Abstract
Objective
Electronic health records (EHR) hold great promise for managing patient information in ways that improve healthcare delivery. Physicians differ, however, in their use of this health information technology (IT), and these differences are not well understood. The authors study the differences in individual physicians' EHR use patterns and identify perceptions of uncertainty as an important new variable in understanding EHR use.
Design
Qualitative study using semi-structured interviews and direct observation of physicians (n=28) working in a multispecialty outpatient care organization.
Measurements
We identified physicians' perceptions of uncertainty as an important variable in understanding differences in EHR use patterns. Drawing on theories from the medical and organizational literatures, we identified three categories of perceptions of uncertainty: reduction, absorption, and hybrid. We used an existing model of EHR use to categorize physician EHR use patterns as high, medium, and low based on degree of feature use, level of EHR-enabled communication, and frequency that EHR use patterns change.
Results
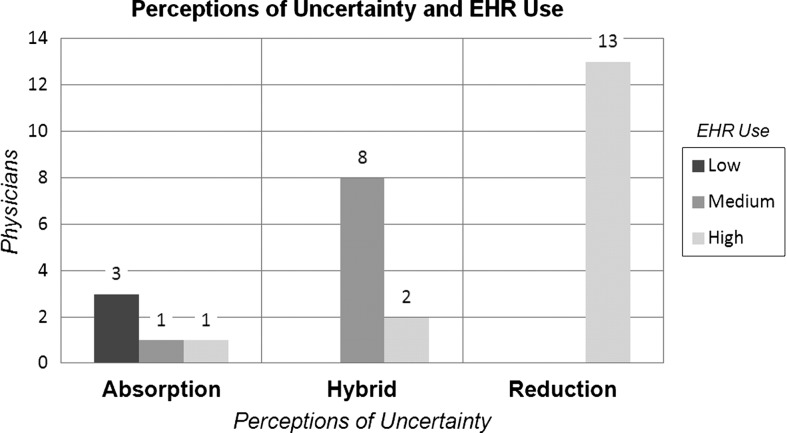
Physicians' perceptions of uncertainty were distinctly associated with their EHR use patterns. Uncertainty reductionists tended to exhibit high levels of EHR use, uncertainty absorbers tended to exhibit low levels of EHR use, and physicians demonstrating both perspectives of uncertainty (hybrids) tended to exhibit medium levels of EHR use.
Conclusions
We find evidence linking physicians' perceptions of uncertainty with EHR use patterns. Study findings have implications for health IT research, practice, and policy, particularly in terms of impacting health IT design and implementation efforts in ways that consider differences in physicians' perceptions of uncertainty.
Keywords: electronic health record use, physician perceptions of uncertainty, complexity science, uncertainty management, ambulatory care
Introduction
Despite recent increases in electronic health record (EHR) implementation1–3 spurred by the Health Information Technology for Economic and Clinical Health Act (HITECH),4 the relationship between EHR use and healthcare quality remains inconsistent.5–8 Insufficient knowledge of how the human element of medical practice intersects with physicians’ EHR use could be contributing to this inconsistency.9–11 Previous research provides foundational insights into many of the socio-technical factors important in EHR design, implementation, and use, including unexpected changes in clinical workflow,12 13 the role of work relationships and communication patterns in practice-level EHR use,14 and the reality of negative unintended consequences.15 16 In spite of major advances made through the application of socio-technical theory to health IT topics,17–20 significant knowledge gaps at the intersection of human behavior and health IT persist, particularly with regard to understanding physicians’ information needs in the context of EHR-enabled healthcare delivery.21
Drawing on statements in a recent report from the Office of the National Coordinator for Health Information Technology (ONC) articulating a lack of understanding of the human element in health IT dissemination and implementation efforts,11 this study seeks to contribute new knowledge at the intersection of human behavior and health IT use in understudied ambulatory care settings.22 We conducted a multi-method qualitative study to better understand individual physician-level differences in EHR use patterns.
Theoretical frameworks
We drew insights from two distinct literatures in conducting this study: complexity science and physicians’ perceptions of uncertainty. Complexity science framed our study from the beginning, influencing data collection and analysis activities. Physicians’ perceptions of uncertainty, however, emerged as a theoretical frame during data analysis. We used both literatures to help interpret our study findings. Although these two frameworks were applied at different points in the study, we introduce them both here.
Complexity science
Complexity science is the study of complex systems,23–27 and has been applied to organizational studies25 27 and information systems research28–31 for over two decades and more recently to medical informatics research.14 19 Complex systems are comprised of heterogeneous and interdependent parts, where the interactions among the parts influence the functioning of the system at local and global levels in unpredictable ways.23 Prior to the introduction of complexity science, the dominant conceptualization of organizations was that of mechanistic systems characterized by predictability.32 From a complexity science perspective, organizations are complex systems made up of diverse agents and non-linear dynamics.23 25 As agents interact locally over time they self-organize, forming global patterns of organizing33; they express emergent properties, properties at one level of a system that cannot be understood by analyzing the same property at another level of the system34 35; and they co-evolve with their environments.28 31
Complexity science principles guided our research efforts in two key ways. First, they shaped the design of our data collection instruments. Rather than developing highly structured interview and observation templates, we developed loosely structured and open-ended data collection guides to increase our likelihood of observing something novel and important. Second, and at a later point in the study, complexity science provided a starting point for understanding the differences in how physicians view the role of information in caring for patients and how they perceive and manage uncertainty25 27 36 in this process. Healthcare delivery systems are complex systems characterized by reducible and irreducible uncertainty, and physicians face both types of uncertainty when they care for patients.23 36 37 The non-linear interdependencies in complex social systems are a major contributor to uncertainty, particularly uncertainty that cannot be reduced with information.23 25 36 We used complexity science and its considerations of uncertainty in our data analysis and interpretation efforts.
