Summary
Over the past few years, obesity has become a major clinical and population concern in the majority of developed countries. Obesity leads to significant systemic disorders, such as hypertension, hypercholesterolemia, hypertriglyceridemia and insulin resistance, and also increases the risk of developing cardiovascular diseases (ischemic heart disease, ischemic stroke), metabolic diseases (type 2 diabetes), certain types of cancer, and degenerative bone disorders (osteoarthritis). Health hazards associated with epidemic of obesity and potential benefits of weight loss have spurred interest in new treatment methods. Bariatric surgical procedures constitute a recognized alternative in cases where conservative management of obesity fails. Several bariatric operations can be distinguished: restrictive procedures, such as adjustable gastric band (AGB) and vertical banded gastroplasty (VBG); predominantly malabsorptive procedures, such as biliopancreatic diversion (BPD), and a combination of both methods, such as Roux-en-Y gastric bypass. The adverse consequences of surgical treatment of obesity include i.a.: intestinal anastomotic leakage, impaired intestinal permeability and internal hernia, dilatation of the stomach, gastrointestinal anastomotic stenosis, marginal ulceration, incisional hernia. Basic knowledge of procedures in the surgical treatment of obesity is of vital importance for the radiologist during evaluation of upper gastrointestinal tract in the early and late postoperative period, allowing correct interpretation of acquired images as well as recognition of typical complications.
Keywords: obesity, bariatric surgery, radiography
Background
Overweight and obesity are nowadays one of the most common health problems in the majority of developed countries. They lead to significant and systemic metabolic disorders e.g. hypertension, hypercholesterolemia, hypertriglyceridemia and insulin resistance. As a consequence, these disorders may lead to ischemic heart disease, brain stroke and type 2 diabetes (with multi-organ complications). Among other consequences, the following should be mentioned: sleep apnea syndrome and severe osteoarthritis. The risk of developing several types of neoplasms (e.g. postmenopausal breast cancer, ovarian cancer, colon cancer) is also higher in obese patients [1,2]. It is estimated that health consequences of obesity are more serious than consequences of tobacco smoking and alcohol consumption [3], whereas treatment of obesity and its comorbidities accounts for about 3–6% of financial expenditures on health protection in developed countries [4]. It was estimated that obesity associated with a BMI greater than 40 kg/m2 reduces life expectancy by an average of 20 years [5].
Conservative treatment of obesity (diet, physical activity, pharmacotherapy) statistically leads to a small (approximately 5–8%) and usually short-term reduction of body weight [6]. Thus, bariatric surgery became an accepted alternative treatment in such cases where a non-surgical approach fails. The aim of this work was to present basic types of bariatric surgical procedures, their most common complications and principles of radiographic imaging.
Epidemiology, Definition and Classification of Obesity
According to the definition accepted by WHO, obesity is a pathological fat accumulation in the human body, exceeding its physiological needs and adaptation abilities, which may have an adverse effect on health. On the other hand, overweight is defined as fat accumulation, exceeding its optimal amount in the human body [7]. Currently, disturbances in body weight regulation are generally classified according to body mass index (BMI), defined as the body weight divided by the square of the height in meters. The range of BMI from 18.5 to 24.9 (kg/m2) means normal weight, from 25 to 29.9 means overweight and ≥30 – obesity. Additionally, according to WHO, obesity is divided into 3 classes (categories) [7]:
Class I – BMI 30.0–34.9;
Class II – BMI 35.0–39.9;
Class III – BMI ≥40.0.
In Poland, approximately 5% of population has a BMI of >35, whereas approximately 1% of population >40 [7]. Morbid obesity (MO) is diagnosed in case of BMI ≥40 or ≥35 with obesity-related comorbidity. From a surgical point of view, there are also: gigantic obesity (BMI >40.0 kg/m2) and super-obesity (BMI >50.0 kg/m2). Factors that influence the development of obesity include i.a.: genetics (e.g. Prader-Willi syndrome, Lurence-Moon-Biedl syndrome, Cohen syndrome, Carpenter syndrome), biological factors (e.g. endocrine disorders in hypothyroidism, Cushing’s syndrome, polycystic ovarian syndrome, growth hormone deficiency, pseudohypoparathyroidism or in hyperinsulinemia), pharmacological factors, namely the use of antidepressants (amitriptyline, doxepin, mirtazapine, mianserin), anxiolytics, neuroleptics (older phenothiazine derivatives as well as new atypical neuroleptics e.g. olanzapine, risperidone), anticonvulsants (valproic acid, carbamazepine), corticosteroids, some beta-adrenolytics and insulin, as well as psychological factors (mood disorders, depression). However, the most porofound influence on obesity development reveal environmental factors associated with the development of civilization and technology. They lead to both reduction of energy expenditures associated with everyday activity and to easy access to high amount of cheap, processed and high-energy food. The situation of excessive energy supply in relation to the requirements of human body (positive energy balance) leads directly to the development of overweight and obesity.
