Abstract
Background:
Although obstructive lung disease (OLD), which includes COPD, affects all the populations, Hispanics seem to be protected against COPD development and progression. Whether this advantage translates into a survival benefit for this population is unknown. We aimed to determine the risk for OLD in Mexican Americans, the largest US Hispanic subgroup, compared with non-Hispanic whites and to assess all-cause mortality in subjects with OLD.
Methods:
We assessed the relationships between Mexican American ethnicity and spirometric OLD and risk of death among 6,456 US adults aged ≥ 40 years who participated in the Third National Health and Nutritional Examination Survey Follow-up Study. We used logistic and Cox regression analyses to estimate the OR for OLD among Mexican Americans and the hazard ratio (HR) for all-cause mortality among Mexican Americans with OLD, respectively.
Results:
After adjustment for demographic factors, socioeconomic status, and COPD risk factors, Mexican Americans had decreased odds of OLD diagnosis compared with whites (OR, 0.72 [95% CI, 0.54-0.95]). Among the 1,734 participants with OLD, 1,054 (60.8%) died during median follow-up of 12 years. In an adjusted model, Mexican Americans had no advantage in mortality from all causes (HR, 0.88 [95% CI, 0.69-1.13]). After accounting for the fact that some Mexican Americans may have moved back to Mexico and died there (thus, had no US death certificate), there was still no difference in mortality between these groups.
Conclusions:
Although Mexican Americans appear to have lower risk for OLD, subjects of this ethnicity with OLD do not seem to have a survival advantage.
Obstructive lung disease (OLD) affects about 28.9 million people in the United States.1 OLD includes asthma and COPD, with the latter being now the third leading cause of death in this country.2 The prevalence of OLD differs among major US populations, with Hispanics having a lower prevalence than non-Hispanic whites.1 Since the Hispanic population is the fastest growing and largest minority in the United States, making up about 50 million people,3,4 an increasing number of Hispanic patients with OLD are expected to seek clinical care. Increased understanding of racial-ethnic differences in OLD will improve disease management and inform the development of health-care policies.
The term “Hispanic paradox” is used to describe the observation that clinical outcomes are comparable or more favorable in Hispanics than whites, despite their lower socioeconomic indexes.5 Hispanic health advantages include lower general mortality rates6 and better birth,7 cancer, and cardiovascular disease outcomes.8 Among Hispanic subgroups, Mexican Americans—the largest subgroup of Hispanics (approximately two-thirds)9—have the lowest general mortality.6 The Hispanic paradox may also be applicable in OLD.10‐13 Early and more recent findings demonstrated that relative to non-Hispanic whites, Hispanics had lower prevalence of emphysema and chronic bronchitis,10,11 OLD,1 and reduced odds of COPD diagnosis.12 However, those studies did not account for health-care variables and nonsmoking risk factors for chronic airflow obstruction, such as occupational exposure to respiratory hazards.1,10‐12,14 Whether the potential “protective effect” of Hispanic ethnicity against OLD holds in a nationally representative sample of US Mexican Americans and translates into a survival benefit in subjects with airway obstruction is unknown.
Based on prior evidence, we hypothesized that compared with whites, Mexican Americans are less likely to have a spirometric diagnosis of OLD and that Mexican Americans with OLD have decreased all-cause mortality. We also sought to determine whether country of birth and duration of residence in the United States have effects on mortality in Mexican Americans with OLD. We based this hypothesis on data demonstrating that foreign-born compared with US-born Mexican Americans have a lower respiratory disease-related mortality rate15 and that the longer a Mexican American stays in the United States, the more likely he or she is to adopt negative health-related behaviors and to be exposed to environmental factors, which contribute to the development of chronic diseases.16 To test these hypotheses we used The National Health and Nutrition Examination Survey (NHANES) III and its Linked Mortality File. Some of the results of this study have been previously reported in the form of an abstract.17
Materials and Methods
Study Design
The NHANES III study was conducted from 1988 to 1994 by the National Center for Health Statistics to assess the health and nutrition status of the civilian, noninstitutionalized US population.18 Follow-up data pertaining to death were available through December 31, 2006, in the Linked Mortality File.19 Briefly, NHANES III used a multistage stratified probability sampling design to ensure a representative sample of the US population. The total sample was 20,050 adults. Subjects underwent a detailed interview and examination. In this analysis, we chose participants who self-reported as either non-Hispanic white (hereafter whites) or Mexican American, were at least 40 years old,20 and had examination performed and a reliable spirometric testing based on the American Thoracic Society21 recommendations (N = 6,456) (Fig 1). The NHANES study was approved by the National Center for Health Statistics Institutional Review Board.
Figure 1.
