Abstract
Objectives:
Levosimendan is a calcium sensitizer drug which has been used in cardiac surgery for the prevention of postoperative low cardiac output syndrome (LCOS) and in difficult weaning from cardiopulmonary bypass (CPB). This study aims to evaluate perioperative hemodynamic effects of levosimendan pretreatment in patients for off-pump coronary artery bypass graft (OPCABG) surgery with low left ventricular ejection fractions (LVEF < 30%).
Materials and Methods:
Fifty patients undergoing OPCABG surgery with low LVEF (<30%) were enrolled in the study. Patients were randomly divided in two groups: Levosimendan pretreatment (Group L) and placebo pretreatment (Group C) of 25 each. Group L, patients received levosimendan infusion 200 μg/kg over 24 h and in Group C Patients received placebo. The clinical parameters measured before and after the drug administration up to 48 h were heart rate (HR; for the hour after drug infusion), cardiac index (CI), and pulmonary capillary wedge pressure (PCWP). The requirement of inotropes, intraaortic balloon pump (IABP), CPB, intensive care unit (ICU) stay, and hospital stay were also measured.
Results:
The patients in group L exhibited higher CI and PCWP during operative in early postoperative period as compared to control group C. Group L also had a less requirement for inotropes, CPB support and IABP with shorter ICU stay as well as hospital stay.
Conclusion:
Levosimendan pretreatment (24 h infusion) in patient for OPCABG with poor LVEF shows better outcomes and hemodynamics in terms of inotropes, CPB and IABP requirements. It also reduces ICU stay.
KEY WORDS: Cardiac index, CPB, hemodynamic optimization, inotropic agents, LCOS, levosimendan, off-pump coronary artery bypass graft, OPCABG surgery, pulmonary capillary wedge pressure
Introduction
Off-pump coronary artery bypass graft (OPCABG) surgery has been used more often primarily to avoid complication of cardiopulmonary bypass (CPB) like systemic inflammatory response, global myocardial ischemia, and risk of aortic manipulation. In OPCABG surgery, the major concern is to maintain hemodynamics during manipulation like lifting and tilting of the heart or head low position of the patient requires exposing lateral or posterior wall of the heart. These manipulations will alter heart rate (HR) and arterial blood pressure (ABP), which ultimately lead to decrease in cardiac output (CO). During manipulation sometimes it may distort tricuspid or mitral valve making the patient hemodynamically unstable. Hemodynamic instability or decrease in CO is found in OPCABG surgery due to local ischemia, distortion of valve, or chamber or wall motion abnormality due to stabilizer. For these, optimization of preload and use of inotropes may be required to maintain hemodynamics.
Inotropes increase myocardial contractility at a cost of increase myocardial oxygen demand. This leads to ischemia and arrhythmias and use of inotropes in this condition may lead to severe compromise in hemodynamics.
Levosimendan exerts vasodilatory properties through activation of ATP-dependent potassium channels (K-ATP) in smooth muscles of peripheral, pulmonary, and coronary vessels with a unique mechanism of action. It enhances myofilament responsiveness to calcium by binding to cardiac troponin C, thereby stabilizing the tropomyosin molecule and prolonging the duration of actinmyosin overlap without a change in the net concentration of intracellular calcium and without increasing myocardial oxygen consumption.[1] It also activates K-ATP channels which are important mediators of ischemia and reperfusion injury and results in coronary vasodilatation to improve heart oxygenation and shows protective effects on the myocardium.[2,3] This leads to a decrease in both afterload and preload, increased coronary blood flow, and a resultant antischemic effect. It is therefore categorized as an antischemic inotropic agent.[4] It shows beneficial immunomodulatory, anti-inflammatory, and antioxidant properties to improve cardiac performance in cardiac ischemia[5] and has been shown to have favorable effects on coronary blood flow as it overrides normal autoregulatory vasodilatory mechanism of coronary circulation.[6] Thus, levosimendan has a potential benefit for patients with myocardial oxygen imbalance and requiring inotropes during OPCABG surgery with low ejection fractions (EF). In addition, an active protein-bound metabolite of levosimendan (OR-1855 OR-1896) may exert clinical effects up to 1 week because of its long half-life. This entire characteristic has encouraged us to study pretreatment of levosimendan in OPCABG surgery with low left ventricular EF (LVEF).[7]
OPCABG surgery achieves better in-hospital outcomes, similar completeness of revascularization, and shorter length of stay compared to conventional CABG.[8,9] The present study was conducted to evaluate the effect of levosimendan infusion preoperatively before 24 h on perioperative hemodynamic stability and myocardial performance in OPCABG surgery with poor LVEF (<30%).
