Abstract
Objectives
The posterior maxillary region often provides a limited bone volume for dental implants. Maxillary sinus elevation via inserting a bone graft through a window opened in the lateral sinus wall has become the most common surgical procedure for increasing the alveolar bone height in place of dental implants in the posterior maxillary region. The purpose of this article is to assess the change of bone volume and the clinical effects of dental implant placement in sites with maxillary sinus floor elevation and autogenous bone graft through the lateral window approach.
Materials and Methods
In this article, the analysis data were collected from 64 dental implants that were placed in 24 patients with 29 lacks of the bone volume posterior maxillary region from June 2004 to April 2011, at the Department of Oral and Maxillofacial Surgery, Inha University Hospital. Panoramic views were taken before the surgery, after the surgery, 6 months after the surgery, and at the time of the final follow-up. The influence of the factors on the grafted bone material resorption rate was evaluated according to the patient characteristics (age and gender), graft material, implant installation stage, implant size, implant placement region, local infection, surgical complication, and residual alveolar bone height.
Results
The bone graft resorption rate of male patients at the final follow-up was significantly higher than the rate of female patients. The single autogenous bone-grafted site was significantly more resorbed than the autogenous bone combined with the Bio-Oss grafted site. The implant installation stage and residual alveolar height showed a significant correlation with the resorption rate of maxillary sinus bone graft material. The success rate and survival rate of the implant were 92.2% and 100%, respectively.
Conclusion
Maxillary sinus elevation procedure with autogenous bone graft or autogenous bone in combination with Bio-Oss is a predictable treatment method for implant rehabilitation.
Keywords: Dental implants, Maxillary sinus floor augmentation, Maxillary sinus, Alveolar bone grafting, Bone resorption
I. Introduction
Dental implants are increasingly being used to replace missing teeth1. Note, however, that there are common problems in the posterior maxillary region such as restriction in the anatomic location, alveolar bone atrophy after prolonged edentulate state, resorption of alveolar bone in patients with periodontitis, and pneumatized sinus cavities causing lack of alveolar bone height. Likewise, lack of bone mass hampers implant restoration in the posterior maxillary region.
Boyne and James2 (1980) reported on the elevation of the maxillary sinus floor in patients with large, pneumatized sinus cavities in preparation for the placement of blade implants. Obviously, in the posterior maxillary region, reduction of vertical bone height is often limited to standard implant placement. Elevation of the maxillary sinus floor is the option to solve this problem. Various surgical techniques have been presented to use the sinus cavity for elevating the sinus membrane and placing bone graft materials.
Tatum3 first proposed dental implant placement in sites with bone graft for sinus floor elevation through the lateral window approach technique and its clinical application. This technology expanded the implant indication of the posterior maxillary region, having the advantages of direct vision when performing surgery, control of the elevated height, effective protection of the sinus mucosa, convenience of bone graft, and accurate positioning. In the study published by Wallace and Froum4, they showed a high success rate using this technology for implant restoration.
As implant technology and bone grafting developed, maxillary sinus bone grafting became a popular form of surgery. Nonetheless, the graft material for maxillary sinus bone grafting has become an object of controversy. Bone grafting materials used for maxillary sinus graft include autogenous bone, allogenous bone, xenogenous bone, and synthetic bone. As the principle of new bone to be formed by autogenous bone, grafted bone exhibits osteoconductivity for osteoblast maturity by stimulating the osteoprogenitor cell of adjacent tissue or plays the role of passive substrate for the osteoprogenitor cell5. Meanwhile, autogenous bone graft has the limit of bone yield but the advantage of no tissue rejection.
This study sought to assess the change of bone volume and success and survival rates of implant placement in sites with bone graft for the elevation of maxillary sinus floor according to the patient's characteristics (age and gender), graft material, implant placement stage, implant size, implant placement region, local infection, surgical complication, and residual alveolar bone height.
II. Materials and Methods
1. Case selection
A total of 79 patients underwent dental implant restorations using sinus floor elevation from June 2004 to April 2011 at the Department of Oral and Maxillofacial Surgery, Inha University Hospital (Incheon, Korea). At least 55 patients failed to comply with the follow-up principle or had systemic diseases, so the remaining 24 patients were included in the analysis. A total of 65 dental implants were inserted. One implant was not inserted into the bone graft region, and this implant was also excluded from the analysis. Therefore, 64 implants were included in this analysis. A total of 47 implants were inserted using two-stage surgery, and 17 implants, using one-stage surgery. Among 24 patients, 5 patients received bilateral surgery. At least 6 patients had single missing tooth, whereas 18 patients had multiple missing tooth. After a healing period of 6 to 13 months (average: 8.8 months), the implant prostheses were restored. The follow-up period was 24 to 68 months (average: 32.4 months).
2. Preoperative examination
Patients received clinical examination over 3 months after tooth extraction, and they were suitable for implant surgery. At least 24 patients had no systemic diseases affecting bone healing, but 3 patients had chronic maxillary sinusitis (CMS). Preoperative panoramic taking was performed to assess bone volume at both the implantation and donor sites to ensure the optimal position of the graft and implant. The bone quality, residual bone height, and existing maxillary sinus morphology were also evaluated on panoramic views.
3. Type of graft material
Autogenous bone was harvested from the mandibular ramus or iliac crest, and then crushed into particulates. Bio-Oss (Geistlich Pharma AG, Wolhusen, Switzerland) was used as xenogenous bone. Autogenous bone alone or composite graft consisting of autogenous bone and Bio-Oss was used as grafting material. After sinus elevation, if the created space for grafting was small with 1 or 2 tooth sites included, autogenous bone was used alone; if not, composite graft was used.
