Abstract
Objective
To develop a conceptual framework for the design of an in-home monitoring system (IMS) based on the requirements of older adults with vision impairment (VI), informal caregivers and eye-care rehabilitation professionals.
Materials and Methods
Concept mapping, a mixed-methods statistical research tool, was used in the construction of the framework. Overall, 40 participants brainstormed or sorted and rated 83 statements concerning an IMS for older adults with VI. Multidimensional scaling and hierarchical cluster analysis were employed to construct the framework. A questionnaire yielded further insights into the views of a wider sample of older adults with VI (n=78) and caregivers (n=25) regarding IMS.
Results
Concept mapping revealed a nine-cluster model of IMS-related aspects including affordability, awareness of system capabilities, simplicity of installation, operation and maintenance, system integrity and reliability, fall detection and safe movement, user customization, user preferences regarding information delivery, and safety alerts for patients and caregivers. From the questionnaire, independence, safety and fall detection were the most commonly reported reasons for older adults and caregivers to accept an IMS. Concerns included cost, privacy, security of the information obtained through monitoring, system accuracy, and ease of use.
Discussion
Older adults with VI, caregivers and professionals are receptive to in-home monitoring, mainly for fall detection and safety monitoring, but have concerns that must be addressed when developing an IMS.
Conclusion
Our study provides a novel conceptual framework for the design of an IMS that will be maximally acceptable and beneficial to our ageing and vision-impaired population.
Keywords: In-home monitoring, in-home monitoring system (IMS), assistive technology, elderly, vision impairment
Background and significance
The proportion of people aged 60 years or older in Australia will increase from 16.4% in 2000 to 29.9% in 2050.1 This worldwide trend will lead to an increase in the number of older people requiring care for vision impairment (VI),2 defined as having a visual acuity of 6/12 or worse in the better eye. For many people, VI (largely due to age-related eye diseases, including macular degeneration and diabetic retinopathy) has a substantial impact on their quality of life and ability to live independently and safely in their own home. VI has been shown to restrict an individual's participation in daily activities; increase falls by almost twofold compared to fully sighted individuals; increase the risk of depressive symptoms; and contribute to placements in residential care facilities.3–9 With a rapidly growing elderly population, and increasing cost and demand for long-term care, novel solutions are needed to help older adults with VI remain independent and safe at home.10
To support independent living in older adults, researchers have begun to explore the role of in-home monitoring.11–13 The purpose of an in-home monitoring system (IMS) is passively to monitor an older adult in their home to detect changes in patterns of behavior (eg, sleeping difficulties, mobility issues) and high-risk situations (eg, falls, leaving the gas on), and to share information about the older adult with the older adult and their caregivers.11 IMS have the potential to support healthy longevity in the home, enhance security, safety and assistance for older adults, and contribute to economic savings for public healthcare systems.13 Presently, it is unclear how older adults with VI can gain most benefit from in-home monitoring or what issues they may face in the deployment of an IMS in their home, given the limited research in this growing segment of the community. Furthermore, current IMS are mostly developed from a technological viewpoint, and are not customized for older users.11 Few studies have attempted to assess the needs and preferences of older users regarding in-home monitoring. However, these studies have some limitations, including small sample sizes,14 the assessment of one user group only (generally the older adult),10 the assessment of people unlikely to require this technology (eg, healthy or young individuals),15 and assessing views on specific aspects of the technology only.10
Objective
The primary aim of this study was to develop a conceptual framework for the design of an IMS based on the requirements of older adults with VI, informal caregivers and eye-care rehabilitation professionals. To this effect, we employed concept mapping, a mixed-methods statistical research tool that allows the ideas of various stakeholders to be explored and integrated into one conceptual framework.16 17 A secondary aim was to survey a larger sample of older adults with VI and informal caregivers to yield further insights regarding IMS.
Materials and methods
Participants
Adults with VI aged 60 years or over (‘patients’) and informal caregivers (‘caregivers’) were recruited from the eye clinics of the Royal Victorian Eye and Ear Hospital (Victoria, Australia). Eye-care rehabilitation professionals (‘professionals’) were recruited from Able Australia (a support service for people living in the community with disabilities) and the Center for Eye Research Australia (CERA), and comprised a fairly even spread of case workers, service coordinators, orthoptists and optometrists. Eye-care rehabilitation professionals were purposefully targeted in this study given their awareness of the impact of VI on an individual's daily life. Ethical approval was provided by the Royal Victorian Eye and Ear Hospital Human Research and Ethics Committee (10/962H). All participants gave written informed consent.
Concept mapping
Concept mapping integrates an exploratory qualitative approach (ie, group brainstorming with stakeholders) with multidimensional scaling (MDS) and hierarchical cluster analysis (HCA).16 17 Concept mapping consists of three stages: data collection through brainstorming, item structuring through sorting and rating, and data analysis using the Concept Systems software package (V.4.0.175; http://www.conceptsystems.com). To reduce the potential for participant fatigue, the brainstorming and item structuring activities were conducted on separate days.
