Abstract
Background:
Aluminum phosphide (ALP) (celphos) is an agricultural pesticide commonly implicated in poisoning. Literature pertaining to the clinical manifestations and treatment outcome of its poisoning among children is limited.
Materials and Methods:
A retrospective chart review was conducted of the medical records of 30 children aged less than 14 years admitted to pediatric intensive care unit (PICU) of a tertiary care hospital in northern India. Demographic, clinical, and laboratory parameters were recorded. The outcome was categorized into “survivors” and “nonsurvivors.”
Results:
The Mean (SD) age of the enrolled children [19 males (63.3%)] was 8.55 (3.07) years. Among the 30 children, 14 (46.67%) were nonsurvivors and the rest 16 (53.33%) were survivors. Nonsurvivors had ingested significantly higher doses of ALP (P < 0.001), and showed higher time lag to PICU transfer (P 0.031), presence of abnormal radiological findings on chest skiagram (P = 0.007), and a higher Pediatric Risk of Mortality (PRISM) III score (P < 0.001) at admission. Use of magnesium sulfate was associated significantly with survival [odds ratio (OR) (95% CI): 0.11 (0.02-0.66); P 0.016].
Conclusion:
The present study highlights that survival among children with ALP poisoning is predicted by dose of ALP ingestion, time lag to medical attention, and higher PRISM score at admission. Use of magnesium sulfate could be associated with better survival among them.
Keywords: Magnesium sulfate, mortality, pediatric intensive care
Introduction
Aluminum phosphide (ALP) (trade name: Celphos) poisoning has emerged as one of the leading causes of poisoning among children, with a mortality ranging from 30 to 100%.[1] ALP is a solid fumigant pesticide, commonly used for grain preservation in many rural households of North India.[2] It is a cheap, easily available, highly toxic substance that has no antidote. Symptoms of ALP poisoning appear within the first few hours following exposure. Treatment of ALP poisoning is mainly supportive, including fluid resuscitation, inotropic support, and mechanical ventilation. Although there are voluminous data from adult patients, literature pertaining to the clinical profile and treatment outcome of children with ALP poisoning is limited.[3,4] Hence, this study was planned to evaluate the clinical characteristics and determine the prognostic factors of ALP poisoning in children from Rohtak district of Haryana.
Materials and Methods
The study was conducted at the Pediatric Intensive Care Unit (PICU) of a tertiary care teaching hospital of North India. Data were collected by a retrospective chart review of all patients admitted from May 2008 to April 2013 with a diagnosis of ALP poisoning. The diagnosis of ALP poisoning was based on alleged history of ingestion of ALP. Forensic reports of gastric aspirates and postmortem findings were not analyzed. A total of 47 case records of children aged less than 12 years with ALP poisoning were retrieved. Patients who died within 2 h of admission or those who took Leave Against Medical Advice (LAMA) (n = 2) or those whose medical records were incomplete (n = 15) were excluded from our study. Among the incomplete case records (n = 15), outcome was fatal in 13 children and the remaining 2 children had absconded from the hospital, hence their final outcome was not known. Children who presented following inhalation of ALP alone were also excluded.
The baseline demographic data including the amount of ALP ingested, nature of poisoning (homicidal or accidental), whether siblings/parents were also poisoned, and time lag to medical attention from the time of ingestion were collected. Presenting complaints, clinical characteristics (Glasgow coma scale, respiratory distress, blood pressure, pallor), and laboratory characteristics [hemoglobin, total leukocyte count, blood creatinine phosphokinase (CPK) level, arterial blood gas, chest X-ray] at the time of admission were recorded. Pediatric Risk of Mortality (PRISM) III score was estimated based on the hemodynamic and laboratory characteristics at admission to PICU.
The management of ALP poisoning in our hospital was primarily supportive. Gastric lavage was performed in all patients within the first hour of admission. All the patients were admitted to PICU for monitoring. Treatment characteristics including number of fluid boluses, use of inotropic drugs like dopamine/dobutamine, and use of magnesium were retrieved. The dose of magnesium sulfate used was 200 mg/kg as infusion in 0-2 h. Total duration of PICU stay was also recorded. The outcome was categorized as “survivor” and “nonsurvivor.”
Statistical analysis
The quantitative variables were presented in terms of Mean (SD) or Median (IQR), and the qualitative variables were presented as numbers (proportions). Comparisons between survivor and nonsurvivor groups were made by unpaired t-test for quantitative data and Chi-square or Fisher's exact test for categorical data. Statistical analysis was performed using SPSS version 15.0. P < 0.05 were considered statistical significant.