Materials and Methods
The study was approved by the internal review board and ethics committee of the institute. During the preoperative visit, patients and their relatives were thoroughly explained about the study and written informed consent for the study was taken. The principles of the Declaration of Helsinki were followed during study.
The patients with single vessel disease requiring graft to left anterior descending artery, double vessel disease, and triple vessel disease with LVEF less than 30% and myocardial perfusion scan showing viability of the affected territory were included in the randomized, double blind study. Patients undergoing urgent, emergent, congenital, valve, aortic, or combined surgeries or who were treated with levosimendan within 3 months or with other inotropes within the previous week and patients with a preoperative intraaortic balloon pump (IABP), significant pulmonary disease, renal dysfunction, liver dysfunction, redo-CABG, or arrhythmias with bundle branch block were not included in the study.
Patients with coronary artery disease (CAD) and low LVEF (<30%) scheduled to undergo OPCABG were prospectively enrolled in the study at our institute. The LVEF was determined by transthoracic echocardiography (TTE). Patients were admitted to the cardiac intensive care unit (ICU) 24 h before the surgery and Swan Ganz Catheter (VIP type-Edward Life Science) was introduced under local anesthesia (LA). CO was measured by injection of cold saline. Patients were randomly assigned according to the medical record numbers to receive a preoperative dose of levosimendan (Inj. Semenda-12.5 mg/ml, Lupin lab.) 200 μg/kg dose is dissolved in 50 ml of normal saline (NS) and started at the rate of 2 ml/h for 24 h in group L or a placebo (Inj. Multivitamin-10 ml, NBZ Pharma) dissolved in NS to mimic the color of levosimendan in group C. The method of administration was similar in both groups. The manner of administration of levosimendan was chosen based on previous experience with the drug.[10]
All patients underwent continuous monitoring of HR, ABP, pulse oximetry, cardiac index (CI), and pulmonary capillary wedge pressure (PCWP). Central venous pressure (CVP), urine output, capnography, nasal temperature, and arterial blood gases (ABG) were also monitored. Hemodynamic parameters were measured for the 1st h after the drug was administered. Readings were taken within the 1st h, at times 0 min (t0), 15 min (t15), 30 min (t30), 45 min (t45), and 60 min (t60) after the administration of the drug at t0. Time 0 (T0 = t0) was defined as the initial hemodynamic measurement before starting of the drug. Time 1 (T1) was recorded 24 h after the administration of levosimendan dose in operation theatre (OT) before induction. Time 2 (T2) denotes the mean of hemodynamic parameters recorded at every 30 min during the surgery. Time 3 (T3) reflects hemodynamic parameters at the time of admission in ICU immediately after surgery. Time 4 (T4), Time 5 (T5), and Time 6 (T6) denote hemodynamic parameters at 12, 24, and 48 h after surgery, respectively.
Anesthetic management and surgical procedures were same in both the groups. Induction and maintenance of general anesthesia with endotracheal intubation was standardized in both the groups. Patients were induced with inj. fentanyl (5 μg /kg), inj. midazolam (0.1 mg /kg), and inj. vecuronium bromide (0.15 mg/kg) + inj. propofol (1 mg/kg) to facilitate intubation and were maintained with air + O2 + sevofluorane and inj. fentanyl (1 μg/kg/h) infusion and inj. vecuronium.(0.1 mg/kg/h). All procedures were performed using OPCABG surgery; but in a few patients (one patient in test group and eight in control group), surgery were completed with help of CPB due to hemodynamic instability along with high inotropic support. CABGs were attempted using the left internal mammary artery (LIMA) and reversed saphenous vein grafts (RSVG) as conduits. Left anterior descending (LAD) artery was revascularized by LIMA, while other coronary arteries were revascularized by RSVG via an aortocoronary anastomosis for complete revascularization.