4. Surgical methods
The surgery for 18 patients was performed under local anesthesia, and the other 6 patients were treated under general anesthesia by one surgeon. The surgery was started with a trapezoid incision made on the alveolar ridge crest, and a full-thickness flap was then raised to expose the lateral antral wall of the sinus fully. After the flap was raised to the desired level, a window was created with a round bur as trapdoor on the lateral buttress of the maxilla. The bottom of the window was located 5 mm above the edge of the maxillary sinus floor. The size of the trapdoor should be determined according to the number of dental implants, should be conducive to peel the mucous membrane of the maxillary sinus, and should be smaller than the area of the lateral wall of the maxillary sinus. The height of this trapdoor should not exceed the width of the sinus to allow a final horizontal position of the new floor. A space was created after the sinus membrane was elevated by the intruded trapdoor. Finally, the bone block was rotated into the top of the space. After peeling the mucous membrane, the movement of bone block and mucous membrane could be seen together with respiration; thus indicating that the maxillary sinus membrane was integrated.
The socket should be gradually expanded and prepared as the implant bed. Because of the low density of bone in the maxillary molar region, the use of osteotome needs to achieve better primary stability. The prepared graft material was grafted in the elevated maxillary sinus cavity, and then implant placement was performed. All of the implants used were External Implant RBT (BioHorizons Implant Systems Inc., Birmingham, AL, USA).
If the residual bone height and bone density are too low, primary implant stability would be jeopardized. Therefore, two-stage surgery should be performed.
5. Radiological examination
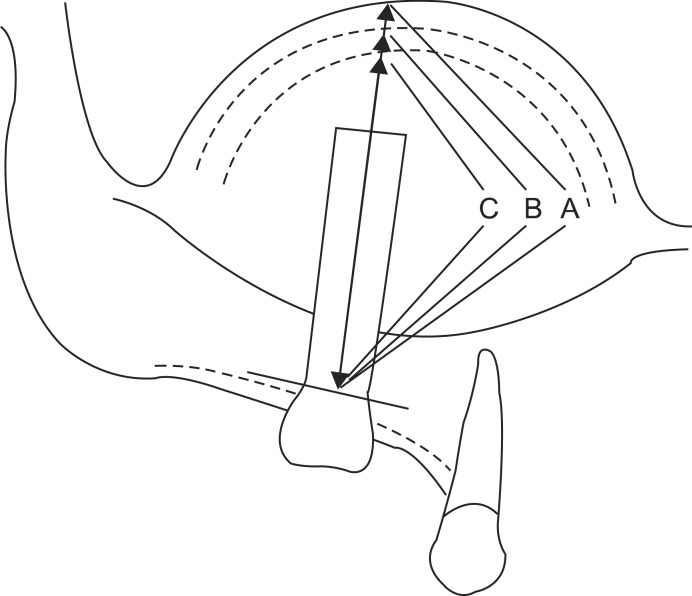
The panoramic images were traced on paper, and all measurements were performed by calibration. The amount of bone augmentation 'A' was evaluated by measuring the distance from the bottommost part of the fixture threads to the uppermost part of the bone graft material on a center-line of fixture after the surgery.(Fig. 1) The same measuring method was applied on a panorama taken 6 months after the surgery 'B' and on the final follow-up 'C'. The amount of resorption of bone graft material 'A-B' 6 months after the surgery and 'A-C' at the final follow-up time was calculated.
Fig. 1.
The measurements for evaluating the amount of bone augmentation. (A: measure of the distance between the uppermost part of bone graft material and the lowermost partof the fixture threads on the panorama, B: measuring of the amount of bone augmentation 6 months after the surgery, C: measuring of the amount of bone augmentation on final follow-up, dotted line: bone resorption)
The resorption rate was calculated as (A-B)/A×100% on 6 months after the surgery and (A-B)/A×100% at the final follow-up time.
To measure marginal bone resorption, the distance between the bottommost part of fixture threads to the top of the alveolar crest as represented in a panorama was measured. The measuring method was based on the panorama obtained immediately after the inserted implant surgery and at the final follow-up time.
6. Postoperative maintenance
All patients took antibiotics to prevent infection and control edema after the surgery. The rest of the treatment was the same as the routine implantation operation. Patients were advised not to blow their nose to avoid pressing on the sinus mucosa. Sutures were removed 7 to 10 days later.
7. Statistical analysis on the resorption rate of bone graft material
With each measurement, statistical analysis on bone resorption 6 months after the surgery and final follow-up was performed using independent-sample t-test and ANOVA by age, gender, implant placement stage, graft materials, implant size, implant placement region, local infection, surgical complication, and residual alveolar bone height. P-values less than 0.05 were considered significant.
8. Follow-up principles
All patients were asked to make a return visit within 1, 3, and 6 months of the surgery and to undergo regular re-examination each year. The contents of the re-examination included the extent of implant stability and condition of tissue surrounding the implant. Patients should take a panoramic radiograph at each return visit and compare the resorption condition of the edge bone surrounding the implant.
Based on the panorama and medical records, preoperative and postoperative complications were examined; the success rates of the implants were evaluated according to the criteria of Albrektsson et al.6 at the time of final follow-up.
III. Results
1. Bone resorption rate by age and gender
The 24 patients who received 64 implants for restoration were included for analysis. A total of 18 male patients received 21 bone grafts, whereas 6 female patients received 8 bone grafts. Patients' age ranged from 18 to 68 years old, with mean age of 49.4 years.
The resorption rate of maxillary sinus bone graft in the 41 to 50-year-old age group was 23.0% and 32.7% on 6 months after the surgery and on the final follow-up, respectively; these were higher than the rates of other age groups. Note, however, that the difference in the resorption rate of maxillary sinus bone graft by patients' age was not significant.(Table 1)
Table 1.
