Abstract
Introduction
Congestive heart failure is a significant cause of morbidity and mortality in Australia. Accurate data for the Northern Territory and Indigenous Australians are not presently available. The economic burden of this chronic cardiovascular disease is felt by all funding bodies and it still remains unclear what impact current measures have on preventing the ongoing disease burden and how much of this filters down to more remote areas. Clear differentials also exist in rural areas including a larger Indigenous community, greater disease burden, differing aetiologies for heart failure as well as service and infrastructure discrepancies. It is becoming increasingly clear that urban solutions will not affect regional outcomes. To understand regional issues relevant to heart failure management, an understanding of the key performance indicators in that setting is critical.
Methods and analysis
The Northern Territory Heart Failure Initiative—Clinical Audit (NTHFI-CA) is a prospective registry of acute heart failure admissions over a 12-month period across the two main Northern Territory tertiary hospitals. The study collects information across six domains and five dimensions of healthcare. The study aims to set in place an evidenced and reproducible audit system for heart failure and inform the developing heart failure disease management programme. The findings, is believed, will assist the development of solutions to narrow the outcomes divide between remote and urban Australia and between Indigenous and Non-Indigenous Australians, in case they exist. A combination of descriptive statistics and mixed effects modelling will be used to analyse the data.
Ethics and dissemination
This study has been approved by respective ethics committees of both the admitting institutions. All participants will be provided a written informed consent which will be completed prior to enrolment in the study. The study results will be disseminated through local and international health conferences and peer reviewed manuscripts.
Keywords: Clinical audit < Health Services Administration & Management, Epidemiology
Introduction
The congestive heart failure (CHF) syndrome is the leading cause for admissions and is in the top three causes for mortality in the Western World. It is associated with significant morbidity, impacts on individual's quality of life and through the necessity of frequent medical and allied health interventions, prescription of pharmacological agents and recurrent hospitalisations, is a source of stress on health resources. Guidelines-based care improves outcomes but challenges exist in implementation. Neglecting this resource-intensive investment leads to poor outcomes and so the cycle perpetuates. CHF is speculated, as no accurate prospective data are available, to be higher in the Northern Territory (NT) and among Indigenous Australians. The recent Central Australian Secondary Prevention of Acute Coronary Syndromes (CASPA) study highlighted a significant burden of CHF, greater among the Indigenous communities,1 confirming earlier studies of under-representation nationally.2 These works have highlighted several key indicators relevant to the NT1–26:
There is a high burden of CHF that cannot be explained by traditional risk factors alone. Among the Indigenous population, given that social factors influence the risk of CHF, the excess in mortality is most likely to be multifactorial in origin, and have its foundations in the economic, social, physiological, psychological and educational disadvantages.1–3
There appears a greater burden of CHF related to rheumatic and non-ischaemic aetiology, which is reversible and has a better prognosis when treatment is delivered or preventive measures are enforced.2–5 14
There appears a greater burden of CHF with comorbidities among Indigenous clients, which requires greater resources to deliver comprehensive care.2 15
There are significant barriers and differentials in access to appropriate, acceptable and evidence-based medical care and preventative measures for Indigenous and remote clients. New delivery methods are important as CHF can largely be delivered as community-based care.13–25
There is significant delay in presentation and receipt of acute care during periods of decompensation, and for geographical and other reasons delay of definitive therapies or procedures.
There is poor uptake of postdischarge services such as cardiac rehabilitation, and at present, unknown demographics will assist implementation of remote allied health or technological-based solutions.3 14
Unique geography—the NT consists of a vast area with two major public hospitals in Alice Springs and Darwin servicing 230 000 clients; approximately 70% of people live within the urban proximity. Specialist services reside at the tertiary hospitals with satellite district hospitals in several smaller townships supporting a small number of visiting specialists. Service planning must take this into account.3 14
External validity—adherence to guidelines early in hospital admission can improve outcomes; however, not all groups meet trial conditions in remote areas nor are trial conditions for dosing strategies reproducible.15 27 28 A consensus on therapeutics strategies is needed.
Lack of accurate prospective data for the listed points makes it difficult to accurately develop a tailored, yet comprehensive heart failure (HF) programme. Developing tools to gather evidence require adhering to standards for validity and reproducibility, which are also lacking. This study is focused on understanding the current evidence base for quantifying healthcare systems and informing the design of diagnostic and management clinical audits that would form the backbone for the direction of CHF disease management systems within an NT context. We thus propose to study the quality and outcomes of care for patients admitted with acute decompensated heart failure (ADHF). We aim to develop key clinical and process of care performance indicators (key performance indicators, KPI) and translate these findings for improved service delivery if and where deficiencies are highlighted. This paper describes the rationale for the Northern Territory Heart Failure Initiative—Clinical Audit (NTHFI-CA) design.
Methods
Aims and scientific hypotheses
The NTHFI-CA survey was designed with four major objectives: first, to develop validated and reproducible KPI for the comprehensive measurement of quality of care and outcomes for clients admitted with ADHF. In this, we aim to measure for the clients, the proportion meeting standardised clinical outcomes, process outcomes and defined targets of secondary prevention and compare by age, ethnicity, sex and place of usual residence. For the health system, identify failures of the health care system in relation to timely acute care and to the provision of secondary CHF care, particularly for Indigenous and remote clients; second, to develop a system of data collection and reporting, that can be used for ongoing quality assessment and improvement across the care continuum; third, the results of the first two objectives, are believed, will help tailor a pilot intervention study similar to the ongoing nurse-led intervention developed around the CASPA-acute coronary syndrome (ACS) study findings; fourth, to accumulate sufficient epidemiology and implementation-focused information to steer future action in the provision, monitoring and development of guidelines-based quality CHF care for rural, urban, Indigenous and Non-Indigenous clients. We hypothesise that patients presenting with ADHF are expected to have: a disproportionate representation of Indigenous clients with advanced systolic impairment; excess of alcohol, ischaemic or rheumatic aetiology; greater comorbidities in diabetes, hypertension, lipid abnormalities and/or renal insufficiency, and with other non-cardiac comorbidities; delayed presentations for Indigenous and remote clients; we hypothesise that treatment for Indigenous and remote clients: are likely suboptimal for the stage of HF; have fewer clinical interventions and support compared with their urban counterparts; are less likely to receive novel therapeutic options or enrolled in multicentre trials; and are more likely to have their HF managed without regular cardiology specialist input.