Perioperative adverse event were analyzed as follows:
Patients requiring high inotropic support defined as requirement of dobutamine > 5 μg/kg/min and/or adrenaline > 0.1 μg/kg/min and/or noradrenaline > 0.1 μg/kg/min). LCOS were defined as presence of low CI (2.2 L/min/m2) with elevated PCWP (>16 mmHg) and partial pressure of arterial oxygen (PaO2) < 60 mm Hg. Acute renal failure were defined when serum (S.) creatinine increases >50% from baseline with or without oliguria (urine output < 0.5 ml/kg/h) or requiring dialysis. Cerebrovascular accidents (CVA) were found if development of a new focal neurological deficit or coma persisting for >48 h (after metabolic causes have been ruled out). A neurologic change persisting <48 h was considered as a transient ischemic attack. Postoperative mortality was defined if death occurred during hospitalization or within 30 days after surgery.
Statistical Analysis
IBM Statistical Package for Social Sciences (SPSS) software version 20 was used for the statistical analysis. Student's t-test and analysis of variance (ANOVA) were used to determine the differences between the groups. P-value < 0.05 was considered significant.
Results
Fifty patients with low LV function (<30%) admitted to U. N. Mehta Institute of Cardiology and Research Center was enrolled for the study during July-December 2012. The patients were randomly divided into two groups of 25 each. Inj. levosimendan and placebo were injected in group L and C, respectively.
The data from these 50 patients were included in statistical analysis. Hemodynamic data were recorded at various time intervals. General and demographic characteristics [Table 1a], Preoperative characteristics [Table 1b] and preoperative medications [Table 2] were comparable between both the groups.
Table 1a.
Characteristics of patients undergoing off-pump coronary artery bypass grafting

Table 1b.
Characteristics of patients undergoing off-pump coronary artery bypass grafting
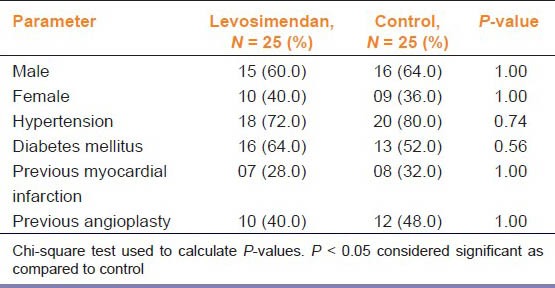
Table 2.
Preoperative medications administered in levosimendan and control groups

Preoperative ICU stay was uneventful in both the groups during Swan Ganz Cathater (VIP type) introduction. Table 3 lists the adverse effects observed during 24 h of levosimendan infusion. A total of nine patients developed mild hypotension most of them resolved with fluid infusions (seven in the levosimendan and two in the control group), but two patients in the levosimendan and one patient in the control group required vasopressors. Headache was observed in three patients in the levosimendan group and in one patient in the control group. Nausea and vomiting were observed in two patients in levosimendan group which were treated symptomatically.
Table 3.