Stage 1: data collection
We sought stakeholder views regarding the following two seeding prompts: (1) ‘How can an IMS be used to enhance quality of life in people with low vision?’, and (2) ‘Concerns people may have related to the use of such technologies include…’. We held four group brainstorming sessions at CERA for patients and caregivers, and one session with professionals at Able Australia. Data saturation (ie, no new information emerged from brainstorming) was reached in this session. A total of 31 participants was recruited for brainstorming (16 patients, eight caregivers and seven professionals). Each session was attended by five to seven participants, and was completed in approximately 1.5 h. Four participants (one patient, one caregiver and two professionals) who could not attend any session were interviewed separately.
Each brainstorming session began with a detailed explanation of the study, which included the distribution of sample sensors among the participants, and the presentation of a 4-min video that was developed by the investigators to illustrate the basic operation and potential uses of an IMS. The video explained, in simple terms, that an IMS is typically equipped with unobtrusive wireless sensors positioned in different areas of the home to collect data about the resident (eg, mobility, use of appliances, time spent in bed, opening and closing of doors). The video then explained that a computer (also in the home) receives the monitoring data and transforms it into behavior patterns (after sufficient traces have been collected) to form the basis of a computational mechanism for detecting departures from the norm. If an abnormal behavior is detected (eg, the cooktop is left on), an alert will be issued in the home to notify the older adult (eg, by means of beeps or computer-generated voiced messages), and if the older adult does not respond, off-site caregivers or healthcare providers will be notified (eg, in the form of telephone or email alerts). After the video and a brief discussion (to allow participants to ask questions about IMS), participants wrote down their responses to the two seeding prompts, following which they shared their ideas with the group, presenting one idea at a time on a projector screen until all ideas were shared. A research assistant was available to assist those participants who needed help with writing or reading.
A total of 376 ideas (‘statements’) was collected and reviewed by two of the authors independently, who then by consensus removed 89 statements (23.7%) that were considered unclear or irrelevant, and combined 204 statements (54.3%) that were repetitious or overlapping. When necessary, statements were revised so that each statement succinctly expressed one clear idea in the form of a requirement (eg, statement 64 was converted from ‘I am worried that maintenance will be too expensive’ to ‘maintainence costs should be low’). The final list of 83 statements was printed onto a set of cards (one statement per card) for stage 2.
Stage 2: item structuring
In total, 24 participants were recruited for item structuring (10 patients, seven caregivers and seven professionals). Of these, 15 had previously participated in brainstorming (nine patients, four caregivers and two professionals). The remaining patients and caregivers were recruited in the same way as for brainstorming, and professionals were recruited from CERA. Most participants completed item structuring in a one-on-one interview with the researcher, but patients and caregivers of the same family were invited to attend an item structuring session together.
Participants were given a set of 83 cards and instructed to organize the cards into piles in any way that made sense to them (based on the conceptual similarities between the statements). The only restrictions were that the number of statement groups had to be greater than 1 and smaller than the number of statements, and there should not be a ‘miscellaneous’ pile. The goal of this task was to determine clusters or themes that emerge from the data and the relationships between these clusters. Following the sorting task, participants considered the relative importance of each statement for supporting independent living in older people with VI, and assigned each statement a rating on a five-point Likert scale that ranged from relatively ‘unimportant’ (1) to ‘extremely important’ (5).
Stage 3: data analysis
The results of stage 2 were entered into the Concept Systems software package to create a concept map depicting the composite thinking of the stakeholders. This package uses MDS and HCA to analyze the themes and patterns among the statements.18 MDS positions the statements on a map based on the sorting results, such that statements that have been frequently sorted in the same pile are positioned close to each other. Goodness-of-fit of the resulting configuration of statements was assessed by its stress value, in which lower values indicate that the configuration adequately represents individual sorting results (stress values <0.35 are considered favourable).18 HCA then aggregates the statements into groups of ideas or ‘clusters’ on the basis of the inter-statement distances, with the number of clusters being configurable. We set the Concept Systems software package to generate cluster maps ranging from two to 15 clusters. One of the authors, together with three professionals who took part in stage 2, examined each cluster map qualitatively to select one cluster configuration that made the most sense conceptually (ie, a cluster configuration that does not result in the loss of potentially relevant themes due to too few clusters, or a configuration that is difficult to interpret due to conceptual overlap across several clusters). Once the final cluster map was selected, each cluster in the map was named on the basis of its content, and the average importance rating for each statement and cluster was calculated, yielding a comprehensive and useful representation of ideas, the relationships between them, and their relative importance.
Questionnaire
We developed a series of questions to yield further insights regarding IMS. The questions were based on the literature and a previously developed questionnaire assessing user views on IMS.19 Our questionnaire was adapted for professionals, but due to a low response rate, we excluded them from our analysis. A total of 78 patients and 25 caregivers completed the questionnaire, including all participants who took part in concept mapping. To reduce fatigue, these participants completed the questionnaire following a lunch break after their session. The remaining patients and caregivers completed the questionnaire with a research assistant at CERA or at home. Unless described otherwise, patients and caregivers answered each question with either ‘yes’, ‘no’ or ‘unsure’.