Resorption rate of bone material by age
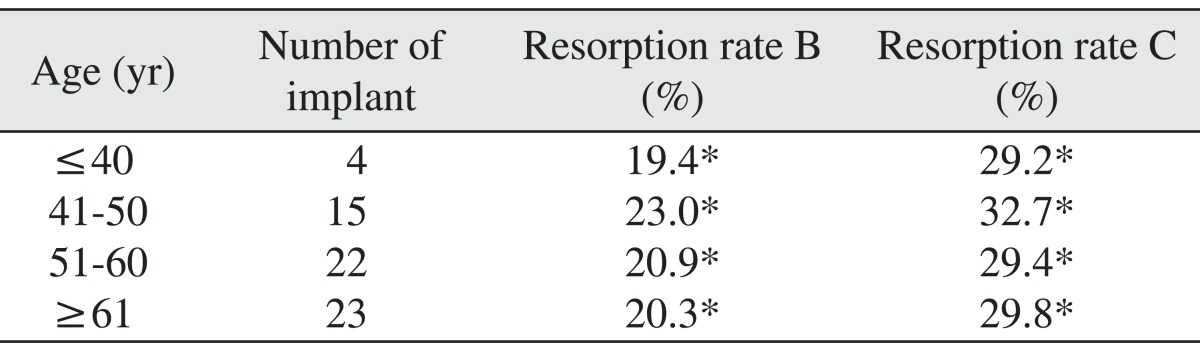
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
The resorption rate of the maxillary sinus bone graft of the male patients' group was 21.7% and 31.1% on 6 months after the surgery and on the final follow-up, respectively; these were higher than the resorption rate of the female patients' group.(Table 2) In particular, the bone resorption rate in the male patients group on the final follow-up was significantly higher than that in female patients (P<0.05). Note, however, that the difference in the resorption rate of maxillary sinus bone graft by patients' gender--6 months after the surgery--was not significant.
Table 2.
Resorption rate of bone material by gender
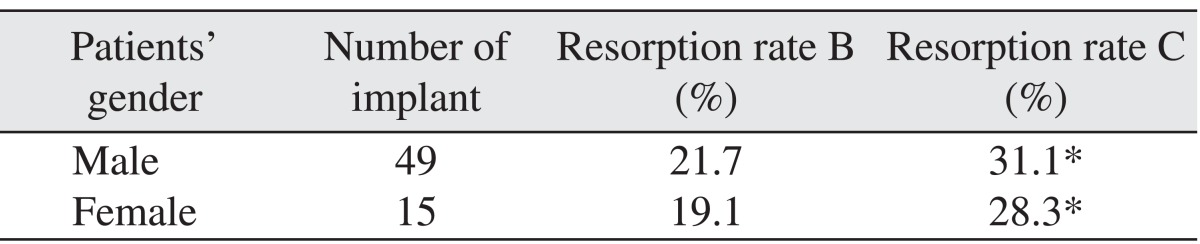
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
2. Bone resorption rate by graft material
At least 14 (48.3%) cases utilized autogenous bone graft material, and 15 (51.7%) cases, autogenous bone in combination with Bio-Oss. The harvested autogenous bone was used in the mandibular ramus (95.3%) and in the iliac crest bone (4.7%). The mixing proportion of autogenous bone and Bio-Oss was 2 : 1 or 3 : 1.
The resorption rate of bone graft material in the group with single autogenous bone graft was 23.1% and 32.1% on 6 months after the surgery and on the final follow-up, respectively. The resorption rate of bone graft material in the group with combined graft of autogenous bone and Bio-Oss was 18.9% and 28.6% on 6 months after the surgery and on the final follow-up, respectively. Bone graft resorption rate in the single autogenous bone material group was significantly higher than that in the autogenous bone with Bio-Oss material group (P<0.05).(Table 3)
Table 3.
Resorption rate of bone material by graft material
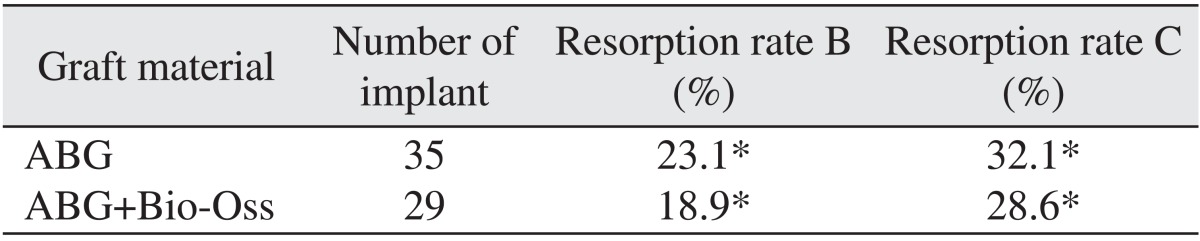
(ABG: autogenous bone graft)
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
Bio-Oss: Switzerland-made particulate graft material.
3. Bone resorption rate by implant placement stage
The decision to perform one-stage or two-stage surgery was mainly based on the available residual bone height and the possibility of achieving primary stability for the inserted implants. In this study, cases wherein one-stage surgery was performed when the residual bone height remained higher than 5 mm were selected, including those wherein two-stage surgery was the option when residual bone height remained lower than 5 mm. A total of 17 implants were used in one-stage surgery, i.e., implantation simultaneously done with sinus floor elevation. On the other hand, 47 implants were used in the two-stage surgery, which involved sinus floor elevation with delayed implant placement, i.e., 4 to 12 months after sinus grafting. The resorption rate of the maxillary sinus bone graft in the one-stage surgery group was significantly higher than that in the two-stage surgery group (P<0.05).(Table 4)
Table 4.
