Abstract
Background
The prevalence of weight loss is a quality indicator for nursing homes (NH), and monthly weight assessments are conducted by NH staff to determine weight loss.
Methods
A longitudinal study was conducted with 90 long-stay residents in four NHs for 12 study months. Monthly weight values documented in the medical record by NH staff were compared to independent weight values collected by research staff using a standardized protocol. Weight loss was defined according to the Minimum Data Set (MDS) criterion: ≥ 5% in 30 days or ≥ 10% in 180 days.
Results
The total frequency of weight loss episodes per person was comparable between NH and research staff weight assessments across the 12 study months. However, monthly weight values recorded by NH staff were consistently higher than values recorded by research staff, which resulted in a higher prevalence of weight loss and earlier identification of weight loss according to research staff weight values using a standardized weighing protocol.
Conclusions
A standardized weighing protocol improved the detection of weight loss among NH residents and should allow for earlier nutrition intervention.
Introduction
Unintentional weight loss is a common problem among nursing home (NH) residents that is associated with adverse, costly clinical outcomes (1–4). A cross-sectional study showed a 9.9% prevalence of weight loss among NH residents according to the Minimum Data Set (MDS) quality indicator criterion (i.e., ≥ 5% in 30 days or 10% in 180 days) (2). Nursing homes are required to weigh residents monthly. Monthly weight values are used to determine the prevalence of weight loss, which is reported quarterly on the MDS as a quality indicator. In one cross-sectional study, research staff used a standardized protocol to review medical record data for up to 12 months for 400 residents in 16 NHs (5). Results showed that NH staff documented monthly weight values for 100% of the study sample, and weight loss based on the monthly weight values documented in the medical record matched weight loss reported on the most recent MDS assessments for the same residents and time period. However, the accuracy of the monthly weight values was not determined as part of this study (5).
A separate study sponsored by the Centers for Medicare and Medicaid Services (CMS) concluded that “prevalence of weight loss” was less accurate than other MDS-derived quality indicators, although the methods used to reach this conclusion were not specified in this study (6). Still, these results raised questions about whether MDS-derived “prevalence of weight loss” should be used as an NH quality indicator. There have been no additional studies, to date, that directly address this question; but, the MDS-derived prevalence of weight loss data have been made available on a CMS public reporting system (http://www.nursinghomecompare.org) due to clinical importance.
Separate studies have evaluated the accuracy of NH staff medical record documentation related to other nutritional care processes including residents’ food and fluid intake, NH staff provision of mealtime feeding assistance, and NH staff delivery of oral liquid nutrition supplements (7–13). The results of these studies showed that NH staff documentation was erroneous for all of these daily nutritional care processes when compared to independent assessments by research staff using standardized, observational protocols. Moreover, NH staff documentation reflected a consistent over-estimate of resident intake and a significantly higher frequency of mealtime feeding assistance and nutrition supplement delivery when compared to independent assessments by research staff (7–13). Given erroneous medical record documentation related to other key nutritional care processes found in previous studies, two hypotheses were tested in this study:
NH staff documentation of monthly weight values will be erroneous compared to independent assessments by research staff using a standardized weighing protocol; and
NH staff documentation of monthly weight values will reflect a consistent over-estimate of residents’ body weight compared to independent assessments by research staff.
Methods
Setting and Recruitment
Participants were recruited from four skilled NHs, one of which was proprietary, housing a total of 433 residents. Nurse-aide level staff-to-resident ratios ranged from 5 to 11 residents per aide (mean = 8.1 ± 2.3) on the day shift (7am to 3pm) and 10 to 15 residents per aide (mean = 12.7 ± 1.6) on the evening shift (3pm to 11pm). Licensed nurse staff-to-resident ratios ranged from 12 to 15 (mean = 13.6 ± 0.9) and 22 to 33 (mean = 27.3 ± 4.4) residents per licensed staff on the day and evening shifts, respectively, across the four sites.