Acceptance of an IMS
In the questionnaire, patients and caregivers were asked if they thought that an IMS would be beneficial to the patient, and answered this question with ‘yes, now’, ‘yes, in the future’, ‘no’ or ‘unsure’. The same format was used by caregivers to indicate whether they believed that an IMS would be of benefit to them (as caregivers).
Reasons for accepting or rejecting an IMS
Participants selected their reasons for accepting an IMS from a list of eight reasons (eg, maintain independence, live a safer life). They could also write down other reasons for accepting or rejecting an IMS. Participants were asked if they thought that an IMS could, overall, help the patient live a safer life, live independently for longer, and improve the patient's quality of life.
Usefulness of receiving notifications and alerts
Participants indicated the usefulness of receiving notifications and alerts regarding numerous situations (eg, appointment reminders) using the following answer format: ‘useful’, ‘not useful’ or ‘unsure’.
Activities acceptable to monitor
Participants indicated the acceptability of monitoring 11 activities in the home (eg, movement around the home), and had the option to list other activities that were acceptable or unacceptable to monitor. On a five-point Likert scale that ranged from ‘unimportant’ (1) to ‘critical’ (5), patients rated how important it is that they control the activities being monitored and when they are monitored, and caregivers rated how important it is that they control what information they receive and how often they receive it.
Concerns regarding an IMS
Participants indicated their level of concern with 11 potential issues (eg, privacy, costs) using the answer format ‘not at all concerned’, ‘concerned’ and ‘very concerned’. Participants also had the option to list other issues and their level of concern with each one.
Information sharing
From a list of 12 recipients (eg, adult children), participants nominated who they would choose to receive information obtained from monitoring. Participants could also nominate other recipients.
Sociodemographic and clinic information
Age, gender, cause of VI and presenting binocular visual acuity was obtained from the patient's hospital file.
Statistical analysis
Descriptive statistics for patients and caregivers were calculated, and any differences between the groups were assessed using the χ2 test or Fisher's exact test. Statistical significance of p≤0.05 was used and is reported in this paper when statistical significance was achieved. Continuous variables (ie, age and duration of VI) are presented as medians (IQR) for non-normally distributed data, and categorical variables are presented as absolute (n) or relative (%) frequencies. All statistical analyses were conducted using Stata release 11.
Results
Participants
A total of 115 participants was recruited for this study. Most patients who completed the brainstorming, sorting/rating tasks and questionnaire were men (75.0%, 80.0% and 65.4%, respectively) and had mild (6/12–6/18) to moderate (6/19–6/60) VI. In contrast, most caregivers were women (62.5%, 57.1% and 72.0%, respectively), and all professionals were women. Table 1 displays the sociodemographic and clinical characteristics of patients and caregivers.
Table 1.
Sociodemographic and clinical characteristics of patients and caregivers
| Concept mapping | ||||||
|---|---|---|---|---|---|---|
| Data collection | Item structuring | Questionnaire | ||||
| Patient (n=16) | Caregiver (n=8) | Patient (n=10) | Caregiver (n=7) | Patient (n=78) | Caregiver (n=25) | |
| Median (IQR) | ||||||
| Age, years | 72 (14.5) | 69 (22) | 67 (16) | 51 (18) | 74.5 (16) | 60 (19) |
| Duration of vision impairment, years | 6.5 (11.4) | 6 (8.8) | 5 (8.0) | |||
| N (percentage*) | ||||||
| Gender (male) | 12 (75) | 3 (38) | 8 (80) | 3 (43) | 51 (65) | 7 (28) |
| Country of birth (Australia) | 8 (50) | 4 (50) | 5 (50) | 6 (86) | 41 (53) | 13 (52) |
| Marital status | ||||||
| Single, never married | 3 (19) | 0 (0) | 2 (20) | 0 (0) | 7 (9) | 2 (8) |
| Separated/divorced | 2 (13) | 0 (0) | 1 (10) | 0 (0) | 7 (9) | 3 (12) |
| Widowed | 2 (13) | 0 (0) | 1 (10) | 0 (0) | 15 (19) | 0 (0) |
| Married | 9 (56) | 8 (100) | 6 (60) | 7 (100) | 49 (63) | 20 (80) |
| Education | ||||||
| None/primary school | 1 (6) | 0 (0) | 1 (10) | 0 (0) | 6 (8) | 0 (0) |
| Some secondary school | 4 (25) | 2 (25) | 2 (20) | 3 (43) | 24 (31) | 10 (40) |
| Secondary school completed | 5 (31) | 3 (38) | 3 (30) | 4 (57) | 9 (12) | 5 (20) |
| Trade/some university | 3 (19) | 2 (25) | 1 (10) | 0 (0) | 24 (31) | 5 (20) |
| University degree or higher | 3 (19) | 1 (13) | 3 (30) | 0 (0) | 14 (18) | 5 (20) |
| Did not answer | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) |
| Self-rated health | ||||||
| Excellent | 3 (19) | 2 (25) | 2 (20) | 1 (14) | 11 (14) | 7 (28) |
| Very good | 2 (13) | 1 (13) | 2 (20) | 3 (43) | 18 (23) | 6 (24) |
| Good | 7 (44) | 4 (50) | 4 (40) | 1 (14) | 27 (35) | 8 (32) |
| Fair | 3 (19) | 0 (0) | 0 (0) | 1 (14) | 15 (19) | 3 (12) |
| Poor | 1 (6) | 1 (13) | 2 (20) | 1 (14) | 6 (8) | 1 (4) |
| Did not answer | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 1 (1) | 0 (0) |
| Primary cause of vision impairment | ||||||
| Age-related macular degeneration | 7 (448) | 6 (60) | 34 (44) | |||
| Diabetic retinopathy | 7 (44) | 2 (20) | 24 (31) | |||
| Glaucoma | 2 (13) | 2 (20) | 8 (10) | |||
| Retinitis pigmentosa | 0 (0) | 0 (0) | 8 (10) | |||
| Other | 0 (0) | 0 (0) | 4 (5) | |||
| Binocular visual acuity (better eye) | ||||||
| Mild (6/12–6/18) | 8 (50) | 6 (60) | 24 (31) | |||
| Moderate (6/19–6/60) | 7 (44) | 3 (30) | 37 (47) | |||
| Severe (>6/60) | 1 (6) | 1 (10) | 17 (22) | |||
*Percentages may not total 100 due to rounding.