Projected outcomes
We anticipate several outcomes from this work: first, identification of the points of weaknesses in the hospital and community health centre systems that impact on urban, rural, Indigenous and Non-Indigenous clients and hopefully lead to the development of focused service improvement models across this care continuum; second, to link with a number of collaborative research projects assessing barriers to care for Indigenous clients suffering with heart diseases; third, lead to the development of ongoing and sustainable quality improvement practices and monitoring within hospital and primary healthcare (PHC) services across the region; fourth, help develop, trial and implement standardised medical discharge summaries and care plans during hospital stay and following discharge; fifth, explore the potential contribution of poor systems of care to the high level of illness faced by Indigenous people; and finally, assessment of the potential barriers that may exist for primary and secondary prevention for CHF. These goals should initially drive improved service delivery and subsequently provide a baseline for evaluating ongoing service outcomes on which to base future acute and preventive programme development and inform the development of alternative models of secondary prevention for NT clients with CHF.
Protocol
The project comprises two specific stages. Stage 1 is the collaborative development of suitable KPI covering process and outcome measures across the continuum of care; and stage 2, involves two phases, is the development of appropriate, feasible data collection tools and their subsequent measurement in hospital and PHC settings.
Development of appropriate clinical indicators (stage 1)
We conducted an extensive literature review with key words “heart failure or acute heart failure or chronic heart failure or CHF”; “database or study design or study rationale or registry” and “Data Collection/or Quality Indicators, Health Care/ or Management Audit/ or performance indicators.mp or Healthcare Disparities/Quality Assurance, Health Care/or Quality of Health Care/or Quality Indicators, Health Care/or quality of care indicators.mp or ‘Outcome and Process Assessment (Health Care)’/or process of care.mp”. Published and established existing KPI for measuring the quality and outcomes of care for patients experiencing ADHF were collated6–12 29–40 The CASPA study KPI was used as a template. Within six domains and five dimensions of care, KPI were added or rested on this template using the American College of Cardiology and the American Heart Association (ACC/AHA) attributes of performance measures.31 Addition or removal required consensus of the principal investigator and one co-investigator. Uniform agreement by all co-investigators was required for accepting the final measures (figures 1 and 2). ACS (as an aetiology for ischaemic cardiomyopathies or aggravator of existing cardiomyopathies) and KPI that were deemed not to add any additional benefit on what was already known from CASPA were also rested.
Figure 1.
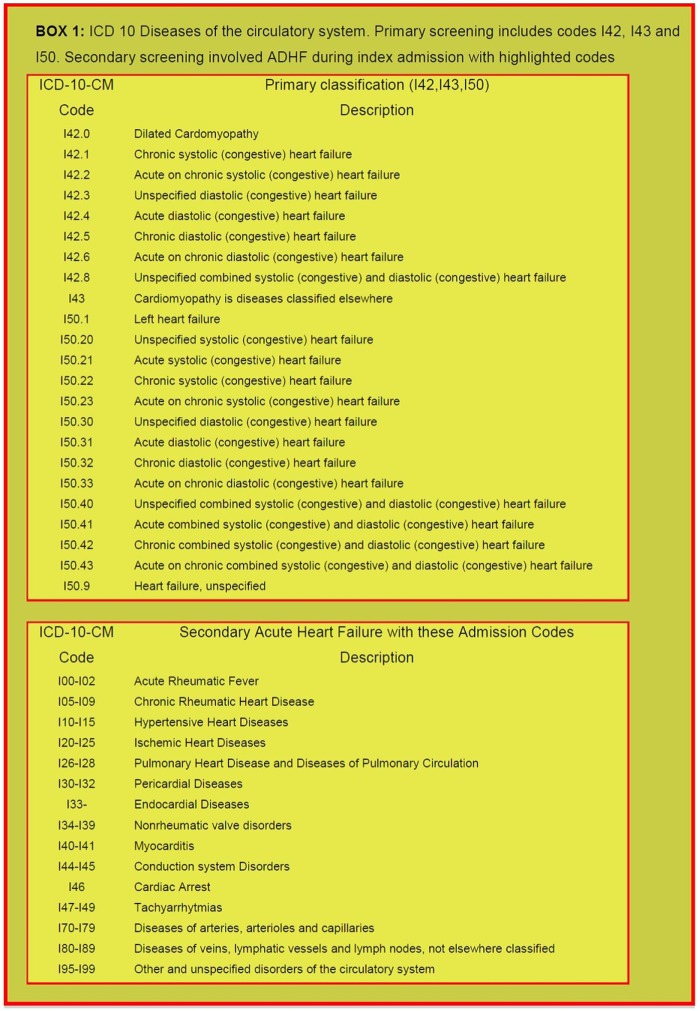
International Classification of Diseases (ICD)-10 of the circulatory system. Primary screening includes codes I42, I43 and I50. Secondary screening involved acute decompensated heart failure during index admission with highlighted codes.
Figure 2.
Design of the NTHFI-CA involved four steps: (A) using a set of standardised principles (blue box) and their attributes (green box) we formulated outlines for each performance attribute (final column). CASPA shaped many aspects of design and implementation attributes; (B) four basic factors shaped the broad study outline; (C) highlights the ethical considerations for studies in the NT; (D) broad disease management goals for which performance measures hope to inform.30–33 CASPA, Central Australian Secondary Prevention of Acute Coronary Syndromes; NT, Northern Territory; NTHFI-CA, Northern Territory Heart Failure Initiative–Clinical Audit.
Study design and registry (stage 2)
The NTHFI-CA registry is a prospective observational cohort study designed to examine the performance of health systems in relation to the acute management and secondary prevention of ADHF in patients admitted to two teaching hospitals in the NT, Royal Darwin Hospital (RDH) and Alice Springs Hospital (ASH) starting September 2013 and followed for 12 months ending September 2015. Performance will be measured against currently available evidence-based guidelines for the treatment and secondary prevention of CHF4 6–11.29–38 Data collected will be entered in the NTHFI-CA study registry located at NT Cardiac Services/Menzies School of Health Research, Darwin. All documentation relating to study participants will be treated in accordance with National Statement of Ethical Conduct in Human Research.41
Eligibility criteria
Patients admitted to either hospital with the diagnosis of HF (International Classification of Diseases (ICD)-10CM I42.0–I42.8, 143.0, 150.0–150.9) will be eligible for the prospective case note audit. The participants will also be drawn from inpatients who develop acute symptoms while in hospital for other reasons. Further assessment will also involve the generation of lists ICD CM I00–I02, I05–I09, I10–I15, I20–I28, I30–I41, I44–I49, I70–I89 and I95–I99 (complicated with acute heart failure) for cross-checking of initial coding and recording of outcome variables. Participants will be considered eligible if the review of medical records demonstrates that they, in fact, have suffered an ADHF based on ACC/AHA and National Health Data Dictionary standardised definitions.