From historical point of view, due to limited access to food before the beginning of the 20th century, obesity was not a widespread disease and occurred especially among representatives of upper social strata. It was not until the last century, especially in its second part, that as a result of civilization and social transformation after the Second World War and technological development, the incidence of obesity started to increase gradually and continuously. In 1997, the World Health Organisation (WHO) announced a global epidemic of obesity [7]. In 2005, experts from WHO estimated that there were 400 million obese people worldwide, which accounted for 9.8% of the world population [6]. Three years later WHO announced that there were more than 500 million obese people worldwide, among them 200 million obese men and 300 million obese women which in total accounted for over 10% of the population [9].
Obesity occurs decidedly more often in developed countries (USA, Western European Countries, Canada, Australia) than in Third World Countries (mainly Africa, Southeast Asia, South and Latin America). Obese people account for 31% of adult population of the USA, whereas pathologically obese for approximately 5% [10]. In England, Germany and Poland, obese people account for approximately 15% of the population [10,11]. According to the National Food and Nutrition Institute data from 2000, overweight was found in 41% of men and in 28.7% of women, whereas obesity was found in 15.7% of men and in 19.9% of women [12]. The WOBASZ survey (2003–2005) found, that the incidence of overweight was 40.4% in men and 27.9% in women; obesity was found in 21.2% of men and in 22.4% of women [13].On the other hand, the NATPOL survey found that overweight affected 34% of adults (39% of men and 29% of women), whereas obesity 19% (19% of men and 19% of women) [14]. The POL MONICA BIS survey from 2001 found that obesity in Poland affected 28% of men and 29% of women [15]. According to the Central Statistical Office data from 1996 and 2004 there were some differences in the distribution of data: in 1996 overweight was found in 12% of women and in 19% of men, obesity in 14% of women and in 10% of men; in 2004 overweight was found in 14% of women and in 20% of men, whereas the percentage of obese people in both of these groups was 13% [16].
The WHO experts estimate that the percentage of overweight and obese people will be still growing in both highly developed and developing countries, reaching even the level of 40% for people with BMI of 30–40 and slightly over 10% for people with morbid obesity [17].
Radiographic Imaging Studies Following Bariatric Surgery
The idea of the application of bariatric surgical procedures appeared during follow-ups of patients after extensive gastric and intestinal resections due to non-bariatric causes, in whom significant weight loss was observed. Pioneering attempts in surgical treatment of obesity, i.e. bariatric surgery, are dated back to the fifties of the 20th century (Kremen and Linner created an anastomosis between the jejunum and the ileum) [17]. In Poland, the first bariatric surgical procedures were performed in the seventies of the 20th century (Payne-DeWind method was used – anastomosis between the jejunum and the colon) [18]. Between 1993 and 2006 in Poland, 2584 different types of bariatric surgical procedures were performed [18]. In the nineties of the 20th century bariatric surgical procedures were performed in Poland in 2 medical centres, whereas in 2008 in as many as 15. Nowadays approximately 65% of all bariatric surgical procedures are performed laparoscopically.
Patients referred to bariatric surgery include adults with permanent class III obesity (BMI ≥40) and adults with class II obesity (BMI ≥35) if obesity-related comorbidities (diabetes, hypertension, ischemic heart disease, obstructive sleep apnea syndrome, severe osteoarthritis) are present [8]. When conservative therapy is ineffective, patient is qualified for surgery. Furthermore, patient must understand the aim and principles of surgical treatment and give informed consent for surgery and postoperative care. The presence of general contraindications to anesthesia and surgery makes the bariatric surgery impossible.
