Abstract
BACKGROUND
The role of bracing in patients with adolescent idiopathic scoliosis who are at risk for curve progression and eventual surgery is controversial.
METHODS
We conducted a multicenter study that included patients with typical indications for bracing due to their age, skeletal immaturity, and degree of scoliosis. Both a randomized cohort and a preference cohort were enrolled. Of 242 patients included in the analysis, 116 were randomly assigned to bracing or observation, and 126 chose between bracing and observation. Patients in the bracing group were instructed to wear the brace at least 18 hours per day. The primary outcomes were curve progression to 50 degrees or more (treatment failure) and skeletal maturity without this degree of curve progression (treatment success).
RESULTS
The trial was stopped early owing to the efficacy of bracing. In an analysis that included both the randomized and preference cohorts, the rate of treatment success was 72% after bracing, as compared with 48% after observation (propensity-score–adjusted odds ratio for treatment success, 1.93; 95% confidence interval [CI], 1.08 to 3.46). In the intention-to-treat analysis, the rate of treatment success was 75% among patients randomly assigned to bracing, as compared with 42% among those randomly assigned to observation (odds ratio, 4.11; 95% CI, 1.85 to 9.16). There was a significant positive association between hours of brace wear and rate of treatment success (P<0.001).
CONCLUSIONS
Bracing significantly decreased the progression of high-risk curves to the threshold for surgery in patients with adolescent idiopathic scoliosis. The benefit increased with longer hours of brace wear. (Funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases and others; BRAIST ClinicalTrials.gov number, NCT00448448.)
A DOLESCENT IDIOPATHIC SCOLIOSIS IS characterized by a lateral curvature of the spine with a Cobb angle of more than 10 degrees and vertebral rotation. Whereas scoliosis develops in approximately 3% of children younger than 16 years of age, only 0.3 to 0.5% have progressive curves requiring treatment.1 Curves larger than 50 degrees are associated with a high risk of continued worsening throughout adulthood and thus usually indicate the need for surgery.2 In the United States in 2009, there were more than 3600 hospital discharges for spinal surgery to correct adolescent idiopathic scoliosis, the total costs of which (approximately $514 million) ranked second only to appendicitis among children 10 to 17 years of age.3
Treatment with rigid bracing (thoracolumbosacral orthosis) is the most common nonoperative treatment for the prevention of curve progression. There are many different brace designs, but with all of them, the objective is to restore the normal contours and alignment of the spine by means of external forces and, in some designs, the stimulation of active correction as the patient moves the spine away from pressures within the brace.
Studies of bracing in adolescent idiopathic scoliosis have suggested that bracing decreases the risk of curve progression.4-10 However, the results were inconsistent, the studies were observational, and only one prospective study enrolled both patients who underwent bracing and those who did not.11,12 Thus, the effect of bracing on curve progression and rate of surgery has remained unclear. We conducted the Bracing in Adolescent Idiopathic Scoliosis Trial (BRAIST) to determine the effectiveness of bracing, as compared with observation, in preventing progression of the curve to 50 degrees or more (a common indication for surgery).
METHODS
STUDY DESIGN
We conducted BRAIST in 25 institutions across the United States and Canada. Enrollment began in March 2007. Initially, the trial was designed solely as a randomized trial. However, enrollment was slower than anticipated, because centers screened fewer eligible patients than anticipated and fewer families accepted randomization than the expected frequency of 25% of those approached. Since the main reason for declining randomization was a stated preference for one treatment over the other, a preference group was added to the trial in November 2009, which allowed patients to participate by choosing their own treatment. Therefore, the final design included both a randomized cohort and a preference cohort, with identical inclusion criteria, protocols, and outcomes assessments (Fig. S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Enrollment was completed in February 2011.
The study was approved by the human subjects committee at each institution and was overseen by an independent data and safety monitoring board appointed by the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The first and second authors take full responsibility for the completeness and integrity of the data reported and for the adherence of the study to the protocol, available at NEJM.org. Additional information about the study initiation and progress is available elsewhere.13 The statistical analysis plan is available with the protocol.
PATIENT POPULATION
The target population for this study was patients with high-risk adolescent idiopathic scoliosis who met current indications for brace treatment: an age of 10 to 15 years, skeletal immaturity (defined as a Risser grade [a measure of the amount of ossification and eventual fusion of the iliac apophysis, on a scale of 0 to 5, with higher grades indicating greater skeletal maturity] of 0, 1, or 214), and a Cobb angle for the largest curve of 20 to 40 degrees.15 To be eligible, patients could not have received previous treatment for adolescent idiopathic scoliosis (Table S2 in the Supplementary Appendix). Eligibility was determined by the local investigators. Standard information about the trial was presented to eligible patients by means of an online education module.
Patients who declined participation in the study were registered as screened, and their age, sex, race and ethnic group, curve type,16 Cobb angle of the largest curve, and reason for declining were recorded in a Web-based enrollment system. Patients providing assent to randomization received a computer-generated assignment to bracing or observation, which was stratified according to curve type (single thoracic curve vs. all other curves); patients in the preference cohort chose bracing or observation. Written informed consent from the parent or guardian was required before any study procedures were initiated.