Physicians’ perceptions of uncertainty
Healthcare delivery systems are complex systems characterized by uncertainty.36–40 As Eddy described it:
“Uncertainty creeps into medical practice through every pore. Whether a physician is defining a disease, making a diagnosis, selecting a procedure, observing outcomes, assessing probabilities, assigning preferences, or putting it all together, he is walking on very slippery terrain. It is difficult for nonphysicians, and for many physicians, to appreciate how complex these tasks are, how poorly we understand them, and how easy it is for honest people to come to different conclusions.”41
Moreover, uncertainty takes many forms in healthcare,36 37 40 41 and has been attributed to three main sources: the complexity of the system itself, the unpredictable trajectories of illnesses, and the limits of scientific knowledge.37 Uncertainty that arises from correctly diagnosing a medically complex patient differs from the uncertainty resulting from a missing laboratory value. In the latter situation, a new test can be ordered and the laboratory value can be obtained, resolving the uncertainty of the laboratory value. In the former situation, the information the physician needs to correctly diagnose the patient may be non-existent; it simply is nowhere to be found. Regardless of the amount of data aggregated or information gathered and processed, some uncertainty in healthcare delivery is irreducible.24 36
Previous research clearly demonstrates that physicians differ in how they perceive and respond to uncertainty.42–45 Examples of how these differences are manifest in practice can be seen in the types and amounts of information sought by physicians for medical decision-making46 47 and in the differences in procedure rates among physicians.48 Physician's information needs play a role in how they perceive and manage uncertainty. Although the relationship between physicians’ perceptions of uncertainty and practice behaviors is recognized, its role in health IT use is not fully understood. We used the physicians’ perceptions of uncertainty literature in conjunction with the complexity science literature to inform data analysis, particularly in terms of selective coding of the data and interpreting results.
Methods
Study design
We conducted a multi-method qualitative study using comparative analysis49 50 to examine individual-level differences in EHR use patterns by physicians working in the same ambulatory care organization, HealthGroup (pseudonym). Previous analyses of practice-level EHR use from the same study have already been published.14 In summary, this previous analysis found that practice-level communication patterns were associated with practice-level EHR use patterns, contributing new knowledge of social factors associated with practice-level EHR use patterns. This previous analysis was deductive49 in that it examined practice communication patterns using an existing model of work relationships.51 The model of EHR use applied in the current analysis of individual physicians’ EHR use was adapted from the previous analyses of practice-level EHR use (details are provided in the ‘Analytical approach’ section below).
The current analysis of individual-level EHR use patterns by physicians was inductive49 in nature. Because we sought a contextually rich understanding of EHR use and aimed to identify new variables important in explaining differences in individual physicians’ EHR use, a qualitative approach was appropriate.52 We collected data in eight purposefully selected53 practices (out of 17) operating within HealthGroup. We selected practices based on their perceived ability to provide a wide range of EHR use patterns53 supported by conversations with HealthGroup's IT department staff. Given that HealthGroup implemented its EHR system 7 years before the start of data collection, the IT department had accumulated considerable experience working with its physicians, and had developed a working knowledge of the differences in how physicians were using the EHR (or not) in their clinical work. Because we sought an understanding of EHR use that included nuanced social and behavioral aspects of how physicians assimilated EHRs into their work routines, we did not use EHR usage logs in this selection process. Rather, we selected practices based on their perceived ability to provide opportunities for us to observe wide-ranging differences in physicians’ EHR use patterns (eg, differences in the extent to which physicians integrated EHR use into clinical work, differences in level of feature use, and differences in tailoring/modifying templates for clinical documentation) across the organization. Selection criteria aimed at maximizing diversity in the main variable of interest (EHR use) is typical in qualitative research using comparative analysis methods.53
We enrolled primary care physicians (n=9) and sub-specialists (n=19) to study differences in EHR use in a diversity of medical specialties. Sub-specialists were endocrinologists, gastroenterologists, rheumatologists, neurologists, and podiatrists. Table 1 provides the clinician demographic data. The first author (HJL) spent 4 weeks in each practice interviewing and observing physicians during normal work activities, spending on average 5–6 h/day for 4 days each week in each practice (640–768 h total time in the field). Semi-structured interviews were conducted with all physicians in each practice. Field notes from direct observation provided additional data.
Table 1.
Clinician demographic data
| Practice | Gender | Age | Practice | Gender | Age |
|---|---|---|---|---|---|
| Family practice 1 | Male | 40–49 | Specialty practice 2 | Male | 60–69 |
| Family practice 1 | Male | 40–49 | Specialty practice 3 | Male | 30–39 |
| Family practice 1 | Female | 30–39 | Specialty practice 3 | Male | 50–59 |
| Family practice 2 | Male | 50–59 | Specialty practice 3 | Female | 30–39 |
| Family practice 2 | Male | 50–59 | Specialty practice 3 | Female | 30–39 |
| Family practice 2 | Female | 30–39 | Specialty practice 3 | Male | 70–79 |
| Family practice 3 | Female | 50–59 | Specialty practice 3 | Female | 30–39 |
| Family practice 3 | Female | 50–59 | Specialty practice 4 | Male | 60–69 |
| Family practice 3 | Male | 30–39 | Specialty practice 4 | Female | 50–59 |
| Specialty practice 1 | Female | 50–59 | Specialty practice 4 | Male | 60–69 |
| Specialty practice 1 | Female | 50–59 | Specialty practice 4 | Male | 30–39 |
| Specialty practice 2 | Male | 40–49 | Specialty practice 5 | Female | 30–39 |
| Specialty practice 2 | Male | 30–39 | Specialty practice 5 | Female | 40–49 |
| Specialty practice 2 | Male | 30–39 | Specialty practice 5 | Male | 30–39 |
Research site
HealthGroup is a non-academic multispecialty outpatient organization located in a large metropolitan area in Texas employing over 120 physicians providing primary and sub-specialty care to its patients. HealthGroup implemented its EHR 7 years prior to data collection. We collected our data before enactment of the HITECH legislation (July 2007–January 2009). While HealthGroup's executive and physician leadership made the EHR purchase decision, the extent to which the EHR was assimilated into work practices was left up to each physician.
The EHR system
HealthGroup implemented one of the leading currently available ambulatory EHR products in 2001. The product was CCHIT certified54 at the time of the study. Physicians could use this EHR system to update medication lists, order laboratory and diagnostic tests, document clinical visits using templates and/or free text fields, generate patient panel reports, check laboratory results, order medication, and track patient data over time. Physicians could use the EHR system to communicate with other physicians and nurses within HealthGroup, with pharmacies via an e-prescribing feature, and with patients via a secure patient portal.
