphorylation
Hyperphosphorylation of tau is believed to be a crucial step in tau mediated neurodegeneration to initiate MT instability, and misfolding and truncation of tau (figure 2). The phosphorylation state of tau is a function of the balance between the activities of tau protein kinases and phosphatases. Thus inhibition of tau kinases and activation of phosphatases represent excellent targets for therapeutic intervention in AD and related dementias.
Inhibition of tau kinases
Some kinases have been shown to phosphorylate tau in vitro,45 but the identities of the physiological and pathological kinases in vivo remain unclear. The most promising candidate kinases for tau phosphorylation are glycogen synthase kinase 3 (GSK-3), cyclin dependent kinase 5 (CDK5), casein kinase 1 (CK1) and protein kinase A (PKA), as well as calmodulin dependent protein kinase II (CaMKII), mitogen activated protein kinases (MAPKs) including ERK1/2, c-Jun N terminal kinase (JNKs) and p38, and MT affinity regulating kinase 1 (MARK1). Among these kinases, GSK-3 and CDK5 are thought to be the best targets for treatment because both phosphorylate tau at a large number of sites, their expression levels in the brain are high and both enzymes have been shown to be associated with all stages of NFT pathology in AD.46–48 GSK-3 has an unusual preference for target proteins, those that have been pre-phosphorylated by priming kinases.48,49 Accumulating evidence suggests that GSK-3 might play a central role between Aβ and tau.50,51 Recent studies suggest that GSK-3α contributes to both SP and NFT pathogenesis while GSK-3β only modulates NFT formation. This emphasises the relevance of GSK-3α, which is less well investigated, as a possible therapeutic target for abrogating formation of AD SPs and NFTs.52
Aβ activates GSK-3β and is essential for Aβ induced neurotoxicity.53–55 APP and PS1 are substrates of GSK-3,56,57 and GSK-3 is thought to regulate Aβ production by interfering with APP cleavage at the γ secretase site.58 Intracerebroventricular anti-Aβ antibody administration to APPswe mice (Tg2576) decreased Aβ and GSK-3β activity.59 Moreover, overexpression of GSK-3β affected spatial memory ability and accelerated NFT formation in a mouse model expressing triple FTDP-17 mutations (G272V, P301L and R406W) and GSK-3β.60 Interestingly, chronic administration of the GSK-3 inhibitor lithium chloride to this mouse model prevented tau hyperphosphorylation and NFT formation, but did not induce disassembly of pre-formed NFTs.61 The attenuations of tau hyperphosphorylation, behavioural impairment and levels of insoluble tau induced by lithium chloride have been described in several other tau Tg mouse models.61–66 Three small clinical trials with lithium (two for mild to moderate AD67,68 and one for amnestic mild cognitive impairment69) have been conducted. The first two trials in AD did not show any beneficial effect of lithium on clinical symptoms or CSF biomarkers. By contrast, the trial in amnestic mild cognitive impairment suggested that lithium treatment was associated with a decrease in p-tau in the CSF and better cognitive performance. Another GSK inhibitor, 2-methyl-5-(3-{4-[(S)-methylsulfinyl] phenyl}-1-benzofuran-5-yl)-1,3,4-oxadiazole, reduces hippocampal tau phosphorylation at GSK-3 sites and ameliorates behavioural dysfunction in 3×Tg-AD mice.70 The non-specific tau kinase inhibitor K252a (for CDK5, GSK3 and ERK1) also reduced levels of hyperphosphorylated tau and ameliorated the motor phenotype in P301L mutant tau Tg mice (JNPL3).71 A novel specific GSK-3 inhibitor, tideglusib (NP-12), was administered to double Tg mice coexpressing human mutant APP and tau, resulting in lower levels of tau phosphorylation, decreased Aβ amyloid deposition and plaque associated astrocytic proliferation, protection of neurones in the EC and CA1 hippocampal subfield against cell death and prevention of memory deficits.72 Currently, phase II clinical trials of tideglusib for the treatment of AD and PSP are ongoing (http://clinicaltrials.gov/ct2/show/NCT01350362), and the Food and Drug Administration and EU have granted tideglusib orphan drug status for treating PSP.
Although other tau protein kinases, including CDK5, CK1 and MAPKs, are considered targets for prevention of tau phosphorylation, no tau kinases other than GSK-3 inhibitors have entered clinical trials to date. It is a challenge to develop inhibitors that are adequately specific for those kinases and these kinases have multiple substrates; inhibition of phosphorylation of these other substrates could cause other side effects.
Activation of phosphatases
The activities of phosphoprotein phosphatase 2A (PP2A) and PP-1 are compromised by ~20% in the AD brain.73–76 The phosphorylation of tau that suppresses its MT binding and assembly activities in adult mammalian brain is regulated by PP2A, not by PP2B,77,78 and PP2A accounts for >70% of all phosphoseryl/phosphothreonyl activity in the human brain.79 Thus PP2A and, in particular, the specific Bα regulatory subunit (or PPP2R2A) form of the PP2A heterrotrimeric complex (PP2A/Bα), has now emerged as a key player in tau dephosphorylation.80 Multiple chemical classes of PP2A enhancers have been identified, including sphingoid, phenolic, anionic and cationic classes.81 However, because PP2A is involved in multiple signal transduction networks that maintain normal cellular homeostasis, indiscriminate activation of PP2A is likely to have many unwanted side effects that will limit clinical utility. Evaluation and comparison of data across studies are difficult and complicated by differences in assay systems, PP2A composition and substrates. Here we describe some candidates for activation of PP2A based on data relating to clinical observations or in vivo observations. For example, it is known that the levels of homocysteine are increased in AD patients, that folate deprivation, which is also observed in AD patients,82 is a major factor contributing to increased homocysteine levels83 and that folate and methyl-folate promote methylation of PP2Ac and subsequent formation of an active Bα containing PPA2 complex that should lead to increased dephosphorylation of tau.84,85 Memantine, a low affinity voltage dependent uncompetitive antagonist of glutamatergic N-methyl-D-aspartate receptors, demonstrates modest efficacy in the treatment of moderate to severe AD. Interestingly, it possesses the ability to enhance PP2A in an indirect manner, attenuating tau hyperphosphorylation in vitro,86 and a 1 year treatment with memantine resulted in a significant decrease in the phosphorylated tau level in the CSF of AD patients.87 Sodium selenate induced dephosphorylation of tau in a PP2A dependent manner in two tau Tg mouse lines, pR5 and K3,88,89 causing reduced phosphorylation of tau, reduced insolubility and reduced behavioural impairment in terms of memory and motor functions, as well as preventing neuronal loss.90
Other post-translational modifications
In addition to phosphorylation, several other post-translational modifications of tau protein, including glycosylation, nitration and acetylation, have been reported. These modifications might alter tau functions directly or indirectly, although those post-translational modifications have received much less attention and are less well understood. O-GlcNAcylation, a type of protein O-glycosylation in which the monosaccharide-N-acetyl-glucosamine (GlcNAc) attaches to serine threonine residues via an O-linked glycosidic bond, regulates phosphorylation of tau in a site specific manner both in vitro and in vivo. At most phosphorylation sites, O-GlcNAcylation negatively regulates tau phosphorylation. The O-GlcNAcylation level in AD brain extracts is decreased compared with that in normal controls.91 Inhibition of the hexosaminidase O-GlcNAcase (OGA) or increased expression of O-β-N-acetylglucosaminyltransferase (OGT) has been shown to reduce levels of phosphorylated tau. Recently, Yuzwa et al92 demonstrated that increasing tau O-GlcNAc with an OGA inhibitor decreased the number of NFTs and protected against neurodegeneration in JNPL3 mice. In addition to single O-GlcNAcylation, multiple other glycosylations, mainly N-linked glycosylations, have been observed on tau in AD patients. Multiple glycosylations of tau are thought to be an early abnormality that can facilitate the subsequent abnormal hyperphosphorylation of tau in AD brain.93 Glycation is a non-enzymatic glycosylation, and PHF-tau from AD brain is highly glycated and forms advanced glycation end products. Advanced glycation end products generate oxygen free radicals, which might contribute to the pathogenesis of AD.94 Recent studies have indicated that acetylation of tau may occur after its phosphorylation and may contribute to tau mediated neurodegeneration by driving tau polymerisation and inhibiting its degradation.95–97 Nitration has been observed on four residues in the tau protein, and each nitration site has a different pathological significance. For example, nitration at Tyr 29 or Tyr 197 increases, but that at Tyr 18 or Tyr 394 decreases, the propensity of tau to form filaments in vitro.98 Antibodies selectively recognising nitration at Tyr 29 or Tyr 197 stain NFTs in AD brain, but an antibody to nitration at Tyr 29 stains some neuronal tau inclusions in the brains of CBD and PSP patients.98 Modulation of these post-translational modifications of tau could be a new therapeutic target, but much more research is needed to advance them into preclinical studies.
Inhibition of tau oligomerisation/fibrillisation
It is still debatable whether fibrillar tau aggregates (ie, NFTs and neuropil threads) are toxic, or if they result from an effort of the cell to sequester toxic oligomers.99 In either case, inhibition of tau polymerisation should be a promising therapeutic target to prevent the toxic effects of tau and increase the levels of monomeric tau, which could contribute to MT stabilisation. Several groups have conducted high throughput screening campaigns to identify aggregation inhibitors.100,101 Here we describe representative studies of such drugs.
