Abstract
Secondary systemic vasculitis and nonbacterial endocarditis are rare events. We report a case presented with different manifestations of underlying malignancy such as systemic vasculitis, non bacterial endocarditis and DIC (disseminated intravascular coagulopathy). Efforts to find the source of malignancy was unsuccessful and due to patient's unwillingness for further evaluation, finally under the diagnosis of metastatic disease of unknown primary, patient is receiving cyclic chemotherapy.
Keywords: Systemic vasculitis, Marantic endocarditis
INTRODUCTION
Vasculitis is a clinicopathologic process characterized by inflammation of and damage to blood vessels. A broad and heterogeneous group of syndromes may result from this process, since any type, size, and location of blood vessel may be involved. Vasculitis and its consequences may be the primary or sole manifestation of a disease; alternatively, vasculitis may be a secondary component of another primary disease like infection, malignancy and rheumatic disease.1, 2, 3, 4, 5 Beside systemic vasculitis, non bacterial thrombotic endocarditis (NBTE) could be a paraneoplastic manifestation of malignancy too.9, 10, 11 The cardiac conditions most commonly resulting in NBTE are mitral regurgitation, aortic stenosis, aortic regurgitation, ventricular septal defects, and complex congenital heart disease. NBTE also arises as a result of a hypercoagulable state; this phenomenon gives rise to the clinical entity of marantic endocarditis (uninfected vegetations seen in patients with malignancy and chronic diseases) and to bland vegetations complicating systemic lupus erythematosus and the antiphospholipid antibody syndrome.12, 13, 14, 15 This topic is about systemic vasculitis and marantic endocardititis as manifestations of underlying malignancy.
CASE PRESENTATION
The patient is 34 y/o man presented with episodic painless purple discoloration and linear ungual hemorrhage of fingers and toes, associated with paresthesia since a month ago. He suffered from difficult walking due to progressive weakness in both lower limbs. He also experienced two episodes of amaurosis fugax in both eyes.
He reported occasionally fever without any special pattern. He also complained of 10-15 mins morning stiffness and 4 kg weight loss during previous month. He also experienced exertional dyspnea and dry cough since 2 weeks ago.
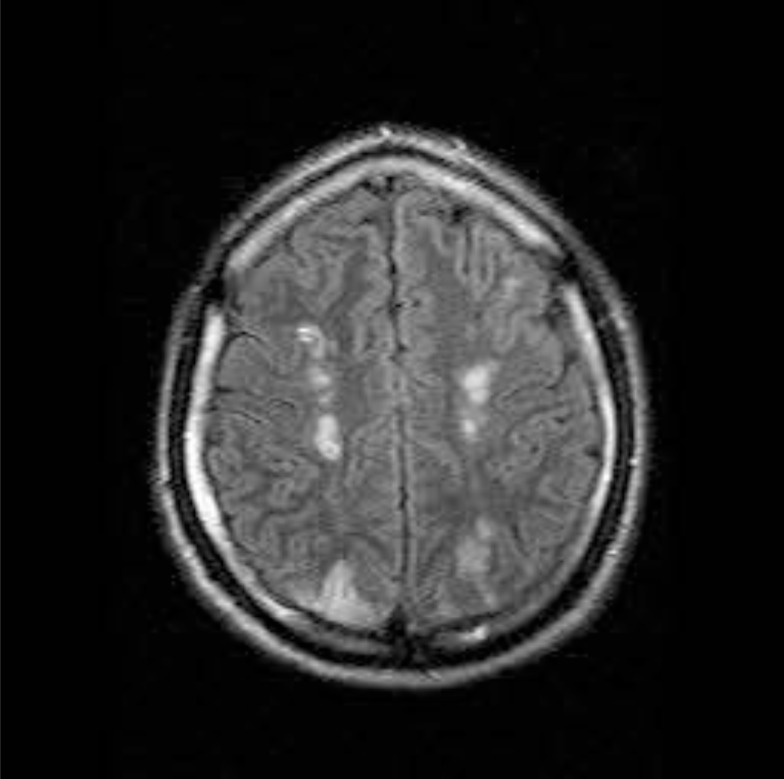
He had a few episodes of vertigo and because of the following symptoms he went to neurologist. Brain MRI which was done (Figure 1) and the patient was referred to rheumatologist for more evaluation.
Figure 1.
MRI findings were: Multiple hyper signal lesions in periventricular and subcortical with involvement of subcortical Mfibers in parietal lobe, preserving basal gangelia, thalamus and corpus callosum, the possibility of demyelinating disease should be considered
He had history of left eye amblyopia since childhood, lumbar disc herniation 10 years ago and unilateral varicocele surgery last year. He took no medications and he did not smoke or use illicit drugs. He was married and worked as a salesman.