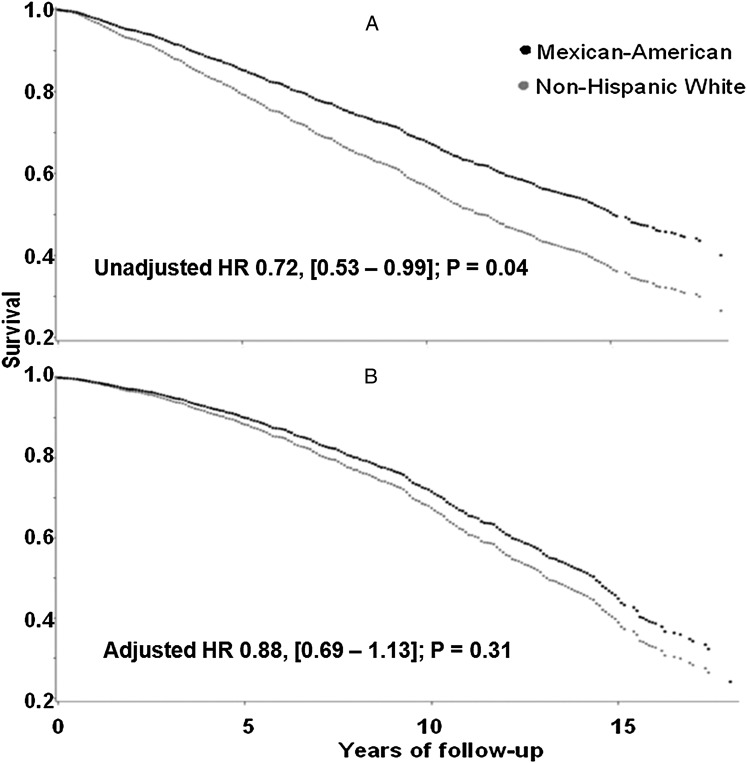
Survival plots for all-cause mortality in subjects aged 40 y or older with obstructive lung disease by race/ethnicity group. A, An unadjusted Cox proportional hazard model shows an advantage in mortality for Mexican Americans (black line) compared with non-Hispanic whites. B, This advantage is no longer apparent in the adjusted model. Adjustment for age, sex, BMI, lifetime smoking status, pack-y of smoking, education level, asthma history, age at asthma diagnosis, dyspnea, and FEV1 % predicted was performed. HR = hazard ratio.
Main Outcomes
The primary outcomes were OLD and all-cause mortality. OLD was defined as a ratio of FEV1 and FVC < 0.7.1 Mortality was determined through matching NHANES III participants with records from the National Death Index (NDI).19
Covariates
Age, sex, country of birth, number of years living in the United States (for immigrant Mexican Americans), education, family income-to-poverty ratio, access to health care, lifetime smoking status, pack-years smoked, exposure to secondhand smoking, comorbidities, work in a high-risk industry, high-risk occupation, and living in urban area were extracted from the Adult Questionnaire at baseline and detailed in e-Appendix 1 (519.4KB, pdf) . We coded the following comorbidities: hypertension, heart attack, chronic heart failure, stroke, diabetes, and cancer. Comorbidities were self-reported or based on physical examination data as detailed in e-Appendix 1 (519.4KB, pdf) . BMI was drawn from the examination file.
Risk factors for chronic airflow obstruction included asthma history, smoking history, exposure to secondhand smoking, high-risk occupation, high-risk industry, and a surrogate for exposure to air pollution. Asthma history was a self-reported physician diagnosis of the disease. A participant was considered to have experienced dyspnea if he/she responded “Yes” to the question regarding the presence of shortness of breath when hurrying or walking up a slight hill.
Statistical Analysis
ORs for OLD were estimated using logistic regression analysis. The main predictor was ethnicity, with white as the reference group. The covariates were chosen a priori based on prior studies12,14,22 and are listed in e-Appendix 1 (519.4KB, pdf) . Results are also reported as prevalence ratios (also called risk ratios), as the prevalence of OLD was high (26.9%). Race-ethnicity differences in all-cause mortality for OLD cases only were assessed using Cox proportional hazard models. Time to event for all-cause mortality was censored at date of death certificate or at December 31, 2006 (time of last follow-up).23 The covariates included in the Cox model are based on prior investigations23‐26 and are described in e-Appendix 1 (519.4KB, pdf) . We also performed a survival analysis to examine the effects of country of birth and time living in the United States on mortality in Mexican American subjects with OLD. Finally, we performed a sensitivity analysis to address the potential bias of our hazard ratio (HR) estimates based on the assumption that some non-US-born Mexican Americans may have moved back to and died in Mexico without having a US NDI death certificate.27 In secondary analyses, we repeated the main analyses using the lower limit of normal (LLN) of the FEV1/FVC ratio28 and in the subset of subjects with OLD and low lung function defined as FEV1/FVC < 0.7 and FEV1 < 80% of the predicted values.29 All analyses incorporated appropriate sampling weights and were performed with the SAS 9.3 callable SUDAAN 10.1 (RTI International) statistical software.