Concept mapping
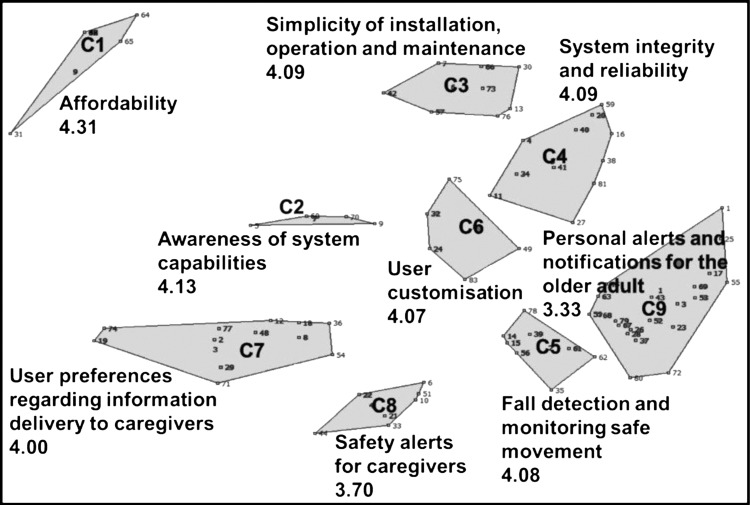
The MDS positioning of the 83 statements had a stress value of 0.22, indicating that the item structuring was adequately represented. A nine-cluster map was selected. Inspection of the clusters revealed that some clusters contained statements that were conceptually more similar to statements in one of the nearby clusters. This led to the re-allocation of 15 statements into conceptually more appropriate clusters. Five of the nine clusters represented generic requirements, that is, ‘affordability’ (cluster 1; C1), ‘awareness of system capabilities’ (C2), ‘simplicity of installation, operation and maintenance’ (C3), ‘system integrity and reliability’ (C4), and ‘user customization’ (C6). The remaining four clusters represented potential services provided by an IMS, that is, ‘fall detection and monitoring safe movement’ (C5), ‘user preferences regarding information delivery to caregivers’ (C7), ‘safety alerts for caregivers’ (C8), and ‘personal alerts and notifications for the older adult’ (C9). Most of the re-allocated statements were moved from C5 to C9, as they pertained to matters of convenience, rather than safety. Figure 1 shows the nine-cluster configuration, and table 2 lists the number of statements in each cluster and its average importance rating, and shows two sample statements for each cluster.
Figure 1.
Spatial location of the 83 statements in the nine clusters.
Table 2.