Resorption rate of bone material by implant placement stage
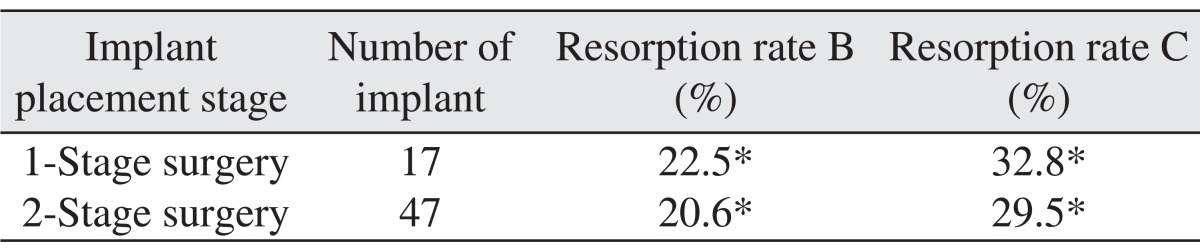
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
4. Bone resorption rate by implant size
Out of a total of 64 implants, there were 20 implants with diameter of 4 mm and 44 implants with diameter of 5 mm. The length was 9 mm in 4 implants, 10.5 mm in 15 implants, 11.5 mm in 7 implants, 12 mm in 27 implants, and 13 mm in 11 implants. There was no significant correlation between the diameter, length of inserted implant, and bone resorption rate.(Table 5)
Table 5.
Resorption rate of bone material by implant size
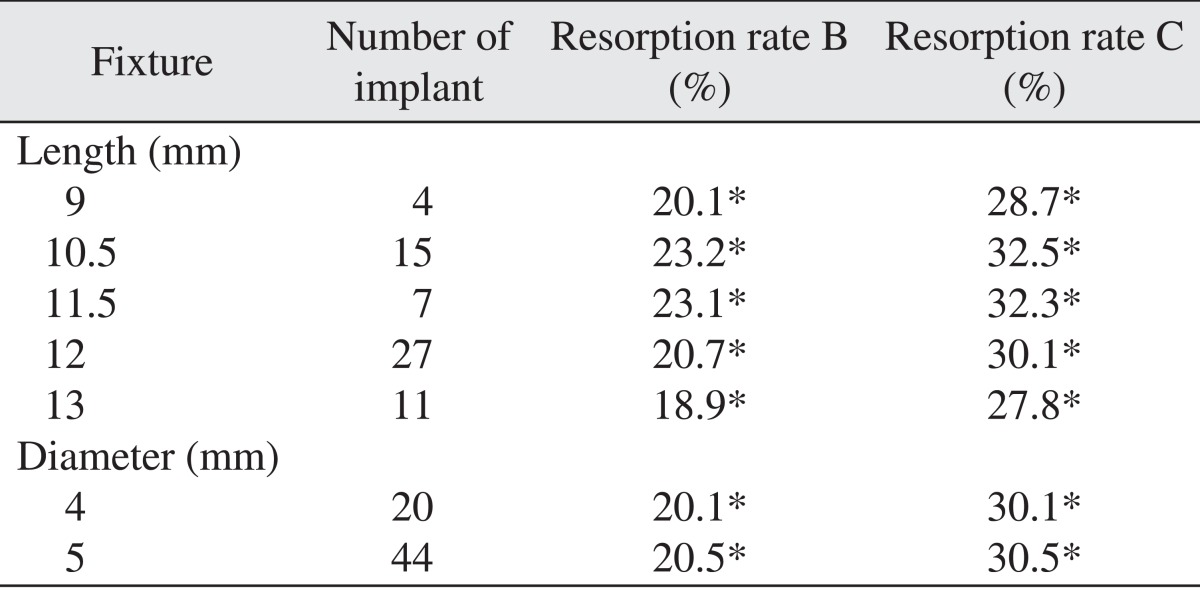
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
5. Bone resorption rate by implant placement region
Out of a total of 64 implants, 3 were placed in the first premolar region, 14, in the second premolar region, 27, in the first molar region, and 20, in the second molar region. Among these, the first molar region showed the highest resorption rate with 22.7% and 32.6% on 6 months after the surgery and on the final follow-up, respectively, whereas the first premolar region showed the lowest resorption rate with 20.3% and 29.8% on 6 months after the surgery and on the final follow-up, respectively. Note, however, that the difference in resorption rate of maxillary sinus bone graft by implant placement region was not significant.(Table 6)
Table 6.
Resorption rate of bone material by placement region
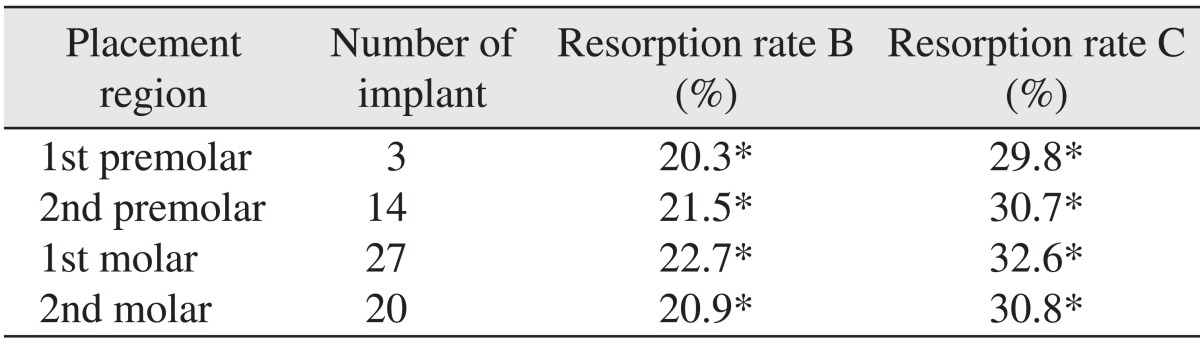
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
6. Bone resorption rate by local infection and surgical complication
Among the 29 maxillary sinus bone graft surgeries of 24 patients, 3 (10.3%) cases suffered from CMS. In 4 (13.8%) maxillary sinuses, perforation of the sinus membrane occurred when the sinus membrane was elevated, but they were cured without any specific abnormality in the perforated region. Local infection and surgical complication did not wield significant impact on the resorption rate of maxillary sinus bone graft.(Table 7)
Table 7.