Results
Compared with whites, Mexican Americans were more likely to be younger, poorer, and have less education and less access to health care. Mexican Americans were more likely to be never smokers and smoke fewer pack-years than whites. Mexican Americans were also more likely to report chronic heart failure and diabetes and less likely to report asthma, hypertension, heart attack, stroke, and cancer. Participants of this ethnicity were more likely to live in urban areas and to work in high-risk occupations or industries (Table 1). Compared with those with complete data (e-Appendix 1 (519.4KB, pdf) ), participants with missing data (n = 904) (e-Fig 1 (519.4KB, pdf) ) were more likely to be older and Mexican American. These participants were also more likely to have ≤ 12 years of school and higher prevalence of self-reported physician diagnoses of both chronic bronchitis and emphysema. There was no difference in sex proportion and lifetime smoking status between these groups.
Table 1.
—Characteristics of Selected Participants by Race/Ethnicity Group (N = 6,456)
| Variable | No. | Non-Hispanic White (n = 4,554) | Mexican American (n = 1,902) | P Value |
| Age, y | < .0001 | |||
| Mean | 6,456 | 57.4 (0.5) | 52.6 (0.3) | |
| ≤ 55 | 2,317 | 49.3 (1.8) | 65.7 (1.2) | |
| 56-70 | 2,110 | 32.0 (1.2) | 27.5 (1.1) | |
| > 70 | 2,029 | 18.7 (1.1) | 6.8 (0.6) | |
| Male sex | 3,126 | 46.9 (0.8) | 48.7 (1.1) | .24 |
| Country of birth | < .0001 | |||
| United States or another country | 5,636 | 99.9 (0.1) | 55.8 (3.0) | |
| Mexico | 810 | a | 44.2 (3.0) | |
| BMI, kg/m2 | < .0001 | |||
| ≤ 18.5 | 101 | 1.7 (0.2) | 4 (0.1) | |
| 18.6-25 | 2,150 | 37.0 (1.2) | 24.1 (1.3) | |
| 25.1-30 | 2,533 | 36.9 (1.0) | 39.5 (1.2) | |
| > 30 | 1,662 | 24.4 (1.1) | 36.0 (1.4) | |
| Education, y | < .0001 | |||
| < 12 | 2,873 | 24.5 (1.5) | 64.8 (2.7) | |
| ≥ 12 | 3,546 | 75.5 (1.5) | 35.2 (2.7) | |
| Family income-to-poverty ratio | < .0001 | |||
| < 1.00 | 921 | 6.0 (0.6) | 29.3 (1.6) | |
| ≥ 1.00 | 4,900 | 94.0 (0.6) | 77 (1.6) | |
| Access to health care | 5,517 | 86.5 (1.0) | 75.7 (1.6) | < .0001 |
| Language at interview | < .0001 | |||
| English | 5,464 | 99.9 (0.1) | 53.7 (3.0) | |
| Spanish | 979 | a | 46.3 (3.0) | |
| Self-reported asthma | 431 | 7.7 (0.5) | 6.0 (0.7) | .04 |
| Smoking status | < .0001 | |||
| Never smoker | 2,890 | 40.2 (1.0) | 49.2 (1.0) | |
| Former smoker | 2,355 | 37.8 (1.0) | 38 (1.0) | |
| Current smoker | 1,211 | 22.1 (1.0) | 20 (1.1) | |
| Pack-y of smoking | < .0001 | |||
| Mean | 3,282 | 30.4 (0.7) | 18.4 (1.5) | |
| < 1 | 2,923 | 42.4 (0.9) | 52.3 (1.1) | |
| 1-19 | 1,538 | 25.9 (0.7) | 32.1 (0.9) | |
| ≥ 20 | 1,711 | 31.7 (0.9) | 15.7 (1.2) | |
| Secondhand smoking | 2,253 | 41.2 (1.6) | 36.9 (1.8) | .06 |
| Comorbidities | ||||
| Hypertension | 3,031 | 39.4 (1.1) | 34.0 (1.4) | .0006 |
| Heart attack | 510 | 6.2 (0.5) | 3.7 (0.5) | .0003 |
| Chronic heart failure | 346 | 3.1 (0.2) | 4.8 (0.4) | < .0001 |
| Stroke | 283 | 3.3 (0.3) | 1.8 (0.2) | .0002 |
| Diabetes | 749 | 7.3 (0.5) | 14.2 (0.8) | < .0001 |
| Cancer | 420 | 6.3 (0.4) | 2.3 (0.5) | < .0001 |
| Living in urban area | 2,678 | 43.7 (4.8) | 56.0 (5.9) | .04 |
| High-risk industry | 2,614 | 36.6 (1.5) | 44.2 (1.4) | .0003 |
| High-risk occupation | 1,817 | 22.0 (1.0) | 35.2 (1.4) | < .0001 |
| Shortness of breath | 1,898 | 29.6 (1.3) | 28.0 (1.5) | .38 |
| FEV1, mL | 6,456 | 2,805 (27) | 2,832 (18) | .36 |
| FEV1 % predicted | 6,456 | 93 (0.5) | 97 (0.4) | < .0001 |
| FEV1/FVC | 6,456 | 0.74 (0.002) | 78 (0.002) | < .0001 |
Data are presented as weighted % (SE) for categorical variables and as weighted mean (SE) for continuous variables. Percents do not sum up 100% for some variables because of rounding. Missing data: country of birth, 10; BMI, 10; education, 37; family income-to-poverty ratio, 635; access to health care, 1; language spoken at interview, 13; lifetime asthma status, 1; pack-y smoked, 284; secondhand smoke exposure, 4; heart attack, 80, diabetes, 7, shortness of breath, 34. Data from NHANES III, Third National Health and Nutrition Examination Survey (1988-1994), National Center for Health Statistics.18
This estimate does not meet the standard statistical reliability and precision (relative SE ≥ 30%).