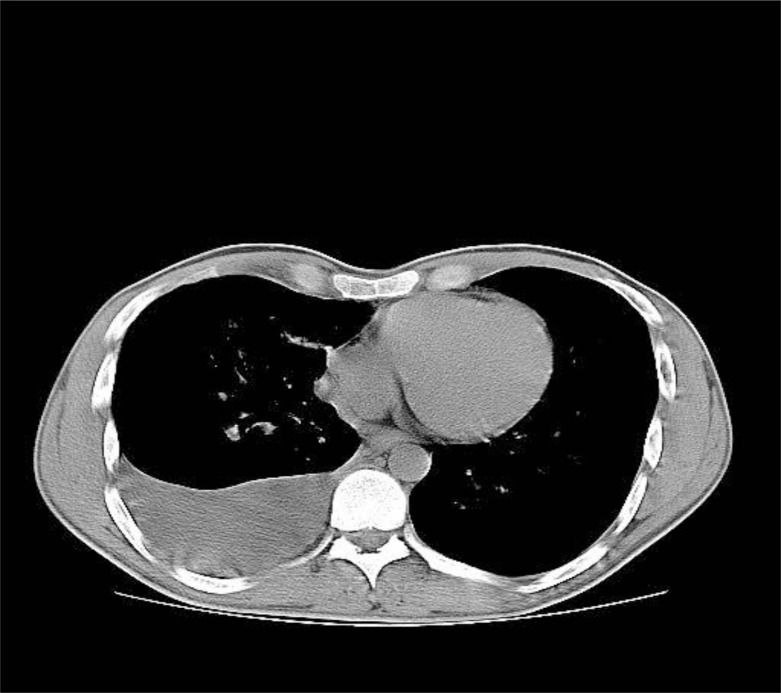
On examination, BP: 115/70, PR: 76/min, T: 37.2 oral, RR: 16/min. Subungual hemorrhage was seen in nearly all fingers plus a purple patch on the left sole. Muscle force, DTR and the remainder of examinations were normal. TTE was done before admission and was normal. A complete blood count and results of liver function tests were normal as were plasma levels of electrolytes, ESR and CRP. Serum Creatinin level was 1.6mg/dl and urine analysis revealed proteinuria and hematuria (Table 1). Under the clinical suspicion of systemic vasculitis, methylprednisolone and cyclophosphamide were administered and patient was scheduled for renal biopsy. Chest CT scan was done and right sided pleural effusion with multiple small nodules in right lung parenchyma was seen (Figure 2). Pleural fluid analysis was exudative (Table 2), so imipenem and ciprofloxacin were started and because of the possibility of underlying malignancy, cytologic analysis of pleural fluid was requested.
Table 1.
Laboratory Results
| WBC | 7.6 | LDH | 2142(u/ml) | ||
| Hb | 13.6 | Total protein | 5.4(mg/dl) | ||
| HCT | 42.5 | CPK | 159(Iu/l) | ||
| Mcv | 82.2 | ESR | <15 | ||
| Plt | 198000 | CRP | 24 | U/A | Prot 2 + |
| Bun | 12(mg/dl) | Wright | - | Blood2 + | |
| Cr | 1.6(mg/dl) | 2ME | - |
Figure 2.
Chest computed tomography showed right side pleural effusion
Table 2.
Pleural Fluid analysis
| Color | Reddish |
| WBC | 5000(segment=40%, lymph=60%) |
| RBC | 70000 |
| Glucose | 105(mg/dl) |
| Protein | 6.4(mg/dl) |
| LDH | 905 |
On the fourth day of admission, he suddenly experiences a very severe right flank pain. U/A and CBC revealed hematuria and leukocytosis (WBC=17500) and abdominopelvic CT scan findings were infracted zones in both kidneys, suggestive for systemic vasculitis or embolic process (Figure 3).
Figure 3.
Abdominopelvic computed tomography showed hypo dense areas suggestive for kidney infarction
Transthorasic echocardiography was repeated and this time a large size mass (12*5 mm) was seen on aortic valve that was suggestive for vegetation, so antibiotics were changed to cefazoline, ampicillin and gentamycin. During the next days Hemoglobin level dropped to 11.3gr/dl and due to thrombocytopenia and abnormal coagulation tests and fragmented RBCs in peripheral blood smear, subclinical DIC was suggested and FFP and packed cell were transfused and renal biopsy was canceled.