Exclusion criteria
Patients will be excluded if they die within 24 h of admission or do not usually reside within either region or whom no follow-up data can be obtained; however, these clients will still provide baseline incidence data. Cases that do not fulfil the case definition of ADHF on review of the notes will also be excluded, and recorded but will not form baseline data.
Population/recruitment of subjects
A dedicated research assistant will recruit consecutive patients who present acutely to either hospital or transferred from remote Indigenous communities from the emergency clinical screen and medical admission lists for. Of these, clients who are Aboriginal, or non-Aboriginal, have a documented urban residence and reside in remote communities will be followed. The participants will also be drawn from inpatients who develop acute symptoms while in hospital for other reasons. Flyers will be posted in emergency, wards, intensive care and a brief presentation will be made to the medical and nursing staff at relevant units. Referrals from hospital staff in this form will be a secondary recruitment strategy. For retrospective audit, lists of individuals will be generated through hospital separation and CCU admissions data for the years 2011 and 2012. The approved research assistant in each site will perform this. An independent physician will review uncertain cases.
Data collection and storage
Data will be collected on a standardised case note extraction form developed during phase I of the project. Information will be accessed through multiple sources including hospital records, PHC clinic records, specialist databases and record systems maintained by visiting district medical officers. The period of interest for data collection will be 0–12 months after discharge following documented ADHF. Data definitions will be standardised and widely accepted case and outcome definitions as outlined in the ACC Clinical Data Standards.9–11 31–37 All cases that demonstrate ambiguity in data definitions or outcome data will initially be discussed with site investigator; if ambiguity persists, the principal investigator and a locally convened panel of the research team will review, and consensus sought.
Measurement of performance
Phase I involves prospectively auditing admitted clients hospital records. Phase II involves further assessment of performance and will involve the auditing of client records held at remote community health centres, urban PHC centres, specialists’ records, hospital records and outpatient and cardiac rehabilitation files. Files are coded and stored by three health providers, NT Department of Health and Community Services (DHCS—ASH/RDH), PHC records and NT Cardiac Services Pty Ltd. NT DHCS hospital separation data, hospital records coding and storage of data follow a nationwide format. PHC records will also be accessed to complete the secondary prevention and follow-up components of the audit and is subject to variability. NT Cardiac, main provider of cardiac diagnostics and outpatient care, databases and coronary intervention information systems holds a range of clinical and cardiac investigation/intervention (angiography, coronary stenting, echocardiography, stress testing) information. This information will be used to complete the data collection sheet for each patient file. Denominator and numerator values for KPI will be based on standardised values from ACC/AHA guidelines, local laboratory specification for biochemical tests and Australian accrediting bodies for invasive and non-invasive investigations. Overall performance will be compared with the National benchmark for CHF outcomes. As this is subject to change, the broad principals will include CSANZ, Heart Foundation and locally published studies that involve a public tertiary HF referral centre from any of the six states in Australia. We will also seek the opinion of several local leading HF clinicians should there be issues standardising these benchmarks.
Participant follow-up
Clients will be followed up to determine subsequent hospitalisation, major medical events and interventions. Similar ICD codes for acute CHF will be used for screening information at 1, 6 and 12 months. Data extraction will include a combination of case notes review, medical databases and contact with PHC and clients directly. Consent for this will be obtained during the initial recruitment.
End points
The main indicators we are measuring cover a range of domains across the spectrum of care for people with ADHF. In brief variables include
- Baseline
- Demographics: age, sex, usual place of residence, ethnicity;
- Background: medical history of CHF and treatments, known risk factors and comorbidities;
- Symptom onset: time, nature, location, first point of contact with PHC, delay times to care.
Prehospital management: appropriate medical/paramedical assessment, provision of prehospital nitrates, diuretics, ventilation and analgesia
Emergency department: presentation, delas, biochemistry, investigations (chest X-ray, ECG, echocardiography), therapeutics (assisted ventilation, intravenous nitrates or diuretics); risk stratification.
Admission details: clinical examination, investigations, management, complications during admission, performance of phase I rehabilitation.
Discharge: discharge diagnosis, discharge status, medication regime, referral to phase II cardiac rehabilitation, discharge planning and referral to PHC provider.
- Outpatients
- Cardiac rehabilitation: attendance and completion of cardiac rehabilitation.
- Secondary prevention: risk factor modification, care plan, cardiac education received, measurement of and achievements of specified target goals for HF and prevention of risk factors related to aetiology (eg, cardiovascular disease, ie, smoking cessation, lipid control, blood pressure control), complications.
- Self-management.
- Depression—PHQ9.
- Outcomes: readmission, major cardiovascular and non-cardiovascular events, mortality.
- IT and telecommunications: availability, access and type of mobile phone and Internet platforms.
Special Ethical Consideration and Adverse Events: cultural and religious issues surrounding confidentiality and storage of human tissue are of significant importance for Indigenous clients. The NT is also host to a diverse multiethnic population. We have thus chosen not to store samples for future use. We have sought specific support from key Indigenous Community groups, NT-DHCS, Cardiac Services, Remote and Primary Health Services, Independent Health Services and Indigenous Health Services, in advance. As primarily a hospital and clinic file audit, this proposal does not directly broach the issues of reciprocity, respect, equality, responsibility, survival and protection, which are critical in Indigenous research, confirmation of which was obtained through the ethics submission. We do not anticipate any other adverse events. We have received full ethics approval to conduct the study by Central Australia and Top End Human Research Committees.