Participants for this study were part of a larger clinical intervention trial, which required residents to be long-stay (non-Medicare), free of a feeding tube, not receiving end-of-life (hospice) care and not on a planned weight loss diet. The larger clinical intervention trial was designed to increase oral food and fluid intake and body weight through the provision of improved feeding assistance care; and, the intervention had a significant effect on both outcomes for the intervention group relative to the control group (14). The purpose of the current study was to evaluate the accuracy of NH staff documentation of residents’ monthly body weight values, and the accuracy of this documentation should not be influenced by the clinical intervention trial or a resident’s assignment to the intervention versus control groups. Although, the prevalence of weight gain and/or loss for study participants assigned to the intervention group (approximately one-half of the sample) is not representative of usual NH care.
A total of 310 (72%) residents met inclusion criteria for the larger study, and written consent was obtained from either the resident or the resident’s responsible party designated in the medical record for 173 (56%) eligible residents. A total of 83 residents were lost from the study over 12 months due to prolonged hospitalization or death (50), transfer out of the facility (18), transfer to hospice (2), feeding tube insertion (2), new planned weight loss diet (1), or consent withdrawal (10). The remaining 90 (52%) residents who completed all 12 study months comprised the sample for this study.
Measures
Demographic, medical and nutritional information was retrieved from each participant’s medical record. Information related to the resident’s need for staff assistance to eat was retrieved from their most recent MDS assessment (section G. physical functioning, item 1h. eating dependency). The MDS eating dependency rating ranges from 0 (independent, no help or oversight needed) to 4 (total dependence, full staff performance of activity) (15). Participants’ cognitive status was assessed by research staff using a standardized, performance-based assessment (Mini-Mental State Examination [MMSE]), with a score range from 0 (severely impaired or comatose) to 30 (cognitively intact) (16). Physician and/or dietitian orders for an oral liquid nutrition supplement and type of prescribed diet were retrieved from medical records. Diet orders were divided into two categories: regular diet versus any type of special diet order, including dietary restrictions (e.g., no added salt, no concentrated sugars) and/or altered texture (e.g., ground, mechanical soft, puree, added thickeners).
Independent Assessment of Body Weight by Research Staff
Independent assessments of body weight were conducted by trained research staff for 12 consecutive study months using a standardized protocol. The standardized protocol required research staff to weigh residents in the morning, prior to breakfast but following incontinence care, while the resident remained in bed clothes without shoes. Research staff used the same facility scale(s) as NH staff for weighing study participants to reduce measurement error due to differences in instrumentation, but research staff ensured the scale was calibrated to zero prior to each weighing episode. All four NHs in this study had two types of scales: chair scale for residents with limited or no ability to stand without staff assistance, and a bed scale for residents who were bed-bound. In most cases, the chair scale was used in all four sites as few study participants were bed-bound. The standardized weighing protocol implemented by research staff was considered the gold standard in this study.
Research staff attempted to weigh participants within the same week, if not the same day, as NH staff scheduled weighing procedures to reduce the number of elapsed days between the two data sources. Nursing home staff recorded weight values were abstracted from each participant’s medical record during the same month that research staff weighed the participant for each of the 12 consecutive study months. Independent assessments of participants’ body weight by research staff were used to calculate Body Mass Index (BMI, Refer to Table 1 footnotes for formula). A BMI value less than 20 was considered indicative of under-nutrition (17).
Table 1.
Demographic, Medical, and Nutritional Characteristics of Participants (n=90)
| Measure | Percent (n) or Mean (±Standard Deviation) |
|---|---|
| Demographic Characteristics | |
| Percent Female | 80.0% (72) |
| Percent White | 78.9% (71) |
| Age | 82.9 (± 10.0) |
| Length of Stay in Years | 2.9 (± 3.3) |
| Medical Characteristics | |
| Percent with a Physician-recorded diagnosis of Depression | 41.1% (37) |
| Percent with a Physician-recorded diagnosis of Dementia | 37.8% (34) |
| Mini Mental State Exam (MMSE) Total Score (0–30) | 15.8 (± 8.7) |
| Nutritional Characteristics | |
| MDS Eating Dependency (0–4)* | 1.0 (± 1.4) |
| Percent MDS Eating Dependency > 0 | 36.7% (33) |
| Percent with an Oral Liquid Nutrition Supplement Order | 48.9% (44) |
| Percent with a Special Diet Ordera | 93.3% (84) |
| Percent with a Body Mass Index (BMI) < 20b | 17.8% (16) |
Minimum Data Set (MDS) eating dependency item (section G. physical functioning, item 1h) is scored: (0) independent, (1) supervision, (2) limited assistance, (3) extensive assistance, (4) totally dependent on staff to eat.