The role of a radiologist in the surgical treatment of obesity consists mainly in evaluation of anatomic conditions immediately after surgery and detection of early and late complications. During the initial evaluation after bariatric surgical procedure it is necessary above all to locate the gastric band (it occurs that the band is installed in front of the stomach, especially during laparoscopic surgery), the volume of the gastric reservoir and the width of its junction with the distal part of the stomach, as well as the continuity of staple line. Radiographic imaging in the early postoperative period is also necessary if early complications occur. The symptoms may include i.a. epigastric pain, persistent discharge from the postoperative wound, food intake difficulty or vomiting – in such cases potential anastomotic leakage, symptoms of an ulcer and features of excessive narrowing of the lumen of the gastrointestinal track (caused by e.g. band installed too tightly or band migration) should be searched for. Examinations in the late postoperative period (usually several months or years after surgery) are often necessary in case of stopping loosing or repeated gain of weight – in such case, above all, it is necessary to evaluate if there is no dehiscence of gastric staple line or loosening of gastric band.
The key role in the evaluation of postoperative changes is played by radiographic imaging because in patients after bariatric surgery it is usually impossible to perform gastroscopy (e.g. due to installed gastric band, which narrows its lumen making passage of the endoscope impossible). Among the most important radiographic imaging procedures there are classic upper gastrointestinal series and gastrointestinal passage examination. The most commonly used is barium sulfate oral suspension due to the best contrasting properties in gastrointestinal tract, absence of adverse reactions, availability and low price. Contraindications of a barium meal include only the early postoperative period in patients with suspected anastomotic leakage – in such situations iodine-based, water-soluble contrast media are used. The examination is performed in a standard way – the passage of contrast medium trough the gastrointestinal tract is observed during fluoroscopy, with patient lying or standing, in AP, diagonal and side-lying position. In some cases, e.g. radiologic features of contrast medium leakage outside the gastrointestinal tract, CT is necessary to confirm the anastomotic leakage and exact location of the leakage point. The use of other radiographic imaging methods for the diagnosis of complications after bariatric surgery is considerably limited. It is theoretically possible during an ultrasound examination to visualize e.g. pathological fluid collections at the operative site, but usually it is impossible to distinguish between postoperative fluid collections and collection due to anastomotic leakage. Several papers describe scintigraphy as a good method to evaluate the gastric emptying time after restrictive surgical procedures [19] and to regulate the gastric bands after AGB [20]. There are no reports on the use of MRI in the evaluation of patients after bariatric surgery.
Classification of Bariatric Operations
Over the past 50 years, there were many different bariatric operations developed. According to the basic classification, there are restrictive, malabsorptive and combined procedures (Table 1). The aim of restrictive procedures is to reduce food intake, most often by installation of a gastric band in the cardiac region of the stomach, which (through narrowing of the gastric lumen) makes intake of larger amounts of food impossible. The aim of malabsorptive procedures is to reduce the capabilities of digestion and absorption through creation of the short bowel syndrome. There are also combined procedures which join the benefits of each of the two above-mentioned methods [18,21–23].
Table 1.
Classification of fundamental bariatric procedures.
| Restrictive procedures | Malabsorptive procedures | Combined procedures |
|---|---|---|
| Vertical banded gastroplasty (VBG) | Biliopancreatic diversion (BPD) | Roux en-Y gastric bypass (RYGB) |
| Adjustable gastric banding (AGB) | Duodenal switch with sleeve gastrectomy (DS) | |
| Sleeve gastrectomy (SG) |
Adjustable gastric banding (AGB)
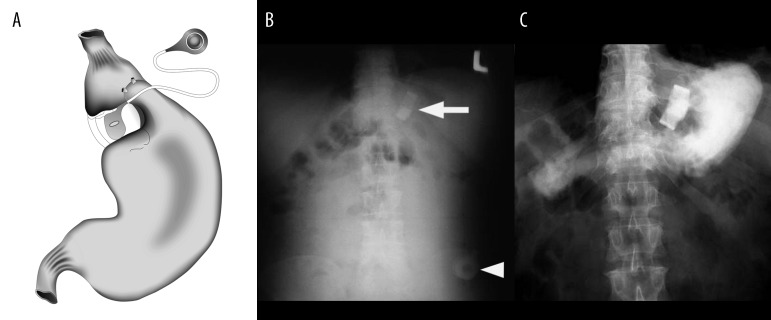
This surgery (most commonly performed laparoscopically) consists of placement of a band below the gastric cardia which is connected to the catheter with a port placed and anchored under the skin on the abdominal wall. The smaller gastric pouch created proximally to the band holds on average 15–20 ml of food, which on the one hand limits the amount of food that can be consumed, and on the other hand leads to early feeling of satiety due to its postprandial dilatation (Figure 1).