Clusters and sample statements with average importance ratings
| No. | Statement | Total no. of statements in cluster | Importance* |
|---|---|---|---|
| Cluster 1: Affordability | 7 | 4.31 | |
| 46 | The costs of the sensors, computer and installation of these devices should be affordable for pensioners | 4.63 | |
| 47 | Financial support should be provided to users of this system for the purchasing, installation and running of the system | 4.46 | |
| Cluster 2: Awareness of system capabilities | 4 | 4.13 | |
| 9 | The limitations of the system should be clearly communicated to the older adult | 4.46 | |
| 60 | The older adult and/or caregiver should be given clear instruction about what to do if the system should stop working | 4.38 | |
| Cluster 3: Simplicity of installation, operation and maintenance | 8 | 4.09 | |
| 13 | The system should be easy to operate | 4.46 | |
| 76 | In the event that one sensor fails, the rest of the sensors will continue to function normally | 4.38 | |
| Cluster 4: System integrity and reliability | 11 | 4.09 | |
| 40 | The system should continue to work during blackouts | 4.63 | |
| 27 | The system should be able to tell the difference between an emergency and non-emergency situation reliably | 4.42 | |
| Cluster 5: Fall detection and monitoring safe movement | 8 | 4.08 | |
| 35 | The system can detect if the older adult has a fall in the home | 4.54 | |
| 39 | The system can monitor the older adults’ safety in the bathroom and toilet (eg, detect slipping) | 4.42 | |
| Cluster 6: User customization | 5 | 4.07 | |
| 49 | If the older adult turns the monitoring system off, the system can remind the older adult to turn it back on again | 4.25 | |
| 32 | The older adult should nominate how they would like alerts issued in their home (ie, audio, visual, vibration) | 4.17 | |
| Cluster 7: User preferences regarding information delivery to caregivers | 12 | 4.00 | |
| 77 | The older adult should choose who they would like to receive information about themselves, including the circumstances for when this information is sent | 4.04 | |
| 18 | Caregivers can choose how they would like to receive notifications and alerts about the older adult (eg, email, text message) | 4.00 | |
| Cluster 8: Safety alerts for caregivers | 7 | 3.70 | |
| 51 | The system can let the caregiver know when the older adult has stayed too long in the bathroom or toilet | 3.92 | |
| 33 | The system can let the caregiver know if the older adult stays too long in bed | 3.79 | |
| Cluster 9: Personal alerts and notifications for the older adult | 21 | 3.33 | |
| 68 | The system can let the older adult know if they leave the stove or gas on for too long | 4.38 | |
| 26 | The system can let the older adult know when appliances have been left on (eg, the iron) | 4.21 | |
*Mean importance rating on a scale from 1 (unimportant) to 5 (very important) as rated by 24 participants. Itaic values are mean important ratings for items within the respective clusters.
Importance rating
Clusters representing generic requirements, namely ‘affordability’ (mean importance rating 4.31), ‘awareness of system capabilities’ (4.13), ‘simplicity of installation, operation and maintenance’ (4.09), ‘system integrity and reliability’ (4.09), and ‘user customization’ (4.07) had the highest average importance ratings. ‘Fall detection and monitoring safe movement’ (4.08) had the highest average importance rating among the clusters representing potential services provided by an IMS. Interestingly, ‘safety alerts for caregivers’ (3.70) and ‘personal alerts and notifications for the older adult’ (3.33) had the lowest average importance ratings overall.
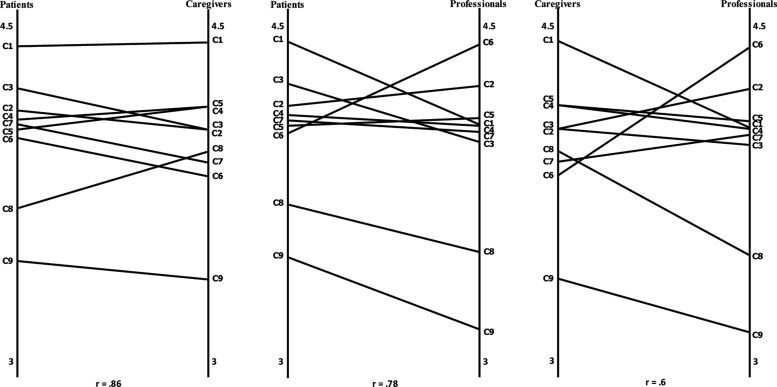
Figure 2 shows the association (Pearson's product moment correlation) between the mean importance ratings of each cluster for each group of stakeholders. A strong association was observed between patients’ and caregivers’ ratings (r=0.86) and between patients’ and professionals’ ratings (r=0.78), while only a moderate association was observed between caregivers’ and professionals’ ratings (r=0.60). Patients and caregivers rated the concept ‘affordability’ higher than professionals, who rated the concept ‘user customization’ higher than patients and caregivers. In addition, patients rated ‘simplicity of installation, operation and maintenance’ higher than caregivers and professionals, highlighting the importance to the older adult of being able to operate the IMS; and caregivers rated ‘safety alerts for caregivers’ higher than both patients and professionals, underscoring the importance to caregivers of receiving notifications and alerts regarding abnormal behavior of the patient.
Figure 2.
Association between average cluster importance ratings and patients and caregivers, patients and professionals and caregivers and professionals. Importance was rated on a scale from 1 to 5, in which 1 is relatively unimportant and 5 is extremely important.
Questionnaire
Acceptance of an IMS
Most patients and caregivers thought that an IMS would benefit the patient in the future (62.8% and 64.0%, respectively) with only a minority nominating now (9.0% and 28.0%, respectively). Remaining patients (28.2%) and caregivers (8.0%) were unsure or did not think an IMS would benefit the patient. Likewise, most caregivers (56.0%) believed an IMS would benefit them (the caregiver) in the future, with only a third (32.0%) thinking an IMS would benefit them now. The remaining 12.0% of caregivers were unsure or did not think an IMS would be of benefit to them. Compared to patients, caregivers were more likely to think that an IMS would be of benefit to the patient now or in the future (p=0.038).
