Abstract
OBJECTIVE
To examine the use of inpatient hysterectomy and explore changes in the use of various routes of hysterectomy and patterns of referral.
METHODS
The Nationwide Inpatient Sample was used to identify all women aged 18 years or older who underwent inpatient hysterectomy between 1998 and 2010. Weighted estimates of national trends were calculated and the number of procedures performed estimated. Trends in hospital volume and across hospital characteristics were examined.
RESULTS
After weighting, we identified a total 7,438,452 women who underwent inpatient hysterectomy between 1998 and 2010. The number of hysterectomies performed annually rose from 543,812 in 1998 to a peak of 681,234 in 2002; it then declined consistently annually and reached 433,621 cases in 2010. Overall, 247,973 (36.4%) fewer hysterectomies were performed in 2010 compared with 2002. From 2002 to 2010 the number of hysterectomies performed for each of the following indications declined: leiomyoma (−47.6%), abnormal bleeding (−28.9%), benign ovarian mass (−63.1%), endometriosis (−65.3%), and pelvic organ prolapse (−39.4%). The median hospital case volume decreased from 83 procedures per year in 2002 to 50 cases per year in 2010 (P<.001).
CONCLUSION
The number of inpatient hysterectomies performed in the United States has declined substantially over the past decade. The median number of hysterectomies per hospital has declined likewise by more than 40%.
LEVEL OF EVIDENCE
III
Hysterectomy is one of the most commonly performed surgical procedures in women.1 Estimates suggest that one in nine women will undergo hysterectomy during their lifetime and that approximately 600,000 procedures are performed each year in the United States.1 Although hysterectomy is the treatment for most gynecologic malignancies, the vast majority of hysterectomies are undertaken for benign gynecologic disease.
Over the past decade, a number of national trends have had a strong influence on the practice of surgery.2,3 First, there has been great interest in conservative, nonsurgical treatments for many diseases.2,4,5 In gynecology, uterine artery embolization has been introduced for the treatment of leiomyomata and non-surgical treatments and ablative therapies are now commonly used for abnormal bleeding.6-10 Similarly, more conservative treatment is now often used for women with cervical dysplasia and uterine-sparing procedures are increasingly used for genital tract malignancies.11,12 Second, minimally invasive surgical techniques have been introduced for many procedures. Although vaginal hysterectomy has been performed for decades, laparoscopically assisted hysterectomy and total laparoscopic hysterectomy have been used since the 1990s and, more recently, robotic-assisted hysterectomy has been described.13-15 Minimally invasive approaches to hysterectomy offer many advantages and may be performed as outpatient procedures.
Finally, for many general surgical procedures, there have been changes in referral patterns based on public reporting and quality initiatives. Efforts have focused on concentrating high-risk and specialized procedures to high-volume facilities and centers of excellence.2 To date, little is known about how these changing trends have influenced hysterectomy rates. We performed a population-based analysis to determine the use of inpatient hysterectomy and explored changes in the use of various routes of hysterectomy and patterns of referral.
PATIENTS AND METHODS
Data from the Nationwide Inpatient Sample from the Agency for Healthcare Research and Quality were used for the analysis. The Nationwide Inpatient Sample, the largest publicly available all-payer inpatient care database in the United States, contains a random sample of approximately 20% of discharges from all hospitals within the United States. The sampling frame for Nationwide Inpatient Sample includes nonfederal, general, and specialty-specific hospitals throughout the United States. Sampled hospitals include both academic and community facilities. The Nationwide Inpatient Sample included approximately 8 million hospital stays from 45 states in 2010.16 Institutional review board exemption was obtained from Columbia University to perform this study.
We analyzed women aged 18 years or older who underwent inpatient hysterectomy between 1998 and 2010. Patients were stratified based on the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) coding into five groups based on the type of hysterectomy performed: abdominal (68.3, 68.39, 68.4, 68.49, 68.9), vaginal (68.5, 68.59), laparoscopic (68.31, 68.41, 68.51), robotic (17.4× and any other code for hysterectomy), and radical (68.6, 68.61, 68.69, 68.7). Each procedure was further classified as a total or subtotal (supracervical) hysterectomy.
Concomitant procedures performed at the time of hysterectomy were recorded based on ICD-9-CM coding and included oophorectomy (either unilateral or bilateral), anterior colporrhaphy, posterior colporrhaphy, and anti-incontinence repair procedures.17-19 Each of the following indications for surgery was examined: leiomyoma, endometriosis, abnormal bleeding, benign ovarian neoplasms, pelvic organ prolapse, and gynecologic cancer. Patients may have had multiple indications for surgery.17-19
Age was classified as less than 40 years, 40–49 years, 50–59 years, 60–69 years, 70–79 years, and 80 or more years. Race was categorized as white, black, Hispanic, other, and unknown. Each patient’s household income was classified by Nationwide Inpatient Sample as low, medium, high, or highest. Similarly, insurance status was grouped as private, Medicare, Medicaid, self-pay, other, and unknown. Risk adjustment for medical comorbidities was performed using the Elixhauser comorbidity index. Patients were categorized based on the number of medical comorbidities into: zero, one, or two or more, as previously reported.20
The hospitals in which patients were treated were characterized based on location (urban, rural), region of the country (northeast, midwest, west, south), size (small, medium, large), and teaching status (teaching, nonteaching). Hospital volume was calculated annually as the total number of hysterectomies performed within a given hospital. For each year, the numbers of patients treated at the highest decile by volume and highest quartile by volume were estimated.