Training and standardisation
This project requires access to data housed and maintained by NT DHCS and NT Cardiac Services. Hospital Separation Data, Hospital Records and PHC Records will be sought from NT DHCS and will be arranged through PI's in Darwin. In the event that PHC records are housed within independent services (non-DHCS clinics), appropriate consultation will be undertaken as requested by the independent services themselves. Formalised consent processes as directed by independent services will be followed. If they wish to perform the audit themselves, as a training and quality assurance process, appropriate training and support will be provided by the research team. All staff recording information will be briefed by training staff from the CASPA study and undergo education in variability or data recording, ambiguous data and differing case records, ICD-10 classification, ACC/AHA guidelines for KPI31 and NHMRC good clinical practice as the minimum requirement. Addressing ambiguity has been discussed under data collection and storage.
Expected sample size
On the basis of generated hospital separation and CCU statistics, 2009, for ASH of 113 and RDH of 450 patients, the sample population will be approximately 150 patients with ADHF at ASH and 500 matched at RDH in the time period 2009. Of the ASH separations, 99 (88%) are identified as being indigenous. The matched (ethnicity and gender) RDH sample extrapolates to 180 (40%), Aboriginal clients in phase II. As data will be collected on three separate occasions for each patient, a robust dataset is expected to identify any significant associations between predictors and patient outcomes. Findings from this investigation will also inform the development of more testable hypotheses in future studies and appropriate sample sizes.
Statistical considerations
All generated data will be entered into and analysed with SPSS V.11.5. Initial data analysis will be conducted to assess for data quality including allowable ranges, data structure and errors. Descriptive statistics for baseline participant characteristics, diagnostics and therapeutics within highlighted domains will be calculated and presented as means (SD), IQR for continuous data and count (per cent) for categorical data. Univariate between group analyses will be performed using t tests for continuous variables, and χ2 tests of association for categorical variables. For study outcome measures, a type 1 error rate of α=0.05 will be used to test for statistical significance. A generalised mixed-effects model approach will be used in the analysis of repeated measures for continuous and categorical outcomes. Mixed-effects models take into account the interindividual differences in intraindividual change with repeated responses and use all the available data on each participant. Mixed models are also unaffected by randomly missing data and therefore do not require imputation methods.42 The model-building strategy will include fitting nested models by sequentially adding blocks of predictor variables: sociodemographics, comorbid disorders and factors related to health service interventions. Interaction terms that are considered to be potentially important from a clinical perspective will be tested and remain in final models if significant. Predicted estimates of outcomes at each time point will be calculated using fitted models of the data in order to examine patterns of individual change. To interpret effect sizes and precision for categorical outcomes, ORs and CIs will be calculated.
Discussion
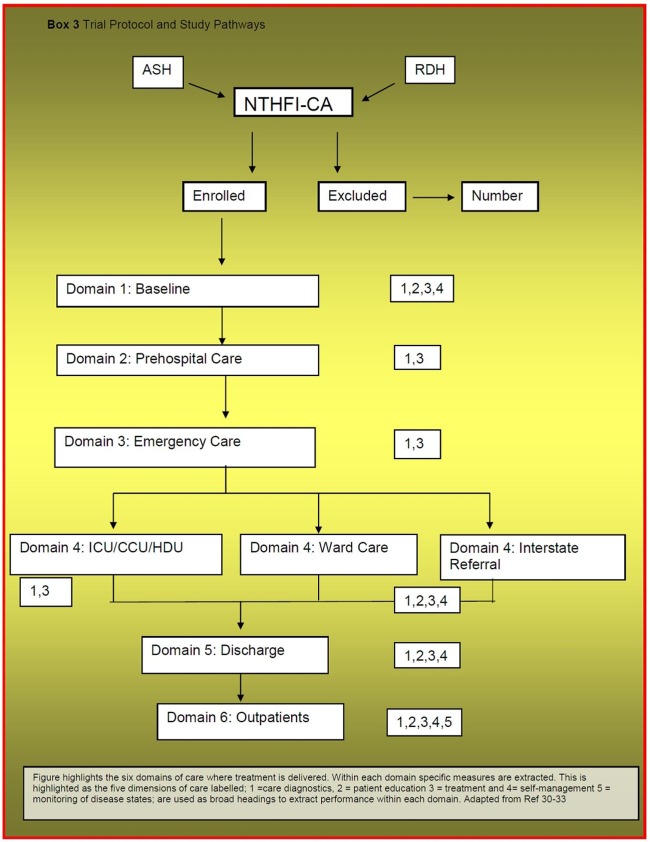
The NTHFI-CA represents one of a few opportunities offered for longitudinal studies designed to extract data that inform service development. Information gathered has to be relevant for current and future needs. It is difficult to determine service factors beyond five yearly intervals. To compensate for this, there have been measures taken to set infrastructure and standardise protocols to facilitate episodic updates in information as well as ensuring reproducibility of study design and implementation. With the actual study design, a series of steps were taken. The first step was establishing basic principles for defining the disease (figure 1, see online supplementary appendix A). The second step involved standardising principles for attributes in KPI, that is, care dimensions (figure 2A, see online supplementary appendices B and C) and the study care domains to be tested, in this case six (figure 2B). The third step involved addressing the broad NT health goals and research conducted in Indigenous population to steer implementation within five key priorities (figure 2C). The fourth step is design of disease management systems in the NT context from the available evidence (figure 2D, see online supplementary appendix D). The resultant study pathway is highlighted in Figure 3. The specific study in greater detail are explored.
Figure 3.
Trial protocol and study pathways.
The ACC/AHA has released several position statements to standardise the process of developing, assessing, implementing performance measures and disease management systems.30–33 From this consensus-driven platform, we identified the target disease, population and explored standardised measures that inform the observation for the required time period. The NTHFI-CA is defined for all stages and causes of CHF, for NT resident population who receive care within six domains of treatment. This broad definition partly relates to uncertainties on actual CHF demographics, and as the yearly admission is unlikely to exceed 500, will not lead to significant difficulties in enrolment. To determine the performance measures, we again explored the position statement. The authors rated 27 potential measures on 13 dimensions using a five-point Likert scales.31 If a KPI received full committee support with a score of at least 3, it was advanced. The process concluded with 7 inpatients’ and 12 outpatients’ measures. These KPI informed five dimensions of care encompassing: diagnostics, patient education (including prognosis and aetiology), treatment, and self-management (for inpatient and outpatient) and monitoring of disease status (for outpatients only).31 This statement did not, however, focus on outcomes as the design was shaped to assist physicians improve care. We have included outcomes, as this is the strongest indicator of funding for vulnerable groups beyond the conventional block funding models. To determine the final KPI, several additional points were considered.