Reasons for accepting or rejecting an IMS
Most patients and caregivers gave the following reasons for accepting an IMS: ‘detect falls or other potentially dangerous situations’ (85.1% and 95.7%, respectively), ‘safety’ (76.1% and 91.3%, respectively), ‘maintain independence’ (86.6% and 56.5%, respectively; p=0.002), ‘peace of mind for the family’ (74.6% and 82.6%, respectively), and ‘assist with visual or hearing impairments’ (68.7% and 73.9%, respectively). Less than half of the patients and caregivers selected the following reasons: ‘remind the patient and caregiver of upcoming appointments’ (47.8% and 43.5%, respectively), ‘manage medications’ (43.3% and 39.1%, respectively), and ‘reduce isolation’ (40.3% and 21.7%, respectively).
Most patients (71.8%) and less than half of the caregivers (44.0%) had reasons to reject an IMS, with some reporting more than one reason. Of these, the most frequently reported reasons were ‘lack of perceived need’ (n=23 and n=3, respectively) and ‘cost’ (n=18 and n=5, respectively).
The majority of patients and caregivers agreed that an IMS would help the older adult live a safer (70.5% and 76.0%, respectively) and more independent (69.2% and 72.0%, respectively) life, but only about half the patients and caregivers (46.2% and 52.0%, respectively) thought that monitoring the patient in the home would improve the patient's quality of life.
Usefulness of receiving notifications and alerts
Most patients (79.5%) and caregivers (96.0%) regarded alerts concerning emergency situations (eg, threats to safety) as useful. In contrast, fewer patients and approximately half of the caregivers regarded notifications regarding the patient's upcoming appointments (48.7% and 52.0%, respectively), whether the patient is not eating or sleeping well (34.6% and 52.0%, respectively), and routine activities (eg, taking medication; 35.9% and 44.0%, respectively) as useful.
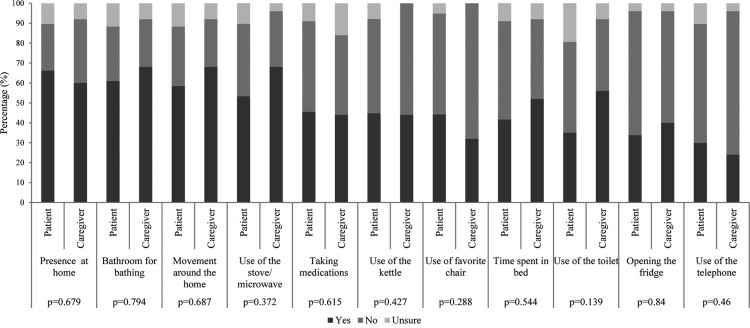
Activities acceptable to monitor
Most patients gave a rating from ‘important’ (3) to ‘critical’ (5) to their ability to control which activities are monitored in the home, as well as when they are monitored (80.7% and 82.1%, respectively). In general, less than half of the patients and caregivers found it acceptable to monitor routine daily activities (eg, use of kettle, fridge; figure 3). An exception was the use of the bathroom for bathing (61.0% and 68.0%, respectively), which is a potentially hazardous activity. This, together with the patients’ and caregivers’ acceptance of monitoring presence in the house (66.2% and 60.0%, respectively) and movement around the house (58.4% and 68.0%, respectively), is consistent with the stakeholders’ concerns regarding fall detection and safety—the most highly rated cluster among the clusters pertaining to services provided by an IMS.
Figure 3.
Acceptability of monitoring activities in your home.
Most caregivers gave a rating from ‘important’ (3) to ‘critical’ (5) to their ability to control what information about the patient they receive and how often they receive it (84.0% and 88.0%, respectively).
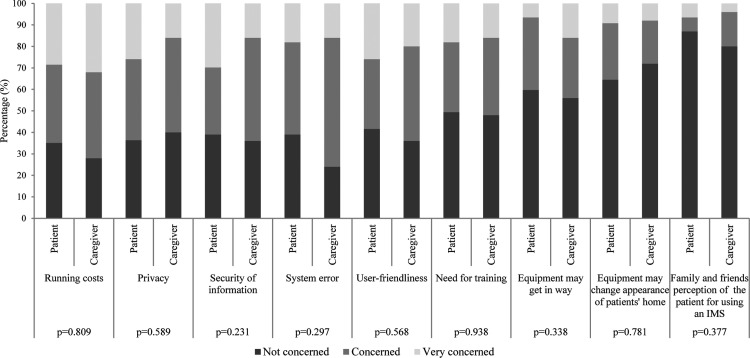
Concerns regarding an IMS
Patients and caregivers were more concerned with how accessible and useable the IMS would be (eg, cost, privacy, security, accuracy and ease of operation) than with the aesthetics of the system or the imposition of transmitting or receiving the information obtained from monitoring (figure 4).
Figure 4.
Patient and caregiver concerns regarding an in-home monitoring system (IMS).