Results
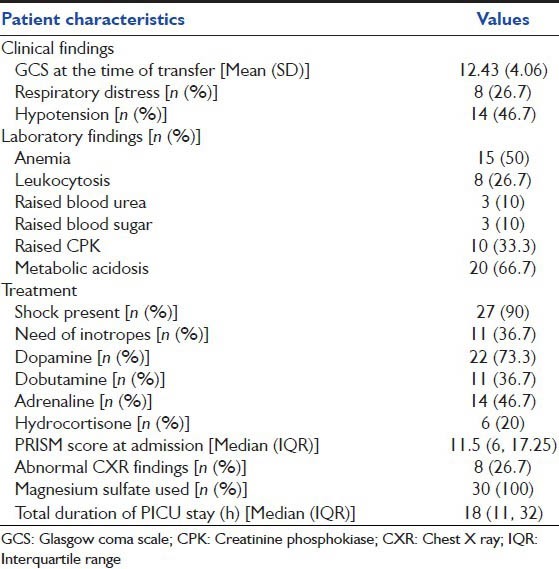
Case records of 30 children [19 (63.3%) males, 11 (36.7%) females] with ALP poisoning were included in the study, of whom 14 (46.67%) had died (nonsurvivors) and the remaining 16 (53.33%) had survived. Majority [28/30 (93.3%)] were from rural background. Mean (SD) age of the enrolled children was 8.55 (3.07) years. Median (IQR) ingested dose of ALP was 3 (3, 9) g. Twenty-five children (83.3%) were of rural background, while the remaining 5 children (16.7%) were of urban background. The presenting symptoms were vomiting [12 (40%)], abdominal pain [3 (10%)], and headache [3 (10%)]. The time lag to PICU transfer from the time of ingestion was 3.10 (1.48) h [Table 1]. Majority of the cases were homicidal [23 (76.7%)], with siblings and parents also poisoned in 14 (46.7%) and 18 (60%) cases, respectively. Median (IQR) duration of PICU stay was 18 (11, 32) h.
Table 1.
Clinical, laboratory, and treatment characteristics of enrolled children (N=30)
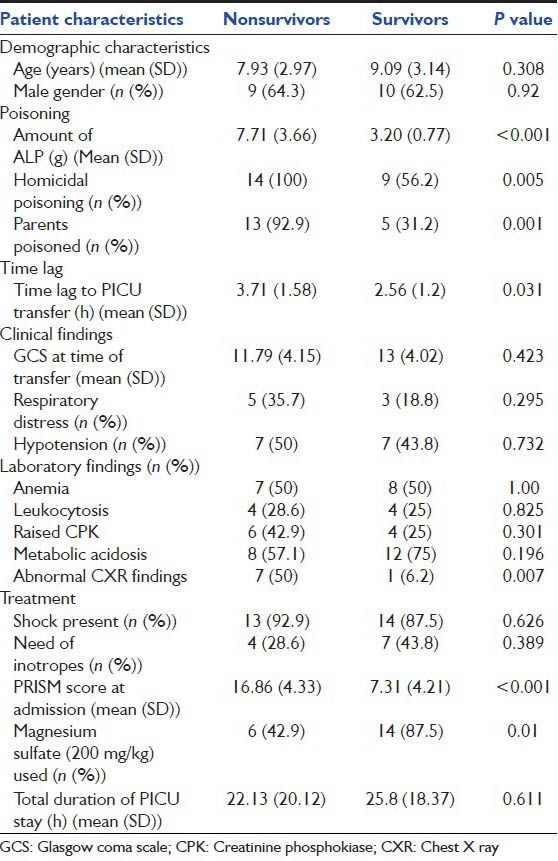
Nonsurvivors had ingested significantly higher doses of ALP (P < 0.001), had higher time lag to PICU transfer (P 0.031), abnormal radiological findings on chest skiagram, a higher PRISM III score at admission, and their parents were also poisoned (P 0.001) [Table 2]. A single dose of 200 mg/kg of magnesium sulfate was used among all the subjects. We observed that the use of magnesium sulfate was significantly more among survivors than among nonsurvivors (P 0.01) [Table 2]. Use of magnesium sulfate was associated significantly with survival [odds ratio (OR) (95% CI): 0.11 (0.02-0.66); P 0.016].