Adverse events occurring during 24 h preoperative infusion in levosimendan and control group

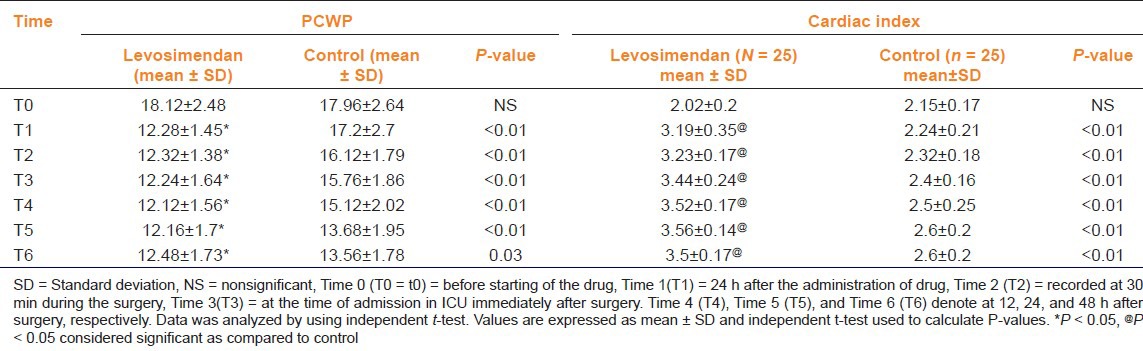
Hemodynamic data recorded at T0 (just before infusions) were similar in both the groups. HR was comparable in 1st h in both the groups [Table 4]. PCWP remained low in the levosimendan group as compared to the control group throughout the perioperative period. A marked reduction in PCWP was observed after 24 h of infusion of levosimendan and was sustained for 48 h postoperatively [Table 5]. Table 5 shows that CI was high in the levosimendan group as compared to the control group and improvement in CI was observed after 24 h of infusion of levosimendan and was sustained for 48 h postoperatively.
Table 4.
Heart rate during 1st h after levosimendan and placebo infusion
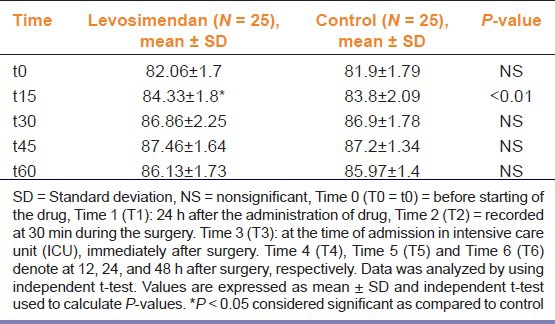
Table 5.
Changes in pulmonary capillary wedge pressure (PCWP) and cardiac index during perioperative period in levosimendan and control group
Patients in the test group showed significant hemodynamic stability in the form of less development of AF, less requirements of inotropic support, IABP and CPB as compared to control group. Only one patient needed CPB and IABP in test group as compared to eight patients in the control group due to hemodynamic instability [Table 6]. AF was treated with inj. amiodarone infusion.
Table 6.
Intraoperative and postoperative adverse events
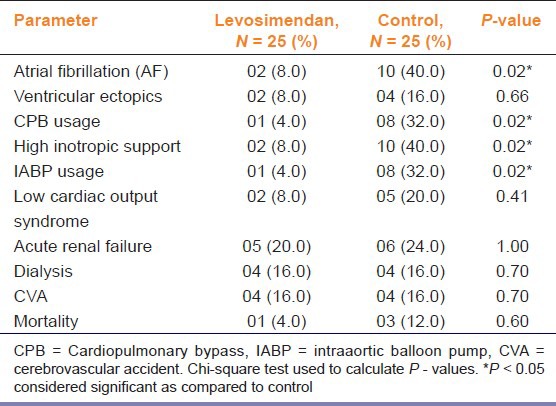
Ventricular ectopics were observed in two patients in the test group and four patients in the control group, which was treated with inj. lignocaine (2% Xylocard).
Renal dysfunction was treated with inj. frusemide, intravenous (IV) fluids, and dialysis. Mortality observed in one patient in group L and three patients in group in the time span of 5-30 days after surgery. All other adverse events found were statistically not significant.
Total ICU stay were significantly low (53.8 h in group L as compared to 59.56 h in group C) (P < 0.0001) and total hospital stay was significantly low (15.20 days in group L as compared to 19.80 days in group C) (P < 0.0001). Time on ventilator and no and types of grafts were comparable in both the groups.