Existing studies: Several recent databases stand as landmark achievements in HF epidemiology and have confirmed clinical understanding of evidence base and positive outcomes.9–11 35 37 43 Interestingly Krumholz et al30 pointed out a disparity between what is conventionally accepted evidence and its generalisabilty. This is particularly so for the NT where there are significant non-traditional factors that impact on the delivery of evidence-based care and affect outcomes. While it would be unreasonable to propose reconducting large CHF studies to incorporate an increasingly diverse group of patients, we have come to realise that the heart of these matters is to develop an intrinsic understanding of the underlying regional demographic differences and service delivery dynamics to be able to formulate informed decisions in implementing the necessary measures, be they simple or more complex. Developing the necessary KPI in these settings is a challenge as there is a divide between perceived optimal care and realistic and deliverable care that, in fact, is optimal for the region. From this, it was evident that some measures needed to be rested (eg, treatment optimisation) and others added (eg, the dimension of technology).
NT experience: The CASPA study was groundbreaking in the sense that it allowed for the first-time exploration of ACS/cardiovascular KPI in Central Australia. The list was formulated from an extensive search of available national and international clinical guidelines, national health priority area indicators and reports and with reference to National Health Performance Committee guidelines and further augmented by performance measures used in published quality improvement projects. Three priorities—process of care, target achievement and outcome indicators for the treatment and prevention were generated. This list underwent scrutiny by 60 key stakeholders, key external content experts and the research team through mailed questionnaires and a workshop convened in Alice Springs. Each stakeholder was asked to grade each potential indicator according to a number of criteria: strength of evidence; feasibility of measurement; plausibility of effects from quality improvement; impact on outcomes and an assessment of the overall utility of the measure. Results were collated and analysed for each indicator (overall grading) and for each of the five criteria across each indicator. Indicators that were graded as high priority, frequently recorded, very plausible and will have a large impact or better were included in the final list (average score on grading scale ≥4). Indicators that demonstrate an across criteria grade of less than 4, but was assessed by key stakeholders as a high or essential priority within the overall (utility) rating, were scrutinised by the project team and included as decided by consensus. Data specifications were then developed according to internationally standardised definitions. Subsequent data collection tools were developed and piloted in a number of hospital and PHC records (n=20) and implemented. The spill-over knowledge assisted greatly in the NTHFI-CA design.
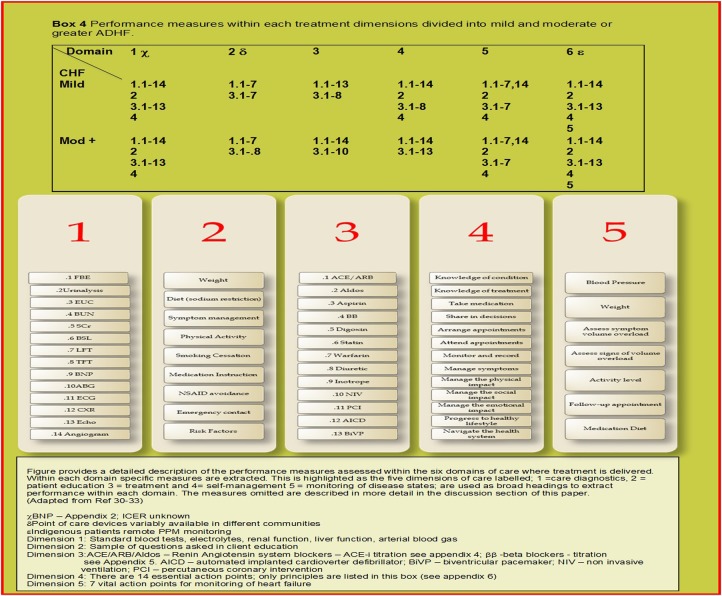
Combining this local and international experience, with the standardised ACC position,31 a conceptual framework KPI reflecting six critical domains for treatment delivery and five principal dimensions of care evolved (figure 3). All these well-established performance measures were individually scrutinised and included or rested. Level of evidence was the predominant scrutinising theme in the second phase. The less validated ‘local knowledge’ and NT health priorities were additional considerations. Study investigators made the decisions on these. Several less well-established indicators were included through recent understanding and development of self-management and IT-based solutions.14 In direct contrast to intervention-themed databases,34 35 focus on specifics in the treatment dimension was given a lower priority (see online supplementary appendices E and F). Figure 4 describes this in greater detail.
Figure 4.
Performance measures within each treatment dimensions divided into mild and moderate or greater acute decompensated heart failure.
Further rationale for specific KPI inclusion or exclusion are as follows: Domain 1: demographics are at the heart of this study. Validated KPI derived from CASPA were used to extract race, culture, language and support networks; further expansion was made in the dimension of HF aetiology with emphasis on ischaemic, hypertensive as well as rheumatic and alcohol-induced causes. Data on tertiary referral centres were collected, as there were two main cardiac surgical referral hospitals. Decision referral patterns vary with the treating physician practices as well as waiting list and urgency. It is established that decisions on percutaneous or surgical revascularisation and valvular restoration or replacement differ at these sites on physician, group consensus and expertise at the respective sites. Details on primary care physician, pharmacy, residence and principal next of kin were deemed important as local and ethnicity were deemed factors in service uptake and delivery. Furthermore, access to primary care could determine: admission, re-admission burden and early measures to prevent deterioration; Domain 2–5: a comprehensive medical history of all systems were included to establish the overall need for chronic medical service needs and factors preventing use or uptake of HF pharmacology, cardiac rehabilitation or referral for invasive management. Biochemistry details were included to establish pattern of establishing HF aetiology and outpatient risk for adverse events. Methods for estimating epidermal growth factor receptor was obtained as much recent work raises validity of estimated measures with illness and demographics, which subsequently alter prescribing practices and outcomes.11 12 44 KPI for depression were expanded, as a high burden was noted in CASPA, this also being a significant factor in many dimensions of self-care and compliance. In hospital, discharge and outpatient indicators were designed to reflect the potential blocks to maximising proven pharmacological prescription and access to cardiac rehabilitation; at the core of these were reasons for non-prescription or subtherapeutic prescription. The actual specifics on medication titration across all domains were rested. It is noted that care and resources are needed to titrate many variables in CHF care, for example, ββ and ACE-I (see online supplementary appendix E, F). This information can be extrapolated from frequency of contact with medical practitioner and central pharmacy prescription slips. Appropriate early therapeutics—to prevent further heart muscle damage, good symptom relief and minimising iatrogenic adverse effects such as renal dysfunction and electrolyte derangements are within the control of the health systems and builds client confidence, and are considered vital. Domain 6: overall, we felt, in the community, that the greatest value in the performance measures related to two critical aspects—impacts on the overall health system (strain and morale) and contributors to poor outcomes (client and non-client). Post hospital access to services and blocks to referrals (non-client) and self-management (client) are factors related to efficiency, planning and client education. Investment in these dimensions would not increase strain on resources, with potential benefit.