Resorption rate of bone material according to local infection and surgical complication
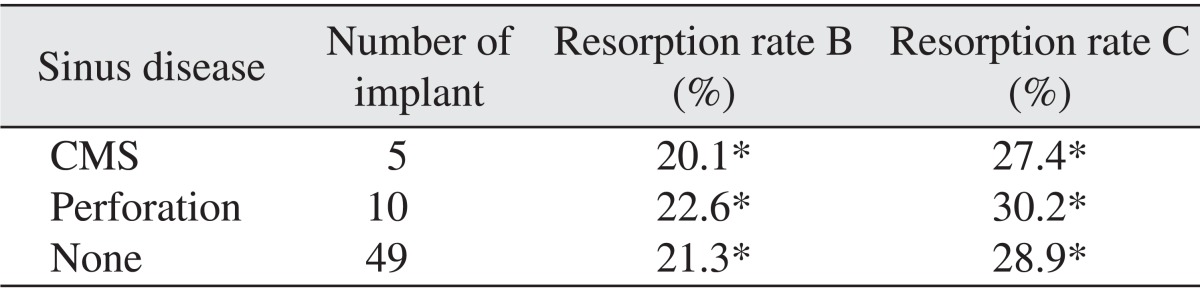
(CMS: chronic maxillary sinusitis)
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up. Perforation: maxillary sinus perforation.
7. Bone resorption rate by residual bone height
In this study, the range of residual bone height was 1.89 to 6.56 mm. This study divided the residual alveolar bone height into two groups: less than 4 mm (22 implants) and over 4 mm (42 implants). The resorption rate of maxillary sinus bone graft in the higher residual bone height group (>4 mm) was significantly higher than that in the lower residual bone height group (<4 mm) (P<0.05).(Table 8)
Table 8.
Resorption rate of bone material by residual bone height
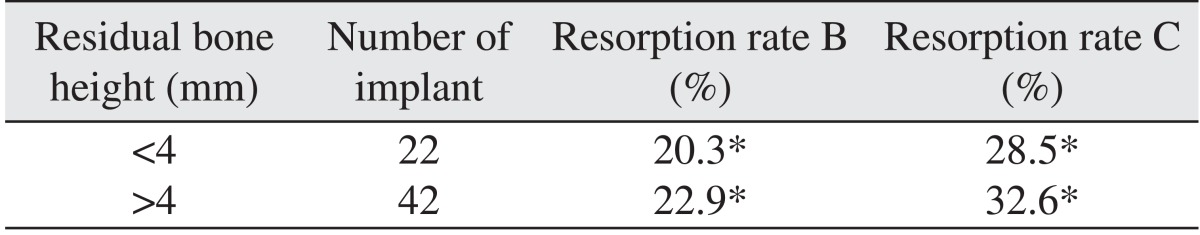
*Statistically significant difference, P<0.05.
Resorption rate B: resorption rate of bone material 6 months after the surgery. Resorption rate C: resorption rate of bone material on the final follow-up.
8. Clinical evaluation and marginal bone resorption
During the healing and follow-up period of these 24 patients, the implants did not exhibit any sign or symptom of pain, infection, and neuropathy. In addition, the panoramic views did not show peri-implant radiolucency, with the implants exhibiting no mobility. Therefore, the dental implant survival rate was pegged at 100%.
According to the panoramic views taken immediately after the implant surgery and at the final follow-up time, the average marginal bone resorption of all 64 implants was 1.28 mm during an average monitoring period of 2.7 years. Marginal bone resorption due to the difference in implant placement stage showed a statistically significant difference at the final follow-up time, with the one-stage surgery group exhibiting less resorption.(Table 9)
Table 9.
Implant placement stage and marginal bone resorption
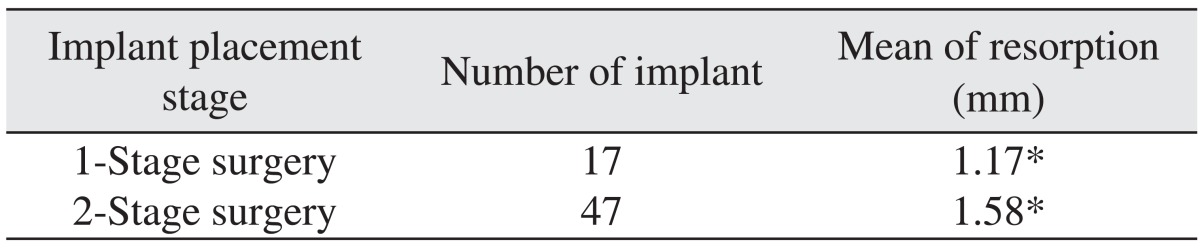
*Statistically significant difference, P<0.05.
In 5 patients, 5 implants exhibited increased marginal bone resorption. Two implants in two male patients with CMS, one implant in one male patient with perforation of the sinus membrane, and two implants in one male patient and one female patient without any disease showed more than 2.0 mm progressive marginal bone resorption during an average monitoring period of 2.7 years. Therefore, the success rate of the implants was 92.2%.
IV. Discussion
After the loss of the maxillary molar tooth, the alveolar bone shows rapid resorption, and the size of the maxillary sinus also increases. Therefore, only the thin bone wall between the oral cavity and the maxillary sinus may remain. To place an implant for such patients, bone graft is done for bone augmentation. Maxillary sinus bone graft surgery is now predictable and is regarded as a safe surgical procedure. Most of the bone graft materials are known to yield a good result in terms of the survival rate of implant, but the maxillary sinus bone graft materials may be absorbed over time7.