Data collection
The first week of data collection in each of the eight practices was dedicated to direct observation (5–6 h/day, 4 days/week=20–24 h total/practice in week 1). Physician interviews were conducted during weeks 2–4. When physician interviews were not taking place, direct observation continued. Given that the number of physicians in each practice ranged from two to six and each interview lasted approximately 30–45 min, the majority of time during data collection was spent on direct observation. Data collection was aimed at identifying distinct patterns of physicians’ EHR use and discovering new variables to help explain these differences. Semi-structured interviews were conducted using an ethnographic approach.55 Interview questions were developed using medical informatics and organizational behavior literature (see the online supplementary material for interview and observation guides). Questions focused on physicians’ beliefs about using an EHR, experiences (both positive and negative) using the EHR, and perceptions of how EHR use influenced patient–physician interaction. Box 1 provides example interview questions. Interviews were audio recorded and transcribed. The Institutional Review Board at The University of Texas at Austin and HealthGroup's executive and physician leadership approved this study.
Box 1. Example interview questions concerning electronic health record (EHR) use.
Describe how you use the EHR in your work.
What features of the EHR do you use?
Do you find the EHR easy/difficult to use?
What kinds of things do you like about using the EHR?
What kinds of things do you dislike about using the EHR?
How often do you change the way you use the EHR? What types of events might precipitate a change in your EHR use?
Is there anything you think is unique about how you use the EHR?
Have you modified or tailored template(s) for your EHR use? If so, how?
Has using an EHR changed the way you practice medicine? If so, how?
Do you involve patients in your EHR use?
We adapted the observation guide from one previously used to study primary care practices.56 Two authors (HJL, RRM) were collaborators on the project that developed the original observation guide. The original observation guide was designed to study the nature of the interactions and relationships among practice members and the time and space for practice members to reflect with each other on routine and non-routine events. We modified this guide to include less data collection on practice member reflection and more data collection on how individuals in the practice interacted with the EHR. The observation guide aided data collection by ensuring a minimum level of standardization in the data collected across the different field sites without over-structuring the data collection in terms of when and where data were collected in each of the practices.
Observations focused on EHR use patterns and included other clinic-level attributes such as physical layout of the work space, description of the workflow for each physician including interactions with others, and description of patient flow. Researcher field notes were written daily immediately following direct observation activities. The first author (HJL) received EHR training for new clinical staff members to improve the data collection effort. Two authors (HJL, RRM) met for half a day each week during data collection to discuss observations from the practices. These meetings facilitated ongoing and critical reflection57 on the data collection process, discussion of early insights and preliminary patterns in the data, and the handling of any issues that emerged during data collection. A supplementary figure summarizing data collection and analysis activities is provided online.
Analytical approach
A constant comparative approach guided data analysis.49 The individual physician was the unit of comparison in this analysis. Open, selective, and axial coding procedures were performed. Two authors independently reviewed and analyzed the data (HJL, RRM). A third author (LKL) provided an additional perspective when differences in interpretations occurred during data analysis. For two of the three authors (RRM, LKL), data were blinded during analysis, such that the researchers were unaware of which physician's data were being analyzed at any given time. This type of blinding was not possible for the author who collected the data.
We analyzed interview transcripts and observation field notes in three steps as regards: (1) theme formation along dimensions of physicians’ EHR use patterns and factors associated with these patterns, (2) theme matching along these same dimensions, and (3) comparisons of these dimensions across all 28 physicians. We developed methodological memos, theoretical memos, and preliminary interpretations in the initial read of the interview transcripts and observation field notes. We refined our preliminary interpretations continually throughout the data analysis process and added new themes when potentially important findings were not captured in the set of existing themes.58 Unifying themes representing interpretations from multiple ideas in the data were merged into larger categories for further analysis. Iterations of this process produced the findings described in the ‘Results’ section.
In applying complexity science as a theoretical frame, we expected to see a role for practice relationships in explaining differences in practice-level EHR use patterns, and results from previous analyses examining this association have been published.14 During data analysis, however, we also observed striking differences in how individual physicians discussed uncertainty and the role of information in managing uncertainty, particularly when responding to questions aimed at understanding specific aspects of EHR use. Questions such as, ‘How does the EHR help you provide care for your patients?’ and ‘How does using the EHR get in the way of caring for your patients?’ were particularly effective in eliciting data on physicians’ thoughts about uncertainty and its management. This unanticipated observation in the data prompted an in-depth analysis of the relationship between individual physicians’ perceptions of uncertainty and their EHR use patterns.
Following the open coding process that identified perceptions of uncertainty as a variable of interest, we developed a codebook to systematically analyze the data for this construct. Organizational theory59–62 and complexity science23 26 36 informed the development of this codebook, and resulted in the perceptions of uncertainty categories of uncertainty reduction and uncertainty absorption.27
Uncertainty reduction
Uncertainty in healthcare organizations is traditionally conceptualized as reducible through information gathering or information processing (ie, information generates a clear understanding of the risks).59–62 For uncertainty that is reducible, information gathering and processing are generally effective. Looking up a test result in an EHR and asking a nurse or a patient for the test result are both examples of uncertainty reduction. When the information that is needed exists, uncertainty reduction is a useful strategy for managing uncertainty. Inspiration for the uncertainty reduction category came from this traditional view of uncertainty and its management.
Uncertainty absorption
Some uncertainties in healthcare delivery, however, are irreducible, or not resolvable with information.23–25 32 36 Irreducible uncertainty is present in patient care processes, illness and disease trajectories, and in the interactions between the two.37 63 How a given patient will respond to a medication is an example of irreducible uncertainty. After the medication is prescribed and taken by the patient, information exists that reduces the uncertainty about the patient's response to the medication. This information becomes available as time elapses, but it was non-existent at the time the medication was prescribed. Organizational researchers have suggested uncertainty absorption as a strategy for managing irreducible uncertainty.27 64 65 March et al state that uncertainty absorption occurs ‘when inferences are drawn from a body of evidence and the inferences, rather than the evidence itself, are then communicated’ (p 165)65. Uncertainty absorption is relationship-based and activated through argumentation, narration, and the exchange of information among individuals. Through these exchanges, new meaning is inferred and uncertainty is absorbed. Inspiration for the uncertainty absorption physician category came from this complexity science-based perspective of irreducible uncertainty. Definitions of the physicians’ perceptions of uncertainty codes used to analyze the data are provided in table 2.