Information sharing
Some categories of recipients did not apply to all participants (eg, five patients did not have adult children). The denominator used to calculate the following proportions was based on the total number of patients and caregivers for which the recipient of information was applicable. Most patients and caregivers nominated the patient's adult children (80.8% and 73.9%, respectively), their own selves (70.5% and 96.0%, respectively), and emergency services (60.3% and 56.0%). Compared to caregivers, more patients nominated the patient's spouse/significant other (78.6% and 52.9%, respectively; p=0.038) and healthcare providers (eg, general practitioner; 61.5% and 48.0%, respectively). The following recipients were less popular with patients and caregivers: a hospital (37.7% and 37.5%, respectively), friends of the patient (32.4% and 13.6%, respectively), neighbors (34.7% and 23.8%, respectively), the patient's siblings (29.5% and 11.1%, respectively), other relatives (19.4% and 9.5%, respectively), and volunteer caregivers (19.4% and 25.0%, respectively).
Discussion
Most IMS now are not designed for end users, especially older adults with functional or sensory impairments.20 This is the first study to canvass the views of older adults with VI, caregivers and eye-care rehabilitation professionals regarding in-home monitoring using concept mapping. Overall, participants were positive towards the concept of in-home monitoring, mainly for the enhancement of independence and safety in the home, but had some concerns that must be addressed when developing an IMS.
Concept mapping revealed nine conceptual dimensions to guide the design of an IMS for older adults with VI. Five clusters represent generic requirements while four clusters pertain to potential services provided by an IMS. The most important concepts to participants were those representing generic requirements, namely ‘affordability.’ Our findings, which are corroborated by results from the questionnaire, indicate that in the context of older adults with VI, the perceived benefits from an IMS are secondary to general concerns regarding affordability,10 usability,11 20–22 and privacy and security,15 21–23 highlighting the significance of these issues to users.
Fall detection and safety were recurring motifs in this study and were the main reasons to accept an IMS. Likewise, ‘fall detection and the monitoring of safe movement’ was the most important concept among the potential services provided by an IMS. Falls pose a significant health hazard for older adults24 25 and understandably are potential benefits of an IMS.11 19 20
According to participants, alerts concerning emergency situations are more useful than systems that monitor routine activities, which is also in support of previous research.22 23 We speculate that the patients and caregivers in this study considered the monitoring of routine activities unnecessary given that most patients were living with someone (and may not need to perform some of these tasks), or determined the monitoring of these activities an invasion of privacy. Considering that most participants saw the potential for in-home monitoring in the future, we posit that people living on their own or people who are more restricted due to functional limitations are more likely to find value in the monitoring of emergency situations and routine activities.
The strengths of this study included the use of concept mapping and the use of three stakeholder groups for concept mapping. The study, however, had some limitations. First, users had either limited or no previous knowledge of IMS. Although we attempted to familiarize our participants with the envisaged capabilities of an IMS before data collection, they may not have fully realized the potential of an IMS to contribute to their own lives or, more generally, to the lives of older adults with VI and their caregivers. Our study also had low representation from individuals living on their own (whose experiences and needs are likely to differ from those of people who live with another person), and no representation from healthcare professionals other than eye-care rehabilitation practitioners (eg, primary care physicians), who may be interested in the information obtained from monitoring. Finally, as we were asking participants for their views on a hypothetical system, it is possible that issues and attitudes regarding a deployed IMS may differ from those identified in the current study. Future feasibility and participatory evaluation studies with older adults with VI, caregivers and healthcare professionals will enable developers to determine the acceptability of particular design features to create products that are suited to people with varying needs.
Conclusion
In summary, this study defined a conceptual framework for the design of an IMS based on the preferences and requirements of older adults with VI, informal caregivers and eye-care rehabilitation professionals. Our findings provide for the first time a basis for the design of an acceptable and useful IMS for older adults with VI.
Acknowledgments
The authors would like to thank the participants for their involvement in this study, and Mr Gerald Thompson and Mr Ashley Zukerman for their work in producing the demonstration video that was used during the brainstorming sessions.
Footnotes
Contributors: All authors contributed to the study design and interpretation of data and gave final approval of the version to be published. Implementation and data analysis: MFL, LB, FB and IZ. Writing of manuscript: MFL, IZ and GR.
Funding: This research was supported in part by grant LP100200405 from the Australian Research Council, and endowments from Meticube, Portugal, VicHealth and the Helen McPherson Smith Trust. CERA receives Operational Infrastructure Support from the Victorian Government.
Competing interests: None.
Ethics approval: Ethics approval was provided by the Royal Victorian Eye and Ear Hospital Human Research and Ethics Committee (10/962H).