Discussion
Levosimendan has been used in the patients with poor left ventricular function, patients with difficulty in weaning from CPB as well as treatment of postoperative low CO syndrome (LCOS).[11]
Levosimendan exerts vasodilatory properties through activation of K-ATP in smooth muscles of peripheral, pulmonary, and coronary vessels. If levosimendan is used after induction of anesthesia, there is possibility of additive effect of anesthetic agents leading to hemodynamic instability in the form of hypotension and tachycardia. These disturbances also aggravated at the time of grafting because of manipulations of heart in OPCABG. Active protein-bound metabolite (OR-1855 and OR-1896) of levosimendan may exert clinical effects up to 1 week because of its long half-life. Levosimendan 24 h preoperatively may avoid hypotension during operation and get benefits of increase in CI and decrease in PCWP.
In the present study, preoperative levosimendan infusion used before 24 h of surgery in patients with CAD and low LVEF posted for OPCABG surgery. We observed that hemodynamic parameters were improved after surgery in both the groups, but improvement with quicker onset of action was observed in patients treated with levosimendan were more. There was improvement in CI and decreasing PCWP perioperatively as well as decreased requirement of inotropes, CPB, and IABP support in levosimendan treated group. It was also observed that preoperative levosimendan infusions reduced the ICU stay and hospital stay.
In the present study, levosimendan infusion was well-tolerated with a low incidence of adverse effects. Lilleberg et al.,[10] demonstrated that high doses of levosimendan as a bolus, shows an increase in the CO resulting into increased stroke volume and increase in the HR which may make it unsuitable for the OPCABG surgery with low LVEF. Therefore, we decided to administer the total dose over 24 h infusions without bolus dose administration. In the 1st h of infusion, we did not observe any significant increase in HR.
OPCABG surgery has been used more often, primarily to avoid complication of CPB[8,9] and during surgery, frequent heart displacement can cause hemodynamic instability; more significantly in patients with low LVEF. During handling of the heart, there is high risk like increase in filling pressures, which may decrease CI and increases right ventricular end diastolic pressure.[12]
There was no significant difference in complete revascularization of all the patients in the present study. Patients in levosimendan group showed better hemodynamic stability during surgery. Requirement of high inotropic support more (10 in group C as compared to two in group L) in the control group as compared to levosimendan group. Moreover, only one patient in group L required CPB and IABP (as cardiac support) compared to eight patients in the group C.
Calcium sensitizers are regarded superior to catecholamine during myocardial stunning.[13] Levosimendan possesses calcium sensitizing activity which produces positive inotropic effect resulting into increased myocardial contractility. However, this is accomplished without increase in cyclic adenosine monophosphate (cAMP) and associated intracellular calcium levels. The end result is no increase in myocardial O2 demand with improved cardiac contractility especially in patients with low LVEF.[13] Levosimendan has positive lusitropic (myocardial relaxation) effects; preserving or improving diastolic properties demonstrated in human clinical studies.[14] We also observed the similar effect in the form of decrease in PCWP.
Follath et al., reported that the levosimendan 24-h infusion in patients with decompensated low-output heart failure increases the CO and decrease in the PCWP. Hemodynamic improvement was achieved better in patients receiving levosimendan compared to dobutamine. Levosimendan also reduced the 1- and 6-month mortality as compare to dobutamine. Levosimendan produced less myocardial ischemia and cardiac arrhythmias than dobutamine.[15]
Tasouli et al.,[16] compared 45 patients with LCOS treated with levosimendan at two different time points in another randomized study. The patients were treated with inotropes and/or balloon counter pulsation (IABP). The study showed better results in those who were treated earlier with levosimendan, having a shorter time on inotropic support, a lower incidence of sepsis, and a shorter ICU stay and hospital stay.[17,18,19] During our study, we have observed similar results.
Levosimendan may also have significant anti-inflammatory properties. Data from various studies suggest that levosimendan might have antiarrhythmic effects, although the outcome of effect in atrial fibrillation (AF) remains controversial.[20]
The dosage of the test drug (levosimendan) employed in the current study differed from previously reported studies.[11] We preferred an infusion of levosimendan without bolus to avoid increase in HR within the hour of administering the bolus dose.