Figure 1.
Laparoscopic adjustable gastric banding (AGB): (A) – scheme, based on [18], own modification; (B) – plain abdominal X-Ray after AGB: a radioopaque band is visible at the location of the gastric cardia (arrow), and a port at the left epigastrium (arrowhead), (C) – a barium meal examination shows correct location of gastric band, just below the gastric cardia.
With the aid of the port, via a transcutaneous puncture, the filling of the band can be regulated, influencing the width of the gastric lumen on its level, thus increasing or decreasing the amount of food intake depending on patients’ needs. Establishing the optimal fill volume of the band is easiest during its gradual filling up during fluoroscopy with oral contrast material.
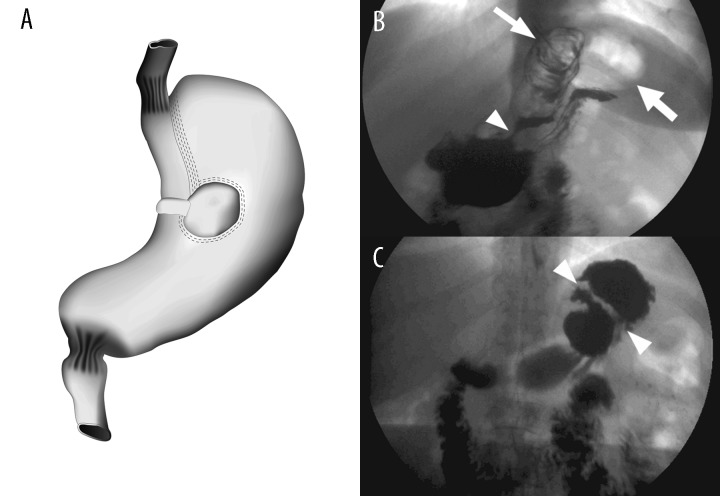
Vertical banded gastroplasty (VGB, Mason procedure)
In Mason procedure, performed via laparoscopy or laparotomy, a „window” between the anterior and posterior gastric wall is created in the area of the lesser curvature of the stomach using the circular stapler; next, a band is placed through the window around the lesser curvature of the stomach and the stomach is partly divided by vertical stapling from the window up to the angle of His. Thus, a small, proximal gastric pouch, approximately 20–30 ml in volume, is created, separated from the gastric fundus with a staple line and from the gastric body with a band narrowing the gastric lumen (Figure 2). The results of Mason procedure and AGB are similar.
Figure 2.
Vertical banded gastroplasty (VBG): (A) – scheme based on [18], own modification; (B) – barium meal examination after Mason’s operation: small proximal gastric pouch (short arrow), gastric lumen narrowing at the location of band (arrowhead, band itself is not visible on X-Ray), and the gastric fundus clearly separated from pouch (thick arrow); (C) – X-Ray of other patient after barium meal highlights correct line of staples (between arrowheads, staples are not visible), separating pouch from the fundus.
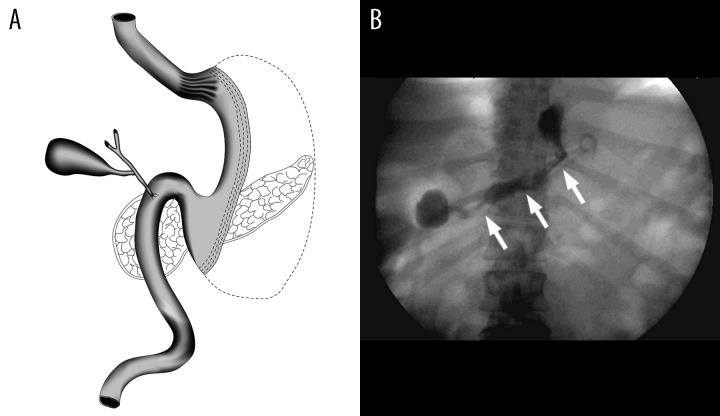
Sleeve gastrectomy (SG)
Sleeve gastrectomy, also known as sleeve gastric resection involves removal of gastric fundus (with an endostapler), larger part of the body of the stomach from the greater curvature side and lower part of the pylorus, leaving a narrow tube along the lesser curvature of the stomach (Figure 3). The created longitudinal pouch is approximately 100–200 ml in volume. This type of surgery is performed in case of complications following AGB and VBG as well as for preparation before more extensive surgery in patients with a very high BMI.
Figure 3.