Patient consent Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pollack ME. Intelligent technology for an aging population: the use of AI to assist elders with cognitive impairment. AI Magazine 2005;26:9–24 [Google Scholar]
- 2.Taylor HR, Keeffe JE, Vu HTV, et al. Vision loss in Australia. Med J Aust 2005;182:565–8 [DOI] [PubMed] [Google Scholar]
- 3.Burmedi D, Becker S, Heyl V, et al. Emotional and social consequences of age-related low vision: a narrative review. Vis Impair Res 2002;4:47–71 [Google Scholar]
- 4.Heyl V, Wahl HW. Psychosocial adaptation to age-related vision loss: a six-year perspective. J Vis Impair Blind 2001;95:739–48 [Google Scholar]
- 5.Lamoureux EL, Chong E, Wang JJ, et al. Visual impairment, causes of vision loss, and falls: the Singapore Malay Eye Study. Invest Ophthalmol Vis Sci 2008;49:528–33 [DOI] [PubMed] [Google Scholar]
- 6.Lamoureux EL, Hassell JB, Keeffe JE. The determinants of participation in activities of daily living in people with impaired vision. Am J Ophthalmol 2004;137:265–70 [DOI] [PubMed] [Google Scholar]
- 7.Rovner BW, Ganguli M. Depression and disability associated with impaired vision: the MoVies project. J Am Geriatr Soc 1998;46:617–19 [DOI] [PubMed] [Google Scholar]
- 8.Wang JJ, Mitchell P, Cumming RG, et al. Visual impairment and nursing home placement in older Australians: the Blue Mountains Eye Study. Ophthalmic Epidemiol 2003;10:3–13 [DOI] [PubMed] [Google Scholar]
- 9.West SK, Munoz B, Rubin GS, et al. Function and visual impairment in a population-based study of older adults. The SEE project. Salisbury Eye Evaluation. Invest Ophthalmol Vis Sci 1997;38:72–82 [PubMed] [Google Scholar]
- 10.Mann WC, Belchoir P, Tomita MR, et al. Older adults’ perception and use of PDAs, home automation system, and home health monitoring system. Top Geriatr Rehabil 2007;23:35–46 [Google Scholar]
- 11.Demiris G, Skubic M, Rantz M, et al. Smart home sensors for the elderly: a model for participatory formative evaluation. Proceedings of the IEEE EMBS International Special Topic Conference on Information Technology in Biomedicine Ioannina, Greece, 2006 [Google Scholar]
- 12.Ohta S, Nakamoto H, Shinagawa Y, et al. A health monitoring system for elderly people living alone. J Telemed Telecare 2002;8:151–6 [DOI] [PubMed] [Google Scholar]
- 13.Sixsmith A. An evaluation of an intelligent home monitoring system. J Telemed Telecare 2000;6:63–72 [DOI] [PubMed] [Google Scholar]
- 14.Courtney K, Demiris G, Rantz M, et al. Needing smart home technologies: the perspective of older adults in continuing care retirement communities. Inform Prim Care 2008;16:195–201 [DOI] [PubMed] [Google Scholar]
- 15.Ziefle M, Röcker C, Holzinger A. Medical technology in smart homes: exploring the user's perspective on privacy, intimacy and trust. In: Proceedings of the 3rd International IEEE Workshop on Security Aspects of Process and Services Engineering (SAPSE 2011), 35th Annual IEEE Computer Software and Applications Conference Munich, Germany, 2011 [Google Scholar]
- 16.Petrucci CJ, Quinlan KM. Bridging the research-practice gap: concept mapping as a mixed methods strategy in practice-based research and evaluation. J Soc Serv Res 2007;34:25–42 [Google Scholar]
- 17.Trochim W, Kane M. Concept mapping: an introduction to structured conceptualization in health care. Int J Qual Health Care 2005;17:187–91 [DOI] [PubMed] [Google Scholar]
- 18.Kane M, Trochim WMK. Concept mapping for planning and evaluation. Thousand Oaks, California: Sage Publications, Incorporated 2006 [Google Scholar]
- 19.Alwan M, Turner B, Kell S, et al. Development of survey instruments to guide the design of health status monitoring systems for the elderly: content validity evaluation. Proceedings of the 2nd IEEE International Conference on Information and Communication Technologies: from Theory to Applications—ICTTA06 Damascus, Syria, 2006 [Google Scholar]
- 20.Demiris G, Rantz MJ, Aud MA, et al. Older adults’ attitudes towards and perceptions of ‘smart home’ technologies: a pilot study. Med Inform Internet Med 2004;29:87–94 [DOI] [PubMed] [Google Scholar]
- 21.Soar J, Croll P. Assistive technologies for the frail elderly, chronic illness sufferers and people with disabilities: a case study of the development of a Smart Home. In: ACIS 2007: Proceedings of the 18th Australasian Conference on Information Systems: The 3 Rs: Research, Relevance and Rigour – Coming of Age. Toowoomba, Australia, 2007 [Google Scholar]
- 22.Wild K, Boise L, Lundell J, et al. Unobtrusive in-home monitoring of cognitive and physical health: reactions and perceptions of older adults. J Appl Gerontol 2008;27:181–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marschollek M, Wolf KH, Plischke M, et al. People's perceptions and expectations of assistive health-enabling technologies: an empirical study in Germany. Assist Technol 2009;21:86–93 [DOI] [PubMed] [Google Scholar]
- 24.Legood R, Scuffham P, Cryer C. Are we blind to injuries in the visually impaired? A review of the literature. Inj Prev 2002;8:155–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tinetti ME, Powell L. Fear of falling and low self-efficacy: a case of dependence in elderly persons. J Gerontol 1993;48:35–8 [DOI] [PubMed] [Google Scholar]