Summary
Kidney transplantation can be associated with various complications that vary from vascular complications to urologic disorders to immunologic adverse effects. In evaluating the recipient with graft dysfunction, clinicians can choose among several imaging modalities, including ultrasonography, nuclear medicine studies, computed tomography, and magnetic resonance imaging. This review discusses the evaluation of the kidney transplant recipient using these imaging procedures, emphasizing the clinical diagnostic utility and role of each modality. A kidney biopsy is often required as a gold standard for diagnostic purposes. However, because of the inherent risks of a kidney biopsy, noninvasive imaging in diagnosing causes of graft dysfunction is a highly desired tool used and needed by the transplant community. Because the diagnostic accuracy varies depending on the time course and nature of the transplant-related complication, this review also addresses the advantages and limitations of each modality. The recent advances in kidney transplant imaging techniques and their clinical implications are also discussed.
Introduction
Kidney transplant dysfunction can present with a rising serum creatinine level, decreasing urine output, and pain and tenderness over the graft, but often it is clinically asymptomatic and presents only with an isolated increase in serum creatinine. Imaging modalities to work up graft dysfunction include ultrasonography (US), computed tomography (CT), nuclear medicine (NM) or molecular imaging, and magnetic resonance imaging (MRI). The timeline in Figure 1 serves as a useful guide to expected complications after transplantation. Table 1 describes imaging modality preferences in common post-transplant complications.
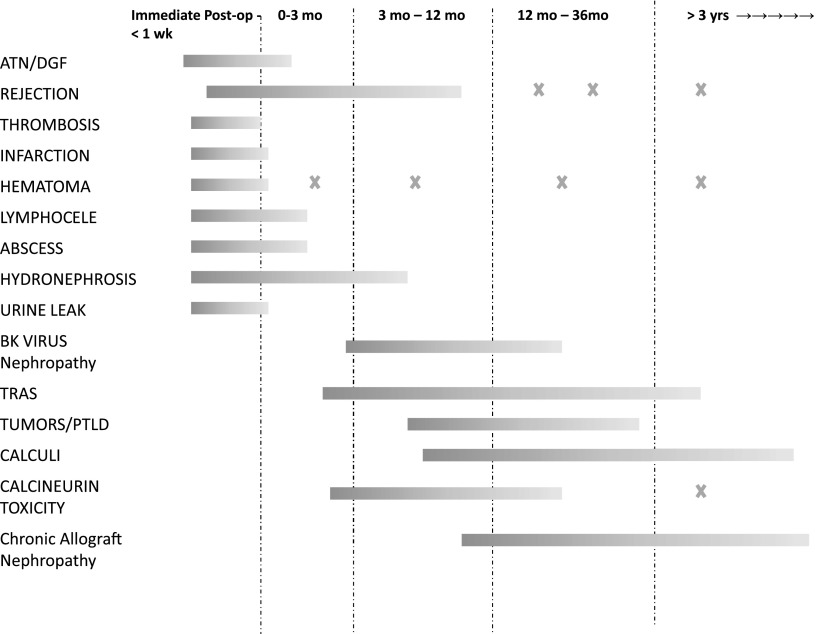
Figure 1.
Timeline of post-transplant complications based on most likely occurrence periods. Certain complications can occur at any time after transplantation, whereas others are related to procedures such as biopsy. For example, hematomas may occur after a biopsy even years after transplant. Please refer to text for further details. ATN, acute tubular necrosis; PTLD, post-transplant lymphoproliferative disorder; TRAS, transplant renal artery stenosis.
Table 1.
Imaging modality preferences in common post-transplant complications
| Variable | Color Doppler Ultrasonography | Computed Tomography | Magnetic Resonance Imaging | Nuclear Medicine Imaging | Digital Subtraction Angiography |
| Immediate postoperative graft dysfunction/ATN | Preferred test to establish vascular flowa Strengths: Noninvasive; quick; portable; detailed information on arterial and venous anatomy, flow, velocity. Rules out hydronephrosis and detects early large perinephric collections. Weakness: User-dependant; technical limitations may obscure vasculature |
Not used to establish DGF/ATN Strengths: Can detect other intra-abdominal catastrophes Weakness: Risk of contrast nephropathy due to contrast agents in early postoperative period limits vascular evaluation |
Not used to establish flow Strengths: None Weakness: Lack of contrast agent in early postoperative period limits vascular evaluation |
Preferred test to establish flowa Strengths: Uptake establishes flow; may diagnose leaks Weakness: Not easily available, time consuming, expensive |
Not used |
| Urinary tract obstruction | Preferred test Strengths: Can be serially followed for resolution, grade severity Weakness: Cannot differentiate functional obstruction from chronic dilatation |
Strengths: Useful to detect nephrolithiasis-related obstruction and extrinsic causes of obstruction | Not used | Second-line test Strengths: Helps differentiate functional obstruction from chronic dilatation |
Not used |
| Transplant renal artery stenosis | Preferred test Strengths: Reasonably high sensitivity in highly trained centers; can be serially followed Weakness: Vessel angulation may limit diagnostic accuracy; operator-dependent, limited specificity, lack of intervention option |
CT angiography not studied extensively in transplants Strengths: Theoretically can achieve high sensitivity and specificity in diagnosis Weaknesses: Risk of contrast nephropathy; lack of intervention option |
Strengths: Confirmatory test in cases of equivocal US findings Weakness: Possible high false-positive rates; risk of NSF in GFR <30 ml/min per 1.73 m2 in gadolinium-based studies |
Not used | Preferred confirmatory second-line test in cases with high suspicion Strength: Simultaneous intervention option Weakness: Risk of contrast nephropathy |
| Fluid collections– (hematomas, abscess, lymphocele, urinomas) | Preferred Strengths: Follow serially, simultaneous drainage option Weakness: Low specificity |
Preferred second-line test Strengths: High specificity, follow serially for resolution, define surgical intervention |
Preferred third-line line test Strength: Useful for equivocal CT and/or US findings |
Useful only in cases of urine leaks | Not used |
| PTLD | Second-line test Weakness: Small lesions cannot be characterized |
Preferred Strengths: High sensitivity, detects extrarenal graft lesions, aids in staging Weakness: Lacks specificity, biopsy required, contrast agent may be needed |
Preferred Strengths: High sensitivity, detects extrarenal graft lesions, aids in staging Weakness: Lacks specificity, biopsy required, contrast agent may be needed |
Not used | Not used |
| Nephrolithiasis | Useful for serial imaging for resolution | Preferred first-line test Strengths: High sensitivity and specificity; contrast agent not needed |
Not used | Not used | Not used |
| Biopsy/biopsy complications | Preferred modality for biopsy and detecting postbiopsy complications Weakness: Small complications can be missed |
Preferred test to serially follow selected complications | Not used | Not used | Preferred second-line test Strengths: High sensitivity and specificity, intervention options, detects small lesions Weaknesses: Contrast nephropathy, inherent risk of procedure |
ATN, acute tubular necrosis; DGF, delayed graft function; CT, computed tomography; US, ultrasonography; NSF, nephrogenic systemic fibrosis; PTLD, post-transplant lymphoproliferative disorder.
Imaging modality preference based on center expertise, emergent availability, and individual initial surgical/clinical course.
Ultrasonography
Color Doppler US is considered the first-line imaging modality to evaluate graft dysfunction because of its portability, rapid technique, and lack of radiation or toxic dye. It also provides some physiologic information about the allograft. The healthy allograft appearance is similar to that of the native kidneys, although clearer detail is usually apparent because of its superficial anatomic location. As a result of the new anastomosis at the uretero-vesical valve junction, high-urine-output state, and mild anastomotic edema, the collecting system of a well functioning allograft is often slightly dilated in the immediate and early postoperative period. The vessels of the healthy transplant, through positioning of the graft in the iliac fossa, may appear as tortuous vessels on imaging that may pose a difficulty in assessing peak velocity measurements, as discussed below in evaluating for transplant renal artery stenosis. The renal arterial resistance index (RI) is a sonographic index calculated as follows:
 |
The renal artery vessels normally demonstrate a low-resistance waveform with an RI<0.7. The normal peak velocity of the transplant renal artery is in the range of 170–210 cm/sec, whereas the renal venous flow is flat with low-velocity waveforms (1,2). Along with renal artery measurements, the proximal and distal iliac vessels also need to be evaluated to compare the flow to the renal artery velocities. Elevated renal artery velocities in the immediate postoperative period do not necessarily represent stenosis requiring intervention because in most cases they normalize over time (3).