Data collection instrument was via Case Report Forms (CRF) designed for a combination of retrospective and prospective audit from combination of several studies such as CASPA and WHICH. The Baker IDI, Flinders University and SAHMRI have extensive track record in electronic CRF. This was greatly beneficial and reduced challenges faced at stage 2. At present, a considerable research work is conducted through the Menzies School of Health Research. As part of this initiative, we have begun the process of developing dedicated office to conduct studies across the cardiac and renal axis. Part of this also involved staff training in good clinical practice and transfer of knowledge from partners to stand as an independent entity.i
Indigenous health in the NT requires a special focus. Australia has seen the first Indigenous premier in 2013 and a measured but controversial statement of removing the Indigenous ministerial portfolio was “there are numerous ministers for many areas and one for all Indigenous affairs”. Current sentiments that move away from race-based programmes are encouraged but with caution. We clarify that out approach does not target any specific communities but is based on needs. It is unfortunate that disadvantaged communities are also marginalised in large studies partly for language, cultural and perceived compliance issues. In this case, the Indigenous community represents a significant group in Australian society who have despairingly worse outcomes. The desire to preserve one’s traditional culture in an ever-modernising world poses huge challenges for these communities and health systems. Poor understanding could lead to stereotyping that could brand some behaviour as recalcitrant, adding to the vicious circle. Respecting these beliefs and tailoring care in lieu of these factors, we were able to advance the CASPA study. This was carried out through acknowledgement of several sensitive areas in the ethics application; Equality—the overarching aims of the research project is based within a framework driven by questions of equality in the provision of healthcare across the continuum for all patients regardless of ethnicity, gender or age, and one based on need as demonstrated by clinical determinants; Survival and Protection—we also recognise that chronic disease research and epidemiology has tended to contribute to deficit approaches to individual pathology, that is, disease is due to bad behaviour. Less focus has been afforded the potential successes and failures in health systems, as contributors to differential outcomes for populations based on ethnicity; Respect—we feel that information generated within this project and the processes developed have the potential to contribute to community-directed health service redevelopment and quality improvement activities; Reciprocity—we feel that this work may identify failures in health systems and therefore identify obligations that are being unmet by systems themselves; Responsibility—reframing the gaze of health inequality, from individual-focused deficits to system failures stands as the key principle on which this extensive work is based, and is a direct effort at ensuring that exploring health inequalities does not undermine and harm Indigenous individuals and communities. These principles may play great importance to future research practices in these areas.
Interim analysis will be conducted at the 6-month mark. It is anticipated at this point lessons learnt and spill-over knowledge from the ongoing CASPA-ACS intervention study may direct minor modifications to the existing CRF. One such area is increasing the KPI in domains 1, 2 and 6 to better understand the barriers to accessing primary care. CHF, an ambulatory case-sensitive condition, can largely be managed in the community with the application of appropriate and timely preventive care and early disease management. The issues that remain unclear at this point are the adequacy and the barriers for accessing such care in each of the remote communities. Of interest, Ansari et al noted that a lack of timely and effective care had an impact on admission rates in rural Victoria particularly among lower socio-economic groups.45 46 A similar understanding in the NT could impact on how we allocate resources in the future.
Measuring performance is not an end in its own right and clinical indicators and their measurement alone are not sufficient to change behaviour in service provision and quality improvement. They must be supplemented with key educational activities (eg, provision of continuous and sustained feedback of results to all levels of service provision), processes to sustain continuous monitoring and assessment and to inform policy development on a local and regional level. Clearly defined dissemination processes and involvement of Aboriginal Health Workers, hospital-based and community-based nurses, allied health professionals and clinicians are essential if practice is to change. Engaging non-governmental (NGO) service providers, data coders, quality improvement staff, NGOs (NHF NT Division, Healthy Living NT), Division of General Practice/PHC and consumer representatives in the development phase of the project so as to ensure alignment between proposed indicators and local needs. The dissemination of key findings through key advisory/research institutions will also increase the awareness nationally/globally and build foundations for future competitive research funding. Finally, we have also been in negotiations for the broader applicability of the findings of and tools utilised within this project with the Australian Collaborative Project (which seeks to measure PHC performance). This stands as a critical method of project outcome dissemination.
Limitations
Conducting clinical studies in the NT is in itself a limitation: first, the realisation of non-traditional risk factors, which impact on management; second, as there are few benchmarks as comparators and; finally, shortfalls in research funding and infrastructure. While no system has the perfect mix of resource input to match service needs to answer this question, for this region, there will be components within many aspects of the study, that is, hypothesis generating, compared with the mainstream. Nonetheless, following the accepted consensus and providing enough information to allow reproducibility are accepted as a positive means for overcoming this limitation. Examples of this were resting KPI that collate in-depth information on medication dosing as per RCTs and large HF databases.30–38 This study will not address whether clinical trial prescribing practices are achieved; instead, we are keen to determine whether there is a system in place to facilitate this, which will be answered. The infrastructure is also in place for the next step to determine whether this can occur. We note that RCT level outcomes relate to achieving prescribing practices in the trials. As examples, online supplementary appendix E/F highlight differences in two medications. As noted, ββ titration is ideally carried out at two weekly intervals and may not need biochemistry, while ACE-I can be carried out at 3–7-day intervals and usually requires assessment of basic biochemistry.ii Addition of aldosterone blockers and other agents are further complexities.ii We are hopeful that relevant information on this will help steer the next phase, an intervention clinical study. This study relied on lessons from ACS study conducted greater than 5 years ago. Unanticipated changes that cannot be standardised could act as confounders, which will only be revealed in time; for example, is potential drop off rate during follow-up. In the standardisation of design—we did not use five-point Likert scale, as the number of NT consultants was only 4. In addition the CHF task force position was comprehensive.31 Finally, clinical practice guidelines are well established, as Krumholtz stated “guidelines are written in a spirit of suggesting diagnostic or therapeutic interventions for patients in most circumstances. Accordingly, significant judgment by clinicians is required to adapt these guidelines to the care of individual patients to ensure accountability in these judgments an evidenced based process is important”. The standardising of clinical judgement and interpretation of guidelines remains contentious and may be more noticeable with fewer cardiologists. As such we intentionally left the criteria for KPI reference broad. This will be narrowed, as lessons are learnt and early data are analysed. This should aid more focused and detailed assessments in the future.