Table 2.
Definitions of physicians’ perceptions of uncertainty codes
| Code | Definition |
|---|---|
| Uncertainty reduction | Observations or statements associated with or indicating strategies for managing uncertainty by reducing it with information or information processing; diminishing knowable risk and striving for certainty |
| Uncertainty absorption | Observations or statements associated with or indicating strategies for managing uncertainty by assimilating it or incorporating it into local circumstances; includes high use of relationships or interdependencies with others including physicians, nursing staff, patients, etc, to manage uncertainty |
We independently coded the interview and observation data for physicians’ perceptions of uncertainty and for EHR use patterns with approximately 2 months’ lag between these analyses. Physicians were categorized in terms of their EHR use patterns using the previously published criteria14 outlined in table 4 (adapted for individual physicians rather than physician–nurse teams). The categories for EHR use were high, medium, and low, and the criteria for inclusion in these categories were the following: (1) degree of EHR feature use, (2) extent to which the EHR is used to communicate with others (both internal and external to the practice), and (3) frequency with which EHR use patterns changed as a result of the rolling out of new features or learning from other sources. We then compared all 28 physicians along these two dimensions, examining the relationship between individual physicians’ perceptions of uncertainty and EHR use patterns.
Table 4.
Summary of electronic health record (her) use categories14
| EHR use category | Definition |
|---|---|
| High | Users in this category display high integration of EHR with work practices. Individuals in this category exhibit the following items: ▸ High feature use (including at least two of the following features) – Reports, flow sheets, and/or other tracking and trending features – EHR-generated patient literature – Macros/quick text feature ▸ High EHR-enabled communication with others inside practice ▸ High EHR-enabled communication with others outside practice ▸ High EHR-enabled communication with pharmacies ▸ Frequently changes EHR use as new features rolled out or learned |
| Medium | Users in this category display moderate integration of EHR with work practices. Individuals in this category can be divided into two types: 1 Users who exhibit high use of some but not all of the items in the high user category. 2 Users who exhibit moderate use of all or most of the items listed. This user type is articulated below: ▸ Moderate feature use (including at least one of the following features): – Reports, flow sheets, and/or other tracking and trending features – EHR-generated patient literature – Macros/quick text feature ▸ Moderate EHR-enabled communication with others inside practice ▸ Moderate or sporadic EHR-enabled communication with others outside practice ▸ Moderate EHR-enabled communication with pharmacies ▸ Rarely or sometimes changes EHR use as new features rolled out or learned |
| Low | Users in this category have low integration of EHR with work practices. Individuals in this category exhibit the following items: ▸ Low/minimal feature use (example minimal documentation) ▸ Low/minimal EHR-enabled communication with others inside practice ▸ Low/minimal EHR-enabled communication with others outside practice ▸ Low/no EHR-enabled communication with pharmacies ▸ Rarely changes EHR use as new features rolled out or learned ▸ May have high reliance on clinical staff to accomplish EHR-related work tasks ▸ May use paper records as primary documentation source |
Results
Physicians’ perceptions of uncertainty
Three categories of physicians’ perceptions of uncertainty were identified during data analysis: reduction, absorption, and hybrid (explained below). Table 3 describes these categories and provides exemplar quotes from the data on each category. While some demographic and medical specialty data of the physicians in each category are reported in describing these results, these details are only provided as additional contextual information.
Table 3.
Description of categories for physician perceptions of uncertainty with exemplar quotes
| Category | Description | Representative quotes |
|---|---|---|
| Uncertainty reduction | Views patient information contained in the medical record as paramount to the practice of medicine Seeks certainty and/or perpetually searches for ways to use information to reduce uncertainty Gives priority to codified patient information over other types of patient information (patient body language, tone of patient–physician interaction, tacit and/or difficult-to-capture aspects of patient encounter, etc) More information, particularly the kinds of information that can be captured in an EHR [electronic health record], always equals better patient care |
‘I'm just maybe a little more compulsive than other people and it satisfies that need in me to know exactly what medicines my patients are on; know exactly what interactions they may have; you know and so for someone with those needs this is a great system.’ (Primary care physician) ‘And you know you want to have the information you need, when you need it. I guess at some point we put all the information into electronic health records and we do away with the charts and if we get records somewhere else, we'll maybe they can just download all in that information in there you know.’ (Primary care physician) ‘I take pride in the fact that if a patient gets dumped in our hospital for an admission, I want them to go to my note first; rather than the internal medicine doctor's history and physical because they get better and more information out because I did write down that they had an appendectomy. That they had three pregnancies but only two kids, and one spontaneous abortion. That kind of information. That's a personal note of pride that actually drives me to be a more excellent record keeper; that's my information that can be used.’ (Specialist) |
| Uncertainty absorption | Views the co-creation and continual exchange of information between patients and physicians during patient encounters as paramount to the practice of medicine Manages uncertainty by engineering rich interactions between themselves and others Gives priority to information that was co-created, discovered, emphasized, and/or nearly missed during patient–physician encounters More information, particularly the kinds of information that can be captured in an EHR, does not always equal better patient care |
‘I don't know if the information I need is in there [EHR].’ (Primary care physician) ‘And, I mean the notes are important, but I really don't know if they're going to help anyone.’ (Specialist) ‘If I don't know exactly what's going on with a patient, that's ok. As long as I can talk with them about their condition in a way that helps them better understand their condition, then I've done my job.’ (Specialist) ‘When I read other people's notes I don't get very much information; I'm interested in [the] practitioner's assessment of putting it all together.’ (Specialist) ‘If I have time, I may go back and enter the chief complaint [in the EHR] later.’ (Specialist) |
| Uncertainty hybrid | Views patient information contained in the medical record as paramount to the practice of medicine Views the creation and exchange of information between patients and physicians during patient encounters as paramount to their practice of medicine Manages uncertainty through information contained in the medical record and through interactions with others More information is necessary but not sufficient for better patient care |
‘I think it's important to do a detailed review of the patients medical record before I go in to see them. That way I can focus on listening to what my patients are trying to tell me.’ (Specialist) ‘Documenting in the medical record is important but sometimes I think we are required to spend too much time documenting and too little time seeing patients.’ (Specialist) |
Physicians categorized as having an uncertainty reduction perspective27 expressed the belief that the information contained in the medical record is paramount to caring for patients. These physicians described themselves as ‘compulsive’ or ‘obsessive documenters,’ and they ‘took pride in their documentation.’ They sought to reduce uncertainty by continually gathering, manipulating, and inputting information in the medical record. Physicians with this view expressed a preference for information that could be captured or codified in the medical record (eg, laboratory results, medications, allergy list, past medical history). For these physicians, the more information that could be captured and processed the better they believed they could care for their patients. Interestingly, these physicians did not differentiate between structured and unstructured data in their desire for information. The distinguishing factor in categorizing physicians as uncertainty reducers was their overarching focus on information as the key driver of uncertainty management. Of the 28 physicians, 13 (eight males; three primary care physicians) were categorized as having an uncertainty reduction perspective.