Special diets included any restrictions (no added salt, no concentrated sugars) or altered texture (ground, mechanical soft, puree, thickened liquids).
Body Mass Index (BMI) formula = 0.454 weight in pounds/(0.254 height in inches)2 A BMI below 20 is considered indicative of under-nutrition.
Data Analyses
Comparisons were conducted between participants who completed all 12 study months (n = 90) and those lost from the study (n = 83) using independent samples T-tests for continuous measures (e.g., age, length of stay, MMSE total score) and chi-square analyses for categorical measures (e.g., special diet orders, diagnosis of dementia or depression). Monthly weight values documented by research staff were compared to values documented by NH staff for each of the 12 months in two ways. First, T-tests for paired samples were conducted using the continuous data (weight in pounds based on the two data sources). Second, monthly difference values were calculated such that a positive difference value indicated that NH staff recorded a value higher than research staff for the same resident and month. The distributions of the monthly difference values were examined for skewness and to identify a potential pattern of over versus under-estimation of body weight by NH staff compared to research staff values. The total number of elapsed days between the two measurement dates (research versus NH staff documentation) also was calculated for each study month.
Primary analyses focused on weight loss episodes according to the two data sources due to the clinical significance of weight loss as an MDS-derived quality indicator. However, secondary analyses also were conducted for weight gain episodes according to the two data sources primarily to determine of the error rate differed for the detection of weight gain episodes relative to weight loss episodes. Episodes of weight loss and/or gain were determined according to each data source (research versus NH staff weight values) using the MDS criteria (≥5% in 30 days or ≥ 10% in 180 days) (15). Thus, a determination of the number of weight change episodes that met the criterion “≥ 5% in 30 days” was based on 11 monthly comparisons (e.g., months 1–2, 2–3, 3–4,…); while, a determination of the number of weight change episodes that met the criterion “≥ 10% in 180 days” was based on six comparisons (i.e., month 1–7, 2–8, 3–9, 4–10, 5–11, 6–12). An attempt was not made to directly compare the weight loss/gain data reported on the most recent MDS assessment by NH staff to the weight loss/gain data collected by research staff for study participants, because MDS data was completed by NH staff at varying time points during the 12 study months for each participant, based on admission date to the facility.
The total frequency of weight loss episodes that met the MDS criteria was calculated for each study participant across the 12 study months based on each data source and compared using a T-test for paired samples (total frequency of weight loss episodes) and a Kappa agreement statistic for the categorical measure (i.e., no episodes of weight loss versus one or more episodes of loss). The data were further examined to identify the first month within which a weight loss/gain episode that met MDS criteria occurred according to each data source to determine if research staff weight values resulted in the earlier identification of a loss/gain compared to NH staff weight values.
Results
Subjects and Setting
Table 1 shows the characteristics of the 90 study participants. Participants lost from the study (n=83) had a shorter length of NH stay (1.9 ± 2.2 years; t = 2.18, p = .013), and a smaller proportion had a special diet order (82.3%, χ2 = 4.93, p = .026) compared to those who completed the study (n = 90 shown in Table 1). There were no other characteristics that were significantly different between the two groups (Table 1).