According to Wang and Luo8, age was one of the major factors influencing bone resorption. In this study, the bone resorption rate of patients in the 41 to 50-year-old age group was 23.0% on 6 months after the surgery and 32.7% at the final follow-up time; these were higher than the rates of the other age groups. Note, however, that the difference in bone resorption rate by patient's age was not statistically significant.(Table 1)
Andreasen et al.9 reported that the gender of the patient was significantly related to bone resorption activity and observed a different degree of bone resorption, noting that it was higher in women than in men. In contrast, this study found the bone graft resorption rate in the male patients' group at the time of final follow-up to be significantly higher than that in the female patients' group. Nonetheless, the difference in bone graft resorption rate by patients' gender 6 months after the surgery was not significant.(Table 2)
Various materials have been used for grafting the sinus floor. The bone graft materials can be categorized into four groups: autogenous bone, allogenous bone, xenogenous bone, and synthetic bone. These bone graft materials can be used alone or in combination with each other. Autogenous bone has been considered the 'gold standard'10 of bone graft material for a long time because of its osteoconductive, osteoinductive, and osteogenic properties11. According to Dragoo and Sullivan12, autogenous bone is a bone graft material with the highest regenerative capability when it comes to alveolar bone defects. Autogenous bone including calvarium, tibia, ribs, or iliac bone can be used. Due to problems such as inconvenience of hospitalization, general anesthesia, postoperative pain, and burden of medical expenses, however, its use has been limited. Alternatively, autogenous bone from the oral cavity such as mental region, mandibular ramus, and zygomatic region has often been used13. In particular, mandibular ramus bone has high ratio of cortical bone, but the harvest of the ramus bone is difficult. Nonetheless, it is the preferred bone graft material for the maxillary sinus due to the low risk of edema and nerve injury compared to mental bone.
When maxillary sinus bone graft using autogenous bone was performed, many cases exhibited considerable bone resorption over time. Furthermore, a study reported that using 100% autogenous bone as bone graft material enabled faster absorption compared to using autogenous bone in combination with bone substitutes. At present, autogenous bone in combination with bone substitutes is used widely14. A histological analysis proved that using bone graft material combining autogenous bone and Bio-Oss enables shortening the time of formation of new bone15. No studies have shown that autogenous bone and bone substitute mixing ratio differences have an impact on the success rate of dental implants, however.
Hatano et al.16 performed simultaneous implant placement with maxillary sinus bone grafting using autogenous bones and xenogeneic bones (Bio-Oss) mixed at a 2 c: 1 ratio and conducted a long-term clinical evaluation. They found that the survival of implants after 2 to 3 years was 94.2%, and that the height of the maxillary sinus floor was similar to the level of the implant apex area or slightly lower. They confirmed that, even in cases grafted with a mixture of autogenous and xenogeneic bones, repneumatization progressed continuously for 2 to 3 years, and that no great change was observed after that. They also concluded that stable maintenance of the height of maxillary sinus bone grafting materials played an important role in implant success.
Kim et al.17 also reported the results of clinical studies on sinus bone resorption after sinus bone grafting and implant placement. In their study, the mean height of the remaining alveolar bone before the surgery, immediately after the surgery, and 1 year after the surgery was 4.9 mm, 19.0 mm, and 17.2 mm, respectively, in group I (xenograft + minimal amount of autogenous bone) and 4.0 mm, 19.2 mm, and 17.8 mm, respectively, in group II (allograft + xenograft + minimal amount of autogenous bone). In this study, the resorption rate after the single graft of autogenous bone was 23.1% and 32.1% on 6 months after the surgery and on the final follow-up, respectively, whereas the resorption rate after a combined graft of autogenous bone and Bio-Oss was 18.9% and 28.6% on 6 months after the surgery and on the final follow-up, respectively. The difference in bone resorption rate by graft material (single autogenous bone or autogenous bone in combination with Bio-Oss) was statistically significant (P<0.05).(Table 3)
Some researchers suggested that, with higher residual bone height (>5 mm), the implant could have better primary stability, and that it would be suitable for maxillary sinus elevation with bone graft and one-stage surgery. When the residual bone height was lower than 5 mm, two-stage surgery was recommended18,19. Corinaldesi et al.20 showed that patients undergoing the simultaneous approach (20 sites) showed mean residual bone height of 5.9±1.77 mm (range, 4 to 9 mm) at baseline. Among patients undergoing the delayed approach (14 sites), mean residual bone height decreased to 3.5±1.16 mm (range, 1.5 to 5 mm). In this study, the mean residual bone height of the one-stage surgery group and two-stage surgery group was 5.67 mm and 3.91 mm, respectively. The resorption rate of the maxillary sinus bone graft in the one-stage surgery group was significantly higher than that in the two-stage surgery group. This is because one-stage surgery for these cases all involved single autogenous bone graft material.(Table 4)
Some studies reported that the small surface area of implant had risk of increasing the resorption rate21. In this study, however, there was no correlation between the implant size and resorption rate.(Table 5) According to Kim and Lee22, there was no correlation with the implant placement region. Similarly, this study found no significant difference by placement region.(Table 6)