Though the number of patients included in the current study is reasonably good as compared to other reports, there is a need to study in large number of patients with low LVEF undergoing OPCABG surgery with a preoperative infusion of levosimendan for 24 h. Our study has several limitations; the CI and PCWP were measured only for 48 h of the postoperative period, in spite of levosimendan duration of action lasting for 1 week. Moreover, the assessment of myocardial contractility by echocardiogram was not performed and we did not measure myocardial markers for damage, which would have shown cardioprotactive action of levosimendan. Continuous CO (CCO) monitoring may increase the hemodynamic details during surgery and early postoperative period. Measurement of mixed venous oxygen saturation (SVO2) might add to the information in the current data set. Moreover, use of transesophageal echocardiography (TEE) performed by the same individual might have been useful to minimize subjective variations. Despite these considerations, favorable results with levosimendan infusion nonetheless provide a stimulus for further research and its use in routine clinical practice.
Conclusions
Preoperative levosimendan infusion in patients with low LVEF undergoing OPCABG was associated with greater improvement in hemodynamic stability during the surgery and early postoperative period. It shows faster onset of action, lower use of inotropic support, CPB, and IABP; including shorter ICU and hospital stay and lower rate of complications as well as morbidity resulting into a reduced financial burden.
Despite our limitations, the current results advocate routine use of levosimendan protocol in patients with low LVEF undergoing OPCABG surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Lehmann A, Boldt J, Kirchner J. The role of Ca++ -sensitizers for the treatment of heart failure. Curr Opin Crit Care. 2003;9:337–44. doi: 10.1097/00075198-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Haikala H, Nissinen E, Etemadzadeh E, Levijoki J, Linden IB. Troponin C-mediated calcium sensitization induced by levosimendan does not impair relaxation. J Cardiovasc Pharmacol. 1995;25:794–801. doi: 10.1097/00005344-199505000-00016. [DOI] [PubMed] [Google Scholar]
- 3.Toller WG, Stranz C. Levosimendan, a new inotropic and vasodilator agent. Anesthesiology. 2006;104:556–69. doi: 10.1097/00000542-200603000-00024. [DOI] [PubMed] [Google Scholar]
- 4.Zinovic IH, Zinovic SH, Milanovic R. Levosimendan in acute heart failure. Signa Vitae. 2008;3(Suppl 1):S13–6. [Google Scholar]
- 5.Liu T, Li G, Xu G. Levosimendan may prevent postoperative atrial fibrillation through anti-inflammatory and antioxidant modulation. J Cardiothorac Vasc Anesth. 2009;23:757–8. doi: 10.1053/j.jvca.2008.09.022. [DOI] [PubMed] [Google Scholar]
- 6.Gruhn N, Nielsen-Kudsk JE, Theilgaard S, Bang L, Olesen SP, Aldershvile J. Coronary vasorelaxant effect of levosimendan, a new inodilator with calciumsensitizing properties. J Cardiovasc Pharmacol. 1998;31:741–9. doi: 10.1097/00005344-199805000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Antila S, Pesonen U, Lehtonen L, Tapanainen P, Nikkanen H, Vaahtera K, et al. Pharmacokinetics of levosimendan and its active metabolite OR-1896 in rapid and slow acetylators. Eur J Pharm Sci. 2004;23:213–22. doi: 10.1016/j.ejps.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Al-Ruzzeh S, Ambler G, Asimakopoulos G, Omar RZ, Hasan R, Fabri B, et al. United Kingdom Multi-Center Comparative Analysis of Early Clinical Outcome. Off-Pump Coronary Artery Bypass (OPCAB) surgery reduces risk-stratified morbidity and mortality: A United Kingdom Multi-Center Comparative Analysis of Early Clinical Outcome. Circulation. 2003;108(Suppl 1):1–8. doi: 10.1161/01.cir.0000087440.59920.a1. [DOI] [PubMed] [Google Scholar]