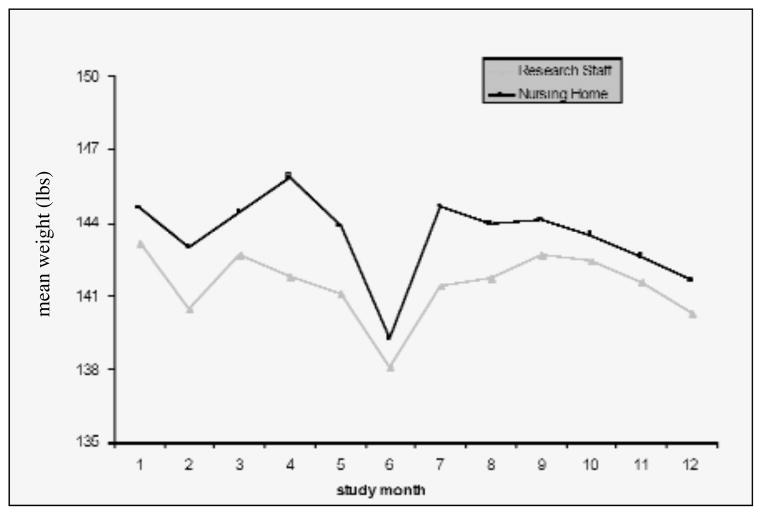
A Comparison of Nursing Home and Research Staff Weight Values
The average number of elapsed days between research and NH staff recorded weight values was 0.1 (± 7.3) days (range 0 to 31) across the 12 study months. Nursing home staff values were significantly correlated with research staff values (Pearson correlation coefficients ranged from 0.951 to 0.997, p<.001, for all 12 months). However, difference values were positively skewed for 9 of the 12 monthly comparisons, indicating a consistent pattern wherein NH weight values were consistently higher than research staff weight values for most months. Figure 1 shows the mean weight for the group of participants according to each data source and study month. NH staff monthly weight values were consistently higher than research staff weight values across all 12 study months (Figure 1).
Figure 1.
Difference between Nursing Home and Research Staff Weight Assessments by Study Month (n=90)
Grey line represents research staff weight values. Black line represents Nursing Home staff weight values. X axis represents the twelve study months from month1 to month12. Y axis represents the mean weight in pounds.
The average total frequency of weight loss episodes that met MDS criteria was 0.5 (± 1.1) and 0.7 (± 1.3) per person across the 12 study months according to NH and research staff recorded weight values, respectively. According to NH staff documentation, 26.7% (n = 24) of the participants experienced one or more weight loss episodes that met MDS criteria during the 12 study months. In comparison, research staff documentation showed a significantly higher proportion of participants, 33.3% (n =30), had experienced one or more weight loss episodes that met MDS criteria (χ2 = 16.36, p = .000). The Kappa agreement statistic between the two data sources was 0.421, p<.001. Nursing home weight values showed weight loss that met MDS criteria for 8 participants (9% of total sample) whose weight loss did not meet criteria according to research staff values. Conversely, research staff values showed weight loss that met criteria for 14 participants (15.5% of total sample) who did not meet criteria according to NH staff values. Of the participants who experienced one or more weight loss episodes meeting MDS criteria according to research staff documentation (n = 30), research staff weight values resulted in the earlier identification of weight loss by one month or more for 73.3% (22 of the 30).
The average total frequency of weight gain episodes that met MDS criteria was 0.2 (± 0.5) and 0.3 (± 0.6) per person across the 12 study months according to NH and research staff recorded weight values, respectively. Nursing home staff documentation showed that 17.8% (n =16) experienced weight gain; where as, research staff values showed that a significantly higher proportion of participants, 22.2% (n =20), experienced weight gain (χ2 = 8.69, p = .003; Kappa = 0.308, p = .003). Nursing home weight values showed weight gain that met MDS criteria for 8 participants (9% of total sample) whose weight gain did not meet criteria according to research staff values. Conversely, research staff values showed weight gain that met criteria for 12 participants (13.3% of total sample) who did not meet criteria according to NH staff values. Of the participants who experienced one or more weight gain episodes that met MDS criteria according to research staff documentation (n =20), research staff values resulted in the earlier identification of the gain by one month or more for 70% (14 of the 20).
Discussion
The purpose of this study was to evaluate the accuracy of monthly weight values documented in the medical record by NH staff compared to research staff weight values using a standardized weighing procedure. Results showed that research staff assessments resulted in a significantly higher prevalence of weight loss episodes that met MDS criteria across the 12 study months. These findings support the contention from a previous study that the MDS “prevalence of weight loss” quality indicator may not be accurate if based on NH staff documentation of residents’ monthly body weight values (6).
Another important finding from this study was that monthly weight values recorded by NH staff were consistently higher than values recorded by research staff, which resulted in the earlier identification of weight loss episodes by research staff. The earlier identification of weight loss using a standardized weighing procedure has implications for earlier nutrition intervention to improve oral intake and prevent further loss, such as an increase in staff attention during meals or offering the resident additional foods and fluids between meals. Both of these nutrition interventions have been shown to improve residents’ daily caloric intake and promote weight gain over time (14, 18). Results also showed that the error rate in NH staff recorded weight values was comparable for detecting weight loss or weight gain. These findings suggest that NH staff have difficulty monitoring monthly changes in residents’ body weights for both episodes of gain and loss.