The prevalence of OLD was lower among Mexican Americans than whites (No., [weighted % ± SE], 302 [12.7% ± 0.7%] vs 1,432 [24.7% ± 0.7%]). Differences in OLD prevalence between these populations were slightly greater when using alternate definitions (e-Table 1 (519.4KB, pdf) ). In univariate analysis, Mexican Americans had lower odds of OLD than whites (e-Table 2 (519.4KB, pdf) ). In the full model, the odds of having OLD for Mexican Americans was attenuated but remained significant (OR, 0.72 [95% CI, 0.54-0.95]) (Table 2). Prevalence ratios of OLD for Mexican Americans were comparable to ORs (e-Table 3 (519.4KB, pdf) ). Other results when we added smoking duration and age at start of smoking or country of birth to this model and when the model was performed only among smokers are shown in the Results section of e-Appendix 1 (519.4KB, pdf) . The ORs were comparable with those of the main analysis.
Table 2.
—Multivariate Logistic Analysis Predicting OLD
| 95% CI | ||||
| Variable | OR | Lower Limit | Upper Limit | P Value |
| Race/ethnicity | .02 | |||
| Non-Hispanic white | 1.00 | … | … | |
| Mexican American | 0.72 | 0.54 | 0.95 | |
| Sex | .0001 | |||
| Female | 1.00 | … | … | |
| Male | 1.63 | 1.28 | 2.08 | |
| Age, y | < .0001 | |||
| 40-55 | 1.00 | … | … | |
| 56-70 | 3.44 | 2.76 | 4.27 | |
| > 70 | 6.77 | 5.39 | 8.50 | |
| BMI, kg/m2 | ||||
| ≤ 18.5 | 2.17 | 1.22 | 3.85 | .007 |
| 18.6-24.9 | 1.00 | … | … | … |
| 25-29 | 0.76 | 0.62 | 0.92 | .005 |
| ≥ 30 | 0.54 | 0.41 | 0.70 | < .0001 |
| Self-reported asthma history | < .0001 | |||
| No | 1.00 | … | … | |
| Yes | 3.77 | 2.84 | 5.01 | |
| Smoking status | ||||
| Never smoker | 1.00 | … | … | … |
| Former smoker | 1.45 | 1.09 | 1.93 | .009 |
| Current smoker | 3.87 | 2.67 | 5.59 | < .0001 |
| Pack-y smoked | 1.01 | 1.01 | 1.02 | < .0001 |
OLD is defined as FEV1/FVC < 0.7. The main predictor is the race/ethnic group, where non-Hispanic white was the reference group. All logistic models incorporated sampling weights. The covariates were those showed in the table and education level, family income-to-poverty ratio, access to health care, secondhand smoke exposure, high-risk industry, high-risk occupation, and living in urban area. Data from NHANES III, Third National Health and Nutrition Examination Survey (1988-1994), National Center for Health Statistics.18 OLD = obstructive lung disease.
Among the 1,734 participants with OLD, 1,054 (60.8%) died (Mexican American, 154), and two had missing vital status during a median follow-up of 12.0 years (interquartile range, 6.3-14.6). In an unadjusted Cox model, Mexican Americans had a lower risk of death from all causes than whites (HR, 0.72 [95% CI, 0.53-0.99]) (e-Table 4 (519.4KB, pdf) ). In the full Cox model, survival benefit for Mexican Americans was no longer apparent (HR, 0.88 [95% CI, 0.69-1.13]) (Fig 1, Table 3). When we added comorbidities (ie, cardiovascular disease, diabetes, cancer) to the survival model, the result was similar (HR, 0.89 [95% CI, 0.70-1.14]; P = .35) to that of the smaller model. Similarly, when we included all the participants with missing data who had assumed OLD in the analysis, the result was also comparable (HR 0.85 [95% CI, 0.64-1.13]; P = .25).
Table 3.