National estimates of the number of inpatient hysterectomies performed were obtained through weighted discharge-level estimates provided by Nationwide Inpatient Sample. Within the Nationwide Inpatient Sample, each patient record contains a “discharge weight.” These weights are calculated by stratifying hospitals within the Nationwide Inpatient Sample based on the following characteristics: geographic region, urban or rural location, teaching status, bed size, and hospital ownership. Based on this schema, a weight is obtained by dividing the number of Nationwide Inpatient Sample discharges within a given hospital stratum by the number of discharges within that universe of hospital discharges within that stratum using data obtained from the American Hospital Association. When the resulting weight is applied, it is an estimate of all hospital discharges within the United States.21
Frequency distributions between categorical variables were compared using χ2 tests. Trends in use of each type of hysterectomy as well as trends based on indication and hospital characteristics are reported descriptively. Mean and median hospital volumes were compared across the years of study using analysis of variance and Kruskal-Wallis tests, respectively. χ2 tests were used to examine changes in the number of patients treated in the top decile and top quartile by volume hospitals over the course of the study.
In addition to the overall analyses, a series of sensitivity analyses were performed. In the sensitivity analyses, the patients who underwent hysterectomy for leiomyomata were selected and trends in performance based on hospital teaching status, hospital size, payer mix, and race were performed. P<.05 was considered statistically significant. All analyses were conducted with SAS 9.13. All statistical tests were two-sided.
RESULTS
A total of 1,507,433 women who underwent inpatient hysterectomy were identified (Table 1). After weighting, this yielded a cohort of 7,438,452 women who underwent inpatient hysterectomy between 1998 and 2010. The total number of hysterectomies performed annually in the United States rose from 543,812 in 1998 to a peak of 681,234 procedures in 2002. From 2002 to 2010, the number of inpatient hysterectomies performed annually declined consistently each year and reached 433,621 cases in 2010 (Fig. 1). Overall, 247,973 (36.4%) fewer inpatient hysterectomies were performed in 2010 compared with 2002.
Table 1.
Clinical and Demographic Characteristics of the Cohort Stratified by Hysterectomy Type
| Abdominal (n=974,096, 64.6%) | Vaginal (n=304,850, 20.2%) | Laparoscopic (n=197,746, 13.1%) | Robotic (n=13,219, 0.9%) | Radical (n=17,522, 1.2%) | P | |
|---|---|---|---|---|---|---|
| Age (y) | <.001 | |||||
| Younger than 40 | 237,087 (24.3) | 79,637 (26.1) | 60,770 (30.7) | 2,215 (16.8) | 4,203 (24.0) | |
| 40–49 | 443,900 (45.6) | 107,089 (35.1) | 86,889 (43.9) | 4,732 (35.8) | 4,782 (27.3) | |
| 50–59 | 169,225 (17.4) | 49,607 (16.3) | 32,298 (16.3) | 3,684 (21.0) | 2,969 (22.5) | |
| 60–69 | 66,407 (6.8) | 35,577 (11.7) | 11,568 (5.9) | 2,003 (15.2) | 2,661 (15.2) | |
| 70–79 | 41,754 (4.3) | 26,338 (8.6) | 5,026 (2.5) | 960 (7.3) | 1,599 (9.1) | |
| 80 or older | 15,633 (1.6) | 6,602 (2.2) | 1,195 (0.6) | 340 (2.6) | 593 (3.4) | |
| Race | <.001 | |||||
| White | 480,557 (49.3) | 176,461 (57.9) | 119,517 (60.4) | 8,607 (65.1) | 9,353 (53.4) | |
| Black | 127,476 (13.1) | 16,237 (5.3) | 13,394 (6.8) | 1,159 (8.8) | 1,386 (7.9) | |
| Hispanic | 69,825 (7.2) | 22,235 (7.3) | 11,417 (5.8) | 876 (6.6) | 1,687 (9.6) | |
| Other | 41,187 (4.2) | 10,058 (3.3) | 7,021 (3.6) | 708 (5.4) | 1,086 (6.2) | |
| Unknown | 255,051 (26.2) | 79,859 (26.2) | 46,397 (23.5) | 1,869 (14.1) | 4,010 (22.9) | |
| Income | <.001 | |||||
| Low | 159,579 (16.4) | 42,260 (13.9) | 31,384 (15.9) | 2,387 (18.1) | 2,872 (16.4) | |
| Medium | 245,627 (25.2) | 78,939 (25.9) | 49,250 (24.9) | 3,024 (22.9) | 3,978 (22.7) | |