Sleeve gastrectomy (SG): (A) – scheme based on [18], own modification. (B) – barium meal examination showing narrow, longitudinal tube-like structure, which remains after surgical removal of a large portion of the stomach along the greater curvature (arrows); moreover, a drain is visible at the postoperative space. In this patient sleeve gastrectomy was performed because of complications after Mason’s operation (VBG).
Biliopancreatic diversion (BPD)
This type of surgery is an example of bypass procedures consisting of partial exclusion of gastrointestinal tract from digestion. It involves resection of the distal 2/3 of the stomach with blind closure of the duodenal stump, transection of the small intestine approximately 70–150 mm from the pylorus, anastomosis of the end of the proximal loop to the side of the ileum approximately 50–100 cm from the ileocecal valve and anastomosis of the distal loop with the remaining part of the stomach (Figure 4). Thus, an enzymatic loop is created (duodenum and proximal jejunum), i.e. alimentary loop consisting of the gastric stump and the distal part of the small intestine and a short common channel. The BPD procedure is performed mainly in patients with a BMI greater than 50.
Figure 4.
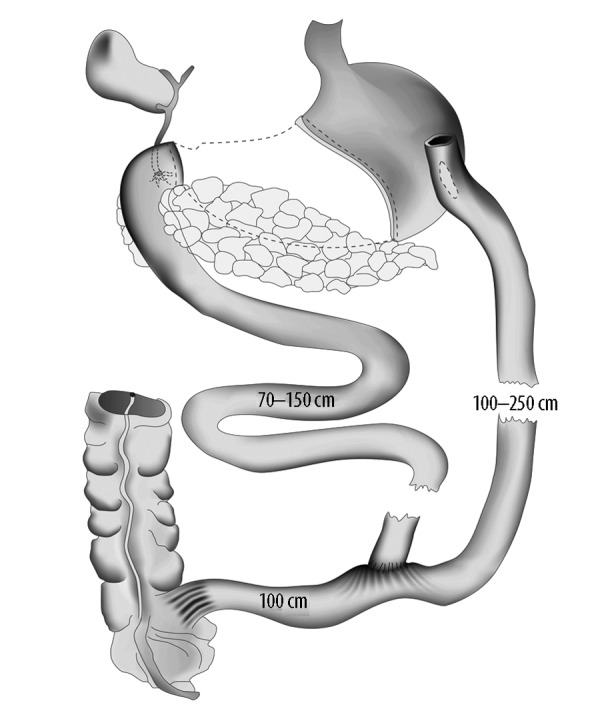
Biliopancreatic diversion (BPD). Scheme based on [18], own modification. Marked intestinal loops: enzymatic loop (70–150 cm), nutritional loop (100–250 cm) and common loop (100 cm proximal to the ileocaecal valve).
Roux-Y gastric bypass
The Roux-Y gastric bypass combines both previously presented restrictive methods limiting the amount of food intake and methods excluding intestinal fragments from digestion and absorption. It involves reduction of the size of the stomach by creating a small pouch below the gastric cardia, its anastomosis with a separated intestinal loop (so-called alimentary loop) and then anastomosis of the enzymatic loop with the alimentary loop approximately 100 cm from the ligament of Treitz (Figure 5). This is the most common bariatric procedure (70% of cases) performed in the USA.
Figure 5.
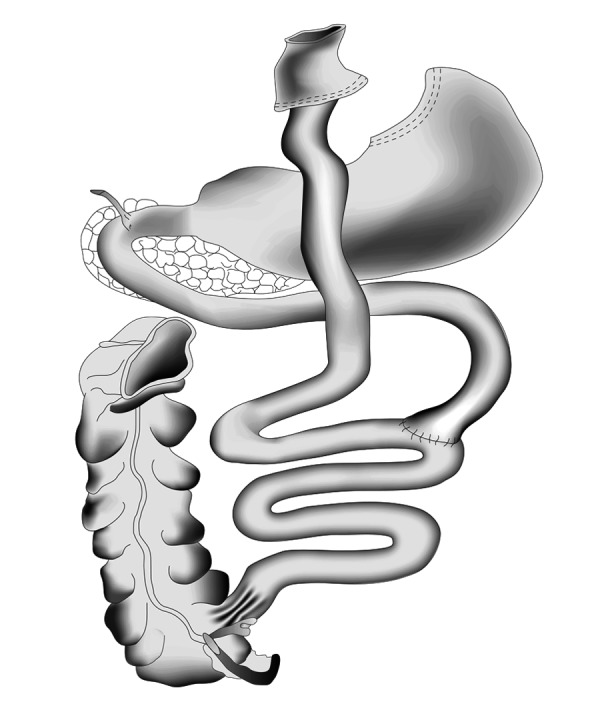
Roux-en-Y gastric bypass (RYGB): scheme based on [18], own modification.