—Adjusted Cox Proportional Hazard Model for All-Cause Mortality in OLD Subjects
| Variable | HR | 95% CI | P Value | |
| Lower Limit | Upper Limit | |||
| Race/ethnicity | .31 | |||
| Non-Hispanic white | 1.00 | … | … | |
| Mexican American | 0.88 | 0.69 | 1.13 | |
| Sex | < .0001 | |||
| Female | 1.00 | |||
| Male | 1.50 | 1.25 | 1.79 | |
| Age, y | 1.11 | 1.10 | 1.13 | < .0001 |
| BMI, kg/m2 | ||||
| ≤ 18.5 | 1.83 | 1.03 | 3.26 | .04 |
| 18.6-24.9 | 1.00 | … | … | … |
| 25-29.9 | 0.87 | 0.70 | 1.08 | .19 |
| ≥ 30 | 0.81 | 0.58 | 1.13 | .20 |
| Smoking status | ||||
| Never smoker | 1.00 | … | … | … |
| Former smoker | 1.07 | 0.81 | 1.40 | .64 |
| Current smoker | 1.70 | 1.23 | 2.35 | .002 |
| Pack-years smoked | 1.002 | 1.000 | 1.004 | .02 |
| FEV1 % predicted | 0.98 | 0.98 | 0.99 | < .0001 |
The main predictor for all the models is the race/ethnic group, where non-Hispanic white was the reference group. The survival model incorporated sampling weights. The HR calculation was made with ascertainment of death based on US death certificates. See e-Table 7 (519.4KB, pdf) for HR estimates assuming that some non-US-born Mexican Americans may have moved back to and died in Mexico (thus, with no US death certificate). The covariates included were those showed in the table and education level, asthma, age of asthma diagnosis (< 18 years old = 1), and dyspnea. Data from NHANES III, Third National Health and Nutrition Examination Survey (1988-1994), National Center for Health Statistics18 and its Linked Mortality File, National Center for Health Statistics.19 HR = hazard ratio. See Table 2 legend for expansion of other abbreviation.
Among 302 Mexican Americans with OLD, 68 out of 142 (47.9%) Mexican-born died compared with 85 out of 159 (53.5%) US-born Mexican Americans. One participant of this ethnicity did not report the country of birth. The survival analysis showed no difference in all-cause mortality between Mexican-born and US-born Mexican Americans (HR, 0.87 [95% CI, 0.54-1.40]). There was no relationship between time living in the United States and mortality among non-US-born Mexican Americans in adjusted models (e-Appendix 1 (519.4KB, pdf) ).
In secondary analyses, using the LLN for the FEV1/FVC ratio to define OLD (n = 1,047), Mexican Americans had lower odds of OLD than whites (OR, 0.61 [95% CI, 0.45-0.84]) (e-Table 5 (519.4KB, pdf) ). Similarly in the multivariable Cox model, there was no survival benefit for Mexican Americans (HR, 0.92 [95% CI, 0.67-1.26]). Results were also consistent in the subset of subjects with OLD and low lung function (n = 811); Mexican Americans again had lower odds of OLD and low lung function than their white counterparts (OR, 0.66 [95% CI, 0.46-0.95]) (e-Table 6 (519.4KB, pdf) ). Finally, Mexican American and white subjects with OLD and low lung function had no differences in mortality (HR, 0.83 [95% CI, 0.58-1.19])
Finally, the results of the sensitivity analysis are shown in e-Table 7 (519.4KB, pdf) . When we assumed increasing return migration rates for non-US-born Mexican Americans, there was a nonsignificant trend to increase all-cause mortality of participants of this ethnicity with OLD compared with whites (HR from 0.98 to 1.23; P value from .87 to .10).
Discussion
In this study of a nationally representative sample of US adults with long-term mortality follow-up, we found that Mexican Americans had a lower likelihood of OLD diagnosis compared with whites. Despite having a lower odds of OLD diagnosis, Mexican Americans with OLD had no difference in mortality compared with whites.
Our study shows that Mexican Americans have lower odds of OLD than their white counterparts. This finding confirms prior findings of Hispanics in New Mexico and extends them in several ways.10,12 First, unlike previous studies, we used a nationally representative sample of Mexican Americans, including foreign-born and US-born subjects as well as both English and Spanish speakers. This allowed us to obtain estimates generalizable to the largest subgroup of US Hispanics. We also used two definitions of OLD and performed the analysis in the subset of subjects with OLD and low lung function only and obtained similar results, which substantiates our main findings. We accounted for several factors that might confound or modify the association between the Mexican American group and OLD, including relevant demographic information (country of birth), socioeconomic status (access to health care), and chronic airflow obstruction risk factors (history of asthma, secondhand smoke exposure, occupational exposures). Although the odds of OLD in Mexican Americans were attenuated after these factors were accounted for, this Hispanic subgroup was still 28% less likely to have OLD than whites. A recent multiethnic study using prebronchodilator data,30 however, did not find differences in the effect of Hispanic ethnicity (vs whites) on the relationship between smoking and FEV1 or OLD defined as the LLN. One of the differences between that and our study is that they included multiple subgroups of Hispanics, which may have obscured a potential advantage for Mexican Americans against OLD.