There are a number of study limitations. First, there was a large attrition rate over the course of the 12-month study, primarily due to death. Second, study participants were predominately female and White; thus, results may not be generalizable to male and/or minority NH residents. Third, findings about the timeliness of weight loss identification are limited to the sub-sample of participants who experienced a weight loss that met MDS criteria.
Despite these limitations, this study provides important data that directly evaluates the accuracy of NH staff weight values documented in the medical record monthly and used to report MDS prevalence of weight loss. Based on these data, NH staff eventually identify clinically significant weight loss episodes among residents but do not consistently identify these episodes as soon as the loss occurs (i.e., within the same month), and it is likely the prevalence of weight loss reported on the MDS reflects a significant under-estimate. There appears to be consensus that NH residents’ weight values represent an important measure of nutritional status and associated care quality and, as such, efforts should be made to ensure accuracy and timeliness in the identification of weight loss episodes. The standardized weighing procedure described in this study may increase the accuracy of weight assessments and result in the earlier identification of weight loss to allow for earlier nutrition intervention (see recommended clinical guideline).
Clinical Guideline for Weighing Procedures in Nursing Homes
A standardized weighing protocol should be used to assess residents’ body weight monthly. The key component of a standardized weighing protocol is consistency for the following elements:
Type of Scale
Residents should be routinely weighed on the same type of scale (e.g., chair versus bed) and staff should ensure the scale is calibrated to zero prior to each weighing episode. If the scale cannot be manually calibrated to zero, a small hand-held weight (5 lb or 10 lb) can be stored near the scale to check accuracy.
Time of Day
Residents should be routinely weighed at the same time of day (e.g., before or after breakfast) each month.
Clothing
Residents should be routinely weighed in their bed clothes for the most accurate body weight to avoid weighing errors due to additional items (e.g., shoes, hat, sweater, lap blanket). If a resident has incontinence, staff should provide incontinence care prior to weighing.
Staff member
Staff responsible for weighing residents should be trained in the operation of the facility scale(s) and the importance of using a standardized procedure to ensure accurate weight values. For auditing purposes, a supervisory-level person should observe the staff while s/he is conducting residents’ weights (e.g., approximately 5 residents per month) to ensure that standardized procedures are being followed consistently and weight values are being recorded accurately. An observation tool for auditing purposes is available (upon request from the first author). In addition, monthly changes in residents’ body weights, ideally, should be calculated via computer to avoid mathematical errors.
Acknowledgments
This research was supported by Grant AG10415 from the National Institute on Aging and Grant AG01026-01A1 from the National Institute of Health, UCLA Claude D. Pepper Older Americans Independence Center. The authors thank all research staff who worked on this project, and Jeremy Berger, who assisted with data management.
Footnotes
There are no financial conflicts of interest for any of the authors.
Each author contributed to study concept, data analysis, interpretation of data, and/or manuscript preparation.
Financial disclosure: None of the authors had any financial interest or support for this paper.