Physicians with an uncertainty absorption perspective27 expressed the belief that the ongoing and attentive exchange of information and the co-creation of knowledge between patients and physicians during a clinical encounter were paramount to the job of caring for patients. Information contained in the medical record was important to these physicians, but much less so than information that was created, uncovered, and emphasized during patient encounters. Quotes such as, ‘I'm not sure the information that I need to care for my patients is in there [the EHR],’ and ‘I'm not sure that what I put in there [the EHR] is helpful to anyone else,’ describe how these physicians spoke about information contained in the EHR. Physicians with this perspective were less obsessive documenters, and they were more willing to let historical details go in favor of engaging in real-time, discovery-oriented conversation66 with patients. These physicians managed uncertainty by interacting mindfully with their patients, nurses, and other providers67 and expressed the belief that information contained in the medical record was often of limited use in caring for their patients. The distinguishing factor in categorizing physicians as uncertainty absorbers was their overarching focus on relationships with others as their primary strategy for managing uncertainty. Of the 28 physicians, five (four males; one primary care physician) were categorized as having an uncertainty absorption perspective.
Selective coding of the data revealed an unexpected third category of physicians’ perceptions of uncertainty: hybrid. Physicians categorized as uncertainty hybrids exhibited a combination of the uncertainty perspectives described in the previous two categories. Importantly, the hybrid category captured the uncertainty perspectives of physicians that were not adequately described by the reduction or absorption categories. These physicians viewed information captured in the medical record as critical to their work. At the same time, they viewed the exchange of information and creation of new knowledge with patients as a critical part of their practice. These physicians talked about both the importance of a thorough review of the medical record for key data points and past medical information and the importance of narrative and storytelling for developing a relationship-based understanding of the whole patient. Because the literature does not assume that individuals cannot exhibit both uncertainty reduction and uncertainty absorption views, we created a hybrid category rather than force physicians into the existing reduction or absorption categories. Of the 28 physicians, 10 (four males; five primary care physicians) were categorized as uncertainty hybrids.
EHR use
We analyzed the interview and observation data using an existing model of EHR use.14 The original model was used to examine practice-level patterns of EHR use. We adapted this model to allow for analysis of EHR use patterns at an individual physician level (see table 4). We categorized physicians’ EHR use as high, medium, or low based on factors including: degree of EHR feature use, level of EHR-enabled communication with others, and frequency that EHR use patterns changed. Physicians who scored high on all three criteria were categorized as high EHR users, and physicians who scored low on all three criteria were categorized as low EHR users. We categorized EHR use as medium for physicians scoring a mixture of high and low on these criteria or medium on all criteria.
Sixteen of the 28 physicians were categorized as high EHR users, nine as medium, and three as low. Of the high EHR users, nine were male and two were primary care physicians. Of the medium EHR users, four were male and six were primary care physicians. Of the low EHR users, all three were male and one was a primary care physician.
Relationship between physicians’ perceptions of uncertainty and EHR use patterns
Comparisons across physicians revealed a marked association between perceptions of uncertainty and EHR use patterns. Physicians categorized as having an uncertainty reduction perspective tended to be high EHR users (13/13). Physicians categorized as having an uncertainty absorption perspective tended to be low EHR users (3/5). Physicians categorized as hybrids tended to be medium EHR users (8/10). Figure 1 provides a graphical summary of these results. A Fisher's exact test of the association between physicians’ perceptions of uncertainty and EHR use patterns was statistically significant (p<0.001).
Figure 1.
Summary of results linking individual physicians’ perceptions of uncertainty with electronic health record (EHR) use.
Discussion
Results from this study suggest that a previously overlooked and potentially important linkage exists between physicians’ perceptions of uncertainty and their EHR use patterns. This linkage was observed across a diverse set of physicians representing a range of outpatient medical specialties. Physicians who viewed uncertainty primarily as reducible through information tended to be high EHR users. Physicians who acknowledged irreducible uncertainty in caring for patients tended to be low EHR users. Physicians who expressed both views of uncertainty tended to be medium EHR users. These findings suggest that perceptions of uncertainty may be more important in understanding physician differences in health IT use than previously believed and should, thus, be considered in future EHR design, implementation, and training efforts.
Healthcare delivery systems are complex systems characterized by reducible and irreducible uncertainty.23 36 37 Information, and thus health IT, plays a distinctly different role in managing these two types of uncertainty. Information gathering and information processing are generally effective at managing reducible uncertainty. Uncertainty about past medical history, family history, and results from previous tests and procedures, for example, is generally reducible with information. On the other hand, some uncertainty in healthcare delivery is irreducible, or not resolvable through information.23–25 32 36 Uncertainty embedded in diagnosis and treatment decisions, for example, is often irreducible. Managing irreducible uncertainty is much more challenging because this type of uncertainty is a product of the non-linear dynamics in complex systems,23 32 which by their nature are difficult to understand, and the information needed to reduce this type of uncertainty does not exist. Therefore, alternative strategies for managing irreducible uncertainty in healthcare delivery are needed, and these strategies need to be incorporated into health IT solutions. Strategies, such as uncertainty absorption, that emphasize the role of relationships and interdependencies among providers and between providers and patients could be key to managing irreducible uncertainty in healthcare delivery. Current health information technologies are generally designed to help clinicians manage the reducible uncertainty they face in caring for patients. Improvements can be made, however, in helping them manage the irreducible uncertainty they face.