Cheong et al.23 reported that 105 maxillary sinuses in 87 patients showed high prevalence of sinus disease. This result supported the fact that maxillary sinus disease was very common among patients who were planning implantation in the maxillary posterior areas. In this study, CMS developed in 3 (10.3%) cases. Note, however, that neither maxillary sinus bone grafting material loss nor implant failure occurred. CMS did not show significant correlation with the resorption rate of maxillary sinus bone graft.(Table 7)
According to Pjetursson et al.24, the most common intraoperative complication was the perforation of the sinus membrane. The mean prevalence of membrane perforation was 19.5%, and range was 0 to 58.3%. Significant statistical correlation was found between residual alveolar bone height and membrane perforation. Due mainly to technical difficulties, maxillary sinus membrane perforation occurs more frequently with a small height of residual alveolar bone. The study by Ardekian et al.25 found no statistical difference in the success rate of the immediate implants placed with sinus bone grafting in patients whose membrane was perforated versus those patients in whom an intact membrane was maintained. In our study, perforation of the sinus membrane was observed in 4 (13.8%) patients. Nevertheless, perforation of the sinus membrane did not show significant correlation with the resorption rate of maxillary sinus bone graft.(Table 7)
According to Jensen et al.26, residual alveolar bone height had the most influence on the survival rate of the implant placed after maxillary sinus elevation, and, if the height was 7 mm or less, bone graft must be done for implant placement. The study by Herzberg et al.21 showed that residual bone height of less than 4 mm tended to promote graft material resorption. Note, however, that this study showed the opposite result. The resorption rate of maxillary sinus bone graft in the higher residual bone height group (>4 mm) was significantly higher than that for the lower residual bone height group (<4 mm). This is because, with higher residual bone height (>4 mm), single autogenous bone graft material was used for the elevation of maxillary sinus floor.(Table 8)
Herzberg et al.21 examined 70 patients with 212 implants placed in 81 maxillary sinus regions during the period 1995 to 2000 and reported 95.5% and 83.7% cumulative survival and success rates, respectively, for 4.5 years. The study of Kim et al.27 showed that the mean marginal bone resorption around the implants was 0.69 mm 1 year after prosthodontic loading. Marginal bone resorption of more than 1.5 mm occurred in 9 implants, for a success rate of 88%. Kim et al.17 also reported mean marginal bone loss--1 year after prosthodontic loading and after 20.8 months' follow-up--of 0.6 mm and 0.7 mm, respectively, in group 1 (xenograft + minimal amount of autogenous bone). At least 3 implants showed bone resorption of more than 1.5 mm within 1 year of loading, for a success rate of 93.9%. On the other hand, mean marginal bone loss 1 year after prosthodontic loading and after 19.7 months' follow-up was 0.7 mm and 1.0 mm, respectively, in group 2 (allograft + xenograft + minimal amount of autogenous bone). A total of 4 implants showed bone resorption of more than 1.5 mm within 1 year of loading, for a success rate of 83.3%.
In this study, marginal bone resorption was measured to be a minimum of 0.61 mm to a maximum of 3.54 mm and a mean of 1.28 mm during an average of 2.7 years after prostheses placement. The one-stage surgery and two-stage surgery showed significant differences in marginal bone resorption, with less bone resorption observed in the former.(Table 9) Two implants in two male patients with CMS, one implant in one male patient with perforation of the sinus membrane, and two implants in one male patient and one female patient without any disease showed more than 2.0 mm progressive marginal bone resorption during an average monitoring period of 2.7 years. Furthermore, overall, no falling off or looseness, pain, infection and abnormal feeling, or inflammation in the peri-implant was observed for the 64 implants. The panoramic views showed no shadows during the 24 to 68 months' follow-up period. Therefore, the success rate and survival rate of the implant were 92.2% and 100%, respectively.
V. Conclusion
This study reported the clinical findings on sinus elevation surgery with immediate implant placement and subsequent implant placement using autogenous bone graft or autogenous bone in combination with Bio-Oss graft. Based on the evaluation results on the resorption level using the panoramic views taken before the surgery, immediately after the surgery, 6 months after the surgery, and final follow-up time, the following conclusions were drawn:
1. The bone graft resorption rate in the male patients group on the final follow-up was significantly higher than that in the female patients group; note, however, that there was no significant difference in bone resorption rate by patients' gender 6 months after surgery.
2. The bone resorption rate after single autogenous bone graft was significantly higher compared to the autogenous bone combined with Bio-Oss.
3. The resorption rate of maxillary sinus bone graft in the one-stage surgery group was significant higher than that in the two-stage surgery group.
4. The resorption rate of maxillary sinus bone graft in the higher residual bone height group (>4 mm) was significant higher than that in the residual bone height group (<4 mm).
5. There was no significant correlation with the resorption rate of maxillary sinus bone graft among patients' age, implant size, implant placement region, local infection, and surgical complication.
6. During an average monitoring period of 2.7 years, the success rate and survival rate of the implant were 92.2% and 100%, respectively.
The results suggest that maxillary sinus floor elevation with autogenous bone graft through the lateral window approach technique is feasible and safe, and that the elevation of maxillary sinus floor is predictable in implant rehabilitation for patients with reduced vertical bone height in the posterior maxillary region.