| High | 251,258 (25.8) | 83,069 (27.3) | 52,566 (26.6) | 3,557 (26.9) | 4,465 (25.5) | |
| Highest | 297,681 (30.6) | 94,784 (31.1) | 60,414 (30.6) | 4,051 (30.7) | 57,777 (33.0) | |
| Unknown | 19,951 (2.1) | 5,798 (1.9) | 4,132 (2.1) | 200 (1.5) | 430 (2.5) | |
| Insurance | <.001 | |||||
| Private | 708,279 (72.7) | 210,815 (69.2) | 156,920 (79.4) | 9,290 (70.3) | 10,488 (59.9) | |
| Medicare | 103,413 (10.6) | 50,205 (16.5) | 14,510 (7.3) | 2,430 (18.4) | 3,350 (19.1) | |
| Medicaid | 88,829 (9.1) | 24,422 (8.0) | 14,678 (7.4) | 890 (6.7) | 2,111 (12.1) | |
| Self-pay | 31,672 (3.3) | 6,863 (2.3) | 3,623 (1.8) | 195 (1.5) | 741 (4.2) | |
| Other | 39,126 (4.0) | 11,526 (3.8) | 7,464 (3.8) | 402 (3.0) | 792 (4.5) | |
| Unknown | 2,777 (0.3) | 1,019 (0.3) | 551 (0.3) | 11 (0.1) | 40 (0.2) | |
| Comorbidity | <.001 | |||||
| 0 | 774,001 (79.5) | 274,107 (89.9) | 171,784 (86.9) | 8,216 (62.2) | 2,727 (15.6) | |
| 1 | 137,480 (14.1) | 27,309 (9.0) | 22,602 (11.4) | 3,876 (29.3) | 9,183 (52.4) | |
| More than 1 | 62,615 (6.4) | 3,434 (1.1) | 3,360 (1.7) | 1,127 (8.5) | 5,612 (32.0) | |
| Region | <.001 | |||||
| Northeast | 156,203 (16.0) | 40,000 (13.1) | 27,580 (14.0) | 2,685 (20.3) | 3,141 (17.9) | |
| Midwest | 220,207 (22.6) | 77,662 (25.5) | 42,320 (21.4) | 3,473 (26.3) | 3,721 (21.2) | |
| South | 414,716 (42.6) | 114,450 (37.5) | 82,028 (41.5) | 4,027 (30.5) | 6,102 (34.8) | |
| West | 182,970 (18.8) | 72,738 (23.9) | 45,818 (23.2) | 3,034 (23.0) | 4,558 (26.0) | |
| Area of residence | <.001 | |||||
| Metropolitan | 842,615 (86.5) | 255,290 (83.7) | 169,315 (85.6) | 12,705 (96.1) | 16,873 (96.3) | |
| Nonmetropolitan | 122,273 (12.6) | 47,085 (15.5) | 26,908 (13.6) | 280 (2.1) | 481 (2.8) | |
| Unknown | 9,208 (1.0) | 2,475 (0.8) | 1,523 (0.8) | 234 (1.8) | 168 (1.0) | |
| Hospital size | <.001 | |||||
| Small | 116,440 (12.0) | 39,983 (13.1) | 28,055 (14.2) | 1,006 (7.6) | 1,278 (7.3) | |
| Medium | 258,414 (26.5) | 84,161 (27.6) | 54,290 (27.5) | 2,667 (20.2) | 3,227 (18.4) | |
| Large | 590,034 (60.6) | 178,231 (58.5) | 113,878 (57.6) | 9,312 (70.4) | 12,849 (73.3) | |
| Unknown | 9,208 (1.0) | 2,478 (0.8) | 1,523 (0.8) | 234 (1.8) | 168 (1.0) | |
| Hospital teaching status | <.001 | |||||
| Nonteaching | 530,628 (54.5) | 180,987 (59.4) | 116,723 (59.0) | 5,183 (39.2) | 4,776 (27.3) | |
| Teaching | 434,260 (44.6) | 121,388 (39.8) | 79,500 (40.2) | 7,802 (59.0) | 12,578 (71.8) | |
| Unknown | 9,208 (1.0) | 2,475 (0.8) | 1,523 (0.8) | 234 (1.8) | 168 (1.0) | |
| Indication for surgery | ||||||
| Leiomyoma | 564,917 (58.0) | 109,463 (35.9) | 92,194 (46.6) | 5,163 (39.1) | 3,282 (18.7) | <.001 |
| Endometriosis | 311,707 (32.0) | 68,259 (22.4) | 68,608 (34.7) | 2,250 (17.0) | 2,190 (12.5) | <.001 |
| Abnormal bleeding | 401,852 (41.3) | 120,439 (39.5) | 99,784 (50.5) | 5,212 (39.4) | 1,235 (7.1) | <.001 |
| Benign neoplasm | 263,989 (27.1) | 40,880 (13.4) | 47,930 (24.2) | 1,916 (14.5) | 1,939 (11.1) | <.001 |
| Pelvic organ prolapse | 56,749 (5.8) | 175,627 (57.6) | 40,014 (20.2) | 1,291 (9.8) | 544 (3.1) | <.001 |
| Gynecologic cancer | 108,352 (11.1) | 3,535 (1.2) | 8,254 (4.2) | 3,504 (26.5) | 14,000 (79.9) | <.001 |
| Concomitant procedures | ||||||
| Salpingo-oophorectomy | 698,201 (71.7) | 81,321 (26.7) | 121,044 (61.2) | 8,721 (66.0) | 13,543 (77.3) | <.001 |
| Anterior colporrhaphy | 11,561 (1.2) | 108,767 (35.7) | 16,429 (8.3) | 255 (1.9) | 194 (1.1) | <.001 |
| Posterior colporrhaphy | 16,015 (1.6) | 91,553 (30.0) | 15,647 (7.9) | 304 (2.3) | 184 (1.1) | <.001 |
| Anti-incontinence procedure | 54,817 (5.6) | 56,581 (18.6) | 19,816 (10.0) | 883 (6.7) | 270 (1.5) | <.001 |
| Hysterectomy type | <.001 | |||||
| Total | 891,027 (91.5) | 304,850 (100) | 171,950 (87.0) | 11,942 (90.3) | 17,522 (100) | |
| Subtotal | 83,069 (8.5) | — | 25,796 (13.1) | 1,277 (9.7) | — |
Data are n (%) unless otherwise specified.