So that health IT can be used to support transformation in the healthcare system, the reasons why seemingly similar physicians use the same EHR system differently from each other need to be elucidated. Consideration of the results from these analyses of individual physician-level EHR use together with the results from our previous analyses of practice-level EHR use generates some important insights. In examining differences in how individual physicians were using the same EHR, we found physicians’ perceptions of uncertainty to be helpful in explaining these differences. We described the information intensive approach to EHR use by uncertainty reductionists, the relationship intensive approach to EHR use by uncertainty absorbers, and the combined information–relationship approach to EHR use by uncertainty hybrids. Our previous study of practice-level EHR use found that seven attributes of practice relationships (trust, mindfulness, heedfulness, respectful interaction, diversity, rich and lean communication, and social/task relatedness) were useful in distinguishing practices with heterogeneous EHR use patterns from practices with homogeneous EHR use patterns. Mindfulness (openness to new ideas) and respectful interaction (honest, self-confident, and appreciative interaction) further distinguished between practices with homogeneous EHR use (low and medium usage) and practices with homogeneous EHR use (high usage). The findings from these two distinct analyses suggest that, in addition to improving informational capacities, future health information technologies must be designed and implemented in ways that improve the social, or relationship, capacities in healthcare delivery.
Implications
The findings from this study have implications for future health IT design, implementation, and training efforts. Reducible uncertainty is generally well managed with existing health IT tools. Irreducible uncertainty, however, presents a different set of challenges for health IT designers, executives, and end-users. Undoubtedly, health IT systems should be designed to collect, store, process, and transfer information from one entity to another. However, they should also be designed to help physicians manage the irreducible uncertainty they face in caring for patients. To accomplish the latter, health IT will need to be designed and implemented in ways that help physicians and other healthcare professionals absorb uncertainty in patient care.
Because this conceptualization of health IT systems is comparatively nascent, it is difficult to fully articulate what the study findings mean for current health IT design and implementation efforts. As a start, our findings provide much needed insight into the information needs and information behaviors of physicians as they provide EHR-enabled care to their patients. In addition to standardized documentation tools, perhaps physicians also need tools that allow multiple providers to synchronously and asynchronously co-create knowledge about shared patients. As currently designed and used, free text fields allow space within the medical record for physicians to think through treatment plans and probable illness trajectories. Improving the usability and utility of free text fields could help physicians absorb uncertainty. For instance, free text fields could be designed for data aggregation across patients and across multiple providers for a single patient, enabling better decision-making and more effective action, particularly when risk is poorly understood. Additionally, health IT should be designed to capture physicians’ thought processes and transfer these thoughts to other providers. Perhaps particularly novel, inconsistent, or out of the ordinary text should be flagged by an EHR as ‘potentially critical to others’ and subsequently ‘pushed’ to all providers sharing that patient. Perhaps most importantly, EHRs should be designed to increase the richness of the relationships and interactions among providers and between providers and their patients,68 and they should help both providers and patients recognize when a seemingly routine medical issue becomes non-routine.69
Differences in individual physicians’ EHR use patterns may be an inherent attribute of health IT-enabled healthcare delivery. If so, health IT dissemination and implementation initiatives that emphasize standardized clinical documentation could be inadvertently driving physicians toward an uncertainty reduction mindset, and thus unwittingly orchestrating the loss of alternative clinical mindsets. Nonetheless, better understanding of the relationships among physicians’ information needs, perceptions of uncertainty, and EHR use are needed.
Limitations
Because of the in-depth qualitative approach, this study was conducted using a small number of physicians within a single care setting. Thus, it is unclear how these findings apply across other healthcare settings. We believe, however, that the perceptions of uncertainty identified in this research are likely similar to the perceptions of uncertainty in other care delivery settings. Likewise, we believe that the linkage between physicians’ perceptions of uncertainty and EHR use observed in this study is likely to be observed in other settings. This study is also limited by the authors’ interpretation of the data. While we interpreted the differences in physicians’ information needs and preferences as differences in perceptions of uncertainty, others might have arrived at alternative interpretations. Other possible interpretations could be differences in visual versus auditory learning styles, data versus relationship orientation, and reductionist versus holistic approaches to medicine. We used open coding procedures to analyze the data to guard against focusing in on a construct too early in the data analysis process, which we believe helps to support our interpretation of the data. The use of interview and observational data (as opposed to EHR logs) to categorize EHR use patterns is another study limitation. Interviews are limited by self-reporting bias and observations are limited by the potential for incomplete sampling. However, because we sought a more contextually based understanding of EHR use and because we spent an extensive amount of time studying these physicians and their EHR use patterns, we believe this categorization method to be appropriate. Additional validation of the uncertainty perceptions identified in this research is needed. Finally, studies examining how patient outcomes are impacted by the interdependency between physicians’ perceptions of uncertainty and EHR use are needed.
Conclusion
This study contributes new understanding of the differences in how individual physicians use an EHR. Our findings demonstrate that physicians differ in how they perceive uncertainty and how they view the role of information in managing uncertainty as they care for patients. Specifically, we find evidence linking individual physicians’ perceptions of uncertainty with their EHR use patterns. This finding holds across a diverse set of 28 physicians representing a variety of medical specialties. The study findings have implications for health IT research, practice, and policy, particularly in terms of their potential impact on future health IT design and implementation initiatives in ways that simultaneously acknowledge differences in physicians’ perceptions of uncertainty and support physicians’ goals of providing high quality health IT-enabled patient care. These findings can also be used to improve understanding of physicians’ information needs in the context of EHR-enabled healthcare delivery. From a complexity science perspective, this study contributes the idea that irreducible uncertainty (uncertainty that cannot be reduced with information) should be recognized in health IT initiatives. More research is needed to assess the transferability of these findings and determine optimal strategies to effectively manage them in practice.
Supplementary Material
Acknowledgments
The authors are sincerely grateful to two anonymous reviewers for sharing their insights on previous versions of this manuscript and to the many clinicians and staff at the ambulatory care organization who participated in the study.
Footnotes
Contributors: All authors meet criteria for authorship. HJL made substantial contributions to study conception and design, acquisition of data, data analysis and interpretation of data, and drafting the article and revising it critically for important intellectual content, and provided final approval of the version to be published. RRM made substantial contributions to conception and design, interpretation of data, and revising the manuscript critically for important intellectual content and provided final approval of the version to be published. DFS, LKL, JAP, and MLP made substantial contributions to interpretation of data and revising the manuscript critically for important intellectual content, and provided final approval of the version to be published.