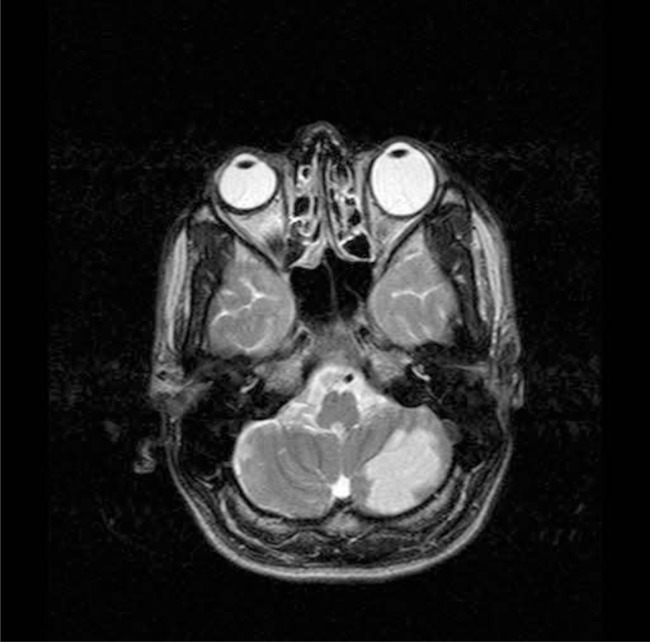
Two days later right hemi paresis was evolved and on examination right hemiparesia without any sphinctral dysfunction or sensory abnormality was detected. This time Brain MRI revealed evidence of one hyper signal lesion in left hemisphere of cerebellum (Figure 4).
Figure 4.
Brain MRI showed a hyper signal lesion in left hemisphere of cerebellum
Transesophageal echocardiography confirmed Aortic vegetation on RCC (7*5mm). On suspicion of underlying malignancy, whole body bone scan was done and findings were increased uptake in posterior ribs and spine, suggestive for metastasis. BMA and BMB were done and normal. Result of cytologic examination on pleural fluid revealed severe mesothelial hyperplasia with cytologic atypia and IHC report was suggestive for Adenocarcinoma with suspected origin of upper GI, pancreas or testis and lung and colon were low likely (negative for TTF 1 and positive for CK 7). At first, patient was candidate for VATS (video assisted thoracic surgery) but due to IHC report and patient unwillingness, VATS was canceled and searching for other sources of metastasis was started. During the admission, because of worsened dyspnea and orthopnea and exudative pleural fluid, chest tube was inserted.
Upper GI endoscopy and biopsy revealed mild anthral gastritis. The results of serum tumor markers were BhCG <1 u/l (normal<10), AFP=3.5Iu/ml (normal=0-10), PSA=0.2ng/ml (normal=upto4), CA19-9=66.9u/ml (normal=0-36), CEA=5.8ng/ml (normal=non smoker < 3.4). Ultrasound of both testicles was normal and abdominopelvic CT was unremarkable for malignancy.
Finally under the diagnosis of metastatis of unknown primary, chemotherapy regimen (Gemcitabin, oxaliplatin, paclitaxel) were administered. Patient had been feeling better after starting therapy and after a few sessions of physiotherapy, he was able to walk. Patient is now doing well and received two chemotherapy periods.
Final Diagnosis
Metastasis disease of unknown primary
DISCUSSION
The patient was presented with multi organ involvement such as skin, brain and kidney that was suggestive of systemic disease. As we discussed below, the main possible diagnosis was overlapping of systemic vasculitis and endocarditis and it's embolic complications, as manifestations of underlying malignancy.
Systemic vasculitis is in two categories; primary or secondary,1, 2 but in our patient, due to negative results of rheumatologic panel, secondary vasculitis associated with primary diseases like malignancy or infection was more compatible with the patient.
Vasculitis can be associated with certain malignancies, particularly lymphoid or reticuloendothelial neoplasms. Leukocytoclastic venulitis confined to the skin is the most common finding; however, widespread systemic vasculitis may occur but it is an uncommon presentation.2
Exudative pleural effusion with positive cytology made this hypothesis more prominent and led us searching for the most common sites of metastatic pleural effusion such as lung carcinoma, breast carcinoma and lymphoma. Due to normal BMA/BMB (bone marrow aspiration and biopsy) and absence of organomegaly or lymphadenopathy, lymphoma was not an appropriate possibility. As IHC report was low likely for lung, being the origin of metastasis, we tried to find other origins such as pancreas, testis and upper GI, but all results were unremarkable for malignancy.