Fig. 1.
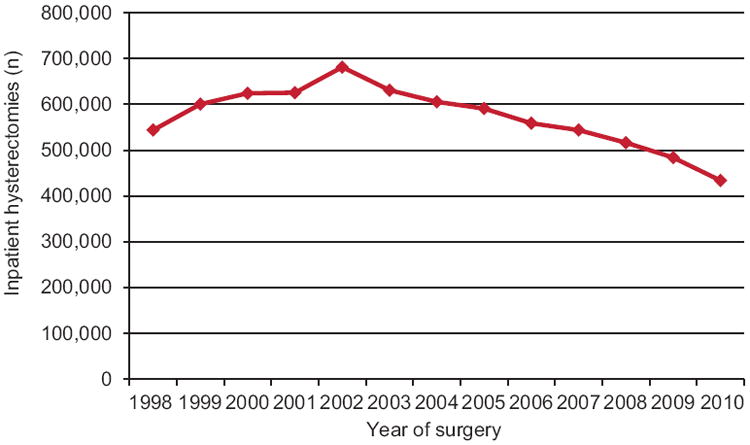
Number of hysterectomies performed stratified by year of the procedure.
Wright. Trends in Use of Inpatient Hysterectomy. Obstet Gynecol 2013.
Figure 2A displays the route of hysterectomy used stratified by year of diagnosis. Abdominal hysterectomy accounted for 65% of procedures in 1998, increased to a peak of 68.9% of cases in 2002, and then declined to 54.2% by 2010. The use of vaginal hysterectomy declined throughout, from 24.8% in 1998 to 16.7% in 2010. Use of laparoscopic hysterectomy increased to a peak of 15.5% of cases in 2006 and then declined to 8.6% of procedures, whereas use of robotic hysterectomy increased from 2008 to 2010 (0.9–8.2%).
Fig. 2.
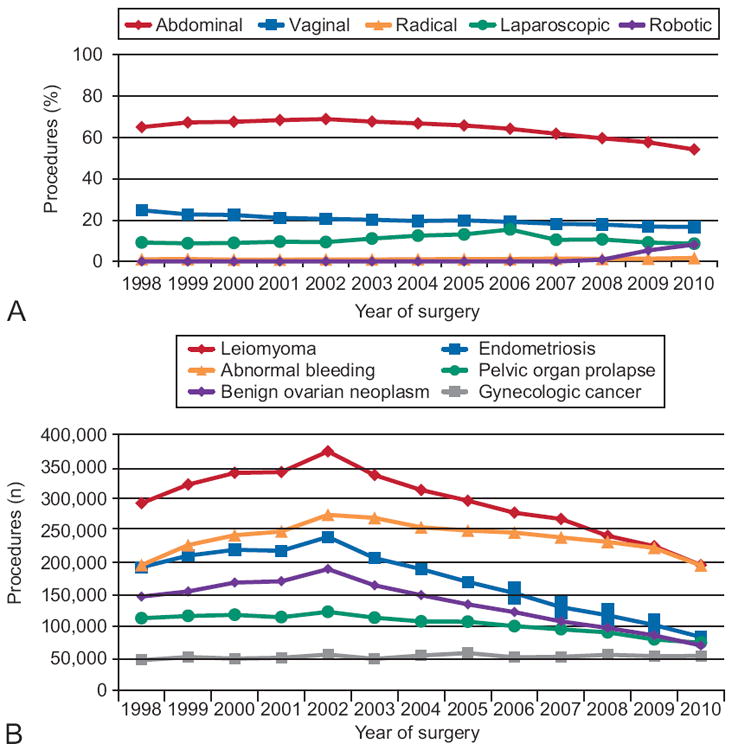
A. Hysterectomies (%) performed via each surgical route by year of procedure. B. Procedures (n) performed each year stratified by indication for surgery.
Wright. Trends in Use of Inpatient Hysterectomy. Obstet Gynecol 2013.
Indications for hysterectomy are shown in Figure 2B. There was a sharp decline in inpatient hysterectomy for leiomyoma that peaked at 373,629 procedures in 2002 and then decreased to 195,735 cases in 2010 (−177,894 cases [−47.6%]). Similarly, hysterectomy for endometriosis rapidly declined from a high of 239,844 operations in 2002 to only 83,158 hysterectomies in 2010 (−156,686 cases [−65.3%]), whereas hysterectomy for benign ovarian mass decreased from 189,560 to 69,937 (−119,623 cases [−63.1%]) during the same timeframe. During the study period, hysterectomy for abnormal bleeding increased to 274,473 in 2002 and then decreased to 195,231 in 2010 (−79,242 cases [−28.9%]). Hysterectomy for pelvic organ prolapse declined from 122,495 cases in 2002 to 74,230 procedures in 2010 (−48,265 cases [−39.4%]). Hysterectomy for gynecologic cancers remained relatively stable with a slight increase from 1998 (47,018) to 2010 (53,506).
Table 2 displays the hospital-level trends in performance of hysterectomy. The mean and median hospital case volumes increased from 1998 to peak values in 2002 (mean 157.2 procedures, standard deviation 201.4; median 83 procedures, interquartile range 15–219). The average hospital volume then decreased over the remaining years of study to a mean of 101.1 cases (standard deviation 131.9) (P<.001) and median of 50 cases (interquartile range 11–134) (P<.001) in 2010. Despite the decrease in mean hospital case volume, the percentage of patients treated at the highest volume hospitals increased over time. The percentage of patients treated at the highest decile by volume hospitals increased from 39.0% in 1998 to 41.5% in 2010 (P<.001). Similarly, 68.8% underwent surgery at the highest quartile by volume hospitals in 1998 compared with 71.2% in 2010 (P<.001).