Conclusion
Achieving optimal care in the remote setting is no different from urban settings. The ability to provide a continuum of care from presentation to post discharge requires activation of proven KPI at each level of care. The significant differences in remote care revolve around the interaction of service infrastructure, personnel, disease burden and cultural sensitivities. As such the outcomes limiting factors are variable and require exploration. The potential gains of these findings in implementing early and later secondary prevention of CHF and its sequelae are undisputed. In addition, little information exists on the provision and outcomes for CHF initiatives for Indigenous populations, which are a significant client base in the remote setting. Even less is known about the postdischarge care. The extent to which care is suboptimal and the acute and long-term HF management among Aboriginal clients could be contributing to the large and growing cardiovascular mortality differentials seen between Aboriginal and non-Aboriginal clients. Thus, the development of meaningful, sustainable public health, clinical and continuous quality improvement policy in the provision of CHF care in the NT requires urgent attention, and must be used to drive the development of better service delivery at the individual and health system levels. It is anticipated that this work will highlight key areas of disparity and inform the implementation of an intervention study.
Supplementary Material
Footnotes
Contributors: All the authors are involved in (1) substantial contributions to conception and design, acquisition of the data, or analysis and interpretation of the data; (2) drafting the article or revising it critically for important intellectual content and (3) final approval of the version to be published.
Competing interests: None.
Funding: All authors have won independent and governmental research funding. PI is supported by the Royal Australasian College of Physicians Fellows Contribution Award.
Ethics approval: TEHREC and CAHREC.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The current data will belong to the NT Cardiology Department. The data will be shared with our partners in FHBHRU, Baker IDI and SAHMRI.
Information on our partners and expertise can be found on the web or via corresponding author.
We have not provided treatment pathways for AICD/CRT/ other pharmacotherapies. These are available from several optimising databases (34, 35, 37).
References
- 1.Brown A. Acute coronary syndromes in Indigenous Australians: opportunities for improving outcomes across the continuum of care. Heart Lung Circ 2010;19:325–36 [DOI] [PubMed] [Google Scholar]
- 2.Woods JA, Katzenellenbogen JM, Davidson PM, et al. Heart failure among Indigenous Australians: a systematic review. BMC Cardiovasc Dis 2012;12:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Health and Human Services, Department of Health NT. KPMG. Development of the Northern Territory Specialist Cardiac Services Plan 2011–2020: final report. KPMG April 2011.
- 4.Expenditures on Health Services for Aboriginal and Torres Strait Islander People Australian Institute of Health and Welfare. 1998–2013 Cat No. HWE 6–57. http://www.aihw.gov.au/publication-detail/?id=60129542787
- 5.Ansari MZ, Henderson T, Ackland M, et al. Congestive cardiac failure: urban and rural perspectives in Victoria. Aust J Rural Health 2003;11:266–70 [DOI] [PubMed] [Google Scholar]
- 6.Krum H, Jelinek MV, Stewart S, et al. Guidelines for the prevention, detection and management of people with chronic heart failure in Australia. Med J Aust 2011;194:405–9 [DOI] [PubMed] [Google Scholar]
- 7.Schoken DD, Benjamin EJ, Fonarrow GC, et al. Prevention of heart failure: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation 2008;117:2544–65 [DOI] [PubMed] [Google Scholar]
- 8.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur Heart J 2008;29:2388–442 [DOI] [PubMed] [Google Scholar]
- 9.Cleland JG, Swedberg K, Follath F, et al. ; Study Group on Diagnosis of the Working Group on Heart Failure of the European Society of Cardiology The European Heart Failure survey program—a survey on the quality of care among patients with heart failure in Europe. Eur Heart J 2003;24:442–63 [DOI] [PubMed] [Google Scholar]
- 10.Fonarow GC, Abraham WT, Albert NM, et al. ; OPTIMIZE-HF Investigators and Hospitals Influence of a performance-improvement initiative on quality of care for hospitalized patients with heart failure: results of the organized program to initiate lifesaving treatment in hospitalized patients heart failure (OPTIMIZE-HF). Arch Intern Med 2007;167:1493–502 [DOI] [PubMed] [Google Scholar]
- 11.Heywood JT, Fonarow GC, Costanzo MR, et al. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. J Cardiac Fail 2007;13:422–30 [DOI] [PubMed] [Google Scholar]
- 12.Ezekowitz J, McAlister FA, Humphries KH, et al. for the APPRAOCH Investigators The association among renal insufficiency, pharmacotherapy, and outcomes in 6247 patients with heart failure and coronary artery disease. J Am Coll Cardiol 2004;44:1587–92 [DOI] [PubMed] [Google Scholar]
- 13.Iyngkaran P, Majoni V, Haste M, et al. Australian Indigenous Chronic Disease Optimization Study (AUSI-CDS) Prospective observational cohort study to determine if an established chronic disease health care model can be used to deliver better heart failure care among Remote Indigenous Australians: Proof of concept. Study Rationale and Protocol. Heart Lung Circ 2013;22:930–9 [DOI] [PubMed] [Google Scholar]
- 14.Iyngkaran P, Harris M, Nadarajan K, et al. Implementing guideline based heart failure care in the Northern territory: challenges and solutions. Heart Lung Circ 2014; in press. [DOI] [PubMed] [Google Scholar]
- 15.Iyngkaran P, Thomas M, Sanders P, et al. Do we need a wider therapeutic paradigm for heart failure with comorbidities?—a remote Australian perspective. Health Care Curr Rev 2013;1:106 [Google Scholar]
- 16.White H, Walsh W, Brown A, et al. Rheumatic heart disease in Indigenous populations. Heart Lung Circ 2010;192:273–81 [DOI] [PubMed] [Google Scholar]