Endocarditis: Our patient suffered from skin lesions that were compatible with janeway and subungual hemorrhage and led us to endocarditis, either bacterial or nonbacterial thrombotic endocarditis (NBTE).6, 7, 8 Cardioembolism is responsible for 20% of ischemic stroke and among the causes of cardioembolism, endocarditis was considered in this patient, responsible for the acute cerebellar stroke and kidney infarctions and due to the size and location of vegetation, NBTE was more compatible with the patient.
Finally due to elevated CA 19-9 and nodularity in right lung, chemotherapy drugs were selected in a way that they could cover pancreas and lung.
REFERENCES
- 1.Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic vasculitides. Arthritis and Rheum. 1994;37:187–192. doi: 10.1002/art.1780370206. [DOI] [PubMed] [Google Scholar]
- 2.Pagnoux C, Cohen P, Guillevin L. Vasculitis secondary to infections. Clin Exp Rheumatol. 2006;24(suppl 2):S71–S81. [PubMed] [Google Scholar]
- 3.Kraemer M, Berlit P. Systemic, secondary and infectious causes for cerebral vasculitis: clinical experience with 16 new European cases. Rheumatol Int. 2009 Oct 13; doi: 10.1007/s00296-009-1172-4. (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 4.Calabrese LH, Duna GF, Lie JT. Vasculitis in the central nervous system. Arthritis Rheum. 1997;40:1189–1201. doi: 10.1002/1529-0131(199707)40:7<1189::AID-ART2>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 5.Minagar A, Fowler M, Harris MK, Jaffe SL. Neurologic presentations of systemic vasculitides. Neurol Clin. 2010;28:171–184. doi: 10.1016/j.ncl.2009.09.015. [DOI] [PubMed] [Google Scholar]
- 6.Asopa S, Patel A, Khan O, Sharma R, Ohri S. Review: non-bacterial thrombotic endocarditis. Eur J Cardio-thorac Surg. 2007;32:696–701. doi: 10.1016/j.ejcts.2007.07.029. [DOI] [PubMed] [Google Scholar]
- 7.Edoute Y, Haim N, Rinkevich D, Brenner B, Reisner S.A. Cardiac valvular vegetations in cancer patients: a prospective echocardiographic study of 200 patients. doi: 10.1016/S0002-9343(96)00457-3. [DOI] [PubMed] [Google Scholar]
- 8.Markides V, Nihoyannopoulos P. Non-bacterial thrombotic endocarditis. Eur J Echocardiogr. 2000;1:291–294. doi: 10.1053/euje.2000.0027. [DOI] [PubMed] [Google Scholar]
- 9.Deitcher SR. Cancer and thrombosis: mechanisms and treatment. J Thromb Thrombolysis. 2003;16(1-2):21–31. doi: 10.1023/B:THRO.0000014589.17314.24. [DOI] [PubMed] [Google Scholar]
- 10.Dvorak HF. Abnormalities of hemostasis in malignant disease. In: Colman RW, Hirsh J, Marder VJ, editors. Hemostasis and Thrombosis. Philadelphia: J. B. Lippincott; 1994. pp. 1238–1254. [Google Scholar]
- 11.Gross L, Friedberg CK. Nonbacterial thrombotic endocarditis, Classification and general description. Arch Intern Med. 1936;58:620–640. [Google Scholar]
- 12.Steiner I. Nonbacterial thrombotic endocarditis--a study of 171 case reports. Cesk Patol. 1993;29(2):58–60. [PubMed] [Google Scholar]
- 13.Bedikian A, Valdivieso M, Luna M, Bodey GP. Nonbacterial thrombotic endocarditis in cancer patients: comparison of characteristics of patients with and without concomitant disseminated intravascular coagulation. Med Pediatr Oncol. 1978;4(2):149–157. doi: 10.1002/mpo.2950040211. [DOI] [PubMed] [Google Scholar]
- 14.Ojeda VJ, Frost F, Mastaglia FL. Non-bacterial thrombotic endocarditis associated with malignant disease: a clinicopathological study of 16 cases. Med J Aust. 1985;142(12):629–631. doi: 10.5694/j.1326-5377.1985.tb113555.x. [DOI] [PubMed] [Google Scholar]
- 15.Kooiker JC, MacLean JM, Sumi SM. Cerebral embolism, marantic endocarditis, and cancer. Arch Neurol. 1976;33(4):260–264. doi: 10.1001/archneur.1976.00500040044006. [DOI] [PubMed] [Google Scholar]