Table 2.
Trends in Hospital Volume for Performance of Hysterectomy Stratified by Year
| 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Volume | ||||||||||||||
| Hospitals | 903 | 900 | 906 | 896 | 883 | 874 | 872 | 873 | 878 | 869 | 877 | 862 | 860 | |
| Patients | 109,914 | 121,101 | 126,421 | 126,044 | 138,803 | 127,943 | 123,653 | 120,758 | 113,562 | 110,579 | 105,313 | 96,435 | 86,907 | |
| Mean | 121.7 | 134.6 | 139.5 | 140.7 | 157.2 | 146.4 | 141.8 | 138.3 | 129.3 | 127.2 | 120.1 | 111.9 | 101.1 | <.001 |
| Standard deviation | 151.6 | 179.6 | 181.2 | 172.3 | 201.4 | 193.3 | 188.9 | 180.6 | 171.3 | 174.0 | 163.6 | 157.1 | 131.9 | |
| Median | 65 | 70 | 72 | 81 | 83 | 80 | 74 | 72 | 64 | 65 | 60 | 50 | 50 | <.001 |
| Interquartile range | 14–173 | 16–183 | 17–199 | 16–201 | 15–219 | 17–202 | 17–191 | 18–184 | 15–173 | 13–175 | 10–160 | 10–148 | 11–134 | |
| Market concentration | ||||||||||||||
| Top decile | ||||||||||||||
| Patients (%) | 42,830 (39.0) | 48,786 (40.3) | 49,826 (39.4) | 84,486 (38.5) | 56,321 (40.6) | 52,426 (41.0) | 51,501 (41.6) | 49,418 (40.9) | 47,460 (41.8) | 46,430 (42.0) | 44,502 (42.3) | 41,913 (43.5) | 36,056 (41.5) | <.001 |
| Hospitals | 90 | 90 | 90 | 89 | 88 | 87 | 87 | 87 | 87 | 87 | 87 | 85 | 86 | |
| Top quartile | ||||||||||||||
| Patients (%) | 75,621 (68.8) | 83,550 (69.0) | 87,196 (69.0) | 85,261 (67.6) | 96,840 (69.8) | 88,539 (69.2) | 86,295 (69.8) | 83,766 (69.4) | 79,643 (70.1) | 78,206 (70.7) | 74,762 (71.0) | 69,180 (71.7) | 61,859 (71.2) | <.001 |
| Hospitals | 227 | 225 | 227 | 224 | 221 | 218 | 218 | 218 | 219 | 217 | 218 | 215 | 216 |
Figure 3 shows the use of hysterectomy based on hospital and regional characteristics. In 2010, non-teaching hospitals performed 83,479 fewer hysterectomies than in 1998, whereas teaching hospitals performed 25,422 fewer cases (P<.001). The percentage of hysterectomies performed at teaching hospitals increased from 43.2% in 1998 to 48.3% in 2010. The number of hysterectomies performed decreased at hospitals regardless of size. Between 2002 and 2010, the number of hysterectomies performed decreased in the northeast (−19,830 cases [−20.3%]), midwest (−58,634 cases [236.2%]), and west (−46,626 [−33.3%]), but the greatest reduction was in the south (−122,523 [−43.5%]). In a series of sensitivity analyses in which the cohort was limited to just those women who underwent hysterectomy for leiomyomas, our findings were largely unchanged.
Fig. 3.
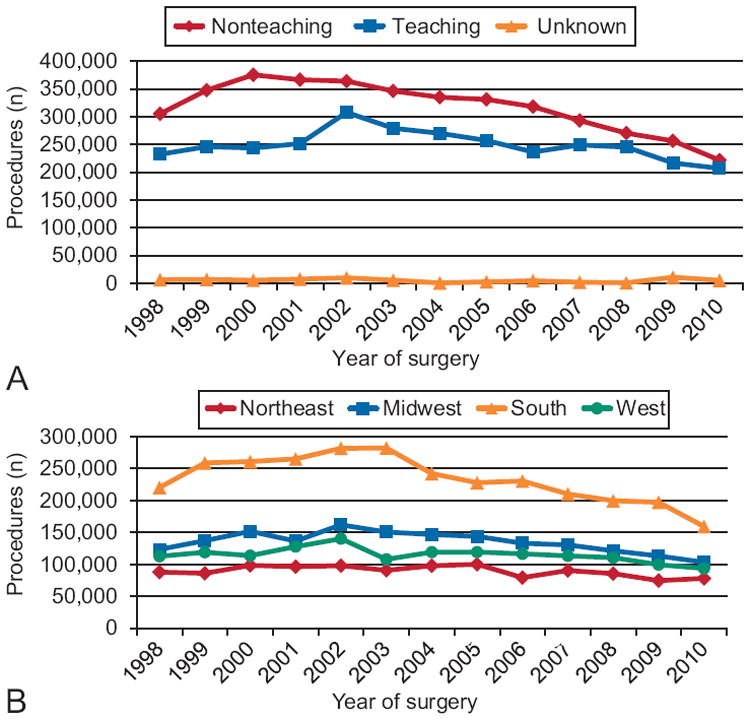
A. Hysterectomies (n) performed each year stratified by hospital teaching status. B. Procedures performed each year stratified by hospital location.