References
- 1.Smith LP, Ng M, Grubor D, Chandu A. Outcomes of dental implants placed in a surgical training programme. Aust Dent J. 2009;54:361–367. doi: 10.1111/j.1834-7819.2009.01163.x. [DOI] [PubMed] [Google Scholar]
- 2.Boyne PJ, James RA. Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg. 1980;38:613–616. [PubMed] [Google Scholar]
- 3.Tatum H., Jr Maxillary and sinus implant reconstructions. Dent Clin North Am. 1986;30:207–229. [PubMed] [Google Scholar]
- 4.Wallace SS, Froum SJ. Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol. 2003;8:328–343. doi: 10.1902/annals.2003.8.1.328. [DOI] [PubMed] [Google Scholar]
- 5.Mellonig JT, Bowers GM, Bailey RC. Comparison of bone graft materials. Part I. New bone formation with autografts and allografts determined by Strontium-85. J Periodontol. 1981;52:291–296. doi: 10.1902/jop.1981.52.6.291. [DOI] [PubMed] [Google Scholar]
- 6.Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1986;1:11–25. [PubMed] [Google Scholar]
- 7.Scarano A, Degidi M, Iezzi G, Pecora G, Piattelli M, Orsini G, et al. Maxillary sinus augmentation with different biomaterials: a comparative histologic and histomorphometric study in man. Implant Dent. 2006;15:197–207. doi: 10.1097/01.id.0000220120.54308.f3. [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Luo Y. Influencing factors on bone resorption after alveolar bone grafting. Zhonghua Kou Qiang Yi Xue Za Zhi. 2005;40:373–375. [PubMed] [Google Scholar]
- 9.Andreasen JO, Paulsen HU, Yu Z, Schwartz O. A long-term study of 370 autotransplanted premolars. Part III. Periodontal healing subsequent to transplantation. Eur J Orthod. 1990;12:25–37. doi: 10.1093/ejo/12.1.25. [DOI] [PubMed] [Google Scholar]
- 10.Tong DC, Rioux K, Drangsholt M, Beirne OR. A review of survival rates for implants placed in grafted maxillary sinuses using meta-analysis. Int J Oral Maxillofac Implants. 1998;13:175–182. [PubMed] [Google Scholar]
- 11.Klijn RJ, Meijer GJ, Bronkhorst EM, Jansen JA. A meta-analysis of histomorphometric results and graft healing time of various biomaterials compared to autologous bone used as sinus floor augmentation material in humans. Tissue Eng Part B Rev. 2010;16:493–507. doi: 10.1089/ten.TEB.2010.0035. [DOI] [PubMed] [Google Scholar]
- 12.Dragoo MR, Sullivan HC. A clinical and histological evaluation of autogenous iliac bone grafts in humans. I. Wound healing 2 to 8 months. J Periodontol. 1973;44:599–613. doi: 10.1902/jop.1973.44.10.599. [DOI] [PubMed] [Google Scholar]
- 13.Misch CM. Comparison of intraoral donor sites for onlay grafting prior to implant placement. Int J Oral Maxillofac Implants. 1997;12:767–776. [PubMed] [Google Scholar]
- 14.Valentini P, Abensur DJ. Maxillary sinus grafting with anorganic bovine bone: a clinical report of long-term results. Int J Oral Maxillofac Implants. 2003;18:556–560. [PubMed] [Google Scholar]
- 15.Tawil G, Mawla M. Sinus floor elevation using a bovine bone mineral (Bio-Oss) with or without the concomitant use of a bilayered collagen barrier (Bio-Gide): a clinical report of immediate and delayed implant placement. Int J Oral Maxillofac Implants. 2001;16:713–721. [PubMed] [Google Scholar]
- 16.Hatano N, Shimizu Y, Ooya K. A clinical long-term radiographic evaluation of graft height changes after maxillary sinus floor augmentation with a 2:1 autogenous bone/xenograft mixture and simultaneous placement of dental implants. Clin Oral Implants Res. 2004;15:339–345. doi: 10.1111/j.1600-0501.2004.00996.x. [DOI] [PubMed] [Google Scholar]
- 17.Kim YK, Yun PY, Kim SG, Kim BS, Ong JL. Evaluation of sinus bone resorption and marginal bone loss after sinus bone grafting and implant placement. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e21–e28. doi: 10.1016/j.tripleo.2008.09.033. [DOI] [PubMed] [Google Scholar]
- 18.McCarthy C, Patel RR, Wragg PF, Brook IM. Sinus augmentation bone grafts for the provision of dental implants: report of clinical outcome. Int J Oral Maxillofac Implants. 2003;18:377–382. [PubMed] [Google Scholar]
- 19.Fugazzotto PA, Vlassis J. Long-term success of sinus augmentation using various surgical approaches and grafting materials. Int J Oral Maxillofac Implants. 1998;13:52–58. [PubMed] [Google Scholar]
- 20.Corinaldesi G, Pieri F, Sapigni L, Marchetti C. Evaluation of survival and success rates of dental implants placed at the time of or after alveolar ridge augmentation with an autogenous mandibular bone graft and titanium mesh: a 3- to 8-year retrospective study. Int J Oral Maxillofac Implants. 2009;24:1119–1128. [PubMed] [Google Scholar]
- 21.Herzberg R, Dolev E, Schwartz-Arad D. Implant marginal bone loss in maxillary sinus grafts. Int J Oral Maxillofac Implants. 2006;21:103–110. [PubMed] [Google Scholar]
- 22.Kim BJ, Lee JH. The retrospective study of survival rate of implants with maxillary sinus floor elevation. J Korean Assoc Oral Maxillofac Surg. 2010;36:108–118. [Google Scholar]
- 23.Cheong CS, Cho BH, Hwang DS, Jung YH, Naa KS. Evaluation of maxillary sinus using cone-beam CT in patients scheduled for dental implant in maxillary posterior area. J Korean Assoc Oral Maxillofac Surg. 2009;35:21–25. [Google Scholar]
- 24.Pjetursson BE, Tan WC, Zwahlen M, Lang NP. A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol. 2008;35(8 Suppl):216–240. doi: 10.1111/j.1600-051X.2008.01272.x. [DOI] [PubMed] [Google Scholar]
- 25.Ardekian L, Oved-Peleg E, Mactei EE, Peled M. The clinical significance of sinus membrane perforation during augmentation of the maxillary sinus. J Oral Maxillofac Surg. 2006;64:277–282. doi: 10.1016/j.joms.2005.10.031. [DOI] [PubMed] [Google Scholar]
- 26.Jensen OT, Shulman LB, Block MS, Iacono VJ. Report of the Sinus Consensus Conference of 1996. Int J Oral Maxillofac Implants. 1998;13(Suppl):11–45. [PubMed] [Google Scholar]
- 27.Kim YK, Yun PY, Im JH. Clinical retrospective study of sinus bone graft and implant placement. J Korean Assoc Maxillofac Plast Reconstr Surg. 2008;30:249–257. [Google Scholar]