Prior studies support a biologic plausibility for the protective effect of Hispanic ethnicity against chronic airflow obstruction. Lung function is heritable, and Coultas et al31 have shown that the lung function of Hispanic offspring correlates with that of their parents. Sood et al32 and Vollmer et al33 have demonstrated that both Hispanic female and male smokers have higher FEV1 measurements than their respective white counterparts. Additionally, Bruse et al12 suggested that Hispanic subjects may be less susceptible to COPD (a component of OLD), because of protective alleles that may be more frequent in their genetic background (or their Native American ancestry). Moreover, participants from Ciudad de México had the lowest prevalence of COPD among five major Latin American cities included in the PLATINO (Proyecto Latinoamericano de Investigación en Obstrucción Pulmonar) study.34 In our study, the potential protective effect of Mexican American ethnicity against OLD was observed despite differences in demographic, socioeconomic, and chronic airflow obstruction risk factors (including asthma history, lifetime smoking status, pack-years smoked, and occupational exposure) compared with whites. Thus, our findings support prior observations in Hispanics and extend them by showing that the lower susceptibility to the deleterious effects of smoking and environmental factors on lung function and having OLD is observed in the largest subgroup of Hispanics, Mexican Americans. Thus, further research efforts toward understanding the factors associated with protection against OLD in Hispanics are needed.
An important finding in our study was that among Mexican Americans with OLD, no benefit in survival was observed when compared with whites with OLD. This finding suggests that the Hispanic paradox may only apply to having OLD. Prior studies by Samet et al11 and Keppel et al35 reported lower mortality rates of chronic lower respiratory diseases in Hispanics than whites from 1958 to 1982 and from 1990 to 2006, respectively. Unlike these studies, our study provides an all-cause mortality HR estimated from a cohort of participants with OLD with long-term mortality follow-up. Our analysis included clinically relevant covariates, including comorbidities associated with increased risk for mortality from OLD in NHANES participants. A potential explanation for the lack of difference in mortality in our study is that once the obstructive impairment of lung function is acquired, both OLD populations are subject to the effects of a variety of conditions that balance their risk of death in long-term follow-up. In a review of the Hispanic paradox, Markides and Eschbach6 stated that among Hispanic subgroups the survival benefit is greatest for immigrants, which may be due to a “healthy immigrant effect.”36 However, as immigrants stay in the United States longer, their protective health behaviors deteriorate, a process termed “negative acculturation.”37 It is unclear whether country of birth and duration of time living in the United States affect long-term mortality in Mexican Americans with OLD. Our current analysis revealed no difference in all-cause mortality between US- and Mexican-born Mexican Americans with OLD. Further, the apparent survival benefit for those living in the United States < 15 years disappeared after adjustment for age. Thus, the healthy immigrant effect and negative acculturation do not seem to have an impact on all-cause mortality in Mexican Americans with OLD.
Limitations
Caution should be exercised when interpreting these results. First, since NHANES III is a survey, misclassification is possible. However, we used an objective definition of OLD and self-reported race/ethnicity, both accepted means of assessing these variables.30,38,39 As NHANES III had only prebronchodilator spirometric values, we may have overestimated the OLD prevalence; however, doing so would not likely have affected the difference we observed between the two populations. Although OLD includes various conditions like asthma and COPD, these obstructive airway diseases share similar genetic and epidemiologic risk factors.40 The association between Mexican American ethnicity and OLD may be biased due to residual confounding by exposure to risk factors for chronic airflow obstruction, including characteristics of smoking (cigarette type, depth of inhalation). Although we accounted for nonsmoking risk factors in our models, their assessments were based on self-reported or possibly imprecise indicators (eg, the surrogate for air pollution), which may not completely capture the exposure to nonsmoking environmental risk factors for chronic airflow obstruction. Further, a number of Mexican Americans may have moved back to and died in Mexico without having an NDI death certificate. They would have been censored and assumed to be alive, which would bias our HR estimates toward a survival advantage for Mexican Americans. Our analysis assuming increasing percentages of non-US-born Mexican Americans emigrated to Mexico and subsequently died there also revealed no survival benefit for Mexican American ethnicity. Additionally, since the survival analysis was performed in subjects with OLD only, the restriction in sample size may have obscured a potential advantage in mortality among Mexican Americans. Similarly, this limitation may have masked differences in mortality between non-US- and US-born Mexican Americans and between immigrants living a short vs long time in the United States. Further research with larger Hispanic cohorts and closer follow-up may provide more definitive conclusions. Finally, because of a relatively small number of deaths due to chronic respiratory conditions, we could not estimate respiratory-specific mortality.
Conclusions
In summary, our study suggests that although Mexican Americans seem to be protected from having OLD, those with OLD do not appear to have a survival benefit. More studies are needed to elucidate the Hispanic paradox in OLD, particularly the mechanisms mediating the lower risk for airway obstruction in Hispanics.