Table 2.
Comparison of clinical characteristics among survivors (n=14) and nonsurvivors (n=16)
Discussion
ALP poisoning has been an important concern of public health in various parts of India. ALP is freely available as a 3 g tablet in the grain markets of North India at a reasonable cost of 55-60 per 10 tablets. It is used as a preservative for wheat, and is accessible only to farmers in various parts of northern India. Although there are a large number of retrospective data from the adult population, literature pertaining to clinical profile and treatment outcome among children with ALP poisoning is limited to a few studies.[3,4] It is surprising to see that the trend of ALP poisoning has shown no decline from early 1980s.[5] Recently there was a report of an entire family who died by suicidal poisoning with celphos in a small village in Haryana, distressed by their family circumstances.[6]
ALP is a common suicidal agent of poisoning among adults, with a peak incidence of its poisoning found in the 21-25 years age group with a male predominance.[5,7] In our study, the average age of poisoning was 8.5 years. It is more common among the populations with a rural background.[7] A similar observation was seen in our study, with a higher number of children from the rural background. ALP is a common cause of accidental and homicidal poisoning in children, with the mortality ranging from 30 to 100%.[1] In our study, the mortality was 47%, which is comparable to that reported in a previous study (58.6%).[3] However, we acknowledge that a sizeable number of case records were excluded with fatal outcome, owing to incomplete information pertaining to our research, which could have led to underestimation of the overall mortality. The toxic dose reported in the literature is >1.5 g.[8] However, we found that the average dose of ALP among the enrolled children in our study was 3 g. The higher dose in our study could be fallacious as explained by the retrospective data retrieval and the possibility of inappropriate history regarding the amount of ALP ingested. Moreover, it is quite possible that homicidal attempt to poison the children could result in forceful spitting or vomiting of the tablet after tasting. Average duration from ingestion to expiry death has been reported to range from within 30 min to 3 days.[9] This was comparable to the mean duration of 22 h obtained in our study.
We found that increasing time lag to PICU transfer, higher amount of ALP ingestion, and higher PRISM III score at admission were significant predictors of mortality among children with ALP poisoning. In a retrospective study in a medical ICU of Morocco, it was observed that higher APACHE II score, presence of shock, lower Glasgow coma score, and use of vasoactive drugs were important prognostic factors for mortality among their adult patients.[10] However, we did not find any significant difference in the presence of shock among survivors and nonsurvivors. These findings are consistent with the findings of previous studies.[9] The possible mechanisms for development of shock among patients with ALP poisoning are peripheral vasodilatation, myocardial depression, and severe pulmonary edema.
We observed in our study that the proportion of patients who received magnesium sulfate was significantly higher among survivors than among nonsurvivors. The role of magnesium sulfate as a treatment option has been described in various studies in adult patients with ALP poisoning.[11,12] The possible mechanism of action of magnesium sulfate among adults was its effect as a cell membrane stabilizing agent reducing the incidence of cardiac arrhythmias. This anti-arrhythmic action could probably result in improvement in myocardial functioning among children with shock. In a prospective study on 50 adult patients with ALP poisoning, it was observed that there was no evidence of hypomagnesemia in these patients and magnesium sulfate therapy was not found to be useful.[13] However, in a randomized controlled trial on the role of magnesium sulfate infusion, higher dose of magnesium sulfate was shown to reduce the mortality in adults.[14] In addition, the magnesium levels in different organs of patients who received magnesium as part of treatment were found to be significantly higher, in comparison to those of controls as well as the patient group not treated with magnesium sulfate.[15] We used a loading dose of 200 mg/kg followed by 40 mg/kg/h infusion. Considering significant improvement in terms of survival, we advocate further prospective trials to study the efficacy and safety of magnesium sulfate in children with ALP poisoning.
The limitation of our study includes absence of correlation with autopsy findings among nonsurvivors, retrospective nature of data collection, and relatively small sample size. We conclude that increase time lag to PICU transfer, higher amount of ALP ingestion, and higher PRISM III score at admission were the significant predictors of mortality among children with ALP poisoning. Use of magnesium sulfate could be considered as an early treatment option in children with ALP poisoning.