Duodenal switch (DS)
This is the next procedure which combines both restrictive and malabsorptive techniques. It involves a transection of the duodenum at 2–4 cm distally from the pylorus with a stapler and suturing to form a blind-ending stump. Afterwards the sleeve gastrectomy (restrictive component) and the biliopancreatic diversion (malabsorptive component) are performed – Figure 6.
Figure 6.
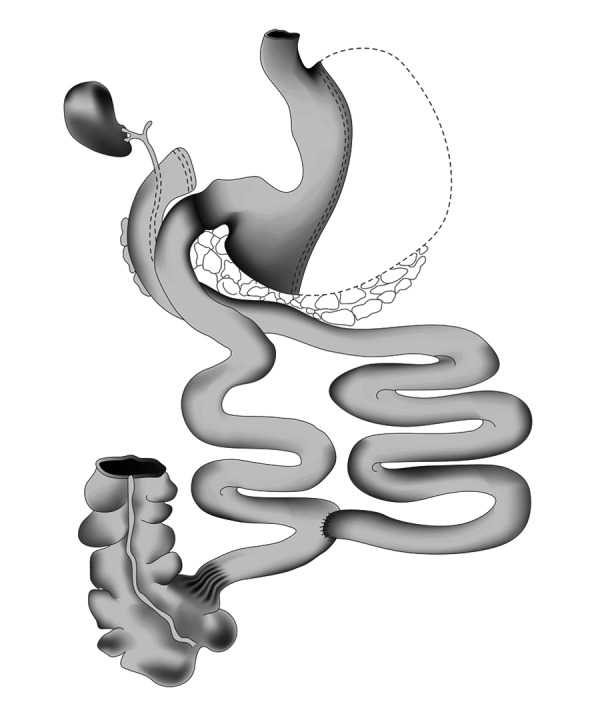
Duodenal switch (DS): scheme based on [18], own modification.
Complications After Bariatric Surgery
Like any other invasive procedure, bariatric surgery is associated with a certain risk of complications. The perioperative mortality is relatively low and is under 1%. Pulmonary embolism is among the most serious postoperative complications, but its diagnostic methods are beyond the scope of this article. Other common complication in the early postoperative period is anastomotic leakage and leakage outside the lumen of the gastrointestinal tract (Figures 7 and 8). Gastric staple line dehiscence (Figure 9), dislocation or other dysfunction of the gastric band (Figure 10), anastomotic stricture and ulcers belong to late complications [21–24]. The most common complications related to particular procedures are shown in Table 2.
Figure 7.

A 29-year-old female patient, a few days after VBG reported epigastric pain and problems with food intake. The examination was performed with water-soluble, iodine-based contrast media. During the first phase of this study (A), which was performed in a supine position, a gastric pouch seemed to be unchanged (arrowheads). After next contrast swallow (B) a leakage from gastric pouch to the left (in the direction of the gastric fundus) is visible (arrows). This picture remained unchanged to the end of the examination, as well as in X-Ray performed several hours later (C, arrow). Irregular shape of contrasted space, lack of well-defined borders and persistence through several hours suggested contrast leakage beyond the gastrointestinal tract. The staple line leakage was confirmed during surgery.
Figure 8.
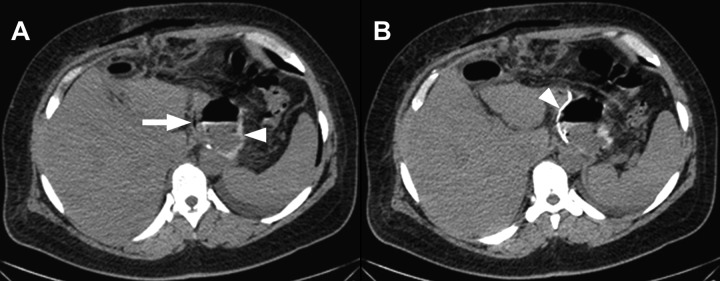
A 46-year-old female patient, who had undergone a sleeve gastrectomy due to complications after VBG. CT was performed to confirm a suspicion of staple line leakage, which was raised after fluoroscopy. To the left of the narrow gastric ‟sleeve” (arrow) there is a space filled by a leaking gastric content (arrowhead) with an air-fluid level and a small amount of contrast medium given orally (A). Hyperdense, linear structure parallel to the lesser curvature corresponds to surgical staples (B, arrowhead). The staple line leakage was confirmed intraoperatively.