Funding: This work was supported by the Ernst & Young Health Care Management Program Graduate Fellowship as part of HJL's Doctoral Program in the Department of Information, Risk & Operations Management, McCombs School of Business, The University of Texas at Austin. Additionally, this material was supported with resources and the use of facilities at the South Texas Veterans Health Care System, Veterans Evidence Based Research Dissemination and Implementation Center (VERDICT), San Antonio, Texas, USA. Support for LKL was provided by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service (REA 05-129, CDA 07-022).
Disclaimer: The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Competing interests: None.
Ethics approval: The Institutional Review Board at The University of Texas at Austin and the executive and physician leadership of the ambulatory care organization approved this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The first author is willing to provide the de-identified study data to those requesting it for legitimate reasons.
References
- 1.Xierali IM, Chun-Ju H, Puffer JC, et al. The rise of electronic health record adoption among family physicians. Ann Fam Med 2013;11:14–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DesRoches CM, Worzala C, Joshi MS, et al. Small, nonteaching, and rural hospitals continue to be slow in adopting electronic health record systems. Health Aff 2012;31:1092–9 [DOI] [PubMed] [Google Scholar]
- 3.Hsiao C, Hing E. Use and characteristics of electronic health record systems among office-based physician practices: United States, 2001–2012. Hyattsville, MD: National Center for Health Statistics, 2012 Dec. (NCHS Data Brief No. 111). [PubMed] [Google Scholar]
- 4.American Recovery and Reinvestment Act of 2009 Open Congress for the 111th United States Congress website. http://www.opencongress.org/bill/111-h1/show (accessed 5 Feb 2012).
- 5.Institute of Medicine Committee on patient safety and health information technology board on health care services, chapter 2: evaluating the current state of patient safety and health IT. Health IT and patient safety: building safer systems for better care. Washington, DC: The National Academies Press, 2011:31–58 [PubMed] [Google Scholar]
- 6.Stead WW, Lin HS.2009. Committee on Engaging the Computer Science Research Community in Health Care Informatics; National Research Council. Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions.
- 7.Black AD, Car J, Pagliari C, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLoS Med 2011;8:e1000387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Landrigan CP, Parry GJ, Bones CB, et al. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med 2010;363:2124–34 [DOI] [PubMed] [Google Scholar]
- 9.Singh H, Spitzmueller C, Petersen NJ, et al. Primary care practitioners’ views on test result management in EHR-enabled health systems: a national survey. J Am Med Inform Assoc 2013;20:727–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fleurant M, Kell R, Jenter C, et al. Factors associated with difficult electronic health record implementation in office practice. J Am Med Inform Assoc 2012;19:541–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: a review of the recent literature shows predominantly positive results. Health Aff 2011;30:464–71 [DOI] [PubMed] [Google Scholar]
- 12.Unertl KM, Weinger MB, Johnson KB, et al. Describing and modeling workflow and information flow in chronic care disease. J Am Med Inform Assoc 2009;16:826–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zheng K, Haftel HM, Hrischl RB, et al. Quantifying the impact of health IT implementations on clinical workflow: a new methodological perspective. J Am Med Inform Assoc 2010;17:454–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanham HJ, Leykum LK, McDaniel RR. Same organization, same electronic health records (EHRs) system, different use: exploring the linkage between practice member communication patterns and EHR use patterns in an ambulatory care setting. J Am Med Inform Assoc 2010;19:382–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ash JS, Sittig DF, Dykstra R, et al. The unintended consequences of computerized provider order entry: findings from a mixed methods exploration. Int J Med Inform 2009;78(Suppl 1):S69–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sittig DF, Classen DC. Safe electronic health record use requires a comprehensive monitoring and evaluation framework. JAMA 2010;303:450–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform 1999;55:87–101 [DOI] [PubMed] [Google Scholar]
- 18.Reddy MC, Paul SA, Abraham J, et al. Challenges to effective crisis management: using information and communication technologies to coordinate emergency medical services and emergency department teams. Int J Med Inform 2009;78:259–69 [DOI] [PubMed] [Google Scholar]
- 19.Sittig DF, Singh H. A new socio-technical model for studying health information technology in complex adaptive healthcare systems. Qual Saf Healthc 2010;19(Suppl 3):i68–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Trist EL, Banforth KW. Some social and psychological consequences of the longwall method of coal getting: an examination of the psychological situation and defenses of a work group in relation to the social structure and technological content of the work system. Hum Relat 1951;4:3–38 [Google Scholar]
- 21.Sittig DF, Singh H. Electronic health records and national patient-safety goals. N Engl J Med 2012;367:1854–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742–52 [DOI] [PubMed] [Google Scholar]
- 23.Cilliers P. Complexity and postmodernism: understanding complex systems. New York, NY: Routledge, 1998 [Google Scholar]
- 24.Zimmerman B, Lindberg C, Plsek P. Edgeware: insights from complexity science for health care leaders. Irving, TX: VHA Inc, 1998 [Google Scholar]
- 25.Anderson P. Complexity theory and organization science. Org Sci 1999;10:216–32 [Google Scholar]
- 26.Bar Yam Y. Chapter 10: health care I: the health care system. Making things work: solving complex problems in a complex world. Cambridge, MA: Knowledge Press, 2004:117–30 [Google Scholar]
- 27.Boisot M, Child J. Organizations as adaptive systems in complex environments: the case of China. Org Sci 1999;20:237–52 [Google Scholar]
- 28.Allen PM, Varga L. A co-evolutionary complex systems perspective on information systems. J Inform Technol 2006;21:229–38 [Google Scholar]