The first tau aggregation inhibitor reported was the phenothiazine methylene blue, which inhibits tau–tau binding.102 This compound has also been used to treat a number of different medical conditions, including inherited methaemoglobinaemia, urinary tract infections, paediatric malaria and it now is in clinical trial as a therapy for AD.103 Methylene blue failed to inhibit abnormal phosphorylation of tau, neuronal cell loss or a swimming defect in a tauopathy zebrafish model.104 However, it did reduce levels of insoluble tau by ~35% and ameliorated locomotion abnormalities in a C elegans tauopathy model.105 In a tauopathy mouse model, rTg4510, methylene blue was administered in two ways: directly to the hippocampal CA3 region using a mini-osmotic pump and peripherally, by adding it to drinking water. Both administrations decreased cognitive deficits and levels of phosphorylated and soluble total tau, but not pre-existing tau pathology. Interestingly, the brain tissue levels of methylene blue in the cerebellum were positively correlated with Morris water maze performance and inversely correlated with soluble tau levels.106 A phase II clinical trial of methylene blue for mild to moderate AD patients demonstrated effectiveness at treating the cognitive deficits, as measured by the Alzheimer’s Disease Assessment Scale-cognitive and the Mini-Mental State Examination.107 These preliminary clinical data are encouraging, but since it was shown that methylene blue inhibits MT polymerisation in vitro,108 it will be important to see data from a complete phase III trial of this drug in AD patients to know if it has therapeutic benefits without deleterious side effects.
Degradation of misfolded tau or NFTs
Another strategy to reduce harmful levels of pathological or toxic tau species, including tau oligomers or fibrils, is to enhance degradation of pathological tau. Tau is thought to be degraded via the ubiquitin–proteasome and lysosomal (autophagy) pathways. Thus it has been proposed that dysregulation of normal protein degradation by molecular chaperones could be responsible for tau aggregation. Heat shock protein (Hsp) 70 and the carboxyl terminus of Hsc70 interacting protein (CHIP) cooperate to ubiquitinate and degrade tau.109 Levels of Hsp70 and CHIP were increased, and CHIP levels were inversely proportional to insoluble tau accumulation in AD brains.110 Additionally, reduction of CHIP increased the accumulation of hyperphosphorylated tau in JNPL3 mice.111 CHIP in collaboration with the Hsp90 chaperone complex has a key role in the removal of phosphorylated tau. Inhibition of Hsp90 reduces the level of phosphorylated tau at sites phosphorylated by GSK3β and CDK5. Administration of an Hsp90 inhibitor to a tauopathy mouse model, JNPL3, induced significant reductions in the levels of both hyperphosphorylated and aggregated mutant tau in the brain. The Hsp90 inhibitor also induced a time dependent reduction in the level of p35 (a CDK5 activator) and tau phosphorylation in primary cultured neurons, and it reduced levels of mutant tau but not WT tau in COS-7 cells cotransfected with p35 and WT tau or P301L mutant tau.112 Binding of Hsp90 to tau facilities a conformational change that could result in its phosphorylation by GSK3 and its aggregation into filamentous structures.
Immunophilins, such as FKBP51 and FKBP52, are co-chaperones of Hsp90–tau complexes. FKBP52 binds directly and specifically to tau, especially in its hyperphosphorylated form. FKBP52 inhibited tubulin polymerisation induced by tau in vitro. Overexpression of FKBP52 in differentiated PC12 cells prevented the accumulation of tau and resulted in reduced neurite outgrowth.113 Because FKBP52 does not bind calci-neurin, modulation of FKBP52 activity with FK506/rapamycin derivatives might offer a means of reducing the pathogenic effects of misfold tau without immunosuppression.
Larger aggregates of tau are not likely to be accessible to the proteasome system, but it is possible they could be degraded by the autophagy lysosomal system, which includes three main pathways for the delivery of cargo to lysosomes: macroautophagy, microautophagy and chaperone mediated autophagy. P301L mutant tau expressing Drosophila treated with rapamy-cin, an autophagy inducer, exhibited reduced aggregation of tau and tau induced neurotoxicity.114 Wang et al115 used an inducible mouse neuroblastoma N2a cell model of tauopathy expressing the repeat domain (tau 244–372) of tau with the ΔK280 deletion mutation (TauRDΔK280) or expressing the full length WT hTau40 isoform. They found that macroautophagy could efficiently degrade both soluble mutant tau and aggregates thereof, whereas proteosomal degradation played only a minor role in this system. Inhibition of macroautophagy by 3-methylamphtamine led to enhanced tau aggregation and tau elicited neurotoxicity in N2a cells expressing TauRDΔK280. Recently, the first paper about the effect of increased autophagy in a mouse model of human tauopathy was published. Administration of trehalose, a mammalian target of rapamycin independent activator of autophagy, reduced the number of AT-100 positive neurons and the amount of insoluble tau protein, with improved neuronal survival in the brain of Tg mice expressing a P301S mutant human tau.116 Truncated tau is thought to be more toxic and amyloidogenic than full length tau so it is interesting that a caspase cleaved form of tau was preferentially degraded via autophagy with a faster turnover rate than was seen for full length tau.117 These findings suggest that the autophagy lysosomal system can contribute to the degradation of pathological tau species. The development of selective autophagy modulators that can enhance clearance of pathological tau species without affecting its physiological functions would be of tremendous therapeutic value for not only tauopathies but also for other proteinopathies.
Inhibition of tau and Fyn expression
Although it is unclear whether Aβ accumulation into SPs directly induces clinical symptoms, including cognitive deficits in humans, Tg mice exhibiting Aβ deposition in the brain commonly show cognitive and behavioural deficits without significant neuronal loss. In one of these lines of mice, a cross between PDAPP mice and tau knockout mice with reduced levels of endogenous tau led to improvement in cognitive deficits and reduced lethality, thereby suggesting that tau is necessary for Aβ induced neurotoxicity.118 However, other studies have not confirmed these findings and instead have shown deleterious effects of reducing tau protein levels in tau knockout mice.119,120 Recently, Ittner et al121 demonstrated a role for Fyn kinase in tau mediated Aβ neurotoxicity in APP23 mice. As Fyn is elevated in the AD brain,122 studies of Fyn overexpression were conducted and showed that overexpressed Fyn exacerbated the synaptic deficits in hAPP (K769N, M671L, V717F) Tg mice, while Fyn depletion reduced the synaptic deficits.123 These Aβ/Fyn induced synaptic and cognitive impairments were dependent on tau expression levels.124 Importantly, Hoover et al125 demonstrated that hyperphosphorylation of tau played a critical role in the mislocalisation of tau to postsynaptic dendritic spines. This caused accumulation of hyperphosphorylated tau within these spines, which can disrupt synaptic function directly and also enhance Aβ/Fyn induced synaptic dysfunction. These findings raise the intriguing possibility of targeting Fyn for the treatment of tauopathies, including AD. They also indicate that tau downregulation might be a therapeutic target, but other studies showing deleterious effects of doing this raise a serious note of caution in taking this approach.119,120 Moreover, a recent study in a cross between homozygous 3×Tg-AD mice and Fyn knockout mice (Fyn(+/−)3×Tg(+/−), 30–60% Fyn reduction) demonstrated inconsistent results. The level of soluble Aβ1–40 was increased in 15–18 month old female Fyn(+/−)3×Tg(+/−) mice, but not in 24 month old mice, whereas in male mice, the level was increased only at 21 months. The level of insoluble Aβ1–40 was almost unchanged except in 21 month old female Fyn(+/−)3×Tg(+/−) mice, which showed a slight increase. Soluble Aβ1–42 levels were not significantly altered at any age. Phosphorylated tau levels were decreased only in 15 month old female mice, but were increased in 24 month old male and female mice. Morris water maze testing at the age of 18 months demonstrated more impaired learning performance in Fyn(+/−)3×Tg(+/−) mice.126
Concerning the effects of a reduction in tau expression levels in tauopathy mouse models, several studies using regulatable mouse models of tauopathies have demonstrated that switching off pathological tau expression leads to recovery of synaptic plasticity, memory impairment and loss of long term potentiation, while neuronal loss was still present and NFTs continued to accumulate.127–129 This indicates that reversal of tau overexpression or enforcing degradation of soluble tau, including misfolded and oligomeric tau (not NFTs), has beneficial effects but this is in the context of tau overexpression which does not reduce the levels of endogenous tau. Hence this is distinctly different from targeting a reduction in normal tau levels for the treatment of AD or related tauopathies wherein there is no evidence for increased levels of tau expression in the disease state.
Inhibition of tau pathology propagation
The concept that AD Aβ pathology can be transmitted from injections of AD brain lysates was first demonstrated in primate by Baker et al,130,131 but this could not be replicated with injections of purified AD PHF tau proteins into non-Tg rat brains.132 However, more recently it was shown that tau pathology can propagate in a cell to cell manner.32 Briefly, brain extracts from P301S mutant human tau Tg mice, which show NFT formation, were injected into the brains of WT human tau Tg mice (ALZ17), which show tau accumulation but no NFT formation. Interestingly, NFTs developed in the brains of ALZ17 mice with the tau pathology spreading along neuronal connections, even to the contralateral non-injected hemisphere, and these NFTs consisted of WT human tau. Additionally, injections of brain extracts from P301S Tg mice into the brains of non-Tg WT mice also induced tau fibril formation.32 These observations indicate that extracellular tau aggregates enter cells and gain access to the cytoplasm where they corrupt the normal endogenous tau and initiate tau fibrillisation following a templated nucleation or seeding process. Secretion and ingestion of tau in cells have been documented in in vitro cell culture systems. Tau aggregates added to the culture medium were taken up by multipotent C17.2 neural stem cells, and these aggregates induced fibrillisation of intracellular tau. Co-culture of C17.2 cells with tau aggregates and C17.2 cells without tau aggregates led to an increase in the numbers of tau aggregate positive cells, indicating the transfer of tau aggregates from cell to cell.29 In another model system, tau fibrils delivered into WT tau expressing cells rapidly recruited large amounts of soluble tau into filamentous inclusions resembling NFTs, and these NFT-like tau aggregates counteracted MT overstabilisation in this cell model due to tau overexpression, thereby indicating that NFT formation might reduce MT stabilisation by recruiting away critical amounts of tau bound to MTs.31 If the hypothesis that tau pathology can spread from cell to cell and facilitates disease progression through extracellular tau aggregates is correct, removal or degradation of extracellular tau aggregates should be a promising therapeutic approach. Indeed, some studies have indicated that tau antibodies decrease tau pathology.
Tau immunisation
Studies of tau immunotherapy appear increasingly promising based on a number of studies conducted in tau Tg mouse models. Five papers describing active immunisation with tau and two papers describing passive immunisation have been published. The data are summarised in table 1. An early study indicated that immunisation of female C57BL/6 mice with full length recombinant tau resulted in neurological deficits with an NFT-like morphology, axonal damage, gliosis and mononuclear infiltration.133 This suggested that an immunisation targeting normal tau could damage neurons and might induce encephalitis. Although other studies cited here used antibodies specific to phosphorylated tau for active immunisation, Asuni et al134 reported that autoantibodies recognising recombinant tau, but not the immunogen, were detected, and that those antibodies decorated neuronal cell bodies and processes. Bi et al135 reported astrogliosis in old but not young immunised pR5 mice. Given the discussion above of the ability of tau to transmit disease, active immunisation strategies carry the risk of transmitting a tauopathy, as has been shown with the peripheral administration of Aβ.136 Thus it would seem that a passive immunisation protocol may be a better therapeutic approach than an active one.
Table 1.
Immunotherapies targeting tau in tauopathy mouse models
| Immunisation | Active
|
Passive
|
|||||
|---|---|---|---|---|---|---|---|
| Asuni et al134 | Boutajangout et al156 | Boinel et al157 | Bi et al135 | Troquier et al158 | Boutajangout et al159 | Chi et al160 | |
| Target peptides/antibody | Tau 378–408 (p396/404), monthly for 8 months | Tau 378–408 (p396/404), first three injections every 2 weeks followed by monthly intervals for 4 months | Tau 195–213 (P202/205), Tau 207–220 (p212/214), Tau 224–238 (p231). An additional injection 1 week later | Tau 395–406(P396/404). An additional injection 2 or 4 weeks later | 417–407(p422), 420–426(p422). First two injections every 2 weeks, followed by monthly intervals for 18 weeks | PHF1 (a monoclonal antibody to p396/404), 250 μg/125 μl ip once a week for 13 weeks | PHF1 or MC1 (a conformation dependent antibody), 15 mg/kg 3 times a week for 2 months and then 10 mg/kg twice a week for 2 months for JNPL3; 15 mg/kg twice a week for P301S |
| Adjuvant | Aluminum adjuvant | Aluminum adjuvant | Complete Freund adjuvant with pertussis toxin | Complete or incomplete Freund’s adjuvant | Complete or incomplete Freund’s adjuvant | ||
| Mouse | JNPL3 (P301L mutant tau Tg mice)161 | htau model (six isoforms of human tau)162 X PS M146L163 X mouse tau KO | K257T/P301S double mutant Tg mice164 | pR5 mice P301L165 | THY-Tau22166 | JNPL3161 | JNPL3,161 P301S167 |
| Onset of tau pathology (age) | 3 months | ? | 6 months | 3 months | 3 months | ~3 months | JNPL3, ~3 months; P301S, 2 months168 |
| Initiation of therapy (age) | 2 months | 3–4 months | 4 months | 4, 8, 18 months | 15 weeks | 9–12 weeks | 2 months |
| Age of sacrifice | 5 or 8 months | 8–9 months | 12 months | 4→14, 8→17, 18→24 | 36 weeks | 6–7 months | 6 months |
| Pathological changes after treatment | % of PHF1 or MC1 positive neurones was decreased | % of PHF1 or AT8 positive neurones was decreased | NFT burden (Gallyas-positive, AT8 positive and AT180 positive cells) was decreased | PHF1 and pS422 immunofluorescent intensities and Gallyas positive neurones were decreased | % of pS422 or AT100 positive neurones in CA1 was slightly reduced. % of AT8 positive neurones was slightly increased | 58% less tau pathology in the dentate gyrus | Tau pathology in the brain stem and the spinal cord was reduced in P301S mice |
| Biochemical changes after treatment | Insoluble p-tau was decreased, but soluble p-tau was increased | Soluble PHF1 tau was significantly decreased, but tau solubility was not affected | AT100 and pS422 positive insoluble tau was decreased | The levels of insoluble tau labelled with PHF1 or CP13 reduced | In JNPL3 and P301S mice, insoluble tau level was decreased | ||
| Cognitive/behavioural changes after treatment | Improvements in Rota-rod, transverse beam test and the maximum velocity in the locomotor test | Improvements in radial arm maze and closed field symmetrical maze object recognition correlated well with reduction in PHF1stained tau aggregates | Improvement in Y maze test | Improvement in traverse beam test | Improvement in Rota rod test | ||
| Other | Age dependent autoantibodies that recognised recombinant tau but not the immunogen were detected | Microgliosis an astrogliosis were unchanged | No differences in parameters of cell infiltrates and axonal damage | Tau immunisation induced astrogliosis in old, but not young pR5 mice | Tau concentration in blood was increased | Microgliosis and astrogliosis were unchanged | Attenuation of body weight loss and delay in onset of weight loss in P301S mice |
ip, intraperitoneal; NFT, neurofibrillary tangle; PHF, paired helical filament.
The mechanisms by which tau directed antibodies ameliorate tau pathology and its related neurodegeneration are unclear. One possible explanation is that they inhibit transmission of tau pathology from cell to cell. Recently, using a co-culture system, Kfoury et al137 reported that an anti-tau monoclonal antibody blocked tau aggregate propagation by trapping fibrils in the extracellular space, preventing their uptake in a dose dependent manner; interestingly, the antibody did not affect intracellular aggregation. However, it also is possible that tau antibodies can enter neurones and decrease intracellular tau aggregates. Alternatively, it is possible that a reduction in the levels of extra-cellular tau using tau antibodies for passive immunisation might facilitate the release of intracellular tau from cells, causing the reduction in cytosolic tau concentration.138
Attenuation of inflammation
It is well known that the inflammatory response plays an important role in AD139,140 and other tauopathies,141,142 and that a chronic inflammatory state, including diabetes mellitus, hypertension and periodontitis, is a risk factor for AD.143 Aβ deposition is considered to be an important inducer of the chronic inflammatory response.144 A relationship between NFT burden and microglial activation has also been demonstrated.145,146 The numbers of interleukin 1α positive microglia and S100β positive astrocytes progressively increased with NFT load in the AD brain.147 Additionally, microglial activation linked to tau deposition has been demonstrated in various tau Tg mice.148–152 Interestingly, microglial activation precedes NFT formation, and administration of an immunosuppressant, FK506, ameliorates microgliosis and tau pathology in a P301S mutant tau Tg mouse model.152 Several clinical trials targeting inflammation have been conducted. Clinical trials evaluating the use of non-steroidal anti-inflammatory drugs and cyclooxygenase 2 inhibitors in AD patients have been disappointing, except for a small beneficial effect on reduced AD incidence.153 A single centre, open label, small group study indicated that pre-spinal injection of etanercept, a tumour necrosis factor inhibitor used for treatment of rheumatoid arthritis, improved cognition in AD patients.154 A phase II, double blind, placebo controlled study of etanercept in AD patients is ongoing (http://clinicaltrials.gov/ct2/show/NCT01068353).
CONCLUSION
Although extensive basic and clinical research investigating the amyloid cascade hypothesis has been conducted and published since the discovery of Aβ by Glenner and Wong nearly 30 years ago,155 this hypothesis still remains to be proven, although no findings to date can clearly negate the amyloid cascade hypothesis. However, in terms of therapeutic development, clinical trials in symptomatic AD patients aimed at removal of Aβ load or suppression of Aβ production in the brain have failed to show any significant clinical efficacy, despite evidence of reducing the Aβ load. Under these circumstances tau, the protein building block of NFTs in AD and related tauopathies, is receiving more attention as a therapeutic target for these disorders. Recent studies have indicated the critical importance of tau in the pathomechanisms of neurodegeneration in AD and related tauopathies, including loss of the physiological functions of tau and gains of pathological functions by tau in AD and other tauopathies. Tau plays an important role in maintaining MT functions in neurons, and either a reduction or increase in tau binding to MTs can lead to impaired axonal transport. Tau might also regulate Aβ induced neurotoxicity and tau oligomers and fibrils could both be the toxic species of tau in the disease state. Tau pathology might expand along neuronal circuits via synaptic transmission. This can explain the topographical expansion of tau pathology from the mesial temporal cortices to the neocortices, and the distribution and expansion of tau pathology may reflect symptoms starting with memory impairments followed by other cognitive deficits such as aphasia, apraxia and agnosia in AD patients. Thus it is hoped that the increasing focus on tau as a target for drug discovery for AD and related tauopathies will culminate in effective disease modifying therapies in the near future.
Acknowledgments
Funding This work was supported by a Grant-in-Aid for Scientific Research (C) grant No 22590948.
Footnotes
Contributors YY designed the draft paper. All authors reviewed the literature included in the paper. All authors were involved in drafting the paper and approved the version to be published. VMYL and JQT revised the draft paper. YY designed the artwork.
Competing interests None.
Provenance and peer reviewed Commissioned; externally peer reviewed.
References
- 1.Alzheimer’s Disease International WHO. Dementia: a public health priority. 2012 [Google Scholar]
- 2.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353–6. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 3.Tiraboschi P, Sabbagh MN, Hansen LA, et al. Alzheimer disease without neocortical neurofibrillary tangles: “a second look”. Neurology. 2004;62:1141–7. doi: 10.1212/01.wnl.0000118212.41542.e7. [DOI] [PubMed] [Google Scholar]
- 4.Delacourte A, David JP, Sergeant N, et al. The biochemical pathway of neurofibrillary degeneration in aging and Alzheimer’s disease. Neurology. 1999;52:1158–65. doi: 10.1212/wnl.52.6.1158. [DOI] [PubMed] [Google Scholar]
- 5.Nelson PT, Alafuzoff I, Bigio EH, et al. Correlation of Alzheimer disease neuropathologic changes with cognitive status: a review of the literature. J Neuropathol Exp Neurol. 2012;71:362–81. doi: 10.1097/NEN.0b013e31825018f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bateman RJ, Xiong C, Benzinger TL, et al. Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N Engl J Med. 2012;367:795–804. doi: 10.1056/NEJMoa1202753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging. 1997;18:351–7. doi: 10.1016/s0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- 8.Braak H, Del Tredici K. The pathological process underlying Alzheimer’s disease in individuals under thirty. Acta Neuropathol. 2011;121:171–81. doi: 10.1007/s00401-010-0789-4. [DOI] [PubMed] [Google Scholar]
- 9.Elobeid A, Soininen H, Alafuzoff I. Hyperphosphorylated tau in young and middle-aged subjects. Acta Neuropathol. 2012;123:97–104. doi: 10.1007/s00401-011-0906-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duyckaerts C. Tau pathology in children and young adults: can you still be unconditionally baptist? Acta Neuropathol. 2011;121:145–7. doi: 10.1007/s00401-010-0794-7. [DOI] [PubMed] [Google Scholar]
- 11.Sheline YI, Morris JC, Snyder AZ, et al. APOE4 allele disrupts resting state fMRI connectivity in the absence of amyloid plaques or decreased CSF Abeta42. J Neurosci. 2010;30:17035–40. doi: 10.1523/JNEUROSCI.3987-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ewers M, Sperling RA, Klunk WE, et al. Neuroimaging markers for the prediction and early diagnosis of Alzheimer’s disease dementia. Trends Neurosci. 2011;34:430–42. doi: 10.1016/j.tins.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koch W, Teipel S, Mueller S, et al. Diagnostic power of default mode network resting state fMRI in the detection of Alzheimer’s disease. Neurobiol Aging. 2012;33:466–78. doi: 10.1016/j.neurobiolaging.2010.04.013. [DOI] [PubMed] [Google Scholar]
- 14.Prvulovic D, Bokde AL, Faltraco F, et al. Functional magnetic resonance imaging as a dynamic candidate biomarker for Alzheimer’s disease. Prog Neurobiol. 2011;95:557–69. doi: 10.1016/j.pneurobio.2011.05.008. [DOI] [PubMed] [Google Scholar]
- 15.Holmes C, Boche D, Wilkinson D, et al. Long-term effects of Abeta42 immunisation in Alzheimer’s disease: follow-up of a randomised, placebo-controlled phase I trial. Lancet. 2008;372:216–23. doi: 10.1016/S0140-6736(08)61075-2. [DOI] [PubMed] [Google Scholar]
- 16.Green RC, Schneider LS, Amato DA, et al. Effect of tarenflurbil on cognitive decline and activities of daily living in patients with mild Alzheimer disease: a randomized controlled trial. JAMA. 2009;302:2557–64. doi: 10.1001/jama.2009.1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Braak H, Braak E. Evolution of the neuropathology of Alzheimer’s disease. Acta Neurol Scand Suppl. 1996;165:3–12. doi: 10.1111/j.1600-0404.1996.tb05866.x. [DOI] [PubMed] [Google Scholar]
- 18.Oddo S, Billings L, Kesslak JP, et al. Abeta immunotherapy leads to clearance of early, but not late, hyperphosphorylated tau aggregates via the proteasome. Neuron. 2004;43:321–32. doi: 10.1016/j.neuron.2004.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Oddo S, Vasilevko V, Caccamo A, et al. Reduction of soluble Abeta and tau, but not soluble Abeta alone, ameliorates cognitive decline in transgenic mice with plaques and tangles. J Biol Chem. 2006;281:39413–23. doi: 10.1074/jbc.M608485200. [DOI] [PubMed] [Google Scholar]
- 20.Goedert M, Spillantini MG, Potier MC, et al. Cloning and sequencing of the cDNA encoding an isoform of microtubule-associated protein tau containing four tandem repeats: differential expression of tau protein mRNAs in human brain. EMBO J. 1989;8:393–9. doi: 10.1002/j.1460-2075.1989.tb03390.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Neve RL, Harris P, Kosik KS, et al. Identification of cDNA clones for the human microtubule-associated protein tau and chromosomal localization of the genes for tau and microtubule-associated protein 2. Brain Res. 1986;387:271–80. doi: 10.1016/0169-328x(86)90033-1. [DOI] [PubMed] [Google Scholar]
- 22.Kosik KS, Orecchio LD, Bakalis S, et al. Developmentally regulated expression of specific tau sequences. Neuron. 1989;2:1389–97. doi: 10.1016/0896-6273(89)90077-9. [DOI] [PubMed] [Google Scholar]
- 23.Dixit R, Ross JL, Goldman YE, et al. Differential regulation of dynein and kinesin motor proteins by tau. Science. 2008;319:1086–9. doi: 10.1126/science.1152993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hong M, Zhukareva V, Vogelsberg-Ragaglia V, et al. Mutation-specific functional impairments in distinct tau isoforms of hereditary FTDP-17. Science. 1998;282:1914–17. doi: 10.1126/science.282.5395.1914. [DOI] [PubMed] [Google Scholar]
- 25.Wang JZ, Xia YY, Grundke-Iqbal I, et al. Abnormal hyperphosphorylation of tau: sites, regulation, and molecular mechanism of neurofibrillary degeneration. J Alzheimers Dis. 2013;33 (Suppl 1):S123–39. doi: 10.3233/JAD-2012-129031. [DOI] [PubMed] [Google Scholar]
- 26.Alonso A, Zaidi T, Novak M, et al. Hyperphosphorylation induces self-assembly of tau into tangles of paired helical filaments/straight filaments. Proc Natl Acad Sci USA. 2001;98:6923–8. doi: 10.1073/pnas.121119298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.de Calignon A, Fox LM, Pitstick R, et al. Caspase activation precedes and leads to tangles. Nature. 2010;464:1201–4. doi: 10.1038/nature08890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin WL, Dickson DW, Sahara N. Immunoelectron microscopic and biochemical studies of caspase-cleaved tau in a mouse model of tauopathy. J Neuropathol Exp Neurol. 2011;70:779–87. doi: 10.1097/NEN.0b013e31822ac9c9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Frost B, Jacks RL, Diamond MI. Propagation of tau misfolding from the outside to the inside of a cell. J Biol Chem. 2009;284:12841–52. doi: 10.1074/jbc.M808759200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santa-Maria I, Varghese M, Ksiezak-Reding H, et al. Paired helical filaments from Alzheimer’s disease brain induce intracellular accumulation of tau in aggresomes. J Biol Chem. 2012;287:20522–33. doi: 10.1074/jbc.M111.323279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo JL, Lee VM. Seeding of normal tau by pathological tau conformers drives pathogenesis of Alzheimer-like tangles. J Biol Chem. 2011;286:15317–31. doi: 10.1074/jbc.M110.209296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Clavaguera F, Bolmont T, Crowther RA, et al. Transmission and spreading of tauopathy in transgenic mouse brain. Nat Cell Biol. 2009;11:909–13. doi: 10.1038/ncb1901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Calignon A, Polydoro M, Suarez-Calvet M, et al. Propagation of tau pathology in a model of early Alzheimer’s disease. Neuron. 2012;73:685–97. doi: 10.1016/j.neuron.2011.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liu L, Drouet V, Wu JW, et al. Trans-synaptic spread of tau pathology in vivo. PLoS ONE. 2012;7:e31302. doi: 10.1371/journal.pone.0031302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cash AD, Aliev G, Siedlak SL, et al. Microtubule reduction in Alzheimer’s disease and aging is independent of tau filament formation. Am J Pathol. 2003;162:1623–7. doi: 10.1016/s0002-9440(10)64296-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Stokin GB, Lillo C, Falzone TL, et al. Axonopathy and transport deficits early in the pathogenesis of Alzheimer’s disease. Science. 2005;307:1282–8. doi: 10.1126/science.1105681. [DOI] [PubMed] [Google Scholar]
- 37.Ishihara T, Hong M, Zhang B, et al. Age-dependent emergence and progression of a tauopathy in transgenic mice overexpressing the shortest human tau isoform. Neuron. 1999;24:751–62. doi: 10.1016/s0896-6273(00)81127-7. [DOI] [PubMed] [Google Scholar]
- 38.Zhang B. Microtubule-binding drugs offset tau sequestration by stabilizing microtubules and reversing fast axonal transport deficits in a tauopathy model. Proc Natl Acad Sci USA. 2005;102:227–31. doi: 10.1073/pnas.0406361102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang B, Carroll J, Trojanowski JQ, et al. The microtubule-stabilizing agent, epothilone D, reduces axonal dysfunction, neurotoxicity, cognitive deficits, and Alzheimer-like pathology in an interventional study with aged tau transgenic mice. J Neurosci. 2012;32:3601–11. doi: 10.1523/JNEUROSCI.4922-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brunden KR, Zhang B, Carroll J, et al. Epothilone D improves microtubule density, axonal integrity, and cognition in a transgenic mouse model of tauopathy. J Neurosci. 2010;30:13861–6. doi: 10.1523/JNEUROSCI.3059-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barten DM, Fanara P, Andorfer C, et al. Hyperdynamic microtubules, cognitive deficits, and pathology are improved in tau transgenic mice with low doses of the microtubule-stabilizing agent BMS-241027. J Neurosci. 2012;32:7137–45. doi: 10.1523/JNEUROSCI.0188-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bassan M, Zamostiano R, Davidson A, et al. Complete sequence of a novel protein containing a femtomolar-activity-dependent neuroprotective peptide. J Neurochem. 1999;72:1283–93. doi: 10.1046/j.1471-4159.1999.0721283.x. [DOI] [PubMed] [Google Scholar]
- 43.Gold M, Lorenzl S, Stewart AJ, et al. Critical appraisal of the role of davunetide in the treatment of progressive supranuclear palsy. Neuropsychiatr Dis Treat. 2012;8:85–93. doi: 10.2147/NDT.S12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yenjerla M, LaPointe NE, Lopus M, et al. The neuroprotective peptide NAP does not directly affect polymerization or dynamics of reconstituted neural microtubules. J Alzheimers dis. 2010;19:1377–86. doi: 10.3233/JAD-2010-1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hanger DP, Anderton BH, Noble W. Tau phosphorylation: the therapeutic challenge for neurodegenerative disease. Trends Mol Med. 2009;15:112–19. doi: 10.1016/j.molmed.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Pei JJ, Grundke-Iqbal I, Iqbal K, et al. Accumulation of cyclin-dependent kinase 5 (cdk5) in neurons with early stages of Alzheimer’s disease neurofibrillary degeneration. Brain Res. 1998;797:267–77. doi: 10.1016/s0006-8993(98)00296-0. [DOI] [PubMed] [Google Scholar]
- 47.Pei JJ, Braak E, Braak H, et al. Distribution of active glycogen synthase kinase 3beta (GSK-3beta) in brains staged for Alzheimer disease neurofibrillary changes. J Neuropathol Exp Neurol. 1999;58:1010–19. doi: 10.1097/00005072-199909000-00011. [DOI] [PubMed] [Google Scholar]
- 48.Kremer A, Louis JV, Jaworski T, et al. GSK3 and Alzheimer’s disease: facts and fiction. Front Mol Neurosci. 2011;4:17. doi: 10.3389/fnmol.2011.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Doble BW, Woodgett JR. GSK-3: tricks of the trade for a multi-tasking kinase. J Cell Sci. 2003;116:1175–86. doi: 10.1242/jcs.00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jope RS, Johnson GV. The glamour and gloom of glycogen synthase kinase-3. Trends Biochem Sci. 2004;29:95–102. doi: 10.1016/j.tibs.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 51.Giese KP. GSK-3: a key player in neurodegeneration and memory. IUBMB Life. 2009;61:516–21. doi: 10.1002/iub.187. [DOI] [PubMed] [Google Scholar]
- 52.Hurtado DE, Molina-Porcel L, Carroll JC, et al. Selectively silencing GSK-3 isoforms reduces plaques and tangles in mouse models of Alzheimer’s disease. J Neurosci. 2012;32:7392–402. doi: 10.1523/JNEUROSCI.0889-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Takashima A, Noguchi K, Sato K, et al. Tau protein kinase I is essential for amyloid beta-protein-induced neurotoxicity. Proc Natl Acad Sci USA. 1993;90:7789–93. doi: 10.1073/pnas.90.16.7789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Takashima A, Noguchi K, Michel G, et al. Exposure of rat hippocampal neurons to amyloid beta peptide (25–35) induces the inactivation of phosphatidyl inositol-3 kinase and the activation of tau protein kinase I/glycogen synthase kinase-3 beta. Neurosci Lett. 1996;203:33–6. doi: 10.1016/0304-3940(95)12257-5. [DOI] [PubMed] [Google Scholar]
- 55.Hoshi M, Sato M, Matsumoto S, et al. Spherical aggregates of beta-amyloid (amylospheroid) show high neurotoxicity and activate tau protein kinase I/glycogen synthase kinase-3beta. Proc Natl Acad Sci USA. 2003;100:6370–5. doi: 10.1073/pnas.1237107100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aplin AE, Gibb GM, Jacobsen JS, et al. In vitro phosphorylation of the cytoplasmic domain of the amyloid precursor protein by glycogen synthase kinase-3beta. J Neurochem. 1996;67:699–707. doi: 10.1046/j.1471-4159.1996.67020699.x. [DOI] [PubMed] [Google Scholar]
- 57.Twomey C, McCarthy JV. Presenilin-1 is an unprimed glycogen synthase kinase-3beta substrate. FEBS Lett. 2006;580:4015–20. doi: 10.1016/j.febslet.2006.06.035. [DOI] [PubMed] [Google Scholar]
- 58.Phiel CJ, Wilson CA, Lee VM, et al. GSK-3alpha regulates production of Alzheimer’s disease amyloid-beta peptides. Nature. 2003;423:435–9. doi: 10.1038/nature01640. [DOI] [PubMed] [Google Scholar]
- 59.Ma QL, Lim GP, Harris-White ME, et al. Antibodies against beta-amyloid reduce Abeta oligomers, glycogen synthase kinase-3beta activation and tau phosphorylation in vivo and in vitro. J Neurosci Res. 2006;83:374–84. doi: 10.1002/jnr.20734. [DOI] [PubMed] [Google Scholar]
- 60.Engel T, Lucas JJ, Gomez-Ramos P, et al. Cooexpression of FTDP-17 tau and GSK-3beta in transgenic mice induce tau polymerization and neurodegeneration. Neurobiol Aging. 2006;27:1258–68. doi: 10.1016/j.neurobiolaging.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 61.Engel T, Goni-Oliver P, Lucas JJ, et al. Chronic lithium administration to FTDP-17 tau and GSK-3beta overexpressing mice prevents tau hyperphosphorylation and neurofibrillary tangle formation, but pre-formed neurofibrillary tangles do not revert. J Neurochem. 2006;99:1445–55. doi: 10.1111/j.1471-4159.2006.04139.x. [DOI] [PubMed] [Google Scholar]
- 62.Leroy K, Ando K, Heraud C, et al. Lithium treatment arrests the development of neurofibrillary tangles in mutant tau transgenic mice with advanced neurofibrillary pathology. J Alzheimers Dis. 2010;19:705–19. doi: 10.3233/JAD-2010-1276. [DOI] [PubMed] [Google Scholar]
- 63.Nakashima H, Ishihara T, Suguimoto P, et al. Chronic lithium treatment decreases tau lesions by promoting ubiquitination in a mouse model of tauopathies. Acta Neuropathol. 2005;110:547–56. doi: 10.1007/s00401-005-1087-4. [DOI] [PubMed] [Google Scholar]
- 64.Noble W, Planel E, Zehr C, et al. Inhibition of glycogen synthase kinase-3 by lithium correlates with reduced tauopathy and degeneration in vivo. Proc Natl Acad Sci USA. 2005;102:6990–5. doi: 10.1073/pnas.0500466102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Perez M, Hernandez F, Lim F, et al. Chronic lithium treatment decreases mutant tau protein aggregation in a transgenic mouse model. J Alzheimers Dis. 2003;5:301–8. doi: 10.3233/jad-2003-5405. [DOI] [PubMed] [Google Scholar]
- 66.Shimada K, Motoi Y, Ishiguro K, et al. Long-term oral lithium treatment attenuates motor disturbance in tauopathy model mice: implications of autophagy promotion. Neurobiol Dis. 2012;46:101–8. doi: 10.1016/j.nbd.2011.12.050. [DOI] [PubMed] [Google Scholar]
- 67.Macdonald A, Briggs K, Poppe M, et al. A feasibility and tolerability study of lithium in Alzheimer’s disease. Int J Geriatr Psychiatry. 2008;23:704–11. doi: 10.1002/gps.1964. [DOI] [PubMed] [Google Scholar]
- 68.Hampel H, Ewers M, Burger K, et al. Lithium trial in Alzheimer’s disease: a randomized, single-blind, placebo-controlled, multicenter 10-week study. J Clin Psychiatry. 2009;70:922–31. [PubMed] [Google Scholar]
- 69.Forlenza OV, Diniz BS, Radanovic M, et al. Disease-modifying properties of long-term lithium treatment for amnestic mild cognitive impairment: randomised controlled trial. Br J Psychiatry. 2011;198:351–6. doi: 10.1192/bjp.bp.110.080044. [DOI] [PubMed] [Google Scholar]
- 70.Onishi T, Iwashita H, Uno Y, et al. A novel glycogen synthase kinase-3 inhibitor 2-methyl-5-(3-{4-((S)-methylsulfinyl)phenyl}-1-benzofuran-5-yl)-1,3,4-oxadiazole decreases tau phosphorylation and ameliorates cognitive deficits in a transgenic model of Alzheimer’s disease. J Neurochem. 2011;119:1330–40. doi: 10.1111/j.1471-4159.2011.07532.x. [DOI] [PubMed] [Google Scholar]
- 71.Le Corre S, Klafki HW, Plesnila N, et al. An inhibitor of tau hyperphosphorylation prevents severe motor impairments in tau transgenic mice. Proc Natl Acad Sci USA. 2006;103:9673–8. doi: 10.1073/pnas.0602913103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sereno L, Coma M, Rodriguez M, et al. A novel GSK-3beta inhibitor reduces Alzheimer’s pathology and rescues neuronal loss in vivo. Neurobiol Dis. 2009;35:359–67. doi: 10.1016/j.nbd.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 73.Gong CX, Singh TJ, Grundke-Iqbal I, et al. Phosphoprotein phosphatase activities in Alzheimer disease brain. J Neurochem. 1993;61:921–7. doi: 10.1111/j.1471-4159.1993.tb03603.x. [DOI] [PubMed] [Google Scholar]
- 74.Gong CX, Shaikh S, Wang JZ, et al. Phosphatase activity toward abnormally phosphorylated tau: decrease in Alzheimer disease brain. J Neurochem. 1995;65:732–8. doi: 10.1046/j.1471-4159.1995.65020732.x. [DOI] [PubMed] [Google Scholar]
- 75.Vogelsberg-Ragaglia V, Schuck T, Trojanowski JQ, et al. PP2A mRNA expression is quantitatively decreased in Alzheimer’s disease hippocampus. Exp Neurol. 2001;168:402–12. doi: 10.1006/exnr.2001.7630. [DOI] [PubMed] [Google Scholar]
- 76.Matsuo ES, Shin RW, Billingsley ML, et al. Biopsy-derived adult human brain tau is phosphorylated at many of the same sites as Alzheimer’s disease paired helical filament tau. Neuron. 1994;13:989–1002. doi: 10.1016/0896-6273(94)90264-x. [DOI] [PubMed] [Google Scholar]
- 77.Bennecib M, Gong CX, Grundke-Iqbal I, et al. Inhibition of PP-2A upregulates CaMKII in rat forebrain and induces hyperphosphorylation of tau at Ser 262/356. FEBS Lett. 2001;490:15–22. doi: 10.1016/s0014-5793(01)02127-5. [DOI] [PubMed] [Google Scholar]
- 78.Gong CX, Lidsky T, Wegiel J, et al. Phosphorylation of microtubule-associated protein tau is regulated by protein phosphatase 2A in mammalian brain. Implications for neurofibrillary degeneration in Alzheimer’s disease. J Biol Chem. 2000;275:5535–44. doi: 10.1074/jbc.275.8.5535. [DOI] [PubMed] [Google Scholar]
- 79.Liu F, Grundke-Iqbal I, Iqbal K, et al. Contributions of protein phosphatases PP1, PP2A, PP2B and PP5 to the regulation of tau phosphorylation. Eur J Neurosci. 2005;22:1942–50. doi: 10.1111/j.1460-9568.2005.04391.x. [DOI] [PubMed] [Google Scholar]
- 80.Xu Y, Chen Y, Zhang P, et al. Structure of a protein phosphatase 2A holoenzyme: insights into B55-mediated Tau dephosphorylation. Mol Cell. 2008;31:873–85. doi: 10.1016/j.molcel.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Voronkov M, Braithwaite SP, Stock JB. Phosphoprotein phosphatase 2A: a novel druggable target for Alzheimer’s disease. Future Med Chem. 2011;3:821–33. doi: 10.4155/fmc.11.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kim JM, Stewart R, Kim SW, et al. Changes in folate, vitamin B12 and homocysteine associated with incident dementia. J Neurol Neurosurg Psychiatry. 2008;79:864–8. doi: 10.1136/jnnp.2007.131482. [DOI] [PubMed] [Google Scholar]
- 83.Shea TB, Lyons-Weiler J, Rogers E. Homocysteine, folate deprivation and Alzheimer neuropathology. J Alzheimers Dis. 2002;4:261–7. doi: 10.3233/jad-2002-4401. [DOI] [PubMed] [Google Scholar]
- 84.Sontag E, Nunbhakdi-Craig V, Sontag JM, et al. Protein phosphatase 2A methyltransferase links homocysteine metabolism with tau and amyloid precursor protein regulation. J Neurosci. 2007;27:2751–9. doi: 10.1523/JNEUROSCI.3316-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sontag JM, Nunbhakdi-Craig V, Montgomery L, et al. Folate deficiency induces in vitro and mouse brain region-specific downregulation of leucine carboxyl methyltransferase-1 and protein phosphatase 2A B(alpha) subunit expression that correlate with enhanced tau phosphorylation. J Neurosci. 2008;28:11477–87. doi: 10.1523/JNEUROSCI.2816-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Chohan MO, Khatoon S, Iqbal IG, et al. Involvement of I2PP2A in the abnormal hyperphosphorylation of tau and its reversal by Memantine. FEBS Lett. 2006;580:3973–9. doi: 10.1016/j.febslet.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 87.Degerman Gunnarsson M, Kilander L, Basun H, et al. Reduction of phosphorylated tau during memantine treatment of Alzheimer’s disease. Dement Geriatr Cogn Disord. 2007;24:247–52. doi: 10.1159/000107099. [DOI] [PubMed] [Google Scholar]
- 88.Pennanen L, Welzl H, D’Adamo P, et al. Accelerated extinction of conditioned taste aversion in P301L tau transgenic mice. Neurobiol Dis. 2004;15:500–9. doi: 10.1016/j.nbd.2003.11.020. [DOI] [PubMed] [Google Scholar]
- 89.Ittner LM, Fath T, Ke YD, et al. Parkinsonism and impaired axonal transport in a mouse model of frontotemporal dementia. Proc Natl Acad Sci USA. 2008;105:15997–6002. doi: 10.1073/pnas.0808084105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.van Eersel J, Ke YD, Liu X, et al. Sodium selenate mitigates tau pathology, neurodegeneration, and functional deficits in Alzheimer’s disease models. Proc Natl Acad Sci USA. 2010;107:13888–93. doi: 10.1073/pnas.1009038107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Liu F, Iqbal K, Grundke-Iqbal I, et al. O-GlcNAcylation regulates phosphorylation of tau: a mechanism involved in Alzheimer’s disease. Proc Natl Acad Sci USA. 2004;101:10804–9. doi: 10.1073/pnas.0400348101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Yuzwa SA, Shan X, Macauley MS, et al. Increasing O-GlcNAc slows neurodegeneration and stabilizes tau against aggregation. Nat Chem Biol. 2012;8:393–9. doi: 10.1038/nchembio.797. [DOI] [PubMed] [Google Scholar]
- 93.Liu F, Zaidi T, Iqbal K, et al. Role of glycosylation in hyperphosphorylation of tau in Alzheimer’s disease. FEBS Lett. 2002;512:101–6. doi: 10.1016/s0014-5793(02)02228-7. [DOI] [PubMed] [Google Scholar]
- 94.Yan SD, Yan SF, Chen X, et al. Non-enzymatically glycated tau in Alzheimer’s disease induces neuronal oxidant stress resulting in cytokine gene expression and release of amyloid beta-peptide. Nat Med. 1995;1:693–9. doi: 10.1038/nm0795-693. [DOI] [PubMed] [Google Scholar]
- 95.Min SW, Cho SH, Zhou Y, et al. Acetylation of tau inhibits its degradation and contributes to tauopathy. Neuron. 2010;67:953–66. doi: 10.1016/j.neuron.2010.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Irwin DJ, Cohen TJ, Grossman M, et al. Acetylated tau, a novel pathological signature in Alzheimer’s disease and other tauopathies. Brain. 2012;135:807–18. doi: 10.1093/brain/aws013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cohen TJ, Guo JL, Hurtado DE, et al. The acetylation of tau inhibits its function and promotes pathological tau aggregation. Nat Commun. 2011;2:252. doi: 10.1038/ncomms1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reynolds MR, Reyes JF, Fu Y, et al. Tau nitration occurs at tyrosine 29 in the fibrillar lesions of Alzheimer’s disease and other tauopathies. J Neurosci. 2006;26:10636–45. doi: 10.1523/JNEUROSCI.2143-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Spires-Jones TL, Kopeikina KJ, Koffie RM, et al. Are tangles as toxic as they look? J Mol Neurosci. 2011;45:438–44. doi: 10.1007/s12031-011-9566-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bulic B, Pickhardt M, Mandelkow EM, et al. Tau protein and tau aggregation inhibitors. Neuropharmacology. 2010;59:276–89. doi: 10.1016/j.neuropharm.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 101.Crowe A, Ballatore C, Hyde E, et al. High throughput screening for small molecule inhibitors of heparin-induced tau fibril formation. Biochem Biophys Res Commun. 2007;358:1–6. doi: 10.1016/j.bbrc.2007.03.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Wischik CM, Edwards PC, Lai RY, et al. Selective inhibition of Alzheimer disease-like tau aggregation by phenothiazines. Proc Natl Acad Sci USA. 1996;93:11213–18. doi: 10.1073/pnas.93.20.11213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schirmer RH, Adler H, Pickhardt M, et al. Lest we forget you—methylene blue…. Neurobiol Aging. 2011;32:2325, e7–16. doi: 10.1016/j.neurobiolaging.2010.12.012. [DOI] [PubMed] [Google Scholar]
- 104.van Bebber F, Paquet D, Hruscha A, et al. Methylene blue fails to inhibit tau and polyglutamine protein dependent toxicity in zebrafish. Neurobiol Dis. 2010;39:265–71. doi: 10.1016/j.nbd.2010.03.023. [DOI] [PubMed] [Google Scholar]
- 105.Fatouros C, Pir GJ, Biernat J, et al. Inhibition of tau aggregation in a novel C. elegans model of tauopathy mitigates proteotoxicity. Hum Mol Genet. 2012;21:3587–603. doi: 10.1093/hmg/dds190. [DOI] [PubMed] [Google Scholar]
- 106.O’Leary JC, 3rd, Li Q, Marinec P, et al. Phenothiazine-mediated rescue of cognition in tau transgenic mice requires neuroprotection and reduced soluble tau burden. Molr Neurodegener. 2010;5:45. doi: 10.1186/1750-1326-5-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Wischik C, Staff R. Challenges in the conduct of disease-modifying trials in AD: practical experience from a phase 2 trial of tau-aggregation inhibitor therapy. J Nutr Health Aging. 2009;13:367–9. doi: 10.1007/s12603-009-0046-5. [DOI] [PubMed] [Google Scholar]
- 108.Crowe A, Huang W, Ballatore C, et al. Identification of aminothienopyridazine inhibitors of tau assembly by quantitative high-throughput screening. Biochemistry. 2009;48:7732–45. doi: 10.1021/bi9006435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Petrucelli L, Dickson D, Kehoe K, et al. CHIP and Hsp70 regulate tau ubiquitination, degradation and aggregation. Hum Mol Genet. 2004;13:703–14. doi: 10.1093/hmg/ddh083. [DOI] [PubMed] [Google Scholar]
- 110.Sahara N, Murayama M, Mizoroki T, et al. In vivo evidence of CHIP up-regulation attenuating tau aggregation. J Neurochem. 2005;94:1254–63. doi: 10.1111/j.1471-4159.2005.03272.x. [DOI] [PubMed] [Google Scholar]
- 111.Dickey CA, Yue M, Lin WL, et al. Deletion of the ubiquitin ligase CHIP leads to the accumulation, but not the aggregation, of both endogenous phospho- and caspase-3-cleaved tau species. J Neurosci. 2006;26:6985–96. doi: 10.1523/JNEUROSCI.0746-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Luo W, Dou F, Rodina A, et al. Roles of heat-shock protein 90 in maintaining and facilitating the neurodegenerative phenotype in tauopathies. Proc Natl Acad Sci USA. 2007;104:9511–16. doi: 10.1073/pnas.0701055104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chambraud B, Sardin E, Giustiniani J, et al. A role for FKBP52 in tau protein function. Proc Natl Acad Sci USA. 2010;107:2658–63. doi: 10.1073/pnas.0914957107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Berger Z, Ravikumar B, Menzies FM, et al. Rapamycin alleviates toxicity of different aggregate-prone proteins. Hum Mol Genet. 2006;15:433–42. doi: 10.1093/hmg/ddi458. [DOI] [PubMed] [Google Scholar]
- 115.Wang Y, Martinez-Vicente M, Kruger U, et al. Tau fragmentation, aggregation and clearance: the dual role of lysosomal processing. Hum Mol Genet. 2009;18:4153–70. doi: 10.1093/hmg/ddp367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Schaeffer V, Lavenir I, Ozcelik S, et al. Stimulation of autophagy reduces neurodegeneration in a mouse model of human tauopathy. Brain. 2012;135:2169–77. doi: 10.1093/brain/aws143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Dolan PJ, Johnson GV. A caspase cleaved form of tau is preferentially degraded through the autophagy pathway. J Biol Chem. 2010;285:21978–87. doi: 10.1074/jbc.M110.110940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Roberson ED, Scearce-Levie K, Palop JJ, et al. Reducing endogenous tau ameliorates amyloid beta-induced deficits in an Alzheimer’s disease mouse model. Science. 2007;316:750–4. doi: 10.1126/science.1141736. [DOI] [PubMed] [Google Scholar]
- 119.Dawson HN, Cantillana V, Jansen M, et al. Loss of tau elicits axonal degeneration in a mouse model of Alzheimer’s disease. Neuroscience. 2010;169:516–31. doi: 10.1016/j.neuroscience.2010.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Lei P, Ayton S, Finkelstein DI, et al. Tau deficiency induces parkinsonism with dementia by impairing APP-mediated iron export. Nat Med. 2012;18:291–5. doi: 10.1038/nm.2613. [DOI] [PubMed] [Google Scholar]
- 121.Ittner LM, Ke YD, Delerue F, et al. Dendritic function of tau mediates amyloid-beta toxicity in Alzheimer’s disease mouse models. Cell. 2010;142:387–97. doi: 10.1016/j.cell.2010.06.036. [DOI] [PubMed] [Google Scholar]
- 122.Shirazi SK, Wood JG. The protein tyrosine kinase, fyn, in Alzheimer’s disease pathology. Neuroreport. 1993;4:435–7. doi: 10.1097/00001756-199304000-00024. [DOI] [PubMed] [Google Scholar]
- 123.Chin J, Palop JJ, Puolivali J, et al. Fyn kinase induces synaptic and cognitive impairments in a transgenic mouse model of Alzheimer’s disease. J Neurosci. 2005;25:9694–703. doi: 10.1523/JNEUROSCI.2980-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Roberson ED, Halabisky B, Yoo JW, et al. Amyloid-beta/Fyn-induced synaptic, network, and cognitive impairments depend on tau levels in multiple mouse models of Alzheimer’s disease. J Neurosci. 2011;31:700–11. doi: 10.1523/JNEUROSCI.4152-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Hoover BR, Reed MN, Su J, et al. Tau mislocalization to dendritic spines mediates synaptic dysfunction independently of neurodegeneration. Neuron. 2010;68:1067–81. doi: 10.1016/j.neuron.2010.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Minami SS, Clifford TG, Hoe HS, et al. Fyn knock-down increases Abeta, decreases phospho-tau, and worsens spatial learning in 3×Tg-AD mice. Neurobiol Aging. 2012;33:825, e15–24. doi: 10.1016/j.neurobiolaging.2011.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Sydow A, Van der Jeugd A, Zheng F, et al. Tau-induced defects in synaptic plasticity, learning, and memory are reversible in transgenic mice after switching off the toxic Tau mutant. J Neurosci. 2011;31:2511–25. doi: 10.1523/JNEUROSCI.5245-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Van der Jeugd A, Hochgrafe K, Ahmed T, et al. Cognitive defects are reversible in inducible mice expressing pro-aggregant full-length human Tau. Acta Neuropathol. 2012;123:787–805. doi: 10.1007/s00401-012-0987-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Santacruz K, Lewis J, Spires T, et al. Tau suppression in a neurodegenerative mouse model improves memory function. Science. 2005;309:476–81. doi: 10.1126/science.1113694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Baker HF, Ridley RM, Duchen LW, et al. Evidence for the experimental transmission of cerebral beta-amyloidosis to primates. Int J Exp Pathol. 1993;74:441–54. [PMC free article] [PubMed] [Google Scholar]
- 131.Baker HF, Ridley RM, Duchen LW, et al. Induction of beta (A4)-amyloid in primates by injection of Alzheimer’s disease brain homogenate. Comparison with transmission of spongiform encephalopathy. Molecular neurobiology. 1994;8:25–39. doi: 10.1007/BF02778005. [DOI] [PubMed] [Google Scholar]
- 132.Shin RW, Bramblett GT, Lee VM, et al. Alzheimer disease A68 proteins injected into rat brain induce codeposits of beta-amyloid, ubiquitin, and alpha 1-antichymotrypsin. Proc Natl Acad Sci USA. 1993;90:6825–8. doi: 10.1073/pnas.90.14.6825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Rosenmann H, Grigoriadis N, Karussis D, et al. Tauopathy-like abnormalities and neurologic deficits in mice immunized with neuronal tau protein. Arch Neurol. 2006;63:1459–67. doi: 10.1001/archneur.63.10.1459. [DOI] [PubMed] [Google Scholar]
- 134.Asuni AA, Boutajangout A, Quartermain D, et al. Immunotherapy targeting pathological tau conformers in a tangle mouse model reduces brain pathology with associated functional improvements. J Neurosci. 2007;27:9115–29. doi: 10.1523/JNEUROSCI.2361-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Bi M, Ittner A, Ke YD, et al. Tau-targeted immunization impedes progression of neurofibrillary histopathology in aged P301L tau transgenic mice. PLoS ONE. 2011;6:e26860. doi: 10.1371/journal.pone.0026860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Eisele YS, Obermuller U, Heilbronner G, et al. Peripherally applied Abeta-containing inoculates induce cerebral beta-amyloidosis. Science. 2010;330:980–2. doi: 10.1126/science.1194516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Kfoury N, Holmes BB, Jiang H, et al. Trans-cellular propagation of tau aggregation by fibrillar species. J Biol Chem. 2012;287:19440–51. doi: 10.1074/jbc.M112.346072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Sigurdsson EM. Immunotherapy targeting pathological tau protein in Alzheimer’s disease and related tauopathies. J Alzheimers Dis. 2008;15:157–68. doi: 10.3233/jad-2008-15202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Akiyama H, Barger S, Barnum S, et al. Inflammation and Alzheimer’s disease. Neurobiol Aging. 2000;21:383–421. doi: 10.1016/s0197-4580(00)00124-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Tarkowski E, Andreasen N, Tarkowski A, et al. Intrathecal inflammation precedes development of Alzheimer’s disease. J Neurol Neurosurg Psychiatry. 2003;74:1200–5. doi: 10.1136/jnnp.74.9.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ishizawa K, Dickson DW. Microglial activation parallels system degeneration in progressive supranuclear palsy and corticobasal degeneration. J Neuropathol Exp Neurol. 2001;60:647–57. doi: 10.1093/jnen/60.6.647. [DOI] [PubMed] [Google Scholar]
- 142.Gerhard A, Trender-Gerhard I, Turkheimer F, et al. In vivo imaging of microglial activation with (11C)(R)-PK11195 PET in progressive supranuclear palsy. Mov Disord. 2006;21:89–93. doi: 10.1002/mds.20668. [DOI] [PubMed] [Google Scholar]
- 143.Profenno LA, Porsteinsson AP, Faraone SV. Meta-analysis of Alzheimer’s disease risk with obesity, diabetes, and related disorders. Biol Psychiatry. 2010;67:505–12. doi: 10.1016/j.biopsych.2009.02.013. [DOI] [PubMed] [Google Scholar]
- 144.Cameron B, Landreth GE. Inflammation, microglia, and Alzheimer’s disease. Neurobiol Dis. 2010;37:503–9. doi: 10.1016/j.nbd.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sheffield LG, Marquis JG, Berman NE. Regional distribution of cortical microglia parallels that of neurofibrillary tangles in Alzheimer’s disease. Neurosci Lett. 2000;285:165–8. doi: 10.1016/s0304-3940(00)01037-5. [DOI] [PubMed] [Google Scholar]
- 146.Cras P, Kawai M, Siedlak S, et al. Microglia are associated with the extracellular neurofibrillary tangles of Alzheimer disease. Brain Res. 1991;558:312–14. doi: 10.1016/0006-8993(91)90783-r. [DOI] [PubMed] [Google Scholar]
- 147.Sheng JG, Mrak RE, Griffin WS. Glial-neuronal interactions in Alzheimer disease: progressive association of IL-1alpha+ microglia and S100beta+ astrocytes with neurofibrillary tangle stages. J Neuropathol Exp Neurol. 1997;56:285–90. [PubMed] [Google Scholar]
- 148.Bellucci A, Westwood AJ, Ingram E, et al. Induction of inflammatory mediators and microglial activation in mice transgenic for mutant human P301S tau protein. Am J Pathol. 2004;165:1643–52. doi: 10.1016/S0002-9440(10)63421-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ikeda M, Shoji M, Kawarai T, et al. Accumulation of filamentous tau in the cerebral cortex of human tau R406W transgenic mice. Am J Pathol. 2005;166:521–31. doi: 10.1016/S0002-9440(10)62274-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sasaki A, Kawarabayashi T, Murakami T, et al. Microglial activation in brain lesions with tau deposits: comparison of human tauopathies and tau transgenic mice TgTauP301L. Brain Res. 2008;1214:159–68. doi: 10.1016/j.brainres.2008.02.084. [DOI] [PubMed] [Google Scholar]
- 151.Zilka N, Stozicka Z, Kovac A, et al. Human misfolded truncated tau protein promotes activation of microglia and leukocyte infiltration in the transgenic rat model of tauopathy. J Neuroimmunol. 2009;209:16–25. doi: 10.1016/j.jneuroim.2009.01.013. [DOI] [PubMed] [Google Scholar]
- 152.Yoshiyama Y, Higuchi M, Zhang B, et al. Synapse loss and microglial activation precede tangles in a P301S tauopathy mouse model. Neuron. 2007;53:337–51. doi: 10.1016/j.neuron.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 153.Breitner JC, Baker LD, Montine TJ, et al. Extended results of the Alzheimer’s disease anti-inflammatory prevention trial. Alzheimers Dement: J Alzheimers Assoc. 2011;7:402–11. doi: 10.1016/j.jalz.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Tobinick E, Gross H, Weinberger A, et al. TNF-alpha modulation for treatment of Alzheimer’s disease: a 6-month pilot study. Med Gen Med. 2006;8:25. [PMC free article] [PubMed] [Google Scholar]
- 155.Glenner GG, Wong CW. Alzheimer’s disease: initial report of the purification and characterization of a novel cerebrovascular amyloid protein. Biochem Biophys Res Commun. 1984;120:885–90. doi: 10.1016/s0006-291x(84)80190-4. [DOI] [PubMed] [Google Scholar]
- 156.Boutajangout A, Quartermain D, Sigurdsson EM. Immunotherapy targeting pathological tau prevents cognitive decline in a new tangle mouse model. J Neurosci. 2010;30:16559–66. doi: 10.1523/JNEUROSCI.4363-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Boimel M, Grigoriadis N, Lourbopoulos A, et al. Efficacy and safety of immunization with phosphorylated tau against neurofibrillary tangles in mice. Exp Neurol. 2010;224:472–85. doi: 10.1016/j.expneurol.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 158.Troquier L, Caillierez R, Burnouf S, et al. Targeting phospho-Ser422 by active tau immunotherapy in the THYTau22 mouse model: a suitable therapeutic approach. Curr Alzheimer Res. 2012;9:397–405. doi: 10.2174/156720512800492503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Boutajangout A, Ingadottir J, Davies P, et al. Passive immunization targeting pathological phospho-tau protein in a mouse model reduces functional decline and clears tau aggregates from the brain. J Neurochem. 2011;118:658–67. doi: 10.1111/j.1471-4159.2011.07337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chai X, Wu S, Murray TK, et al. Passive immunization with anti-Tau antibodies in two transgenic models: reduction of Tau pathology and delay of disease progression. J Biol Chem. 2011;286:34457–67. doi: 10.1074/jbc.M111.229633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Lewis J, McGowan E, Rockwood J, et al. Neurofibrillary tangles, amyotrophy and progressive motor disturbance in mice expressing mutant (P301L) tau protein. Nat Genet. 2000;25:402–5. doi: 10.1038/78078. [DOI] [PubMed] [Google Scholar]
- 162.Andorfer C, Acker CM, Kress Y, et al. Cell-cycle reentry and cell death in transgenic mice expressing nonmutant human tau isoforms. J Neurosci. 2005;25:5446–54. doi: 10.1523/JNEUROSCI.4637-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Duff K, Eckman C, Zehr C, et al. Increased amyloid-beta42(43) in brains of mice expressing mutant presenilin 1. Nature. 1996;383:710–13. doi: 10.1038/383710a0. [DOI] [PubMed] [Google Scholar]
- 164.Rosenmann H, Grigoriadis N, Eldar-Levy H, et al. A novel transgenic mouse expressing double mutant tau driven by its natural promoter exhibits tauopathy characteristics. Exp Neurol. 2008;212:71–84. doi: 10.1016/j.expneurol.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 165.Gotz J, Chen F, Barmettler R, et al. Tau filament formation in transgenic mice expressing P301L tau. J Biol Chem. 2001;276:529–34. doi: 10.1074/jbc.M006531200. [DOI] [PubMed] [Google Scholar]
- 166.Schindowski K, Bretteville A, Leroy K, et al. Alzheimer’s disease-like tau neuropathology leads to memory deficits and loss of functional synapses in a novel mutated tau transgenic mouse without any motor deficits. Am J Pathol. 2006;169:599–616. doi: 10.2353/ajpath.2006.060002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Allen B, Ingram E, Takao M, et al. Abundant tau filaments and nonapoptotic neurodegeneration in transgenic mice expressing human P301S tau protein. J Neurosci. 2002;22:9340–51. doi: 10.1523/JNEUROSCI.22-21-09340.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Delobel P, Lavenir I, Fraser G, et al. Analysis of tau phosphorylation and truncation in a mouse model of human tauopathy. Am J Pathol. 2008;172:123–31. doi: 10.2353/ajpath.2008.070627. [DOI] [PMC free article] [PubMed] [Google Scholar]