Supplementary Material
Online Supplement
Acknowledgments
Author contributions: Dr Diaz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Dr Diaz: contributed to conception and design of the study; acquisition of data; analysis and interpretation; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Dr Come: contributed to conception and design of the study; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Dr Mannino: contributed to conception and design of the study; analysis and interpretation; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Dr Pinto-Plata: contributed to conception and design of this study and creation, revision, and final approval of the manuscript.
Dr Divo: contributed to conception and design of this study and creation, revision, and final approval of the manuscript.
Dr Bigelow: contributed to conception and design of the study; analysis and interpretation; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Dr Celli: contributed to conception and design of the study; analysis and interpretation; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Dr Washko: contributed to conception and design of the study; analysis and interpretation; drafting the manuscript for important intellectual content; and creation, revision, and final approval of this manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Mannino has received honoraria/consulting fees and served on speaker bureaus for GlaxoSmithKline, Novartis Corporation, Pfizer Inc, AstraZeneca, Forest Laboratories, Inc, and Creative Educational Concepts. Furthermore, he has received royalties from UpToDate, Inc. Dr Celli is on the advisory boards of GlaxoSmithKline, Boehringer-Ingelheim GmbH, AstraZeneca, and Almirall, SA. He also has a grant from AstraZeneca to study cardiac function in patients with COPD. Dr Washko has received consulting fees from Spiration, Inc, and his spouse is an employee of Merck & Co, Inc. Drs Diaz, Come, Pinto-Plata, Divo, and Bigelow have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Additional information: The e-Appendix, e-Figure, and e-Tables can be found in the “Supplemental Materials” area of the online article.
Abbreviations
- HR
hazard ratio
- LLN
lower limit of normal
- NDI
National Death Index
- NHANES
National Health and Nutrition Examination Survey
- OLD
obstructive lung disease
Footnotes
Funding/Support: Dr Diaz is supported by National Institutes of Health [Grant 1K01 HL118714-01] and the 2013 Brigham and Women’s Hospital Minority Career Development Award.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB. Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination surveys from 1988-1994 to 2007-2010. Chest. 2013;143(5):1395-1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miniño AM, Murphy SL, Xu J, Kochanek KD. Deaths: final data for 2008. Natl Vital Stat Rep. 2011;59(10):1-126 [PubMed] [Google Scholar]
- 3.Humes KR, Jones NA, Ramirez RR. Overview of the race and origin Hispanic: 2010. 2010 Census brief. US Census Bureau website. 2011. http://www.census.gov/prod/cen2010/briefs/c2010br-02.pdf. Accessed January 30, 2012
- 4.Brehm JM, Celedón JC. Chronic obstructive pulmonary disease in Hispanics. Am J Respir Crit Care Med. 2008;177(5):473-478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101(3):253-265 [PMC free article] [PubMed] [Google Scholar]
- 6.Markides KS, Eschbach K. Aging, migration, and mortality: current status of research on the Hispanic paradox. J Gerontol B Psychol Sci Soc Sci. 2005;60(Spec No 2):68-75 [DOI] [PubMed] [Google Scholar]
- 7.Brown HL, Chireau MV, Jallah Y, Howard D. The “Hispanic paradox”: an investigation of racial disparity in pregnancy outcomes at a tertiary care medical center. Am J Obstet Gynecol. 2007;197(2):197.e1-e7 [DOI] [PubMed] [Google Scholar]
- 8.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W. Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers. 2009;77(6):1707-1746 [DOI] [PubMed] [Google Scholar]
- 9.Vega WA, Rodriguez MA, Gruskin E. Health disparities in the Latino population. Epidemiol Rev. 2009;31:99-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samet JM, Schrag SD, Howard CA, Key CR, Pathak DR. Respiratory disease in a New Mexico population sample of Hispanic and non-Hispanic whites. Am Rev Respir Dis. 1982;125(2):152-157 [DOI] [PubMed] [Google Scholar]
- 11.Samet JM, Wiggins CL, Key CR, Becker TM. Mortality from lung cancer and chronic obstructive pulmonary disease in New Mexico, 1958-82. Am J Public Health. 1988;78(9):1182-1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruse S, Sood A, Petersen H, et al. New Mexican Hispanic smokers have lower odds of chronic obstructive pulmonary disease and less decline in lung function than non-Hispanic whites. Am J Respir Crit Care Med. 2011;184(11):1254-1260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Drummond MB. The Hispanic paradox unraveled? Am J Respir Crit Care Med. 2011;184(11):1222-1223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hnizdo E, Sullivan PA, Bang KM, Wagner G. Airflow obstruction attributable to work in industry and occupation among US race/ethnic groups: a study of NHANES III data. Am J Ind Med. 2004;46(2):126-135 [DOI] [PubMed] [Google Scholar]