Figure 9.

A 32-year-old female patient, who had gone VBG several years earlier, admitted to surgeon because of a re-growth of bodyweight. A radiogram from barium meal examination at slightly oblique projection shows barium leakage (arrow) through the staple line into the gastric fundus. It is a typical appearance of staple line dehiscence.
Figure 10.

Gastric band dysfunction after VBG, resulting in a widening of the outflow from small gastric pouch into the distal part of the stomach. Gastric lumen’s width at the location of band measured 11 mm (between arrowheads) and was comparable to the width of the gastric cardia during its relaxation. A body mass re-growth was clinically observed.
Table 2.
The most common complications of bariatric surgery.
| AGB | VBG | RYGB | BPD, DS, SG |
|---|---|---|---|
| Gastric ulcer | Stenosis at the junction between the upper and lower gastric pouches | Gastrointestinal anastomotic stenosis, leakage or ulceration | Leakage from the resection line of the greater curvature of the stomach |
| Gastric band migration | Dilatation of the canal between the upper and lower gastric pouches | Gastric pouch dilatation | Gastrointestinal or duodenointestinal anastomotic ulceration and leakage |
| Enlargement and overhanging of the proximal gastric pouch | Staple line dehiscence | Postoperative incisional hernia | Postoperative incisional hernia |
| Stomal obstruction | Gastric ulcer and band erosion | Intestinal obstruction secondary to adhesions | |
| Port infection, dislocation or leakage |
Conclusions
With the growing percentage of obese patients in society, the number of patients in whom bariatric procedures are performed will be growing as well. These patients will be more often referred to radiological institutes to undergo postoperative evaluation and to have early as well as late complications diagnosed.
The basis of diagnostic radiological imaging in these patients is the use of a single-contrast examination of the upper gastrointestinal tract and examination of intestinal passage, in particular cases supplemented by computed tomography. The knowledge of basic principles of surgical procedures used in the treatment of obesity has a significant meaning for a radiologist in the evaluation of contrast examinations of the upper gastrointestinal tract in the early and late postoperative period facilitating their correct interpretation as well as making the recognition of typical postoperative complications easier.
References
- 1.Szczeklik A. Choroby wewnętrzne. 1st ed. Wyd. Medycyna Praktyczna; Kraków: 2006. [in Polish] [Google Scholar]
- 2.Buchwald H. Consensus Conference Statement Bariatric surgery for morbid obesity: Health implications for patients, health professionals, and third-party payers. Surg Obes Relat Dis. 2005;1(3):371–81. doi: 10.1016/j.soard.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Zimmet PZ, Alberti KG. Introduction: globalization and the non-communicable disease epidemic. Obesity (Silver Spring) 2006;14:1–3. doi: 10.1038/oby.2006.1. [DOI] [PubMed] [Google Scholar]
- 4.Ackroyd R, Mouiel J, Chevallier JM. Cost-effectiveness and budget impact of obesity surgery in patients with type-2 diabetes in three European countries. Obes Surg. 2006;16:1488–503. doi: 10.1381/096089206778870067. [DOI] [PubMed] [Google Scholar]
- 5.Fontaine KR, Redden DT, Wang C. Years of life lost due to obesity. JAMA. 2003;289(2):187–93. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 6.Pannala R, Kidd M, Modlin IM. Surgery for obesity: panacea or pandora’s box? Dig Surg. 2006;23:1–11. doi: 10.1159/000092800. [DOI] [PubMed] [Google Scholar]
- 7.Obesity, preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:I–XII. 1–253. [PubMed] [Google Scholar]