Parenchymal Abnormalities
In delayed graft function due to acute tubular necrosis (ATN), US findings are nonspecific on gray-scale imaging. Apart from graft swelling or enlargement, there can be obscured corticomedullary differentiation, decreased echogenicity, and scattered heterogenous areas of increased echogenicity. Findings may be totally normal as well. Color Doppler US may reveal nonspecific elevated RIs (>0.80), which are also seen in calcineurin inhibitor (CNI) toxicity as well as in rejection. In rejection, apart from graft swelling, nonspecific findings include mild hydronephrosis and elevated peak systolic velocities (PSVs) in the transplant renal artery, thought to be due to immune-mediated inflammation of the ureter and transplant renal artery, respectively, leading to a functional narrowing often seen more prominently at the anastomotic sites. Graft swelling or enlargement can be seen in several conditions, including a normal early postoperative state, as well as in delayed graft function, cellular or humoral rejection, acute CNI toxicity, and obstruction.
In CNI toxicity, US may show completely normal results or nonspecific findings, such as graft swelling, increased or decreased renal echogenicity, and loss of corticomedullary differentiation. Color Doppler US may show a nonspecific RI increase of >0.80. Consequently, biopsy may be required for diagnosis. Long-term CNI use can lead to chronic allograft nephropathy, in which US may show thinned cortices, smaller kidneys, or normal findings. The RI may be elevated in chronic allograft nephropathy and may be a valuable predictor of long-term allograft survival when measured at 3 months after transplantation (4). The RI has also been associated with surrogate measures of vascular compliance, such as recipient age and pulse pressure index, but not with chronic allograft damage, compared with histomorphometry, in patients with stable renal function (5). Hence, the role and follow-up of RI remain controversial and deserve more research.
BK virus nephropathy occurs in up to 5%–10% of kidney transplants, usually within the first 12–18 months of transplantation. US findings are nonspecific, although obstructive features have been reported because of the ureteral involvement of the virus (6). Serum- and urine-based PCR along with biopsy findings supporting BK virus tubular damage is required for confirmatory diagnosis (7).
Collecting System Complications
Urologic complications have decreased in frequency in the current era of advanced surgical techniques and ureteral stents compared with earlier reports; rates range between 3% and 9% (8–10). The transplant ureter can be involved because of its delicate vascular supply, which originates from the renal hilum, or due to any damage to accessory arteries leading to ischemia of the ureter.
Ureteral obstruction is reported to occur in about 2%–5% of kidney transplant recipients. The site of obstruction most commonly involved is the anastomosis into the bladder, and roughly 90% of stenoses occur in the distal third of the ureter. The degree of obstruction can be expressed using a grading system, such as grade I through IV, or as mild, moderate, or severe, although these grades are subjective and operator- and time-dependent (Figure 2). If the urothelium has been chronically stretched, the collecting system may never collapse again, making it very difficult it to distinguish chronic residual dilatation from functional obstruction. Nuclear renography with diuretic challenge, as discussed later, can be useful in differentiating residual dilation from true obstructive uropathy. In addition, percutaneous drainage may be occasionally used if results are equivocal. In the setting of severe rejections or ATN, the intrinsic parenchymal tension may limit dilatation of the collecting system, leading to underdiagnosis. Color Doppler US provides limited information because the RI may be nonspecifically elevated in hydronephrosis. Overall, serial US provides more clinically relevant information and sensitivity in many cases.
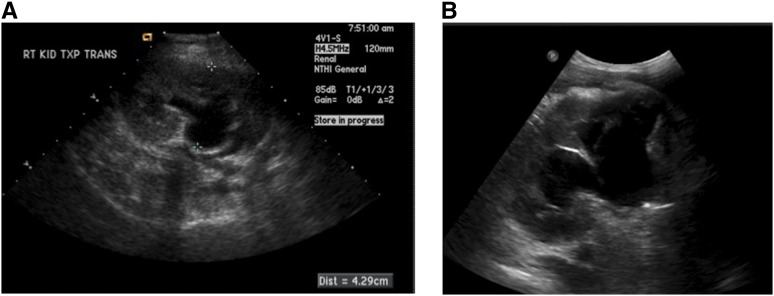
Figure 2.
Grayscale ultrasonographic findings of obstructive hydronephrosis. (A) Moderate obstructive hydronephrosis. (B) Severe obstructive hydronephrosis.
Urologic complications are extremely common in pediatric transplants, and patients with posterior urethral valves undergoing renal transplantation are at increased risk for postoperative vesico-ureteral reflux problems even after surgical repair (11,12). Pediatric post-transplant hydronephrosis has correlated with worsening renal function and increased incidence of pyelonephritis, necessitating more aggressive preoperative and postoperative urologic testing and management (13). Most of the testing and management require US or endo-ureteral imaging, and its role and a proposed algorithm are outlined nicely by Barrero et al. (14).
Urine leaks can occur in 1%–5% of renal transplant recipients (15–17) and usually occur early after transplantation. The clinical presentation of urine leaks includes intense pain and swelling over or around the graft that radiates to surrounding areas, fevers, and change in graft function. Extravasation most commonly occurs from distal ureteric sites because of rejection or ischemia; it can also occur at the ureteroneocystostomy site because of obstruction or incomplete bladder closure. Caliceal and upper proximal ureteric leaks are less common; they are thought to be secondary to segmental infarction in patients with accessory renal arteries, ligation of a polar artery, or a postbiopsy complication (15). US reveals nonspecific, usually nonseptated, well defined anechoic fluid collection, in most cases adjacent to the lower pole of the transplant. The leak may be extraperitoneal or intraperitoneal; if the latter, it may lead to ascites. Drainage can be performed under US guidance, and testing the fluid for creatinine helps differentiate it from seromas or lymphoceles. Fluid from urinomas will have a higher concentration of creatinine compared with the serum (Figure 3).
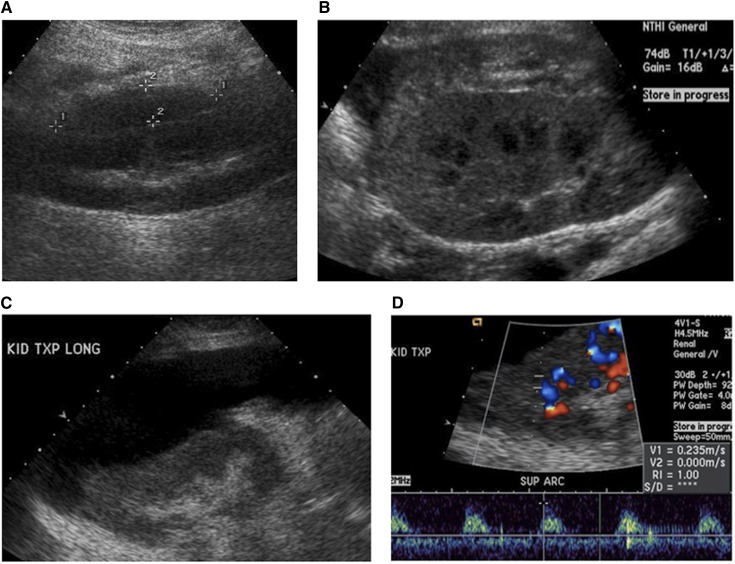
Figure 3.
Post-transplant perinephric complications. (A) Acute hematoma on postoperative day 1 as imaged on grayscale ultrasonography. (B) Subacute hematoma identified on postoperative day 12 with septated complex fluid collection (arrow), along with acute subcapsular hematoma (arrowhead). (C) Large peritransplant lymphocele identified 2 weeks after transplantation, seen as a relatively anechoic fluid collection causing extrinsic compression of the graft. (D) Color Doppler ultrasonography showing high resistance indices in graft dysfunction due to extrinsic compression from a large lymphocele. Very high resistance index of 1.0 is noted.
Perinephric Complications
In the immediate postoperative period, hematomas are the most commonly encountered fluid collections. The overall incidence of postoperative hematomas varies from 4%–8% (18–20). They can be subcapsular or perinephric and are usually small, with spontaneous resolution. They may also result from trauma or biopsy. US findings demonstrate an echogenic fluid collection in the acute phase and become less echogenic over time as clot lysis occurs.