Wright. Trends in Use of Inpatient Hysterectomy. Obstet Gynecol 2013.
DISCUSSION
These data suggest that the number of inpatient hysterectomies performed in the United States has declined substantially with nearly one-fourth of a million fewer procedures in 2010 than 2002. There has been minimal market concentration for hysterectomy with a resultant decrease of more than 40% in the median number of procedures performed per hospital.
A number of factors have likely contributed to the substantial decline in the number of inpatient hysterectomies. Perhaps most importantly, a number of less invasive alternatives to hysterectomy have diffused into practice over the past decade for benign gynecologic disease.6-8,10,22-27 Uterine artery embolization is now frequently used for symptomatic uterine leiomyomas and is associated with satisfaction rates similar to hysterectomy and a quicker return to normal activities.7 Similarly, endometrial ablation is a less invasive alternative to hysterectomy for symptomatic vaginal bleeding.6,8,23-27 Over a relatively short period of time, the number of hysterectomies performed for uterine leiomyomata and genital tract bleeding has dropped substantially.
Although uterine-sparing surgical options have been introduced for many gynecologic disorders, there has also been a general trend toward more conservative, nonsurgical management for a number of diseases. Hormonal therapy is frequently used for abnormal bleeding.9,28 Increased evidence is now available for numerous pharmacologic interventions for the treatment of endometriosis-related pain, including oral contraceptives, gonadotropin-releasing hormone agonists, tranexamic acid, nonsteroidal anti-inflammatory drugs, progestins, androgen derivatives, and several alternative medicine approaches.5,29-33 Finally, there is growing evidence that many ovarian cysts are low risk for malignancy and can safely be monitored by ultrasonography.4,34
An important consideration in the current analysis is that the Nationwide Inpatient Sample does not capture same-day surgery and, as a result, patients discharged on the day of surgery were not included. Our findings thus represent inpatient hysterectomies. This likely led to some underestimation of the number of hysterectomies performed, particularly for laparoscopic and robotic procedures. Nonetheless, the Nationwide Inpatient Sample represents one of the only data sources that allows extrapolation of population-level procedural trends in the United States and provides valuable data regarding the patterns of care of women.
Along with the rapid decline in the rate of hysterectomy, we noted a marked reduction in the average hospital case volume for the procedure. Over the past decade, there has been a general trend toward increasing hospital procedural volume for high-risk surgical procedures. This trend has predominantly been observed for procedures with a strong association between outcomes and surgical volume.2 The hospital-level trends for hysterectomy have been similar to coronary artery bypass graft, also a procedure that has seen a rapid decline in use over the past decade. In a report of Medicare beneficiaries, Birkmeyer and colleagues2 noted that the median hospital volume of coronary artery bypass graft decreased from 244 cases in 1999–2000 to 130 procedures in 2007–2008. From 2002 to 2010, the median hospital hysterectomy volume decreased by more than 40%. Although the relationship between volume and outcome for hysterectomy is less robust than for more high-risk procedures, decreasing hospital volume may have important implications for quality and resource use.17,19,35
Despite the inclusion of a large cohort of patients, we recognize a number of important limitations. In the Nationwide Inpatient Sample, classification of hysterectomy is based solely on ICD-9-CM coding and, therefore, we cannot exclude the possibility that the type of procedure performed was miscoded in a small number of women. Because new procedures are introduced, there is a lag before the introduction of an ICD-9-CM code. Although it is likely that a small number of laparoscopic and robotic procedures was incorrectly classified before the introduction of a claims code, this misclassification would have minimal effect given the large sample. Likewise, we lack data on clinical characteristics likely to influence the route of surgery, including prior surgical procedures, pathology, patient health factors, and other uterine factors. The Nationwide Inpatient Sample lacks data on longitudinal follow-up. As such, we lack data on whether a woman had previously undergone hysterectomy and are unable to calculate age-specific rates of hysterectomy. This has important implications with the aging of the population and the increase in the number of elderly women.
If the total number of hysterectomies, including both inpatient and outpatient procedures, falls significantly, this could result in an adverse effect on resident training, which has already become increasingly challenging given the number of modalities now available to perform hysterectomy. A recent survey found that 58% of graduating residents were “completely prepared” to perform an abdominal hysterectomy compared with only 28% for vaginal, 22% for laparoscopic, and 3% for robotic hysterectomy.36 A large number of residents are now obtaining postresidency training in minimally invasive surgery as well as other gynecologic subspecialties. Improved surgical simulation systems may partially compensate for decreasing teaching volume as well.
These trends also have important implications for practicing gynecologists. As with hospital volumes, if the overall hysterectomy rate is declining, it will be associated with lower physician case volumes. A study of laparoscopic hysterectomy found that 39% of women who underwent surgery between 2000 and 2006 were treated by a low-volume surgeon compared with greater than 50% from 2007 to 2010.17 With fewer available procedures, some gynecologists may alter their practice patterns and refer even uncomplicated procedures to other health care providers. Based on these data, the decline in the hysterectomy rate appears to be continuing and, as such, these trends will likely have an important influence on the practice of gynecology going forward.