- 8.Wyleżoł M, Paśnik K, Dąbrowiecki S, et al. Polskie rekomendacje w zakresie chirurgii bariatrycznej. Wideochirurgia i inne techniki małoinwazyjne. 2009;4(Supl.1):S31–S33. [in Polish] [Google Scholar]
- 9.Description of the global burden of NCDs, their risk factors and determinants. Chapter I. World Health Organization; Apr, 2011. Global status report on noncommunicable diseases 2010; pp. 14–16. [Google Scholar]
- 10.Pannala R, Kidd M, Modlin IM. Surgery for obesity: panacea or pandora’s box? Dig Surg. 2006;23:1–11. doi: 10.1159/000092800. [DOI] [PubMed] [Google Scholar]
- 11.Caterson ID, Gill TP. Obesity: epidemiology and possible prevention. Best Prac Res Clin Endocrinol Metab. 2002;16:595–610. doi: 10.1053/beem.2002.0228. [DOI] [PubMed] [Google Scholar]
- 12.Jarosz M. Otyłość, żywienie, aktywność fizyczna, zdrowie Polaków. Diagnoza stanu odżywiania, aktywności fizycznej i żywieniowych czynników ryzyka otyłości oraz przewlekłych chorób niezakaźnych w Polsce (1960–2005) Instytut Żywności i Żywienia; Warszawa: 2006. [in Polish] [Google Scholar]
- 13.Program WOBASZ. Wyd. Vol. 90. Instytut Kardiologii; Warszawa: 2005. Wieloośrodkowe Ogólnopolskie Badanie Stanu Zdrowia Ludności; pp. 1–128. [in Polish] [Google Scholar]
- 14.Zdrojewski T, Babińska Z, Bandosz P. Związek nadwagi i otyłości z podwyższonymi wartościami ciśnienia tętniczego w badaniach reprezentacyjnych grup dorosłych Polaków w 1997 i 2002 roku (NATPOL II, NATPOL III) Med Metab. 2002;6:32. [in Polish] [Google Scholar]
- 15.Rywik S, Pająk A, Broda G, et al. Częstość występowania nadwagi i otyłości w wybranych populacjach Polski – Pol-Monica BIS Projekt. Med Metabol. 2003;2:8–15. [in Polish] [Google Scholar]
- 16.Raport GUS: Stan zdrowia ludności Polski w 2004 r. www.stat.gov.pl/cps/rde/xbcr/gus/stan_zdrowia_2004.pdf. [in Polish]
- 17.Finkelstein EA, Khavjou OA, Thompson H, et al. Obesity and severe obesity forecasts through 2030. Am J Prev Med. 2012;42(6):563–70. doi: 10.1016/j.amepre.2011.10.026. [DOI] [PubMed] [Google Scholar]
- 18.Stanowski E, Paśnik K. Chirurgiczne leczenie otyłości – aktualny stan wiedzy. Wideochirurgia i inne techniki małoinwazyjne. 2008;3(2):71–86. [in Polish] [Google Scholar]
- 19.Hladik P, Vizda J, Mala E, et al. The contribution of gastric emptying scintigraphy to the treatment of obesity with gastric bandage – preliminary results. Biomed Pap Med FacUnivPalacky Olomouc Czech Repub. 2008;152(1):125–28. doi: 10.5507/bp.2008.020. [DOI] [PubMed] [Google Scholar]
- 20.Susmallian S, Filyavich A, Maiershon I, et al. Dynamic Radioisotope Scintigraphy for Gastric Banding Adjustment. Obesity Surgery. 2004;14(4):520–23. doi: 10.1381/096089204323013532. [DOI] [PubMed] [Google Scholar]
- 21.Smith C, Gardiner R, Kubicka R, et al. Dieschbourg: Radiology of gastric restrictive surgery. Radio Graphics. 1985;5:193–216. doi: 10.1148/radiology.153.2.6484161. [DOI] [PubMed] [Google Scholar]
- 22.Scheirey C, Scholz F, Shah F, et al. Radiology of the Laparoscopic Roux-en-Y Gastric Bypass Procedure: Conceptualization and Precise Interpretation of Results. Radio Graphics. 2006;26:1355–71. doi: 10.1148/rg.265055123. [DOI] [PubMed] [Google Scholar]
- 23.Mitchell M, Carabetta J, Shah, et al. Duodenal Switch Gastric Bypass Surgery for Morbid Obesity: Imaging of Postsurgical Anatomy and Postoperative Gastrointestinal Complications. Am J Roentgenol. 2009;193:1576–80. doi: 10.2214/AJR.08.1941. [DOI] [PubMed] [Google Scholar]
- 24.Szydłowski K, Frask A, Michalik M, et al. Powikłania po chirurgicznym leczeniu otyłości w materiale własnym. Wideochirurgia i inne techniki małoinwazyjne. 2008;3(2):45–52. [in Polish] [Google Scholar]