- 15.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum Biol. 2002;74(1):83-109 [DOI] [PubMed] [Google Scholar]
- 16.Sundquist J, Winkleby M. Country of birth, acculturation status and abdominal obesity in a national sample of Mexican-American women and men. Int J Epidemiol. 2000;29(3):470-477 [PubMed] [Google Scholar]
- 17.Diaz AA, Come CE, Mannino DM, et al. COPD in Mexican-Americans and non-Hispanic whites: an analysis of diagnosis and survival in the Third National Health and Nutrition Survey (NHANES III); follow-up study [abstract]. Am J Respir Crit Care Med. 2013;187:A3646 [Google Scholar]
- 18.National Center for Health Statistics Plan and operation of the Third National Health and Nutrition Examination Survey, 1988-1994. Vital Health Stat 1. 1994;1(32). http://www.cdc.gov/nchs/data/series/sr_01/sr01_032.pdf. DHHS Publication No. (PHS) 94-1308. Published 1994. Accessed January 31, 2012 [PubMed] [Google Scholar]
- 19.NHANES III linked mortality file Centers for Disease Prevention and Control website. http://www.cdc.gov/nchs/data_access/data_linkage/mortality/nhanes3_linkage.htm. Accessed January 31, 2012
- 20.Agusti A, Calverley PM, Celli B, et al. ; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:12220831787 [Google Scholar]
- 21.Statement of the American Thoracic Society Standardization of spirometry—1987 update. Am Rev Respir Dis. 1987;136(5):1285-1298 [DOI] [PubMed] [Google Scholar]
- 22.Eisner MD, Anthonisen N, Coultas D, et al. ; Committee on Nonsmoking COPD, Environmental and Occupational Health Assembly An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(5):693-718 [DOI] [PubMed] [Google Scholar]
- 23.Diaz-Guzman E, Khosravi M, Mannino DM. Asthma, chronic obstructive pulmonary disease, and mortality in the US population. COPD. 2011;8(6):400-407 [DOI] [PubMed] [Google Scholar]
- 24.Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368(4):351-364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012 [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Mannino DM, Zhao G, Li C, Croft JB. Changes in mortality among US adults with COPD in two national cohorts recruited from 1971-1975 and 1988-1994. Chest. 2012;141(1):101-110 [DOI] [PubMed] [Google Scholar]
- 27.Jasso G, Rosenzweig MR. Estimating the emigration rates of legal immigrants using administrative and survey data: the 1971 cohort of immigrants to the United States. Demography. 1982;19(3):279-290 [PubMed] [Google Scholar]
- 28.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159(1):179-187 [DOI] [PubMed] [Google Scholar]
- 29.Mannino DM, Gagnon RC, Petty TL, Lydick E. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988-1994. Arch Intern Med. 2000;160(11):1683-1689 [DOI] [PubMed] [Google Scholar]
- 30.Powell R, Davidson D, Divers J, et al. Genetic ancestry and the relationship of cigarette smoking to lung function and per cent emphysema in four race/ethnic groups: a cross-sectional study. Thorax. 2013;68(7):634-642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coultas DB, Hanis CL, Howard CA, Skipper BJ, Samet JM. Heritability of ventilatory function in smoking and nonsmoking New Mexico Hispanics. Am Rev Respir Dis. 1991;144(4):770-775 [DOI] [PubMed] [Google Scholar]
- 32.Sood A, Stidley CA, Picchi MA, et al. Difference in airflow obstruction between Hispanic and non-Hispanic white female smokers. COPD. 2008;5(5):274-281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vollmer WM, Enright PL, Pedula KL, et al. Race and gender differences in the effects of smoking on lung function. Chest. 2000;117(3):764-772 [DOI] [PubMed] [Google Scholar]
- 34.Menezes AM, Perez-Padilla R, Jardim JR, et al. ; PLATINO Team Chronic obstructive pulmonary disease in five Latin American cities (the PLATINO study): a prevalence study. Lancet. 2005;366(9500):1875-1881 [DOI] [PubMed] [Google Scholar]
- 35.Keppel KG, Pearcy JN, Heron MP. Is there progress toward eliminating racial/ethnic disparities in the leading causes of death? Public Health Rep. 2010;125(5):689-697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harhay MO. The Hispanic paradox and chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(11):1246. [DOI] [PubMed] [Google Scholar]
- 37.Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med. 2005;29(2):143-148 [DOI] [PubMed] [Google Scholar]
- 38.Winker MA. Measuring race and ethnicity: why and how? JAMA. 2004;292(13):1612-1614 [DOI] [PubMed] [Google Scholar]
- 39.Garcia-Aymerich J, Serra Pons I, Mannino DM, Maas AK, Miller DP, Davis KJ. Lung function impairment, COPD hospitalisations and subsequent mortality. Thorax. 2011;66(7):585-590 [DOI] [PubMed] [Google Scholar]
- 40.Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64(8):728-735 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement