Abstract
Diabetes mellitus is a systemic disease that increases the risk of infections. Exogenous endophthalmitis is an inflammatory disease to which diabetic patients are more predisposed to than nondiabetic patients undergoing any intraocular intervention. This might be because of the change in the immune and inflammatory factors that intervene in wound healing and in the bacterial flora of the ocular adnexa. We conducted a literature review to assess the risk of exogenous endophthalmitis in diabetic patients undergoing cataract extraction, pars plana vitrectomy, and intravitreal injections and to check whether its treatment differ from in non-diabetics. We found that diabetic patients are more predisposed to virulent organisms and that the incidence of ophthalmic symptoms was not substantially different in diabetic versus nondiabetic patients. Regarding treatment, all patients with light perception should receive pars plana vitrectomy, while those with hand motion and better vision should be given an intravitreal antibiotics injection. Some authors recommend vitrectomy to diabetic patients with even counting figure vision.
1. Introduction
Infectious endophthalmitis is defined as the infestation of the intraocular compartment by microorganisms. It represents one of the most severe and potentially devastating inflammatory reactions seen in the eye and it often results in irreversible visual loss [1, 2]. Based on the site of entry of this agent, endophthalmitis can be divided into an infection of either exogenous or endogenous origin. While the former condition most commonly occurs after intraocular surgery or trauma, the latter form is believed to be linked to septicemia. Postoperative bacterial endophthalmitis is a rare, but severe complication of intraocular surgery. The infecting bacteria by replication and release of toxins can damage the intraocular structures, and the inflammatory reaction of the host seems to contribute even further to the damage [3].
Patients with diabetes mellitus (DM) known to have an impaired immune response may be at a higher risk for developing postoperative infections. Effectively at the cellular and humoral levels, there is suboptimal response to different antigens in addition to altered phagocytic capabilities [4–7]. Moreover, it is established that impaired neutrophil bactericidal function is strongly associated with poor glycemic control [8, 9]. Furthermore, the tear film, the first immunological barrier for the ocular system, is altered in patients with DM. There is documented decrease in the breakup time and an established decrease in Schirmer's test [10]. Finally, it has been demonstrated that diabetes mellitus alters the corneal epithelial basement membrane resulting in basal cell degeneration manifested clinically as a superficial punctate keratitis and breakdown of the barrier function of this front line epithelium resulting in greater fragility of the eyeball [11–17].
These deficiencies in the protective features inherent to the eye seem to all associate with the duration of the disease and the serum level of glycosylated hemoglobin HbA1c [18, 19]. Elevated levels of of glucose seem to impair epidermal growth factor receptor (EGFR) signaling and suppress basal cell multiplication and wound-induced AKT phosphorylation [20–22]. This anomaly results in delayed healing of the epithelial defect, which may be associated with sight-threatening complications, such as stromal opacities, surface irregularities, microbial keratitis, and increased risk of acute postoperative endophthalmitis due to delayed and improper wound closure [22]. Independent of all the above and with the raised levels of glucose in the skin, mucous membranes and the tear film of patients with DM, microorganisms growth seems definitely promoted.
2. Epidemiology
The reported incidence of postoperative endophthalmitis varies by the specific surgical procedure, but overall the occurrence has declined substantially in the past century. The incidence of endophthalmitis after cataract surgery has decreased from approximately 10% in the late 1800s to 0.58% in the mid-1900s to 0.09% in the early 1990s to 0.04% during the period 1995 to 2001 [1, 23–26]. Rates of endophthalmitis after conventional pars plana vitrectomy (PPV) have further decreased over the past 25 years. Since Ho and Tolentino reported an endophthalmitis rate as high as 0.15% after PPV in 1984, in subsequent years, the incidence has decreased to a range from 0.018% to 0.07% [25–32]. The question that whether sutureless vitrectomy increases the risk of endophthalmitis is still controversial [31, 33, 34]. Past literature suggests that subjects with diabetes have an increased tendency, after cataract surgery, to develop endophthalmitis [1, 32, 35, 36]. A plethora of reports show that approximately 14 to 21% of postoperative patients who develop endophthalmitis are diabetic [37–40].
3. Symptoms and Presentation
The incidence of ophthalmic symptoms was not substantially different in diabetic versus nondiabetic subjects, especially that patients presenting with ocular pain are nearly as frequent in both types of subjects: the diabetic and the nondiabetic. The median number of days from onset of symptoms to presentation also did not differ in both types of patients (on the average 4 days) [38]. The differences were essentially a trend towards a more opaque media in diabetic subjects upon examination than in the nondiabetics. A retinal vessel could not be seen with indirect ophthalmoscopy at presentation in 90% of diabetics, versus 77% in nondiabetic patients. Also, the incidence of rubeosis at presentation was 8.6% in diabetics versus 1.9% in the nondiabetics [38]. Table 1 summarizes the frequency of symptoms in diabetic patients and in nondiabetic patients.
Table 1.
Visual outcome and symptoms in diabetics versus nondiabetics.
| Diabetics | Nondiabetics | |
|---|---|---|
| Posttreatment visual outcome | (%) | (%) |
| ≥5/200 | 79.6 | 90 |
| ≥20/100 | 55.6 | 77.4 |
| ≥20/40 | 38.9 | 55.3 |
| Anterior segment characteristics | (%) | (%) |
| Cataract wound normal | 82.8 | 82.0 |
| Hypopyon | 89.7 | 85.1 |
| Rubeosis | 8.6 | 1.9 |
| Bacterial growth (risk) | ||
| Gram+ | Increased | — |
| Gram− | Same | Same |
| Virulent organisms | 26% | 22% |
| Incidence of retinal detachment (Posttreatment) | 6.9% | 8.6% |
| Early procedure performed | 20.7% | 8.8% |
| Late procedure performed | 31% | 27.1% |
4. Types of Isolated Microorganisms and Antibiotics Sensitivity
Postoperative endophthalmitis is most often associated with gram-positive organisms (75%–80%), next in frequency are gram-negative organisms (15%–29%), and least often fungi (3%–13%). When cultures were obtained from nondiabetic patients they were likely to show no growth in as many as twice the number noted in cultures from diabetic subjects that is at 33% versus 15%, respectively. In addition, the microorganisms that grew from eyes of diabetic subjects had a preponderance of more virulent organisms at 26% versus 22% isolated from eyes in nondiabetic patients [38]. The most common organism isolated from diabetic patients with acute endophthalmitis is coagulase-negative Staphylococcus [37]. In another study, both type 1 and type 2 diabetic patients grew staphylococcus epidermis and staphylococcus aureus at 11.79% and 11.7%, respectively for type 1, and 24.2% and 21.2% for type 2 [10]. There was a trend for a higher preponderance of coagulase-negative staphylococcal isolates in patients who had preexisting diabetic retinopathy [10]. Phillips and Tasman found a higher prevalence of gram-negative isolates of Staph organisms among their patients. Remarkably none of their patients had gram-negative endophthalmitis [41]. Of note, is the conjunctival flora of diabetic subjects differed from that isolated from nondiabetic subjects [10].
As for resistance to antibiotics, very few reports exist in the literature comparing resistance to antibiotics among different microorganisms isolated from patients with diabetes as opposed to those without. On the one hand, resistance was observed and reported to penicillin, ampicillin, and tetracycline in S. aureus isolates, on the other hand resistance to vancomycin was absent, thus singling out this antibiotic as the most effective therapeutic option [10].
5. Treatment
Endophthalmitis still poses a challenge to both the timing and the modality of treatment. To date, the largest series that has directed the standard of care remains to be the EVS, which in summary recommends the following. In eyes with LP vision or better, tap and injection were as favored as the use of pars plana vitrectomy plus tap. While in eyes with LP vision or worse the group that underwent the PPV fared better than patients who received tap with intravitreal antibiotics only. Subanalysis of the patients with diabetes in the EVS cohort was inconclusive although it suggested a more favorable outcome for patients who underwent a vitrectomy regardless of their visual outcome [42] (Figure 1: summary of the study is included in the flowchart).
Figure 1.
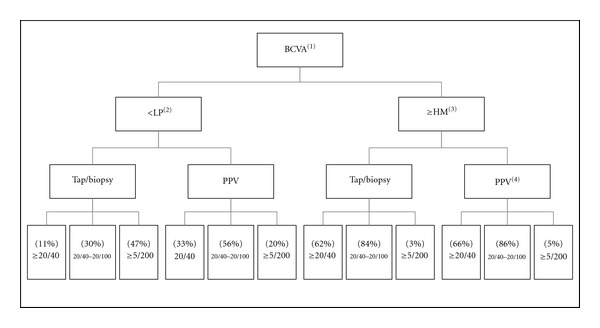
Visual outcome of endophthalmitis vitrectomy study. (1) Best corrected visual acuity, (2) light perception, (3) hand motion, (4) pars plana vitrectomy.
The use of intravitreal dexamethasone along with the antibiotics injection is still controversial. On the one hand, if intravitreal steroids are given early enough in the course of endophthalmitis, there might be some benefit for better outcome in endophthalmitis through a reduction in the inflammatory response to the infectious organism [43–46]. In one study done on nondiabetic patients who developed endophthalmitis, there was a trend towards a better visual outcome in patients with suspected bacterial endophthalmitis when treated with a combination of intravitreal antibiotics and dexamethasone [47]. On the other hand, another report demonstrated that intravitreal steroids may not be effective for acute endophthalmitis besides and it is important to be cautious using it, keeping in mind its potential toxicity and blunting of the immune response that is necessary to combat infections [48]. Jett et al. noted that combining intravitreal steroids with antibiotics may have beneficial effects in eyes infected with only bacteria that are nontoxin-producing and are less virulent; they reported that manipulation of the timing of dexamethasone administration did not have any significant effect on the treatment outcome [49]. It is obvious that studies on the use and timing of intravitreal steroids in diabetic patients with endophthalmitis are badly needed to establish a solid basis for treatment that would constitute standardized care.
6. Systemic Antibiotics
Prior results from EVS demonstrated that systemic antibiotics were not effective in the management of acute postcataract extraction endophthalmitis [40].
7. Visual Outcome after Treatment
The outcome of vision in patients with diabetes treated for endophthalmitis is usually less successful than in patients with no diabetes. Phillips and Tasman found that 26% of patients with diabetes achieved a final postoperative visual acuity equal or slightly more than 20/200 in contrast to 59% in patients without diabetes. Additionally, 30% of these diabetic patients failed to have not even light perception vision [41]. In an exploratory analysis among patients in the Endophthalmitis Vitrectomy Study (EVS), 58 out of 420 (13.8%) eyes of diabetic patients were analysed over a 9-month period, 80% achieved visual acuity of 5/200 or greater in contrast to 90% in patients who had no diabetes. Along this trend, 55% and 39% of subjects with diabetes achieved a final visual acuity equal or slightly greater than, respectively, 20/100 or greater and 20/40 or greater, compared to 77% and 55% in nondiabetic patients, respectively. As to patients who presented with better than LP vision, diabetic subjects achieved 20/40 more often when vitrectomy was applied (57%) than with tap/biopsy (40%) [38, 40]. No operative complications were observed in either group although early postoperative interventions were significantly higher in the group of diabetic patients (20.7%). However, the statistical power is very low because of the small number of subjects with diabetes [38]. Thus, until a large clinical trial studying treatment outcome in diabetic patients with better than LP vision is done, it is recommended that initial vitrectomy or tap/biopsy are reasonable approaches for diabetic patients with better than LP vision [50].
8. Endophthalmitis and Intravitreal Injection
Endophthalmitis, although a rare complication of intravitreal injection, is a serious and clinically relevant concern. This is because there are situations in which the frequency and number of injections are obligatory to avoid potential loss of vision, which otherwise may be permanent in spite of prompt and appropriate management [51]. Its incidence per injection of either bevacizumab, ranibizumab, pegaptanib, or triamcinolone ranges from 0.009% to 1.9% [51–56]. The pathogens most commonly isolated from intravitreal cultures are Staphylococcus epidermidis and staphylococci coagulase-negative [57–59]. Optimum management of the ocular surface before, during, and after intravitreal injections remains controversial. A topical combination of povidone-iodine is the only preoperative substance proven in a randomized clinical trial to reduce the risk of endophthalmitis after intraocular surgery [58, 60]. In the 2008 ASRS meeting, it has been suggested that 40% of retina specialists use topical antibiotics before anti-vascular endothelial growth factor intravitreal injections, and 86% use topical antibiotics after anti vascular endothelial growth factor intravitreal injections. In a report from the DRCR.NET, a low rate of endophthalmitis can be achieved by means of a protocol that includes use of topical povidone-iodine, a sterile lid speculum, and topical anesthetic, but does not require topical antibiotics, sterile gloves, or a sterile drape [58]. Achievement of a low rate of endophthalmitis postintravitreal injections does not require topical antibiotic prophylaxis a day before or after the injection [58].
9. Endophthalmitis after PPV
In a 20-year retrospective review of patients who developed acute onset endophthalmitis after pars plana vitrectomy at Bascom Palmer Eye Institute, 5 out of 6 patients had diabetes. Patients presented with an initial visual acuity ranging from 20/300 to light perception. Visual outcome postsurgery was poor with 4 out of 6 patients having a final vision of light perception or worse. Initial advanced retinopathy stages that these patients had might have hampered any improvement in vision. This is further supported by the Post-Vitrectomy Endophthalmitis Study, where 61% of the patients (11/18) had diabetes mellitus [32].
The visual outcome of postvitrectomy endophthalmitis is usually poor [28, 32]. Eyes undergoing sutureless vitrectomy may have an increased risk of infectious endophthalmitis compared to 20-gauge vitrectomy. Series reported earlier suggest that there was an increased risk of endophthalmitis, in contrast to more recent series, which so far report mixed results [31, 34, 61–69]. Meanwhile, variable hypotheses have been advanced to explain why sutureless transconjunctival PPV may lead to a higher rate of postoperative endophthalmitis. Some theories relate it to a lack of complete wound closure. Ultrasound biomicroscopy demonstrates that 25-gauge wounds reappose within 2 weeks [70, 71]. We do not know whether the level of ischemia caused by diabetes interferes in the proper wound healing of the sclera and the development of fibrovascular ingrowth into the vitreous base. Some suggests leaving air- or gas-filled vitreous cavity would allow sclera wound apposition secondary to the surface tension that develops at the wound interface [34, 51, 72]. Others propose that lower infusion rates are a feature of sutureless vitrectomy, and the reduced influx and efflux of fluid may allow a greater bacterial inoculum to remain in the eye [73]. In addition, less vitreous gel is removed during sutureless PPV versus 20-gauge PPV and the residual vitreous skirt may facilitate bacterial adherence and sequester bacteria [74, 75]. Future retrospective or prospective trials need to take into consideration certainly several factors.
Treatment of postvitrectomy endophthalmitis is analogous to treatment of other types of postoperative endophthalmitis. The best treatment option for gas-filled eyes with postvitrectomy endophthalmitis is not yet established. Intravitreal antibiotics are generally recommended in such eyes, but the dosage and specific drug may vary. The recommended standard dose age of intravitreal antibiotics could be beneficial in even up to 50% of gas-filled eyes [28].
10. Diabetic Retinopathy and Endophthalmitis
Diabetic retinopathy may become worse with any inflammatory process because eyes in diabetic subjects are susceptible to usually upsurging in some inflammatory factors. Huamonte and associates reported two cases of progression of diabetic retinopathy associated with the inflammatory processes typically associated with sarcoidosis [76]. This concept is further supported by the progression of diabetic retinopathy after cataract extraction. Several authors have shown that retinopathy progression after cataract surgery strongly correlates with the level of preoperative retinopathy [77–82]. Patients with preexisting diabetic retinopathy may be at increased risk for rapid retinopathy progression and a poorer visual outcome after endophthalmitis [37, 83]. So, the visual outcome after endophthalmitis treatment is highly dependent on the level of the damage caused by diabetic retinopathy before the development of endophthalmitis; this prompted the specialists in the field to recommend close monitoring of diabetic patients after endophthalmitis, whether or not they have preexisting DR.
In conclusion, although no large-scale study has looked exclusively at subjects with diabetes and endophthalmitis, analysis of the subgroup of patients with diabetes in studies comprising both (patients with diabetes and patients without) suggest that virulence is worse in the former group, growth of organisms is faster and a more aggressive treatment bares a better result. Even though no study has addressed the sutureless trend and the higher risk of endophthalmitis in patients with diabetes, it is wise to consider more conventional wound closures. Special care and more forceful management are warranted in every step. Finally, diabetic retinopathy, if preexisting, progresses to worse, therefore, more frequent retina examinations are advised in this particular subgroup.
Conflict of Interests
The authors have no financial interest in any product mentioned in the study.
References
- 1.Kattan HM, Flynn HW, Pflugfelder SC, Robertson C, Forster RK. Nosocomial endophthalmitis survey: current incidence of infection after intraocular surgery. Ophthalmology. 1991;98(2):227–238. [PubMed] [Google Scholar]
- 2.May DR, Peyman GA. Endophthalmitis after vitrectomy. American Journal of Ophthalmology. 1976;81(4):520–521. doi: 10.1016/0002-9394(76)90314-7. [DOI] [PubMed] [Google Scholar]
- 3.Callegan MC, Engelbert M, Parke DW, Jett BD, Gilmore MS. Bacterial endophthalmitis: epidemiology, therapeutics, and bacterium-host interactions. Clinical Microbiology Reviews. 2002;15(1):111–124. doi: 10.1128/CMR.15.1.111-124.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moutschen MP, Scheen AJ, Lefebvre PJ. Impaired immune responses in diabetes mellitus: analysis of the factors and mechanisms involved. Relevance to the increased susceptibility of diabetic patients to specific infections. Diabete et Metabolisme. 1992;18(3):187–201. [PubMed] [Google Scholar]
- 5.Al-Kassab AS, Raziuddin S. Immune activation and T cell subset abnormalities in circulation of patients with recently diagnosed type I diabetes mellitus. Clinical and Experimental Immunology. 1990;81(2):267–271. doi: 10.1111/j.1365-2249.1990.tb03329.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Abrass CK. Fc receptor-mediated phagocytosis: abnormalities associated with diabetes mellitus. Clinical Immunology and Immunopathology. 1990;58(1):1–17. doi: 10.1016/0090-1229(91)90144-y. [DOI] [PubMed] [Google Scholar]
- 7.Carnazzo G, Mirone G, Turturici A, et al. Pathophysiology of the immune system in elderly subjects with or without diabetes and variations after recombinant interleukin-2. Archives of Gerontology and Geriatrics. 1989;9(2):163–180. doi: 10.1016/0167-4943(89)90037-x. [DOI] [PubMed] [Google Scholar]
- 8.Alba-Loureiro TC, Munhoz CD, Martins JO, et al. Neutrophil function and metabolism in individuals with diabetes mellitus. Brazilian Journal of Medical and Biological Research. 2007;40(8):1037–1044. doi: 10.1590/s0100-879x2006005000143. [DOI] [PubMed] [Google Scholar]
- 9.Mowat A, Baum J. Chemotaxis of polymorphonuclear leukocytes from patients with diabetes mellitus. New England Journal of Medicine. 1971;284(12):621–627. doi: 10.1056/NEJM197103252841201. [DOI] [PubMed] [Google Scholar]
- 10.Bilen H, Ates O, Astam N, Uslu H, Akcay G, Baykal O. Conjunctival flora in patients with type 1 or type 2 diabetes mellitus. Advances in Therapy. 2007;24(5):1028–1035. doi: 10.1007/BF02877708. [DOI] [PubMed] [Google Scholar]
- 11.Friend J, Ishii Y, Thoft RA. Corneal epithelial changes in diabetic rats. Ophthalmic Research. 1982;14(4):269–278. doi: 10.1159/000265202. [DOI] [PubMed] [Google Scholar]
- 12.Taylor HR, Kimsey RA. Corneal epithelial basement membrane changes in diabetes. Investigative Ophthalmology and Visual Science. 1981;20(4):548–553. [PubMed] [Google Scholar]
- 13.Azar DT, Spurr-Michaud SJ, Tisdale AS, Gipson IK. Altered epithelial-basement membrane interactions in diabetic corneas. Archives of Ophthalmology. 1992;110(4):537–540. doi: 10.1001/archopht.1992.01080160115045. [DOI] [PubMed] [Google Scholar]
- 14.Zagon IS, Sassani JW, McLaughlin PJ. Insulin treatment ameliorates impaired corneal reepithelialization in diabetic rats. Diabetes. 2006;55(4):1141–1147. doi: 10.2337/diabetes.55.04.06.db05-1581. [DOI] [PubMed] [Google Scholar]
- 15.Inoue K, Okugawa K, Amano S, et al. Blinking and superficial punctate keratopathy in patients with diabetes mellitus. Eye. 2005;19(4):418–421. doi: 10.1038/sj.eye.6701497. [DOI] [PubMed] [Google Scholar]
- 16.Rehany U, Ishii Y, Lahav M, Rumelt S. Ultrastructural changes in corneas of diabetic patients: an electron-microscopy study. Cornea. 2000;19(4):534–538. doi: 10.1097/00003226-200007000-00026. [DOI] [PubMed] [Google Scholar]
- 17.Saini JS, Khandalavla B. Corneal epithelial fragility in diabetes mellitus. Canadian Journal of Ophthalmology. 1995;30(3):142–146. [PubMed] [Google Scholar]
- 18.Manning BD, Cantley LC. AKT/PKB signaling: navigating downstream. Cell. 2007;129(7):1261–1274. doi: 10.1016/j.cell.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panka DJ, Atkins MB, Mier JW. Targeting the mitogen-activated protein kinase pathway in the treatment of malignant melanoma. Clinical Cancer Research. 2006;12(7):2371s–2375s. doi: 10.1158/1078-0432.CCR-05-2539. [DOI] [PubMed] [Google Scholar]
- 20.Rao GN. Dr. P. Siva Reddy Oration. Diabetic keratopathy. Indian Journal of Ophthalmology. 1987;35(5-6):16–36. [PubMed] [Google Scholar]
- 21.Xu KP, Li Y, Ljubimov AV, Yu FSX. High glucose suppresses epidermal growth factor receptor/phosphatidylinositol 3-kinase/akt signaling pathway and attenuates corneal epithelial wound healing. Diabetes. 2009;58(5):1077–1085. doi: 10.2337/db08-0997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu K, Yu FS. Impaired epithelial wound healing and EGFR signaling pathways in the corneas of diabetic rats. Investigative Ophthalmology & Visual Science. 2011;52(6):3301–3308. doi: 10.1167/iovs.10-5670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Javitt JC, Vitale S, Canner JK, et al. National outcomes of cataract extraction: endophthalmitis following inpatient surgery. Archives of Ophthalmology. 1991;109(8):1085–1089. doi: 10.1001/archopht.1991.01080080045025. [DOI] [PubMed] [Google Scholar]
- 24.Allen HF, Mangiaracine AB. Bacterial endophthalmitis after cataract extraction: a study of 22 infections in 20,000 operations. Archives of ophthalmology. 1964;72:454–462. doi: 10.1001/archopht.1964.00970020454003. [DOI] [PubMed] [Google Scholar]
- 25.Aaberg TM, Flynn HW, Schiffman J, Newton J. Nosocomial acute-onset postoperative endophthalmitis survey: a 10-year review of incidence and outcomes. Ophthalmology. 1998;105(6):1004–1010. doi: 10.1016/S0161-6420(98)96000-6. [DOI] [PubMed] [Google Scholar]
- 26.Eifrig CWG, Flynn Jr. HW, Scott IU, Newton J. Acute-onset postoperative endophthalmitis: review of incidence and visual outcomes (1995–2001) Ophthalmic Surgery and Lasers. 2002;33(5):373–378. [PubMed] [Google Scholar]
- 27.Ho PC, Tolentino FI. Bacterial endophthalmitis after closed vitrectomy. Archives of Ophthalmology. 1984;102(2):207–210. doi: 10.1001/archopht.1984.01040030157016. [DOI] [PubMed] [Google Scholar]
- 28.Eifrig CWG, Scott IU, Flynn HW, Smiddy WE, Newton J. Endophthalmitis after pars plana vitrectomy: incidence, causative organisms, and visual acuity outcomes. American Journal of Ophthalmology. 2004;138(5):799–802. doi: 10.1016/j.ajo.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 29.Sakamoto T, Enaida H, Kubota T, et al. Incidence of acute endophthalmitis after triamcinolone-assisted pars plana vitrectomy. American Journal of Ophthalmology. 2004;138(1):137–138. doi: 10.1016/j.ajo.2004.02.072. [DOI] [PubMed] [Google Scholar]
- 30.Zhang S, Ding X, Hu J, Gao R. Clinical features of endophthalmitis after vitreoretinal surgery. Yan Ke Xue Bao. 2003;19(1):39–43. [PubMed] [Google Scholar]
- 31.Kunimoto DY, Kaiser RS. Incidence of Endophthalmitis after 20- and 25-Gauge Vitrectomy. Ophthalmology. 2007;114(12):2133–2137. doi: 10.1016/j.ophtha.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 32.Cohen SM, Flynn HW, Murray TG, et al. Endophthalmitis after pars plana vitrectomy. Ophthalmology. 1995;102(5):705–712. doi: 10.1016/s0161-6420(95)30965-7. [DOI] [PubMed] [Google Scholar]
- 33.Scott IU, Flynn HW, Dev S, et al. Endophthalmitis after 25-gauge and 20-gauge pars plana vitrectomy: incidence and outcomes. Retina. 2008;28(1):138–142. doi: 10.1097/IAE.0b013e31815e9313. [DOI] [PubMed] [Google Scholar]
- 34.Parolini B, Romanelli F, Prigione G, Pertile G. Incidence of endophthalmitis in a large series of 23-gauge and 20-gauge transconjunctival pars plana vitrectomy. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2009;247(7):895–898. doi: 10.1007/s00417-009-1063-0. [DOI] [PubMed] [Google Scholar]
- 35.Montan PG, Koranyi G, Setterquist HE, Stridh A, Philipson BT, Wiklund K. Endophthalmitis after cataract surgery: risk factors relating to technique and events of the operation and patient history: a retrospective case-control study. Ophthalmology. 1998;105(12):2171–2177. doi: 10.1016/S0161-6420(98)91211-8. [DOI] [PubMed] [Google Scholar]
- 36.Scott IU, Flynn HW, Feuer W. Endophthalmitis after secondary intraocular lens implantation: a case- control study. Ophthalmology. 1995;102(12):1925–1931. doi: 10.1016/s0161-6420(95)30774-9. [DOI] [PubMed] [Google Scholar]
- 37.Dev S, Pulido JS, Tessler HH, et al. Progression of diabetic retinopathy after endophthalmitis. Ophthalmology. 1999;106(4):774–781. doi: 10.1016/S0161-6420(99)90166-5. [DOI] [PubMed] [Google Scholar]
- 38.Doft BH, Wisniewski SR, Kelsey SF, Groer-Fitzgerald S. Diabetes and postcataract extraction endophthalmitis. Current Opinion in Ophthalmology. 2002;13(3):147–151. doi: 10.1097/00055735-200206000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Jain IS, Luthra CL, Das T. Diabetic retinopathy and its relation to errors of refraction. Archives of Ophthalmology. 1967;77(1):59–60. doi: 10.1001/archopht.1967.00980020061012. [DOI] [PubMed] [Google Scholar]
- 40.Doft B, Nakamura T, Walonker AF, et al. Results of the endophthalmitis vitrectomy study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Archives of Ophthalmology. 1995;113(12):1479–1496. [PubMed] [Google Scholar]
- 41.Phillips WB, Tasman WS. Postoperative endophthalmitis in association with diabetes mellitus. Ophthalmology. 1994;101(3):508–518. doi: 10.1016/s0161-6420(13)31268-8. [DOI] [PubMed] [Google Scholar]
- 42.Doft BH. Treatment of postcataract extraction endophthalmitis: a summary of the results from the endophthalmitis vitrectomy study. Archives of Ophthalmology. 2008;126(4):554–556. doi: 10.1001/archopht.126.4.554. [DOI] [PubMed] [Google Scholar]
- 43.Graham RO, Peyman GA. Intravitreal injection of dexamethasone. Treatment of experimentally induced endophthalmitis. Archives of Ophthalmology. 1974;92(2):149–154. doi: 10.1001/archopht.1974.01010010155016. [DOI] [PubMed] [Google Scholar]
- 44.Park SS, Samiy N, Ruoff K, D’Amico DJ, Baker AS. Effect of intravitreal dexamethasone in treatment of pneumococcal endophthalmitis in rabbits. Archives of Ophthalmology. 1995;113(10):1324–1329. doi: 10.1001/archopht.1995.01100100112040. [DOI] [PubMed] [Google Scholar]
- 45.Mao LK, Flynn HW, Miller D, Pflugfelder SC. Endophthalmitis caused by Staphylococcus aureus. American Journal of Ophthalmology. 1993;116(5):584–589. doi: 10.1016/s0002-9394(14)73200-3. [DOI] [PubMed] [Google Scholar]
- 46.Irvine WD, Flynn HW, Miller D, Pflugfelder SC. Endophthalmitis caused by gram-negative organisms. Archives of Ophthalmology. 1992;110(10):1450–1454. doi: 10.1001/archopht.1992.01080220112031. [DOI] [PubMed] [Google Scholar]
- 47.Gan IM, Ugahary LC, van Dissel JT, et al. Intravitreal dexamethasone as adjuvant in the treatment of postoperative endophthalmitis: a prospective randomized trial. Graefe’s Archive for Clinical and Experimental Ophthalmology. 2005;243(12):1200–1205. doi: 10.1007/s00417-005-0133-1. [DOI] [PubMed] [Google Scholar]
- 48.Shah GK, Stein JD, Sharma S, et al. Visual outcomes following the use of intravitreal steroids in the treatment of postoperative endophthalmitis. Ophthalmology. 2000;107(3):486–489. doi: 10.1016/s0161-6420(99)00139-6. [DOI] [PubMed] [Google Scholar]
- 49.Jett BD, Jensen HG, Atkuri RV, Gilmore MS. Evaluation of therapeutic measures for treating endophthalmitis caused by isogenic toxin-producing and toxin-nonproducing Enterococcus faecalis strains. Investigative Ophthalmology and Visual Science. 1995;36(1):9–15. [PubMed] [Google Scholar]
- 50.Doft BH, Wisniewski SR, Kelsey SF, Fitzgerald SG. Diabetes and postoperative endophthalmitis in the endophthalmitis vitrectomy study. Archives of Ophthalmology. 2001;119(5):650–656. doi: 10.1001/archopht.119.5.650. [DOI] [PubMed] [Google Scholar]
- 51.Cavalcante LL, Cavalcante ML, Murray TG, et al. Intravitreal injection analysis at the Bascom palmer eye institute: evaluation of clinical indications for the treatment and incidence rates of endophthalmitis. Clinical Ophthalmology. 2010;4(1):519–524. doi: 10.2147/opth.s11094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fintak DR, Shah GK, Blinder KJ, et al. Incidence of endophthalmitis related to intravitreal injection of bevacizumab and ranibizumab. Retina. 2008;28(10):1395–1399. doi: 10.1097/IAE.0b013e3181884fd2. [DOI] [PubMed] [Google Scholar]
- 53.Mason JO, White MF, Feist RM, et al. Incidence of acute onset endophthalmitis following intravitreal bevacizumab (Avastin) injection. Retina. 2008;28(4):564–567. doi: 10.1097/IAE.0b013e3181633fee. [DOI] [PubMed] [Google Scholar]
- 54.Pilli S, Kotsolis A, Spaide RF, et al. Endophthalmitis associated with intravitreal anti-vascular endothelial growth factor therapy injections in an office setting. American Journal of Ophthalmology. 2008;145(5):879–882. doi: 10.1016/j.ajo.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 55.Scott IU, Flynn HW. Reducing the risk of endophthalmitis following intravitreal injections. Retina. 2007;27(1):10–12. doi: 10.1097/IAE.0b013e3180307271. [DOI] [PubMed] [Google Scholar]
- 56.El-Mollayess GM, Noureddine BN, Bashshur ZF. Bevacizumab and neovascular age related macular degeneration: pathogenesis and treatment. Seminars in Ophthalmology. 2011;26(3):69–76. doi: 10.3109/08820538.2010.545100. [DOI] [PubMed] [Google Scholar]
- 57.Klein KS, Walsh MK, Hassan TS, et al. Endophthalmitis after anti-VEGF injections. Ophthalmology. 2009;116(6):p. 1225. doi: 10.1016/j.ophtha.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 58.Bhavsar AR, Googe JM, Stockdale CR, et al. Risk of endophthalmitis after intravitreal drug injection when topical antibiotics are not required: the diabetic retinopathy clinical research network laser-ranibizumab-triamcinolone clinical trials. Archives of Ophthalmology. 2009;127(12):1581–1583. doi: 10.1001/archophthalmol.2009.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Diago T, McCannel CA, Bakri SJ, Pulido JS, Edwards AO, Pach JM. Infectious endophthalmitis after intravitreal injection of antiangiogenic agents. Retina. 2009;29(5):601–605. doi: 10.1097/IAE.0b013e31819d2591. [DOI] [PubMed] [Google Scholar]
- 60.Speaker MG, Menikoff JA. Prophylaxis of endophthalmitis with topical povidone-iodine. Ophthalmology. 1991;98(12):1769–1775. doi: 10.1016/s0161-6420(91)32052-9. [DOI] [PubMed] [Google Scholar]
- 61.Taylor SRJ, Aylward GW. Endophthalmitis following 25-gauge vitrectomy. Eye. 2005;19(11):1228–1229. doi: 10.1038/sj.eye.6701737. [DOI] [PubMed] [Google Scholar]
- 62.Taban M, Ufret-Vincenty RL, Sears JE. Endophthalmitis after 25-gauge transconjunctival sutureless vitrectomy. Retina. 2006;26(7):830–831. doi: 10.1097/01.iae.0000244272.13890.cc. [DOI] [PubMed] [Google Scholar]
- 63.Shimada H, Nakashizuka H, Hattori T, Mori R, Mizutani Y, Yuzawa M. Incidence of endophthalmitis after 20- and 25-Gauge vitrectomy. Causes and prevention. Ophthalmology. 2008;115(12):2215–2220. doi: 10.1016/j.ophtha.2008.07.015. [DOI] [PubMed] [Google Scholar]
- 64.Hu AYH, Bourges JL, Shah SP, et al. Endophthalmitis after pars plana vitrectomy: a 20- and 25-gauge comparison. Ophthalmology. 2009;116(7):1360–1365. doi: 10.1016/j.ophtha.2009.01.045. [DOI] [PubMed] [Google Scholar]
- 65.Mason JO, Yunker JJ, Vail RS, et al. Incidence of endophthalmitis following 20-gauge and 25-gauge vitrectomy. Retina. 2008;28(9):1352–1354. doi: 10.1097/IAE.0b013e318180d308. [DOI] [PubMed] [Google Scholar]