Conclusion
We conclude that the predictors of mortality among children with ALP poisoning were higher dose of ALP ingestion and delay in medical attention. In addition, we found that the use of magnesium sulfate for treatment of children with ALP poisoning was associated with better survival. We believe stringent laws to curtail free access of celphos tablets in grain markets, faster access to health center, and early administration of magnesium sulfate could probably improve the survival among children with celphos poisoning.
Acknowledgment
We thank the help of Dr. Geeta Gathwala, Head of Department, Department of Pediatrics, PGIMS, Rohtak for promoting this research activity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Mehrpour O, Jafarzadeh M, Abdollahi M. A systematic review of aluminium phosphide poisoning. Arh Hig Rada Toksikol. 2012;63:61–73. doi: 10.2478/10004-1254-63-2012-2182. [DOI] [PubMed] [Google Scholar]
- 2.Hosseinian A, Pakravan N, Rafiei A, Feyzbakhsh SM. Aluminum phosphide poisoning known as rice tablet: A common toxicity in North Iran. Indian J Med Sci. 2011;65:143–50. [PubMed] [Google Scholar]
- 3.Singh S, Singhi S, Sood NK, Kumar L, Walia BN. Changing pattern of childhood poisoning (1970-1989): Experience of a large north Indian hospital. Indian Pediatr. 1995;32:331–6. [PubMed] [Google Scholar]
- 4.Gupta SK, Peshin SS, Srivastava A, Kaleekal T. A study of childhood poisoning at National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. J Occup Health. 2003;45:191–6. doi: 10.1539/joh.45.191. [DOI] [PubMed] [Google Scholar]
- 5.Singh D, Tyagi S, Bansal YS, Mandal SP, Thind AS. ALP fatalities: A 24 years experience. J Indian Acad Forensic Med. 2007;29:12–6. [Google Scholar]
- 6.Distressed over girl's kidnapping and rape, poor family consumes poison. [Last accessed on 2013 Jun 26]. Available from: http://www.tribuneindia.com/2013/20130423/haryana.htm#2 .
- 7.Kapoor AK, Sinha US, Singh AK, Mehrotra R. An epidemiological study of ALP poisoning at Allahabad? [Last accessed on 2013 Jul 06]. Available from: http://www.indianjournals.com/ijoraspxtarget=ijor: iijfmt and volume=5 and issue=2 and article=002 .
- 8.Anger F, Paysant F, Brousse F, Normand IL, Develay P, Gaillard Y, et al. Fatal aluminium phosphide poisoning. J Anal Toxicol. 2000;24:90–2. doi: 10.1093/jat/24.2.90. [DOI] [PubMed] [Google Scholar]
- 9.Chopra JS, Kalra OP, Malik VS, Sharma R, Chandna A. ALP poisoning: A prospective study of 16 cases in one year. Postgrad Med J. 1986;62:1113–5. doi: 10.1136/pgmj.62.734.1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Louriz M, Dendane T, Abidi K, Madani N, Abouqal R, Zeggwagh AA. Prognostic factors of acute ALP poisoning. Indian J Med Sci. 2009;63:227–34. [PubMed] [Google Scholar]
- 11.Chugh SN, Jaggal KL, Sharma A, Arora B, Malhotra KC. Magnesium levels in acute cardiotoxicity due to ALP poisoning. Indian J Med Res. 1991;94:437–9. [PubMed] [Google Scholar]
- 12.Chugh SN, Kolley T, Kakkar R, Chugh K, Sharma A. A critical evaluation of anti-peroxidant effect of intravenous magnesium in acute ALP poisoning. Magnes Res. 1997;10:225–30. [PubMed] [Google Scholar]
- 13.Siwach SB, Singh P, Ahlawat S, Dua A, Sharma D. Serum and tissue magnesium content in patients of aluminium phosphide poisoning and critical evaluation of high dose magnesium sulphate therapy in reducing mortality. J Assoc Physicians India. 1994;42:107–10. [PubMed] [Google Scholar]
- 14.Chugh SN, Kumar P, Aggarwal HK, Sharma A, Mahajan SK, Malhotra KC. Efficacy of magnesium sulphate in aluminium phosphide poisoning-comparison of two different dose schedules. J Assoc Physicians India. 1994;42:373–5. [PubMed] [Google Scholar]
- 15.Siwach SB, Dua A, Sharma R, Sharma D, Mehla RK. Tissue magnesium content and histopathological changes in non-survivors of aluminiumphosphide poisoning. J Assoc Physicians India. 1995;43:676–8. [PubMed] [Google Scholar]