- 29.Merali Y. Complexity and information systems: the emergent domain. J Infor Technol 2006;21:210–28 [Google Scholar]
- 30.Tanriverdi H, Rai A, Venkatramen N. Reframing the dominant quest of information systems strategy research for complex adaptive business systems. Inform Syst Res 2010;21:822–34 [Google Scholar]
- 31.Vidgen R, Wang X. Coevolving systems and the organization of agile software development. Inform Syst Res 2009;20:355–76 [Google Scholar]
- 32.Sornette D. Critical phenomenon in natural sciences. Berlin: Springer, 2006 [Google Scholar]
- 33.Kauffman S. At home in the universe: the search for the laws of self-organization and complexity. Oxford: Oxford University Press, 1995 [Google Scholar]
- 34.Epstein J. Generative social science: studies in agent-based computational modeling. Princeton, NJ: Princeton University Press, 2007 [Google Scholar]
- 35.Holland JH. Emergence: from chaos to order. Reading, MA: Addison-Wesley, 1998 [Google Scholar]
- 36.McDaniel RR, Driebe D. Uncertainty and surprise in complex systems: questions on working with the unexpected. Berlin: Springer-Verlag, 2005 [Google Scholar]
- 37.Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Making 2011;31:828–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Leykum LK, Pugh JA, Lawrence VA, et al. Organizational interventions employing principles of complexity science have improved outcomes for patients with Type II diabetes. Implement Sci 2007;2:1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Leykum LK, Parchman M, Pugh J, et al. The importance of organizational characteristics for improving outcomes in patients with chronic disease: a systematic review of congestive heart failure. Implement Sci 2010;5:1–34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Plsek PE, Greenhalgh T. Complexity science: the challenge of complexity in health care. BMJ 2001;323:625–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eddy DM. Variations in physician practice: the role of uncertainty. Health Aff 1984;3:74–89 [DOI] [PubMed] [Google Scholar]
- 42.Allison JJ, Kiefe CI, Cook EF, et al. The association of physician attitudes about uncertainty and risk taking with resource use in Medicare HMO. Med Decis Making 1998;18:320–29 [DOI] [PubMed] [Google Scholar]
- 43.Gerrity MS, DeVellis RF. Physicians’ reactions to uncertainty in patient care: a new measure and new insights. Med Care 1990;28:724–36 [DOI] [PubMed] [Google Scholar]
- 44.Kvale J, Berg L, Groff JY, et al. Factors associated with residents’ attitudes toward dying patients. Fam Med 1999;31:691–6 [PubMed] [Google Scholar]
- 45.Politi MC, Clark MA, Ombao H, et al. The impact of physicians’ reactions to uncertainty on patients’ decision satisfaction. J Eval Clin Pract 2011;17:575–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mishel MH. Uncertainty in illness. J Nurs Scholarship 1988;20:225–32 [DOI] [PubMed] [Google Scholar]
- 47.Roos NP, Roos LL. High and low surgical rates: risk factors for area residents. Am J Pub Health 1981;71:591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Goyert GL, Bottoms SF, Treadwell MC, et al. The physician factor in cesarean birth rates. N Engl J Med 1989;320:706–9 [DOI] [PubMed] [Google Scholar]
- 49.Bernard HR, Ryan GW. Chapter 15: analytics induction and qualitative comparative analysis. Analyzing qualitative data: systematic approaches. Los Angeles, CA: Sage, 2010:325–40 [Google Scholar]
- 50.Strauss A, Corbin J. Basics of qualitative research: techniques and procedures for developing grounded theory. 2nd edn Thousand Oaks, CA: Sage, 1998 [Google Scholar]
- 51.Lanham HJ, McDaniel RR, Jr, Crabtree BF, et al. How improving practice relationships among clinicians and nonclinicians can improve quality in primary care. Jt Comm J Qual Patient Saf 2009;35:457–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chiasson M, Reddy M, Kaplan B, et al. Expanding multi-disciplinary approaches to healthcare information technologies: what does information systems offer medical informatics? Int J Med Inform 2007;76(Suppl 1):S89–97 [DOI] [PubMed] [Google Scholar]
- 53.CCHIT. https://www.cchit.org/find-cchit (accessed 20 Feb 2013).
- 54.Eisenhardt KM. Building theories from case study research. Acad Manage Rev 1989;14:532–50 [Google Scholar]
- 55.Spradley JP. Interviewing an informant. The ethnographic interview. Belmont, CA: Wadsworth, 1979, 55–68 [Google Scholar]
- 56.Stroebel KC, McDaniel RR, Crabtree BF, et al. How complexity science can inform a reflective process for improvement in primary care practices. Jt Comm J Qual Patient Saf 2005;31:438–46 [DOI] [PubMed] [Google Scholar]
- 57.Schön DA. The reflective practitioner. New York City: Basic Books, 1983 [Google Scholar]
- 58.Crabtree BF, Miller WL. Doing qualitative research. Thousand Oaks, CA: Sage, 1999 [Google Scholar]
- 59.Daft R, Lengel R. Information richness: a new approach to managerial behavior and organization design. In: Cummings L. Research in Organizational Behaviour. Greenwich: JAI Press, 1984:191–233 [Google Scholar]
- 60.Galbraith JR. Designing complex organizations. Reading, MA: Addison-Wesley, 1973 [Google Scholar]
- 61.Shannon CE. A mathematical theory of communication. Bell System Technical J 1948;27:623–56 [Google Scholar]
- 62.Tushman ML, Nadler DA. Information processing as an integrating concept in organizational design. Acad Manage Rev 1978;3:613–24 [Google Scholar]
- 63.West BJ. Chapter 4: the uncertainty of health. Where medicine went wrong: rediscovering the path to complexity. Singapore: World Scientific Publishing Co., 2006:119–72 [Google Scholar]
- 64.Ashmos DP, Duchon D, McDaniel RR, et al. What a mess! Participation as a simple managerial rule to ‘complexify’ organizations. J Manag Stud 2002;39: 189–206 [Google Scholar]
- 65.March JG, Simon HA, Guetzkow HS. Organizations. Cambridge, MA: Blackwell, 1958 [Google Scholar]
- 66.Jordan ME, Lanham HJ, Crabtree BF, et al. The role of conversation in health care interventions: enabling sensemaking and learning. Implement Sci 2009;4:1–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Epstein RM. Mindful practice. JAMA 1999;282:833–9 [DOI] [PubMed] [Google Scholar]
- 68.Daft R, Lengel R. Information richness: a new approach to managerial behavior and organization design. In: Cummings L. Research in organizational behavior. Greenwich: JAI Press, 1984:191–233 [Google Scholar]
- 69.Hedberg B, Jonsson S. Designing semi-confusing information systems for organizations in changing environments. Acc Organ Soc 1978;3:47–64 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.