- 66.Chen JK, Khurana RN, Nguyen QD, Do DV. The incidence of endophthalmitis following transconjunctival sutureless 25- vs. 20-gauge vitrectomy. Eye. 2009;23(4):780–784. doi: 10.1038/eye.2008.160. [DOI] [PubMed] [Google Scholar]
- 67.Matsuyama K, Kunitomi K, Taomoto M, Nishimura T. Early-onset endophthalmitis caused by methicillin-resistant Staphylococcus epidermidis after 25-gauge transconjunctival sutureless vitrectomy. Japanese Journal of Ophthalmology. 2008;52(6):508–510. doi: 10.1007/s10384-008-0583-1. [DOI] [PubMed] [Google Scholar]
- 68.Acar N, Unver YB, Altan T, Kapran Z. Acute endophthalmitis after 25-gauge sutureless vitrectomy. International Ophthalmology. 2007;27(6):361–363. doi: 10.1007/s10792-007-9081-6. [DOI] [PubMed] [Google Scholar]
- 69.Bahrani HM, Fazelat AA, Thomas M, et al. Endophthalmitis in the era of small gauge transconjunctival sutureless vitrectomymeta analysis and review of literature. Seminars in Ophthalmology. 2010;25(5-6):275–282. doi: 10.3109/08820538.2010.518109. [DOI] [PubMed] [Google Scholar]
- 70.Keshavamurthy R, Venkatesh P, Garg S. Ultrasound biomicroscopy findings of 25 G Transconjuctival sutureless (TSV) and conventional (20G) pars plana sclerotomy in the same patient. BMC Ophthalmology. 2006;6, article 7 doi: 10.1186/1471-2415-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Singh A, Chen JA, Stewart JM. Ocular surface fluid contamination of sutureless 25-gauge vitrectomy incisions. Retina. 2008;28(4):553–557. doi: 10.1097/IAE.0b013e31816690d4. [DOI] [PubMed] [Google Scholar]
- 72.Kreiger A. Sclerotomy complications following pars plana vitrectomy. British Journal of Ophthalmology. 2001;85(1):121–122. doi: 10.1136/bjo.85.1.121b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Fujii GY, De Juan E, Humayun MS, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109(10):1807–1812. doi: 10.1016/s0161-6420(02)01179-x. [DOI] [PubMed] [Google Scholar]
- 74.Meredith TA. Antimicrobial pharmacokinetics in endoph-thalmitis treatment: studies of ceftazidime. Transactions of the American Ophthalmological Society. 1993;91:653–699. [PMC free article] [PubMed] [Google Scholar]
- 75.Chen SDM, Mohammed Q, Bowling B, et al. Vitreous wick syndrome—a potential cause of endophthalmitis after intravitreal injection of triamcinolone through the pars plana. American Journal of Ophthalmology. 2004;137(6):1159–1161. doi: 10.1016/j.ajo.2004.01.028. [DOI] [PubMed] [Google Scholar]
- 76.Huamonte FU, Cyrlin MN, Tessler HH, Goldberg MF. Retinopathy in diabetes associated with sarcoidosis. Annals of Ophthalmology. 1980;12(11):1290–1297. [Google Scholar]
- 77.Jaffe GJ, Burton TC. Progression of nonproliferative diabetic retinopathy following cataract extraction. Archives of Ophthalmology. 1988;106(6):745–749. doi: 10.1001/archopht.1988.01060130815029. [DOI] [PubMed] [Google Scholar]
- 78.Jaffe GJ, Burton TC, Kuhn E, Prescott A, Hartz A. Progression of nonproliferative diabetic retinopathy and visual outcome after extracapsular cataract extraction and intraocular lens implantation. American Journal of Ophthalmology. 1992;114(4):448–456. doi: 10.1016/s0002-9394(14)71857-4. [DOI] [PubMed] [Google Scholar]
- 79.Pollack A, Dotan S, Oliver M. Progression of diabetic retinopathy after cataract extraction. British Journal of Ophthalmology. 1991;75(9):547–551. doi: 10.1136/bjo.75.9.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Cheng H, Franklin SL. Treatment of cataract in diabetics with and without retinopathy. Eye. 1988;2(6):607–614. doi: 10.1038/eye.1988.113. [DOI] [PubMed] [Google Scholar]
- 81.Schatz H, Atienza D, McDonald HR, Johnson RN. Severe diabetic retinopathy after cataract surgery. American Journal of Ophthalmology. 1994;117(3):314–321. doi: 10.1016/s0002-9394(14)73138-1. [DOI] [PubMed] [Google Scholar]
- 82.Cunliffe IA, Flanagan DW, George NDL, Aggarwaal RJ, Moore AT. Extracapsular cataract surgery with lens implantation in diabetics with and without proliferative retinopathy. British Journal of Ophthalmology. 1991;75(1):9–12. doi: 10.1136/bjo.75.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lai TYY, Kwok AKH, Lam DSC, Bhende P, Dev S, Pulido JS. Progression of diabetic retinopathy after endophthalmitis. Ophthalmology. 2000;107(4):619–621. doi: 10.1016/s0161-6420(99)00153-0. [DOI] [PubMed] [Google Scholar]