- 9.Sohrabi F, Mispireta LA, Fiocco M, Dibos LA, Buescher PC, Sloane PJ. Effects of off-pump coronary artery bypass grafting on patient outcome. J Investig Med. 2003;51:27–31. doi: 10.2310/6650.2003.33529. [DOI] [PubMed] [Google Scholar]
- 10.Lilleberg J, Nieminen MS, Akkila J, Heikkilä L, Kuitunen A, Lehtonen L, et al. Effects of a new calcium sensitizer, levosimendan, on hemodynamics, coronary blood flow and myocardial substrate utilization early after coronary artery bypass grafting. Eur Heart J. 1998;19:660–8. doi: 10.1053/euhj.1997.0806. [DOI] [PubMed] [Google Scholar]
- 11.Slawsky MT, Colucci WS, Gottlieb SS, Greenberg BH, Haeusslein E, Hare J, et al. Acute hemodynamic and clinical effects of levosimendan in patients with severe heart failure. Study Investigators. Circulation. 2000;102:2222–7. doi: 10.1161/01.cir.102.18.2222. [DOI] [PubMed] [Google Scholar]
- 12.Mathison M, Edgerton JR, Horswell JL, Akin JJ, Mack MJ. Analysis of hemodynamic changes during beating heart surgical procedures. Ann Thorac Surg. 2000;70:1355–60. doi: 10.1016/s0003-4975(00)01590-3. [DOI] [PubMed] [Google Scholar]
- 13.Meyer K, Klocke RC, Schipke JD, Gams E, Korbmacher B. Ca 2+ sensitizer superior to catecholamine during myocardial stunning? Eur J Cardiothorac Surg. 2008;34:326–31. doi: 10.1016/j.ejcts.2008.04.042. [DOI] [PubMed] [Google Scholar]
- 14.Dernellis J, Panaretou M. Effects of levosimendan on restrictive left ventricular filling in sever heart failure: A combined hemodynamic and Doppler echocardiographic study. Chest. 2005;128:2633–9. doi: 10.1378/chest.128.4.2633. [DOI] [PubMed] [Google Scholar]
- 15.Follath F. Levosimendan in patients with low-output heart failure: Lessons from the LIDO trial. Ital Heart J. 2003;42:34–8S. [PubMed] [Google Scholar]
- 16.Tasouli A, Papadoupolos K, Antoniou T, Kriaras I, Stavridis G, Degiannis D, et al. Efficacy and safety of perioperative infusion of levosimendan in patient with compromised cardiac function undergoing open-heart surgery: Importance of early use. Eur J Cardiothoracic Surg. 2007;32:629–33. doi: 10.1016/j.ejcts.2007.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Husedzinović I, Barisin S, Bradić N, Barisin A, Sonicki Z, Milanović R. Levosimendan as a new strategy during off-pump coronary artery bypass grafting: Double-blind randomized placebo-controlled trial. Croat Med J. 2005;46:950–6. [PubMed] [Google Scholar]
- 18.Tritapepe L, De Santis V, Vitale D, Guarracino F, Pellegrini F, Pietropaoli P, et al. Levosimendan pretreatment improves outcomes in patients undergoing coronary artery bypass graft surgery. Br J Anaesth. 2009;102:198–204. doi: 10.1093/bja/aen367. [DOI] [PubMed] [Google Scholar]
- 19.Levin R, Degrange M, Del Mazo C, Tanus E, Porcile R. Preoperative levosimendan decreases mortality and the development of low cardiac output in high risk patients with severe left ventricular dysfunction undergoing coronary artery bypass grafting with cardiopulmonary bypass. Exp Cli Cardiol. 2012;17:1–6. [PMC free article] [PubMed] [Google Scholar]
- 20.Kowalczyk M, Banach M, Lip GY, Kozłowski D, Mikhailidis DP, Rysz J. Levosimendan — a calcium sensitising agent with potential anti-arrhythmic properties. Int J Clin Pract. 2010;64:1148–54. doi: 10.1111/j.1742-1241.2010.02396.x. [DOI] [PubMed] [Google Scholar]