Acknowledgments
Dr. Wright (NCI R01CA169121-01A1) and Dr. Hershman (NCI R01CA134964) are recipients of grants from the National Cancer Institute. Dr. Tsui is the recipient of a fellowship from the National Cancer Institute (T32 CA09529).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
References
- 1.Wu JM, Wechter ME, Geller EJ, Nguyen TV, Visco AG. Hysterectomy rates in the United States, 2003. Obstet Gynecol. 2007;110:1091–5. doi: 10.1097/01.AOG.0000285997.38553.4b. [DOI] [PubMed] [Google Scholar]
- 2.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med. 2011;364:2128–37. doi: 10.1056/NEJMsa1010705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birkmeyer JD, Siewers AE, Finlayson EV, Stukel TA, Lucas FL, Batista I, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–37. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 4.Modesitt SC, Pavlik EJ, Ueland FR, DePriest PD, Kryscio RJ, van Nagell JR., Jr Risk of malignancy in unilocular ovarian cystic tumors less than 10 centimeters in diameter. Obstet Gynecol. 2003;102:594–9. doi: 10.1016/s0029-7844(03)00670-7. [DOI] [PubMed] [Google Scholar]
- 5.Streuli I, de Ziegler D, Santulli P, Marcellin L, Borghese B, Batteux F, et al. An update on the pharmacological management of endometriosis. Expert Opin Pharmacother. 2013;14:291–305. doi: 10.1517/14656566.2013.767334. [DOI] [PubMed] [Google Scholar]
- 6.Cooper KG, Bain C, Parkin DE. Comparison of microwave endometrial ablation and transcervical resection of the endometrium for treatment of heavy menstrual loss: a randomised trial. Lancet. 1999;354:1859–63. doi: 10.1016/S0140-6736(99)04101-X. [DOI] [PubMed] [Google Scholar]
- 7.Gupta JK, Sinha A, Lumsden MA, Hickey M. Uterine artery embolization for symptomatic uterine fibroids. The Cochrane Database of Systematic Reviews. 2012;(5) doi: 10.1002/14651858.CD005073.pub3. Art. No.: CD005073. [DOI] [PubMed] [Google Scholar]
- 8.Lethaby A, Hickey M, Garry R, Penninx J. Endometrial resection/ablation techniques for heavy menstrual bleeding. The Cochrane Database of Systematic Reviews. 2009;(4) doi: 10.1002/14651858.CD001501.pub3. Art. No.: CD001501. [DOI] [PubMed] [Google Scholar]
- 9.Lethaby AE, Cooke I, Rees M. Progesterone or progestogen-releasing intrauterine systems for heavy menstrual bleeding. The Cochrane Database of Systematic Reviews. 2005;(4) doi: 10.1002/14651858.CD002126.pub2. Art. No.: CD002126. [DOI] [PubMed] [Google Scholar]
- 10.Moss JG, Cooper KG, Khaund A, Murray LS, Murray GD, Wu O, et al. Randomised comparison of uterine artery embolisation (UAE) with surgical treatment in patients with symptomatic uterine fibroids (REST trial): 5-year results. BJOG. 2011;118:936–44. doi: 10.1111/j.1471-0528.2011.02952.x. [DOI] [PubMed] [Google Scholar]
- 11.Wright JD, Shah M, Mathew L, Burke WM, Culhane J, Goldman N, et al. Fertility preservation in young women with epithelial ovarian cancer. Cancer. 2009;115:4118–26. doi: 10.1002/cncr.24461. [DOI] [PubMed] [Google Scholar]
- 12.Rob L, Skapa P, Robova H. Fertility-sparing surgery in patients with cervical cancer. Lancet Oncol. 2011;12:192–200. doi: 10.1016/S1470-2045(10)70084-X. [DOI] [PubMed] [Google Scholar]
- 13.Wright JD, Burke WM, Wilde ET, Lewin SN, Charles AS, Kim JH, et al. Comparative effectiveness of robotic versus laparoscopic hysterectomy for endometrial cancer. J Clin Oncol. 2012;30:783–91. doi: 10.1200/JCO.2011.36.7508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarlos D, Kots LA. Robotic versus laparoscopic hysterectomy: a review of recent comparative studies. Curr Opin Obstet Gynecol. 2011;23:283–8. doi: 10.1097/GCO.0b013e328348a26e. [DOI] [PubMed] [Google Scholar]
- 15.Wright JD, Neugut AI, Wilde ET, Buono DL, Tsai WY, Hershman DL. Use and benefits of laparoscopic hysterectomy for stage I endometrial cancer among medicare beneficiaries. J Oncol Pract. 2012;8:e89–99. doi: 10.1200/JOP.2011.000484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nationwide Inpatient Sample (NIS) Healthcare Cost and Utilization Project (HCUP) Rockville (MD): Agency for Healthcare Research and Quality; 2007–2009. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Retrieved November 6, 2009. [PubMed] [Google Scholar]
- 17.Wallenstein MR, Ananth CV, Kim JH, Burke WM, Hershman DL, Lewin SN, et al. Effect of surgical volume on outcomes for laparoscopic hysterectomy for benign indications. Obstet Gynecol. 2012;119:709–16. doi: 10.1097/AOG.0b013e318248f7a8. [DOI] [PubMed] [Google Scholar]
- 18.Rogo-Gupta L, Rodriguez LV, Litwin MS, Herzog TJ, Neugut AI, Lu YS, et al. Trends in surgical mesh use for pelvic organ prolapse from 2000 to 2010. Obstet Gynecol. 2012;120:1105–15. doi: 10.1097/aog.0b013e31826ebcc2. [DOI] [PubMed] [Google Scholar]
- 19.Rogo-Gupta LJ, Lewin SN, Kim JH, Burke WM, Sun X, Herzog TJ, et al. The effect of surgeon volume on outcomes and resource use for vaginal hysterectomy. Obstet Gynecol. 2010;116:1341–7. doi: 10.1097/AOG.0b013e3181fca8c5. [DOI] [PubMed] [Google Scholar]
- 20.van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 21.Healthcare Cost and Utilization Project (HCUP) On-line Tutorial Series. Available at: http://www.hcup-us.ahrq.gov/tech_assist/tutorials.jsp. Retrieved February 12, 2013.
- 22.van der Kooij SM, Hehenkamp WJ, Volkers NA, Birnie E, Ankum WM, Reekers JA. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 5-year outcome from the randomized EMMY trial. Am J Obstet Gynecol. 2010;203:105.e1–13. doi: 10.1016/j.ajog.2010.01.049. [DOI] [PubMed] [Google Scholar]
- 23.Meyer WR, Walsh BW, Grainger DA, Peacock LM, Loffer FD, Steege JF. Thermal balloon and rollerball ablation to treat menorrhagia: a multicenter comparison. Obstet Gynecol. 1998;92:98–103. doi: 10.1016/s0029-7844(98)00141-0. [DOI] [PubMed] [Google Scholar]
- 24.Sambrook AM, Bain C, Parkin DE, Cooper KG. A randomised comparison of microwave endometrial ablation with transcervical resection of the endometrium: follow up at a minimum of 10 years. BJOG. 2009;116:1033–7. doi: 10.1111/j.1471-0528.2009.02201.x. [DOI] [PubMed] [Google Scholar]
- 25.Kleijn JH, Engels R, Bourdrez P, Mol BW, Bongers MY. Five-year follow up of a randomised controlled trial comparing NovaSure and ThermaChoice endometrial ablation. BJOG. 2008;115:193–8. doi: 10.1111/j.1471-0528.2007.01427.x. [DOI] [PubMed] [Google Scholar]
- 26.Bhattacharya S, Cameron IM, Parkin DE, Abramovich DR, Mollison J, Pinion SB, et al. A pragmatic randomised comparison of transcervical resection of the endometrium with endo-metrial laser ablation for the treatment of menorrhagia. Br J Obstet Gynaecol. 1997;104:601–7. doi: 10.1111/j.1471-0528.1997.tb11540.x. [DOI] [PubMed] [Google Scholar]
- 27.Middleton LJ, Champaneria R, Daniels JP, Bhattacharya S, Cooper KG, Hilken NH, et al. Hysterectomy, endometrial destruction, and levonorgestrel releasing intrauterine system (Mirena) for heavy menstrual bleeding: systematic review and meta-analysis of data from individual patients. BMJ. 2010;341:c3929. doi: 10.1136/bmj.c3929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gupta J, Kai J, Middleton L, Pattison H, Gray R, Daniels J. Levonorgestrel intrauterine system versus medical therapy for menorrhagia. N Engl J Med. 2013;368:128–37. doi: 10.1056/NEJMoa1204724. [DOI] [PubMed] [Google Scholar]
- 29.Brown J, Pan A, Hart RJ. Gonadotrophin-releasing hormone analogues for pain associated with endometriosis. The Cochrane Database of Systematic Reviews. 2010;(12) doi: 10.1002/14651858.CD008475.pub2. Art. No.: CD008475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu X, Hamilton KD, McNicol ED. Acupuncture for pain in endometriosis. The Cochrane Database of Systematic Reviews. 2011;(9) doi: 10.1002/14651858.CD007864.pub2. Art. No.: CD007864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Flower A, Liu JP, Chen S, Lewith G, Little P. Chinese herbal medicine for endometriosis. The Cochrane Database of Systematic Reviews. 2009;(3) doi: 10.1002/14651858.CD006568.pub2. Art. No.: CD006568. [DOI] [PubMed] [Google Scholar]
- 32.Allen C, Hopewell S, Prentice A, Gregory D. Nonsteroidal anti-inflammatory drugs for pain in women with endometriosis. The Cochrane Database of Systematic Reviews. 2009;(2) doi: 10.1002/14651858.CD004753.pub3. Art. No.: CD004753. [DOI] [PubMed] [Google Scholar]
- 33.Selak V, Farquhar C, Prentice A, Singla A. Danazol for pelvic pain associated with endometriosis. The Cochrane Database of Systematic Reviews. 2007;(4) doi: 10.1002/14651858.CD000068.pub2. Art. No.: CD000068. [DOI] [PubMed] [Google Scholar]
- 34.McDonald JM, Modesitt SC. The incidental postmenopausal adnexal mass. Clin Obstet Gynecol. 2006;49:506–16. doi: 10.1097/00003081-200609000-00010. [DOI] [PubMed] [Google Scholar]
- 35.Wright JD, Herzog TJ, Siddiq Z, Arend R, Neugut AI, Burke WM, et al. Failure to rescue as a source of variation in hospital mortality for ovarian cancer. J Clin Oncol. 2012;30:3976–82. doi: 10.1200/JCO.2012.43.2906. [DOI] [PubMed] [Google Scholar]
- 36.Burkett D, Horwitz J, Kennedy V, Murphy D, Graziano S, Kenton K. Assessing current trends in resident hysterectomy training. Female Pelvic Med Reconstr Surg. 2011;17:210–4. doi: 10.1097/SPV.0b013e3182309a22. [DOI] [PubMed] [Google Scholar]