Development of lymphoceles after kidney transplantation is a frequent complication, with an incidence ranging from 0.6%–33.9%. Clinical presentation signs are usually pain over the graft, swelling, or change in graft function. Lymphatic leakage can be caused by disrupting lymphatic channels during the preparation of the recipient iliac vessels or by the graft itself (21). A high percentage of lymphoceles are diagnosed incidentally because most perirenal lymphatic collections are small and asymptomatic. Immunosuppressive drugs, such as sirolimus and everolimus; higher body mass index; and high-dose steroid therapy have been linked with a higher risk of developing lymphatic-related complications. Lymphoceles usually occur medial to the transplant, between the graft and the bladder, and in most cases develop over several weeks after transplantation. They appear as anechoic collections and may have septations. US-guided percutaneous drainage is the recommended first line of treatment, with a success rate >50%.
Vascular Complications
Transplant renal artery stenosis (TRAS) is usually diagnosed within the first year after transplantation, with an incidence rate of 8.3 cases per 1000 patient-years (22). Up to 50% of TRAS cases occur at the site of the anastomosis, and there does not appear to be any difference between end-to-end anastomoses and end-to-side anastomoses (23,24). TRAS is usually due to clamp perfusion injury, incorrect suture technique, or inflammatory fibrotic reaction to the suture material. Some data suggest that postanastomosis stenosis can occur secondary to delayed graft function, rejections, and, rarely, viral infections (25–27). Other risk factors include deceased-donor compared with live-donor transplants (as a result of immunologic factors and prolonged cold ischemia time), while progressive atherosclerosis is associated with late-onset TRAS (22).
Color Doppler US is a well-accepted screening tool for suspected TRAS and can be highly reliable tool in very experienced and well trained centers (28). Stenotic segments appear as focal areas of color aliasing because of increased flow velocity. Selective evaluation with duplex Doppler techniques can characterize and grade the flow disturbance. Many criteria are used to detect TRAS using color Doppler US. Peak systolic velocity (PSV), intrarenal dampening of flow, and RI are the important diagnostic measures. Doppler criteria for significant stenoses include the following: (1) focal frequency shifts >7.5 KHz (when a 3-MHz transducer is used) or PSV >2 m/sec, (2) a velocity gradient between stenotic and prestenotic (iliac vessel) segments of 2:1, and (3) marked distal disturbance (spectral broadening). In the renal parenchyma, tardus-parvus waveform abnormalities can be observed (29). Although various thresholds have been reported for the PSV, its sensitivity and specificity are not absolute. The software depends on the operator’s estimate of the angle of insonation, and the accuracy of the angle correction depends on the course of the artery. Arteries with straight, well delineated courses usually lead to a more confident diagnosis with higher sensitivity and specificity. In cases of high PSV alone without clinical findings, a closer repeat follow-up is recommended instead of immediate intervention (Figure 4) (3).
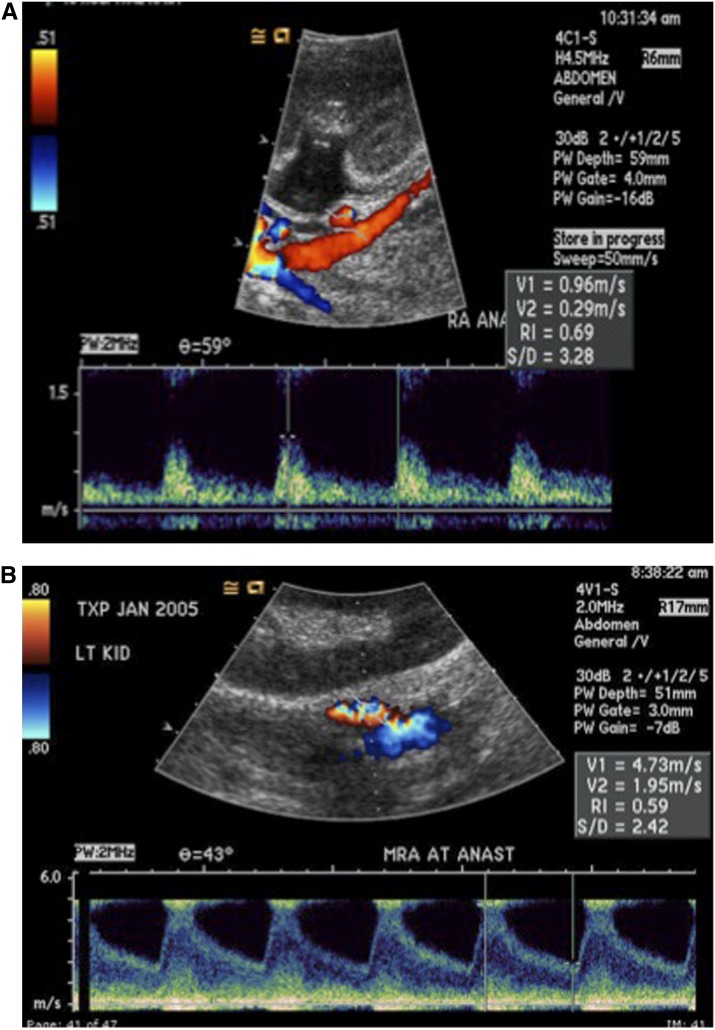
Figure 4.
Color Doppler ultrasonography (US) evaluation of transplant renal artery stenosis. (A) Normal color Doppler US showing normal peak systolic velocity at the anastomosis site with a value of 0.96 m/sec and normal resistance index of 0.69. (B) Color Doppler US in a patient with transplant renal artery stenosis, with peak systolic velocity of 4.73 m/sec at the anastomosis site. Note color distortion suggesting turbulent flow along with spectral broadening of Doppler wave form (lower section). Iliac velocity (not shown) was 1.3 m/sec, and digital subtraction angiography confirmed hemodynamically significant transplant renal artery stenosis requiring angioplasty and stenting.
Arterial thrombosis is now a rare complication, with a prevalence of 0.5%–2%, and usually occurs in the early post-transplant period. However, it is a major cause of early (<1 week) graft loss (30) where the flow in both main and intrarenal arteries is completely absent. Segmental infarcts appear as poorly marginated, hypoechoic masses or a hypoechoic mass with a well defined echogenic wall. Global infarction will appear as a hypoechoic, diffusely enlarged kidney (29). With color Doppler US imaging, segmental infarcts appear as wedge-shaped areas without color flow in, although these findings may also be seen in severe pyelonephritis or transplant rupture. Gray-scale US findings in renal vein thrombosis include an enlarged kidney, while color Doppler US shows reduced or absent venous flow, with increased resistance on the arterial side; this often results in reversed diastolic flow on Doppler images. MR venography can help confirm this complication in transplants. As is the case with arterial thromboses, early recognition of renal vein thrombosis is crucial because rarely, the allograft can be salvaged by prompt venous thrombectomy.
Postbiopsy Complications
Despite advances in noninvasive diagnostic tests and techniques, US-guided percutaneous core needle biopsy is still required in many cases of allograft dysfunction. Macroscopic hematuria after biopsy occurs in 1%–7% of biopsies and is usually self-limiting (31–35). Color Doppler US can easily demonstrate arteriovenous fistulas (AVFs) and pseudoaneurysms as localized areas of disorganized color that extend outside the confines of the normal vessel in the renal parenchyma. This appearance is caused by perifistula vibration and is detected with the more sensitive color Doppler units. The vibrating interfaces in the perivascular tissue produce phase shifts in the reflected sound wave and result in random color assignment in this region. AVFs classically appear as abnormal high-velocity turbulent flow isolated to a single segmental or interlobar artery and paired vein that produces aliasing on color Doppler images. The feeding artery shows a high-velocity, low-resistance waveform, and the draining vein demonstrates arterialization (29,36). A mimic of an AVF is an intrarenal arterial stenosis causing similar high-velocity flow and tissue vibration, except there is no change in venous waveform (Figure 5).
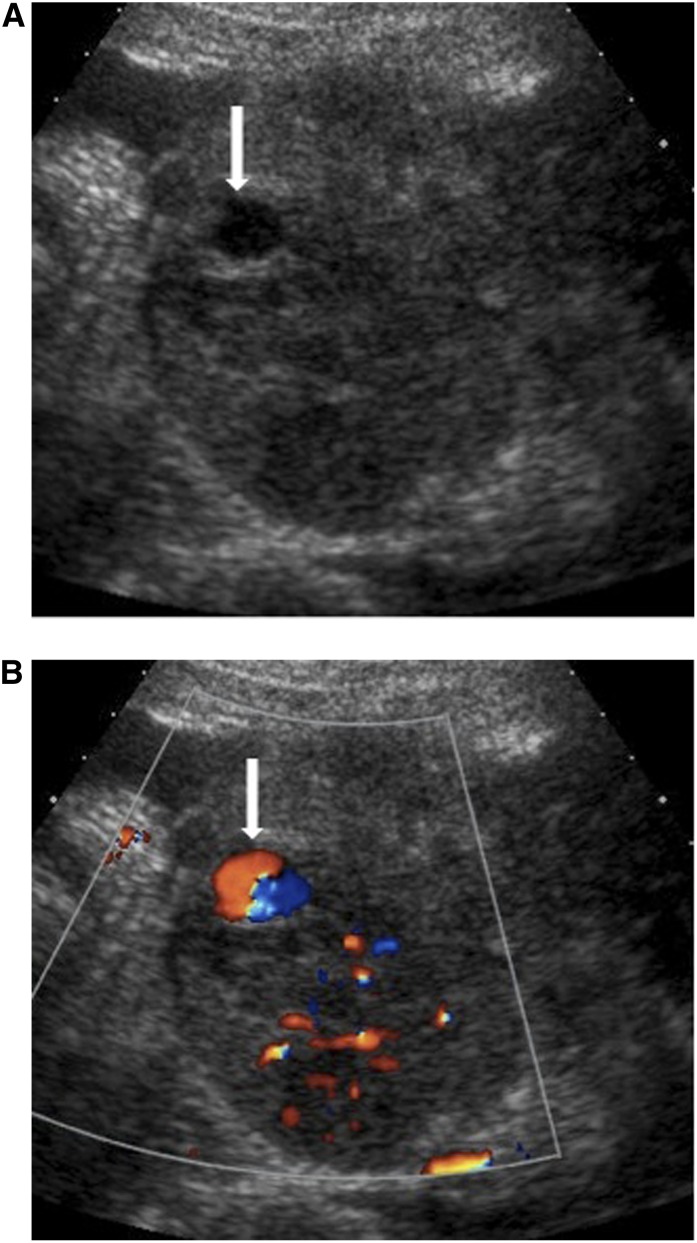
Figure 5.
Doppler ultrasonography evaluation of postbiopsy arteriovenous fistula. (A) Grayscale image showing a hypoechoic-like structure (arrow) 1 week after a percutaneous kidney transplant biopsy in a patient who presented with ongoing hematuria. (B) Color Doppler ultrasonography evaluation showing turbulent arteriovenous flow within the region (arrow), compatible with a large arteriovenous fistula.
Newer US Techniques
Contrast-enhanced sonography (CES) with injected agitated microbubbles may have a much higher sensitivity and specificity and may be more useful for detecting infarction and cortical necrosis, particularly in ischemic renal transplants (37). CES provides quantitative information on microvascular perfusion of the renal allografts and offers improved diagnostic significance compared with color Doppler US for the detection of chronic allograft nephropathy. In contrast to conventional color Doppler US RIs and pulsatility indices, renal blood flow estimated by CES is highly significantly related to serum creatinine. ATN and vascular rejection are associated with characteristic changes of the time intensity curve of CES. Quantitative determination of arterial arrival of a US contrast medium in the early phase after kidney transplantation has been studied and may identify acute rejection earlier than do conventional techniques (38). In patients with normal graft function, the regular inflow of contrast medium is demonstrated in all regions of the graft. However, in patients with delayed graft function, the inflow of the contrast medium was delayed, the time of inflow to the regions of interest significantly differed between those two groups. There is a significantly longer inflow time of the contrast medium to the cortex and renal pyramids in patients with acute rejection than in recipients with ATN. Hence, CES may be a valuable diagnostic tool for determining the cause of delayed graft function (39), as well as postbiopsy AVF evaluation.
US-based elastography (elasticity) has also been explored as a novel noninvasive technique for the assessment of renal allograft fibrosis. This technique has demonstrated high reliability in liver allografts and liver fibrosis. Parenchymal stiffness can be measured by this transient elastography technique and correlates with histologic measures of interstitial fibrosis. Further long-term longitudinal assessments might make it a useful tool to identify patients with chronic allograft nephropathy, thereby allowing early interventions in reducing progressive fibrosis (40,41).
Computed Tomography
CT provides superb anatomic detail of the graft and surrounding tissues, although its use is limited because of the requirement for nephrotoxic contrast agents.
Post-transplant lymphoproliferative disorders (PTLDs) are unique complications in transplant recipients, occurring in 2%–10% of recipients. They may present as a diffuse homogenous infiltrated lesion or a focal intraparenchymal lesion, or may be localized near the allograft. Because of the time-dependent and heterogenous nature of PTLD, all three modalities—US, CT, and MRI—can be used in the diagnostic work-up of patients suspected of having PTLD. Minimally enhanced masses of the transplant renal hilum that encase the hilar vessels are a characteristic finding in PTLD on MRI. CT findings are nonspecific and may include nonenhancing or peripherally enhancing, low-attenuating masses (Figure 6) (42). Because renal limited PTLD is rare and most PTLDs occur in nonrenal sites, noncontrast region-specific CT is generally considered the first-line imaging in patients suspected of having PTLD.
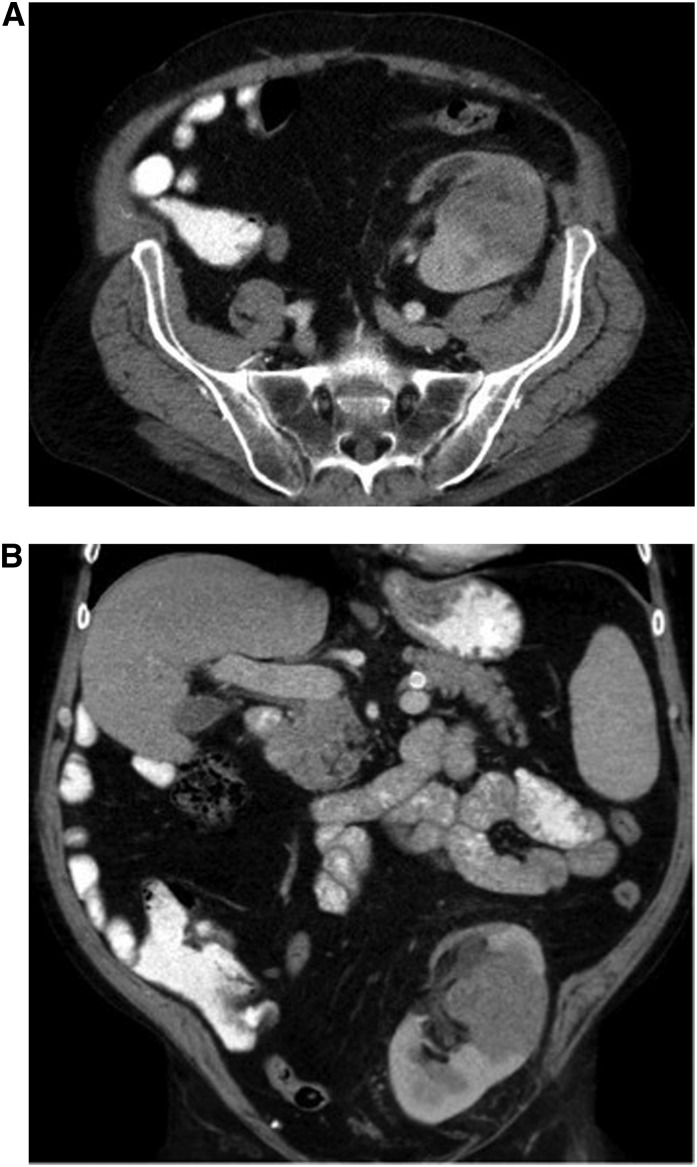
Figure 6.
Computed tomography images of a patient 2 years after transplantation. The patient presented with hematuria, rising creatinine level, and pain over the graft. Transverse (A) and coronal (B) images show a soft tissue mass centered at the midpole of the transplanted kidney, which is heterogeneous in attenuation and measures 6.0 cm × 5.4 cm × 7.0 cm, extending from the lateral cortex to the renal hilum. The remainder of the transplanted kidney is uniformly enhancing with intravenous contrast agent. Biopsy showed post-transplant lymphoproliferative disease.
The CT appearance of a urinoma is a peritransplant fluid collection that may contain contrast opacified fluid that is isodense to the collecting system fluid (if the leak is active at the time of CT). CT appearance of perigraft hematomas are time dependent, as with other hematomas. Acute hematoma appears as a fluid collection with hyperattenuating areas before intravenous administration of contrast material, a finding that is consistent with fresh blood. The presence of an asymptomatic, hyperattenuating perirenal collection after surgery is common and can be treated conservatively if it does not increase in size. CT of lymphoceles shows them to have variable characteristics, and they are usually sharply circumscribed. Their CT attenuation values are usually lower than those of recent hematomas and abscesses. CT-based angiography can be used in the evaluation of TRAS, but digital subtraction angiography offers simultaneous invasive measurements as well as therapeutic interventional options.
However, because ionizing radiation poses a recognized risk for malignancies, the effects of multiple pre- and post-transplant radiation in the setting of immunosuppression may enhance this risk (43).
Multidetector CT (MDCT) with three-dimensional reconstruction has become the technique of choice in the evaluation of potential living kidney donors because of the detailed visualization of renal parenchymal disease, arterial and venous anomalies, and collecting system abnormalities. MDCT has 93%–99% accuracy in the identification of accessory renal arteries, prehilar branching, and renal venous anomalies (44). Many groups also consider MDCT angiography to be more sensitive and accurate than contrast-enhanced MR angiography in the detection of supernumerary arteries before living donor nephrectomy.
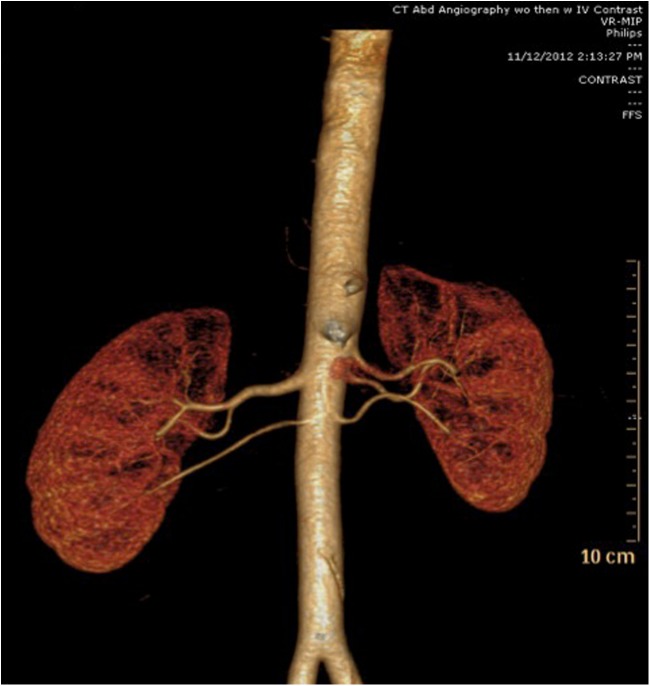
Measurements of kidney volumes, based on MDCT three-dimensional measurements, are used in the selection process, and studies have shown a correlation between donor kidney volume and recipient graft function. Larger kidney volumes are correlated with improved kidney function at 1 year (45). Renal length and volumes also correlate with recipient renal function up to 36 months after transplantation. A low ratio of cortical volume to recipient weight has been associated with diminished graft function at 36 months (45–47). Hence, volumetric measurements are now becoming an important tool in selecting laterality, along with nephron dose matching with the recipient (Figure 7). There also seems to be a reasonable correlation between volume measurements and percentage of calculated renal function based on total volume, as measured by three-dimensional CT angiography compared with split renal function measurements measured by NM imaging (48). Selective cases may require dual testing with NM imaging to help leave the donor with the higher functioning kidney.
Figure 7.
Multidetector computed tomography (CT) with CT angiography and three-dimensional reconstruction of a healthy predonation living-kidney donor. Multiple arteries are seen on CT angiographic evaluation: three on the right and two on the left. Decisions for selecting right versus left kidney are based on vasculature, along with careful review of volume measurements.
Nuclear Medicine Imaging
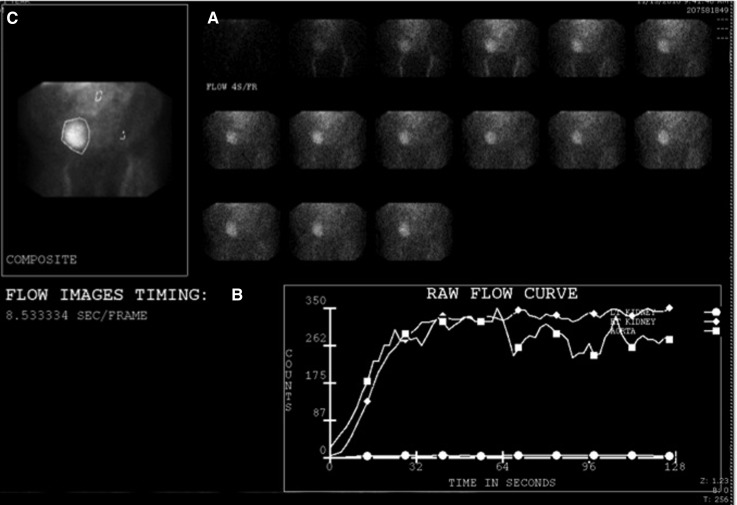
NM imaging of the allograft is a noninvasive, non-nephrotoxic tool to evaluate graft dysfunction, particularly in the early postoperative period. In cases of arterial thrombosis, renal scintigraphy and time activity curves show absent or reduced perfusion in the graft. This finding is nonspecific, however, because it may be seen with other causes of parenchymal failure, including graft rejection and urinary obstruction. In ATN, NM imaging typically shows good perfusion on the angiographic phase, with preserved concentration during the parenchymal second phase. The excretory third phase shows minimal excretion of the radiotracer agent into the collecting system and bladder. Because of poor plasma clearance of the agent, there is also high surrounding tissue background activity. In rejection, NM renography demonstrates decreased perfusion and delayed transplant visualization, with poor parenchymal uptake and high background activity (Figure 8). Because of the nonspecific and nondiagnostic capability of US and NM imaging modalities, clinical correlation is extremely important; US-guided renal biopsy remains the gold standard for confirmatory diagnosis for ATN or rejection. NM imaging has no role in the diagnostic evaluation of suspected TRAS.
Figure 8.
Nuclear medicine images of a kidney transplant on postoperative day 1 with delayed graft function secondary to acute tubular necrosis. Dynamic images (A) of the study shows a normal prompt perfusion pattern to the transplanted kidney. Decreased excretion and clearance to transplant kidney are consistent with acute tubular necrosis. Trace bladder activity is noted. Radiopharmaceutical agent was 99mTc mertiatide (MAG3). (B) Regions of interest are drawn around the kidney. (C) Curves generated of the activity within that region as a function of time in ATN.
In cases of urinary obstruction, NM imaging shows normal perfusion and parenchymal uptake of the tracer but persistent radiotracer activity in the pelvis and collecting system. However, it is possible that NM imaging may be less sensitive because impaired allograft function often causes impaired uptake. In urine leaks, NM imaging shows extravasation of radiotracer into an area that is outside the collecting system or an area that was initially “cold” to confirm urine leaks. Delayed NM images with slow tracer accumulation help in detecting very small leaks.
In renal infarcts, NM images can show lack of perfusion, absent visualization of the transplanted kidney, and poor clearance of the tracer, along with a photopenic space in the expected location of the transplant where a photopenic region or wedge-shaped “cold” defect may be seen. However, these findings are not specific because hyperacute or accelerated acute rejection, cortical necrosis, and renal vein thrombosis can have similar clinical, Doppler US, and scintigraphic features. Finally, NM imaging can be used to measure GFR before living-donor kidney transplantation.
Magnetic Resonance Imaging
MRI has increasingly become popular in kidney transplants and can be used as a second-line imaging technique if US or CT has been nondiagnostic in cases of parenchymal lesions or perinephric collections. MR angiography can be used to diagnose or confirm TRAS (Figure 9). It has the advantage of requiring a gadolinium chelate that is not nephrotoxic. However, in cases of GFR<30 ml/min per 1.73 m2, gadolinium-based contrast agents cannot be used because of their risk of causing nephrogenic systemic fibrosis. Newer imaging acquisition techniques are being developed that may allow better vascular imaging without the use of gadolinium-based dye. Some reports have found that MR angiography correlated well with the gold standard digital subtraction angiography, whereas others have reported that compared with color Doppler US and digital subtraction angiography, MR angiography may be of limited diagnostic value for diagnosing TRAS because of an up to 75% false-positive rate with MR angiography (49). This is thought to be due to a major intravoxel phase dispersion, which may result from tortuosity of the vessel or a sharp angulation between the artery and the parent vessel. Figure 10 provides a comprehensive algorithm for using color Doppler US, digital subtraction angiography, and MR angiography for suspected TRAS.
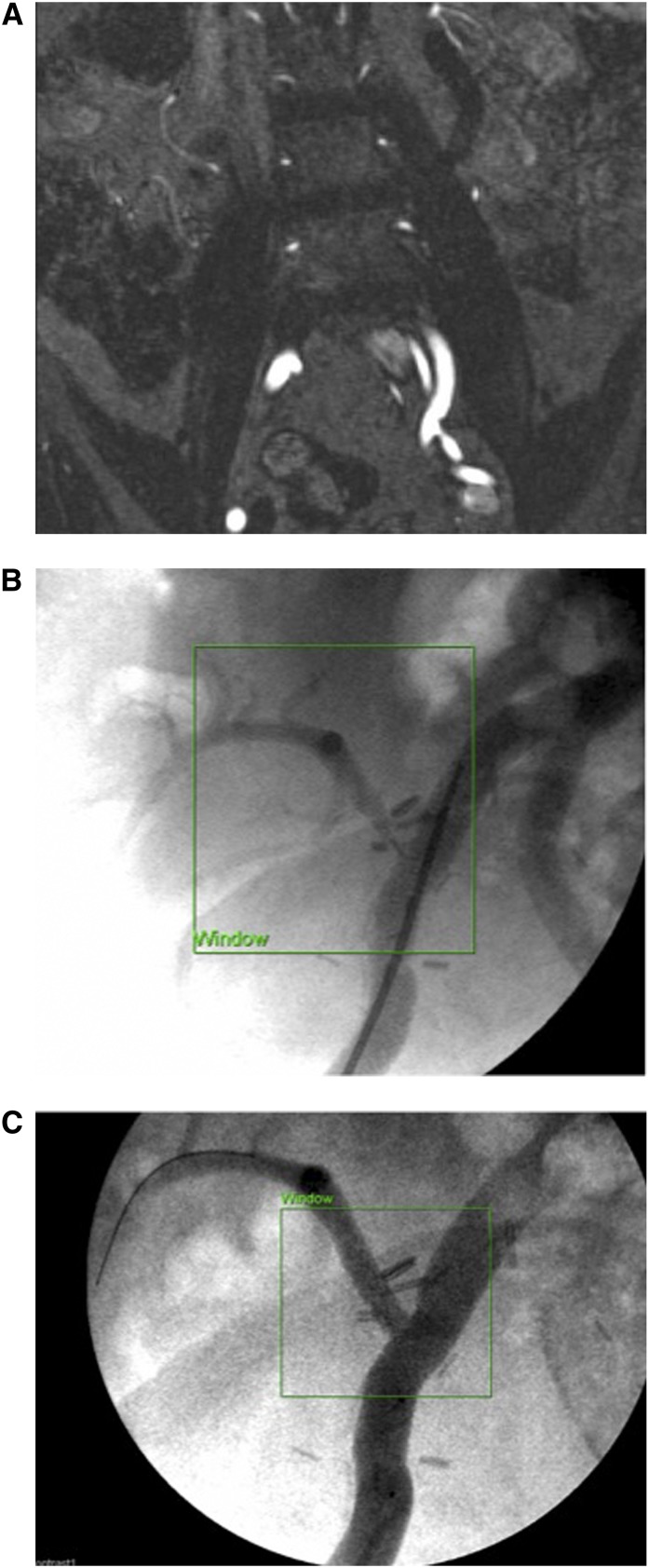
Figure 9.
Transplant renal artery stenosis (TRAS). (A) Magnetic resonance angiography in a patient 6 months after transplant, with suspected TRAS showing a tight stenosis at the anastomosis site of the transplant renal artery to the iliac vessel with an approximate diameter of 75% reduction in lumen. Because of the angle and course of the vessel, the graft itself is not visualized in this view. (B) Digital subtraction angiography in a patient with TRAS showing a tight stenosis at the anastomosis with 80% stenosis in conjunction with a pressure gradient of >20mmHg across the stenosis. (C) Postangioplasty ballooning with stenting showing patent flow at the anastomosis site.
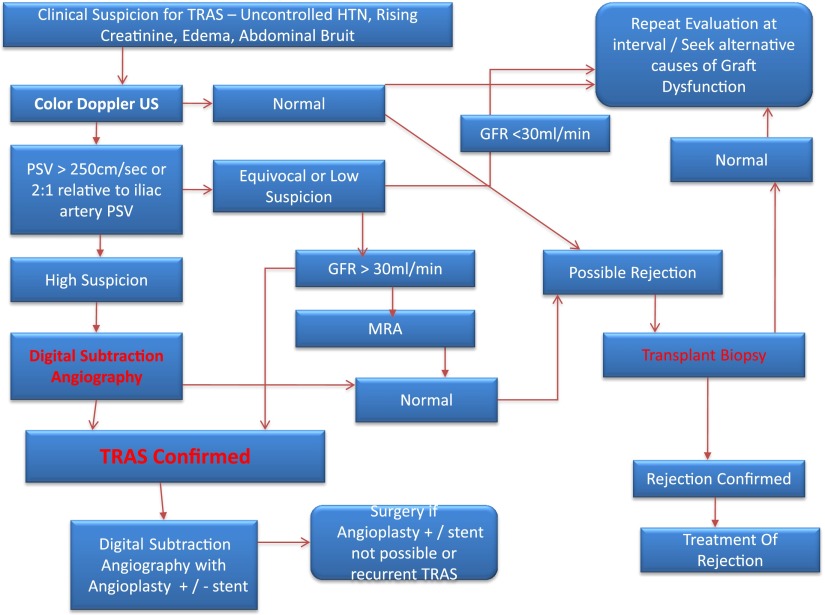
Figure 10.
Proposed algorithm for the diagnosis and management of transplant renal artery stenosis. HTN, hypertension; MRA, magnetic resonance angiography; PSV, peak systolic velocity; TRAS, transplant renal artery stenosis; US, ultrasonography.
MR angiography can be used to confirm renal infarcts when results on US or CT are equivocal. Dynamic enhanced MR imaging can be useful for diagnosing both segmental and global infarctions as well as renal artery thrombosis. Infarctions show loss of corticomedullary differentiation on T1- and T2-weighted images with homogenous low-intensity signal on T1 and high signal intensity on T1-weighted images (50).
Newer MR techniques, such as diffusion-tensor imaging at 3T imaging sequences, show that medullary fractional anisotropy and apparent diffusion coefficient exhibit a good correlation with renal function in adult grafts with impaired function (estimated GFR <30 ml/min per 1.73 m2). Hence, it may provide noninvasive information for functional assessment of such renal allografts (51). Blood oxygenation level–dependent MRI techniques at 3T imaging are also feasible and reproducible in renal transplant recipients, in whom there is significantly lower medullary oxygenation levels noted in those with acute rejection (52); these techniques could also serve as useful noninvasive imaging tools to help differentiate between ATN and acute rejection in the early postoperative period (53).
Other potential advantages of three-dimensional whole-kidney MR renography is the ability to diagnose regional disease and avoid the inherent sampling errors of a renal biopsy. Yamamoto et al. have used a new quantitative analysis method of MR renography, which includes multicompartment tracer kinetic modeling, to noninvasively diagnose acute rejection or ATN after kidney transplantation using low-dose (4 ml) gadoteridol administration. The relative risks of low-dose gadolinium-based MR renography compared with renal biopsy for differentiating ATN from acute rejection need further consideration (54).
Research Techniques in Imaging Kidney Transplants
Newer research modalities are constantly being developed to aid in noninvasive diagnosis of graft dysfunction. Ultra-small particles of iron oxide are macromolecular agents based on iron; these 20- to 30-nm dextrans, coated in a formulation chemically known as ferumoxtran-10, are not filterable across the glomerulus. In models of allograft rejection, uptake of ultra-small particles of iron oxide corresponds with the loss of signal in the renal parenchyma and the degree of lymphocytic infiltration. Others have shown that graft fluorodeoxyglucose positron emission tomography is a new option for early, noninvasive, and specific detection and follow-up of acute rejection; this technique can be used to differentiate acute rejection from ATN and CNI toxicity (55). Furthermore, ongoing research is studying intravital microscopy in kidney transplants. This technique has been used in mice models of kidney transplantation; authors have found brief ischemia to be associated with increase in microvascular leakage, along with renal tubular cell death, without significant changes in leukocyte adhesion or capillary blood flow. This highly powerful tool appears very promising and can be used to differentiate and study the role of the dynamic immune cells in different disease states, such as rejection, ischemia, and tolerance (51).
The hope is that further advances in all imaging modalities will continue to expand the role of noninvasive diagnostic testing and therapeutics in kidney transplantation. Currently, US and the other modalities remain an indispensable tool for evaluating the kidney transplant recipient with graft dysfunction or post-transplant related complications.
Disclosures
None.
Acknowledgments
Images were kindly provided by Dr. Bilal Tahir, Assistant Professor of Clinical Radiology and Imaging Sciences, Department of Radiology, Indiana University School of Medicine.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Friedewald SM, Molmenti EP, Friedewald JJ, Dejong MR, Hamper UM: Vascular and nonvascular complications of renal transplants: Sonographic evaluation and correlation with other imaging modalities, surgery, and pathology. J Clin Ultrasound 33: 127–139, 2005 [DOI] [PubMed] [Google Scholar]
- 2.Jakobsen JA, Brabrand K, Egge TS, Hartmann A: Doppler examination of the allografted kidney. Acta Radiol 44: 3–12, 2003 [PubMed] [Google Scholar]
- 3.Siskind E, Lombardi P, Blum M, Tyrell R, Villa M, Kuncewitch M, Olsen EM, Alex A, Lumermann L, Bhaskaran MC, Jhaveri KD, Sachdeva M, Calderon K, Greben C, Putterman D, Gandras E, Caplin D, D’ Agostino C, Pellerito J, Coppa G, Molmenti EP: Significance of elevated transplant renal artery velocities in the postoperative renal transplant patient. Clin Transplant 27: E157–E160, 2013 [DOI] [PubMed] [Google Scholar]
- 4.Radermacher J, Mengel M, Ellis S, Stuht S, Hiss M, Schwarz A, Eisenberger U, Burg M, Luft FC, Gwinner W, Haller H: The renal arterial resistance index and renal allograft survival. N Engl J Med 349: 115–124, 2003 [DOI] [PubMed] [Google Scholar]
- 5.Vallejos A, Alperovich G, Moreso F, Cañas C, de Lama ME, Gomà M, Fulladosa X, Carrera M, Hueso M, Grinyó JM, Serón D: Resistive index and chronic allograft nephropathy evaluated in protocol biopsies as predictors of graft outcome. Nephrol Dial Transplant 20: 2511–2516, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Chang CY, Gangji A, Chorneyko K, Kapoor A: Urological manifestations of BK polyomavirus in renal transplant recipients. Can J Urol 12: 2829–2836, 2005 [PubMed] [Google Scholar]
- 7.Wiseman AC: Polyomavirus nephropathy: A current perspective and clinical considerations. Am J Kidney Dis 54: 131–142, 2009 [DOI] [PubMed] [Google Scholar]
- 8.Shoskes DA, Hanbury D, Cranston D, Morris PJ: Urological complications in 1,000 consecutive renal transplant recipients. J Urol 153: 18–21, 1995 [DOI] [PubMed] [Google Scholar]
- 9.Göğüs C, Yaman O, Soygür T, Bedük Y, Göğüs O: Urological complications in renal transplantation: Long-term follow-up of the Woodruff ureteroneocystostomy procedure in 433 patients. Urol Int 69: 99–101, 2002 [DOI] [PubMed] [Google Scholar]
- 10.Kocak B, Baker TB, Koffron AJ, Leventhal JR: Ureteral complications in the era of laparoscopic living donor nephrectomy: Do we need to preserve the gonadal vein with the specimen? J Endourol 24: 247–251, 2010 [DOI] [PubMed] [Google Scholar]
- 11.Routh JC, Yu RN, Kozinn SI, Nguyen HT, Borer JG: Urological complications and vesicoureteral reflux following pediatric kidney transplantation. J Urol 189: 1071–1076, 2013 [DOI] [PubMed] [Google Scholar]
- 12.Nuininga JE, Feitz WF, van Dael KC, de Gier RP, Cornelissen EA: Urological complications in pediatric renal transplantation. Eur Urol 39: 598–602, 2001 [DOI] [PubMed] [Google Scholar]
- 13.Chu L, Jacobs BL, Schwen Z, Schneck FX: Hydronephrosis in pediatric kidney transplant: Clinical relevance to graft outcome. J Pediatr Urol 9: 217–222, 2013 [DOI] [PubMed]
- 14.Barrero R, Fijo J, Fernandez-Hurtado M, García-Merino F, León E, Torrubia F: Vesicoureteral reflux after kidney transplantation in children. Pediatr Transplant 11: 498–503, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Streeter EH, Little DM, Cranston DW, Morris PJ: The urological complications of renal transplantation: A series of 1535 patients. BJU Int 90: 627–634, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Davari HR, Yarmohammadi H, Malekhosseini SA, Salahi H, Bahador A, Salehipour M: Urological complications in 980 consecutive patients with renal transplantation. Int J Urol 13: 1271–1275, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Karakayali H, Bilgin N, Moray G, Demirbaş M, Ozkardes H: Major urological complications in 1051 consecutive renal transplants. Transplant Proc 28: 2339–2340, 1996 [PubMed] [Google Scholar]
- 18.Dimitroulis D, Bokos J, Zavos G, Nikiteas N, Karidis NP, Katsaronis P, Kostakis A: Vascular complications in renal transplantation: A single-center experience in 1367 renal transplantations and review of the literature. Transplant Proc 41: 1609–1614, 2009 [DOI] [PubMed] [Google Scholar]
- 19.Galmes I, Burgos FJ, Borrego J, Orofino L, del Hoyo J, Rodríguez R, Rodríguez-Luna JM, Fernández E, Lovaco F, Escudero A: Vascular complications in renal transplantation [Article in Spanish]. Actas Urol Esp 19: 8–14, 1995 [PubMed] [Google Scholar]
- 20.Yap R, Madrazo B, Oh HK, Dienst SG: Perirenal fluid collection after renal transplant. Am Surg 47: 287–290, 1981 [PubMed] [Google Scholar]
- 21.Ulrich F, Niedzwiecki S, Fikatas P, Nebrig M, Schmidt SC, Kohler S, Weiss S, Schumacher G, Pascher A, Reinke P, Tullius SG, Pratschke J: Symptomatic lymphoceles after kidney transplantation - multivariate analysis of risk factors and outcome after laparoscopic fenestration. Clin Transplant 24: 273–280, 2010 [DOI] [PubMed] [Google Scholar]
- 22.Hurst FP, Abbott KC, Neff RT, Elster EA, Falta EM, Lentine KL, Agodoa LY, Jindal RM: Incidence, predictors and outcomes of transplant renal artery stenosis after kidney transplantation: analysis of USRDS. Am J Nephrol 30: 459–467, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Henning BF, Kuchlbauer S, Böger CA, Obed A, Farkas S, Zülke C, Scherer MN, Walberer A, Banas M, Krüger B, Schlitt HJ, Banas B, Krämer BK: Percutaneous transluminal angioplasty as first-line treatment of transplant renal artery stenosis. Clin Nephrol 71: 543–549, 2009 [PubMed] [Google Scholar]
- 24.Patel NH, Jindal RM, Wilkin T, Rose S, Johnson MS, Shah H, Namyslowski J, Moresco KP, Trerotola SO: Renal arterial stenosis in renal allografts: Retrospective study of predisposing factors and outcome after percutaneous transluminal angioplasty. Radiology 219: 663–667, 2001 [DOI] [PubMed] [Google Scholar]
- 25.Kamali K, Abbasi MA, Behzadi AH, Mortazavi A, Bastani B: Incidence and risk factors of transplant renal artery stenosis in living unrelated donor renal transplantation. J Ren Care 36: 149–152, 2010 [DOI] [PubMed] [Google Scholar]