- 17.Clark RA, Eckert KA, Stewart S, et al. Rural and urban differentials in primary care management of chronic heart failure: new data from the CASE study. MJA 2007;186:441–5 [DOI] [PubMed] [Google Scholar]
- 18.Thomas DP, Heller RF, Hunter JM. Clinical consultations in an aboriginal community controlled health service: a comparison with general practice. Aust NZ J Public Health 1998;22:86–91 [DOI] [PubMed] [Google Scholar]
- 19.Clark RA, Driscoll A, Nottage J, et al. Inequitable provision of optimal services for patients with chronic heart failure: a national geo-maping study. MJA 2007;186:169–73 [DOI] [PubMed] [Google Scholar]
- 20.Phillips SM, Marton RL, Tofler GH. Barriers to diagnosing and managing heart failure in primary care. MJA 2004;191:78–81 [DOI] [PubMed] [Google Scholar]
- 21.Clark RA, McLennan S, Eckert K, et al. Chronic heart failure beyond city limits. Rural Remote Health 2005;5:443.(online) [PubMed] [Google Scholar]
- 22.Ong MA, Weeramanthri TS. Delay times and management of acute myocardial infarction in Indigenous and non Indigenous people in the Northern Territory. MJA 2000;173:201–4 [DOI] [PubMed] [Google Scholar]
- 23.Cunningham J. Diagnostic and therapeutic procedures among Australian hospital patients identified as Indigenous. MJA 2002;176:58–62 [DOI] [PubMed] [Google Scholar]
- 24.Rowley KG, Daniel M, Skinner K, et al. Effectiveness of a community-directed ‘healthy lifestyle’ program in a remote Australian aboriginal community. Aust N Z J Public Health 2000;24:136–44 [DOI] [PubMed] [Google Scholar]
- 25.Driscoll A, Davidson P, Clark R, et al. Tailoring consumer resources to enhance self care in chronic heart failure. Aust Crit Care 2009;22:133–40 [DOI] [PubMed] [Google Scholar]
- 26. Sheperd F, Battye K, Chalmers E. Improving access to cardiac rehabilitation for remote Indigenous clients. Aust N Z J Public Health 2003;27:632–6. [DOI] [PubMed] [Google Scholar]
- 27.Teng THK, Hung J, Finn J. The effect of evidence-based medication use on long-term survival in patients hospitalized for heart failure in Western Australia. MJA 2010;192:306–10 [DOI] [PubMed] [Google Scholar]
- 28.Wang OJ, Krumholz HM. Clinical trial participation: are we studying the patients we are trying to treat? Eur J Heart Fail 2009;11:1021–2 [DOI] [PubMed] [Google Scholar]
- 29.Najafi F, Dobson AJ, Jamrozik K. Recent changes in heart failure hospitalizations in Australia. Eur J Heart Fail 2007;9:228–33 [DOI] [PubMed] [Google Scholar]
- 30.Krumholz HM, Currie PM, Riegel B, et al. ; American Heart Association Disease Management Taxonomy Writing Group A taxonomy for disease management: a scientific statement from the American Heart Association Disease Management Taxonomy Writing Group. Circulation 2006;114:1432–45 [DOI] [PubMed] [Google Scholar]
- 31.Bonow RO, Bennett S, Casey DE, et al. Clinical performance measures for adults with chronic heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures. Circulation 2005;112:1853–87 [DOI] [PubMed] [Google Scholar]
- 32.Spertus JA, Bonow RO, Chan P, et al. ACCF/AHA New insights into the methodology of performance measurement: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures. Circulation 2010;122:2091–106 [DOI] [PubMed] [Google Scholar]
- 33.Riegel B, Lee CS, Sochalski J. Developing an instrument to measure heart failure disease management program intensity and complexity. Circ Cardiovasc Qual Outcomes 2010;3:324–30 [DOI] [PubMed] [Google Scholar]
- 34.Fonarow GC, Abraham WT, Albert NM, et al. Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF): rationale and design. Am Heart J 2004;148:43–51 [DOI] [PubMed] [Google Scholar]
- 35.Fonorrow GC, Yancy CW, Albert NM, et al. Improving the use of evidence based heart failure therapies in the outpatient settings: the IMPROVE HF performance improvement registry. Am Heart J 2007;154:12–38 [DOI] [PubMed] [Google Scholar]
- 36.Cleland JCF, Sewdberg K, Cohen-Solal A, et al. ; The Euro Heart Failure Survey of The EUROHEART Survey Programme: a survey on the quality of care among patients with heart failure in Europe. Euro J Heart Fail 2000;2:123–32 [DOI] [PubMed] [Google Scholar]
- 37.Ambedkar AV, Fonarrow GC, Hernandez AF, et al. Characteristics and in-hospital outcomes for non-adherant patients with heart failure: get with the Guidelines-Heart Failure (GWTG-HF). Am Heart J 2009;158:644–52 [DOI] [PubMed] [Google Scholar]
- 38.Patterson ME, Hernandez AF, Hammill BG, et al. Process of care performance measures and long-term outcomes in patients hospitalized with heart failure. Med Care 2010;48:210–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Silver MA, Peacock WF, Diercks DB. Optimizing treatment and outcomes in acute heart failure beyond initial triage. CHF 2006;12:137–45 [DOI] [PubMed] [Google Scholar]
- 40.Gheorghiade M, Zannad F, Sopko G, et al. Acute heart failure syndromes: current state and framework for future research. Circulation 2005;112:3958–68 [DOI] [PubMed] [Google Scholar]
- 41.National Statement of Ethical in Human Research National Health and Medical Research Council Australian Research Council Australian Vice-Chancellors’ Committee 2007.
- 42.Gueorguieva R, Krystal JH. Move over ANOVA: progress in analyzing repeated-measures data and its reflection in papers published in the archives of general psychiatry. Arch Gen Psychiatry 2004;61:310–17 [DOI] [PubMed] [Google Scholar]
- 43.Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices primary results of the registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation 2010;122:585–96 [DOI] [PubMed] [Google Scholar]
- 44.Iyngkaran P, Thomas M, Majoni W, et al. Comorbid heart failure and renal impairment—epidemiology and management. Cardiorenal Med 2012;2:281–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ansari Z. A review of literature on access to primary health care. Aust J Prim Health 2007;13:80–95 [Google Scholar]
- 46.Ansari Z, Barbetti T, Carson NJ, et al. The Victorian ambulatory care sensitive conditions study: rural and urban perspectives. Soz Präventivmed 2003;48:33–43 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.