References
- 1.Abassi AA, Rudman D. Undernutrition in the nursing home: Prevalence, consequences, causes, and prevention. Nutr Rev. 1994;52(4):113–122. doi: 10.1111/j.1753-4887.1994.tb01403.x. [DOI] [PubMed] [Google Scholar]
- 2.Blaum CS, Fries BE, Fiatarone MA. Factors associated with low body mass index and weight loss in nursing home residents. J Gerontol A:Bio Sci Med Sci. 1995;50A:M162–M168. doi: 10.1093/gerona/50a.3.m162. [DOI] [PubMed] [Google Scholar]
- 3.Dwyer JT, Coleman KA, Krall E, et al. Changes in relative weight among institutionalized elderly adults. J Gerontol A:Bio Sci Med Sci. 1987;42(3):246–251. doi: 10.1093/geronj/42.3.246. [DOI] [PubMed] [Google Scholar]
- 4.Sullivan DH, Johnson LE, Bopp MM, Roberson PK. Prognostic significance of monthly weight fluctuations among older nursing home residents. J Gerontol A:Bio Sci Med Sci. 2004;59A(6):633–639. doi: 10.1093/gerona/59.6.m633. [DOI] [PubMed] [Google Scholar]
- 5.Simmons SF, Garcia ET, Cadogan MP, et al. The Minimum Data Set weight-loss quality indicator: Does it reflect differences in care processes related to weight loss? J Am Geriatr Soc. 2003;51:1410–1418. doi: 10.1046/j.1532-5415.2003.51459.x. [DOI] [PubMed] [Google Scholar]
- 6.The National Quality Forum. National Voluntary Consensus Standards for Nursing Home Care: A consensus report. Washington, DC: National Quality Forum; 2004. [Google Scholar]
- 7.Castellanos VH, Andrews YN. Inherent flaws in a method of estimating meal intake commonly used in long-term-care facilities. J Am Diet Assoc. 2002;102(6):826–830. doi: 10.1016/s0002-8223(02)90184-7. [DOI] [PubMed] [Google Scholar]
- 8.Kayser-Jones J, Schell ES, Porter C, et al. A prospective study of the use of liquid oral dietary supplements in nursing homes. J Am Geriatr Soc. 1998;46:1378–1386. doi: 10.1111/j.1532-5415.1998.tb06004.x. [DOI] [PubMed] [Google Scholar]
- 9.Kayser-Jones J, Schell E, Porter C, Paul S. Reliability of percentage figures used to record the dietary intake of nursing home residents. Nursing Home Medicine. 1997;5(3):69–76. [Google Scholar]
- 10.Pokrywka HS, Koffler KH, Remsburg R, et al. Accuracy of patient care staff in estimating and documenting meal intake of nursing home residents. J Am Geriatr Soc. 1997;45:1223–1227. doi: 10.1111/j.1532-5415.1997.tb03774.x. [DOI] [PubMed] [Google Scholar]
- 11.Schnelle JF, Bates-Jensen B, Chu L, Simmons SF. Accuracy of nursing home medical record information about care process delivery: Implications for staff management and improvement. J Am Geriatr Soc. 2004;52(8):1378–1383. doi: 10.1111/j.1532-5415.2004.52372.x. [DOI] [PubMed] [Google Scholar]
- 12.Simmons SF, Reuben D. Nutritional intake monitoring for nursing home residents. A comparison of staff documentation, direct observation, and photography methods. J Am Geriatr Soc. 2000;48:209–213. doi: 10.1111/j.1532-5415.2000.tb03914.x. [DOI] [PubMed] [Google Scholar]
- 13.Simmons SF, Patel AV. Nursing home staff delivery of oral liquid nutritional supplements to residents at risk for unintentional weight loss. J Am Geriatr Soc. 2006;54(9):1372–1376. doi: 10.1111/j.1532-5415.2006.00688.x. [DOI] [PubMed] [Google Scholar]
- 14.Simmons SF, Keeler E, Xiaohui ZM, Schnelle JF. Prevention of unintentional weight loss in nursing home residents: A controlled trial of feeding assistance. J Am Geriatr Soc. doi: 10.1111/j.1532-5415.2008.01801.x. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Health Care Financing Administration. Long Term Care Facility Resident Assessment Instrument (RAI) User’s Manual, Minimum Data Set, Version 2. Natick: MA, Eliot Press; 1999. [Google Scholar]
- 16.Molloy DW, Alemayehu E, Roberts R. A standardized Mini-Mental State Examination (SMMSE): Its reliability compared to the traditional Mini-Mental State Examination (MMSE) Am J Psychiatry. 1991;148:102–105. doi: 10.1176/ajp.148.1.102. [DOI] [PubMed] [Google Scholar]
- 17.Thomas DR, Ashmen W, Morley JE, Evans WJ the Council for Nutritional Strategies in Long-Term Care. Nutritional management in long term care: Development of a clinical guideline. J Gerontol A:Bio Sci Med Sci. 2000;55A(12):M725–M734. doi: 10.1093/gerona/55.12.m725. [DOI] [PubMed] [Google Scholar]
- 18.Simmons SF, Schnelle JF. Individualized feeding assistance care for nursing home residents: Staffing requirements to implement two interventions. J Gerontol A:Bio Sci Med Sci. 2004;59A(9):966–973. doi: 10.1093/gerona/59.9.m966. [DOI] [PubMed] [Google Scholar]