- 26.Audard V, Matignon M, Hemery F, Snanoudj R, Desgranges P, Anglade MC, Kobeiter H, Durrbach A, Charpentier B, Lang P, Grimbert P: Risk factors and long-term outcome of transplant renal artery stenosis in adult recipients after treatment by percutaneous transluminal angioplasty. Am J Transplant 6: 95–99, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Hernández D, Rufino M, Armas S, González A, Gutiérrez P, Barbero P, Vivancos S, Rodríguez C, de Vera JR, Torres A: Retrospective analysis of surgical complications following cadaveric kidney transplantation in the modern transplant era. Nephrol Dial Transplant 21: 2908–2915, 2006 [DOI] [PubMed] [Google Scholar]
- 28.Schwenger V, Hinkel UP, Nahm AM, Morath C, Zeier M: Color doppler ultrasonography in the diagnostic evaluation of renal allografts. Nephron Clin Pract 104: c107–c112, 2006 [DOI] [PubMed] [Google Scholar]
- 29.Akbar SA, Jafri SZ, Amendola MA, Madrazo BL, Salem R, Bis KG: Complications of renal transplantation. Radiographics 25: 1335–1356, 2005 [DOI] [PubMed] [Google Scholar]
- 30.Humar A, Matas AJ: Surgical complications after kidney transplantation. Semin Dial 18: 505–510, 2005 [DOI] [PubMed] [Google Scholar]
- 31.Yablon Z, Recupero P, McKenna J, Vella J, Parker MG: Kidney allograft biopsy: Timing to complications. Clin Nephrol 74: 39–45, 2010 [DOI] [PubMed] [Google Scholar]
- 32.Gainza FJ, Minguela I, Lopez-Vidaur I, Ruiz LM, Lampreabe I: Evaluation of complications due to percutaneous renal biopsy in allografts and native kidneys with color-coded Doppler sonography. Clin Nephrol 43: 303–308, 1995 [PubMed] [Google Scholar]
- 33.Kolb LG, Velosa JA, Bergstralh EJ, Offord KP: Percutaneous renal allograft biopsy. A comparison of two needle types and analysis of risk factors. Transplantation 57: 1742–1746, 1994 [PubMed] [Google Scholar]
- 34.Merkus JW, Zeebregts CJ, Hoitsma AJ, van Asten WN, Koene RA, Skotnicki SH: High incidence of arteriovenous fistula after biopsy of kidney allografts. Br J Surg 80: 310–312, 1993 [DOI] [PubMed] [Google Scholar]
- 35.Boschiero LB, Saggin P, Galante O, Prati GF, Dean P, Longo M, Ancona G: Renal needle biopsy of the transplant kidney: Vascular and urologic complications. Urol Int 48: 130–133, 1992 [DOI] [PubMed] [Google Scholar]
- 36.Pearl AL, Ragavendra N, Schiepers C: Diagnostic imaging in kidney transplantation. In: Handbook of Kidney Transplantation, edited by Danovitch GM, Philadelphia, Lippincott Williams & Wilkins, 2007, 291–310 [Google Scholar]
- 37.Correas JM, Claudon M, Tranquart F, Hélénon AO: The kidney: Imaging with microbubble contrast agents. Ultrasound Q 22: 53–66, 2006 [PubMed] [Google Scholar]
- 38.Schwenger V, Hinkel UP, Nahm AM, Morath C, Zeier M: Real-time contrast-enhanced sonography in renal transplant recipients. Clin Transplant 20[Suppl 17]: 51–54, 2006 [DOI] [PubMed] [Google Scholar]
- 39.Grzelak P, Szymczyk K, Strzelczyk J, Kurnatowska I, Sapieha M, Nowicki M, Stefanczyk L: Perfusion of kidney graft pyramids and cortex in contrast-enhanced ultrasonography in the determination of the cause of delayed graft function. Ann Transplant 16: 48–53, 2011 [PubMed] [Google Scholar]
- 40.Gómez-Almaguer D, Vela-Ojeda J, Jaime-Pérez JC, Gutiérrez-Aguirre CH, Cantú-Rodríguez OG, Sobrevilla-Calvo P, Rivas-Vera S, Gómez-Rangel JD, Ruiz-Argüelles GJ: Allografting in patients with severe, refractory aplastic anemia using peripheral blood stem cells and a fludarabine-based conditioning regimen: The Mexican experience. Am J Hematol 81: 157–161, 2006 [DOI] [PubMed] [Google Scholar]
- 41.Gimeno FA, Calvo J, Loinaz C, Meneu JC, Pérez B, Gomez R, Jiménez C, Abradelo M, Moreno A, Sesma A, García I, Moreno E: Comparative analysis of the results of orthotopic liver transplantation in patients with and without portal vein thrombosis. Transplant Proc 37: 3899–3903, 2005 [DOI] [PubMed] [Google Scholar]
- 42.Borhani AA, Hosseinzadeh K, Almusa O, Furlan A, Nalesnik M: Imaging of posttransplantation lymphoproliferative disorder after solid organ transplantation. Radiographics 29: 981–1000, discussion 1000–1002, 2009 [DOI] [PubMed] [Google Scholar]
- 43.Nguyen KN, Patel AM, Weng FL: Ionizing radiation exposure among kidney transplant recipients due to medical imaging during the pretransplant evaluation. Clin J Am Soc Nephrol 8: 833–839, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chu LC, Sheth S, Segev DL, Montgomery RA, Fishman EK: Role of MDCT angiography in selection and presurgical planning of potential renal donors. AJR Am J Roentgenol 199: 1035–1041, 2012 [DOI] [PubMed] [Google Scholar]
- 45.Hugen CM, Polcari AJ, Farooq AV, Fitzgerald MP, Holt DR, Milner JE: Size does matter: Donor renal volume predicts recipient function following live donor renal transplantation. J Urol 185: 605–609, 2011 [DOI] [PubMed] [Google Scholar]
- 46.Sikora MB, Shaaban A, Beddhu S, Bourija H, Wei G, Baird B, Truax CM, Shihab FS: Effect of donor kidney volume on recipient outcome: Does the “dose” matter? Transplantation 94: 1124–1130, 2012 [DOI] [PubMed] [Google Scholar]
- 47.Yano M, Lin MF, Hoffman KA, Vijayan A, Pilgram TK, Narra VR: Renal measurements on CT angiograms: Correlation with graft function at living donor renal transplantation. Radiology 265: 151–157, 2012 [DOI] [PubMed] [Google Scholar]
- 48.Soga S, Britz-Cunningham S, Kumamaru KK, Malek SK, Tullius SG, Rybicki FJ: Comprehensive comparative study of computed tomography-based estimates of split renal function for potential renal donors: Modified ellipsoid method and other CT-based methods. J Comput Assist Tomogr 36: 323–329, 2012 [DOI] [PubMed] [Google Scholar]
- 49.Loubeyre P, Cahen R, Grozel F, Trolliet P, Pouteil-Noble C, Labeeuw M, Tran Minh VA: Transplant renal artery stenosis. Evaluation of diagnosis with magnetic resonance angiography compared with color duplex sonography and arteriography. Transplantation 62: 446–450, 1996 [DOI] [PubMed] [Google Scholar]
- 50.Fang YC, Siegelman ES: Complications of renal transplantation: MR findings. J Comput Assist Tomogr 25: 836–842, 2001 [DOI] [PubMed] [Google Scholar]
- 51.Camirand G: New perspectives in transplantation through intravital microscopy imaging. Curr Opin Organ Transplant 18: 6–12, 2013 [DOI] [PubMed] [Google Scholar]
- 52.Sayar H, Sharfuddin AA, Taber TE, Mehta R: Chronic myeloid leukemia within a year of kidney transplant with elevated alkaline phosphatase correlated with imatinib therapy. Exp Clin Transplant 9: 336–339, 2011 [PubMed] [Google Scholar]
- 53.Paradela M, González D, Parente I, Fernández R, De La Torre MM, Delgado M, García JA, Fieira E, Bonhome C, Maté JM: Surgical risk factors associated with lung transplantation. Transplant Proc 41: 2218–2220, 2009 [DOI] [PubMed] [Google Scholar]
- 54.Banchs HL, González V, González Cancel I, Quintana C, Calderón R, Altieri PI: Heart transplantation in females: The experience in Puerto Rico. Bol Asoc Med P R 97: 248–256, 2005 [PubMed] [Google Scholar]
- 55.Reuter S, Schnöckel U, Schröter R, Schober O, Pavenstädt H, Schäfers M, Gabriëls G, Schlatter E: Non-invasive imaging of acute renal allograft rejection in rats using small animal F-FDG-PET. PLoS ONE 4: e5296, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]