STUDY INTERVENTIONS
Patients in the observation group received no specific treatment. Patients in the bracing group received a rigid thoracolumbosacral orthosis, prescribed to be worn for a minimum of 18 hours per day. Participating centers prescribed the type of brace used in their normal clinical practice. Wear time was determined by means of a temperature logger (StowAway or TidbiT data logger, Onset Computer) embedded in the brace and programmed to log the date, time, and temperature every 15 minutes. A temperature of 28.0°C (82.4°F) or higher17,18 indicated that the brace was being worn. Patients who received a brace were considered to be treated, regardless of their level of compliance with prescribed brace wear.
Both patients and clinicians were aware of the assigned treatment. However, all radiographic evaluations and outcome determinations were made at the central coordinating center by two readers (a research associate and a musculoskeletal radiologist) who were unaware of the treatment assignment and the treatment received.
DATA-COLLECTION AND FOLLOW-UP PERIODS
We collected radiographic, clinical, orthotic, and self-reported data at 6-month intervals. Adverse events and quality-of-life scores were monitored at each follow-up assessment and reported to the data and safety monitoring board. A complete list of these data is provided in Table S3 in the Supplementary Appendix. The type of brace (Boston, Wilmington, or one of several other designs), specific customizations, and modifications over time were recorded. Temperature-monitor data were downloaded every 6 months by the research coordinator.
OUTCOMES
The primary outcome was determined when the first of two conditions was met: curve progression to 50 degrees or more (treatment failure) or skeletal maturity without this degree of curve progression (treatment success). The original maturity outcome was based on the change in vertical height, with adjustment for the change in the Cobb angle.19 Owing to concerns regarding the accuracy and reliability of this measure, maturity was redefined as a Risser grade of 4 for girls (75 to 100% ossification of the iliac apophysis, corresponding to near-cessation of growth) or 5 for boys (100% ossification of the apophysis with fusion to the ilium) and a Sanders digital maturity stage of 7 (defined as closure of all physes of the phalanges).20 This change was made before any analysis of the data. In the case of disagreement between the two primary readers regarding the treatment outcome, a third reader who was unaware of the treatment assignment and the treatment received broke the tie.
The score on the Pediatric Quality of Life Inventory (PedsQL), a generic quality-of-life instrument used in studies of acute and chronic illness, was a secondary outcome.21,22 PedsQL scores range from 0 to 100, with higher scores indicating a better quality of life. Other secondary outcomes (not reported here) included health and functioning,23 self-image,24 and perception of spinal appearance.25
STATISTICAL ANALYSIS
The initial sample-size calculations assumed randomization and an equal number of patients in each study group. The treatment-failure rate for bracing was set at 15% on the basis of the literature and the consensus of the protocol-development committee. A survey of potential study participants indicated that at least a 50% reduction in the risk of curvature progression warranting surgery would be required for patients to choose bracing,26 so the treatment-failure rate in the observation group was set at 30%. With an alpha level set at 0.05, a power of 90%, and allowance for a 10% loss to follow-up, we calculated that a sample of 384 patients was required.
The statistical analysis plan prespecified a primary analysis that included data from the combined randomized and preference cohorts according to the treatment received and a secondary intention-to-treat analysis that included data only from the randomized cohort. In both analyses, we used logistic regression to estimate the odds ratio for successful treatment (indicated by skeletal maturity with a Cobb angle of <50 degrees) in the bracing group, as compared with the observation group.
In the primary analysis, we used propensity-score adjustment to control for potential selection bias due to nonrandom treatment assignment in the preference cohort.27 The propensity-score–derivation model was constructed with the use of multivariable logistic regression, with bracing as the dependent variable. We made an a priori decision to include the baseline age and the Cobb angle of the largest curve, along with a variable indicating whether the patient had undergone randomization. Additional variables, with no missing values, that were unbalanced between the study groups at a significance level of 0.05 were also considered for inclusion. The treatment effect was defined as the odds of success as a function of the treatment received, with adjustment for the duration of follow-up and quintiles of the propensity score.
Prespecified interim analyses were performed as requested by the data and safety monitoring board. The cumulative type I error rate was maintained at the planned level of 0.05 by means of the Lan–DeMets28 spending-function approach with the O’Brien–Fleming29 spending function. In addition to the effectiveness analysis, the data and safety monitoring board requested periodic evaluation of the patients’ first 6 months of temperature-monitor data to assess whether patients were complying with the treatment at a level that would allow us to observe a treatment effect if, in fact, one existed. The average time (in hours) of brace wear per day was calculated and divided into quartiles. The chi-square test was used to assess the association between wear time and the rate of success.
RESULTS
EARLY TERMINATION OF THE EFFECTIVENESS STUDY
The first interim analysis (September 2012) included 178 patients, and the second (January 2013) included 230 patients. The prespecified P value for stopping the study because of efficacy was 0.00821. The primary analysis yielded an adjusted odds ratio of 2.03 (95% confidence interval [CI], 1.12 to 3.68; P = 0.0197), indicating a treatment benefit in favor of bracing. The data and safety monitoring board recommended termination of the trial not only on the basis of this analysis (with the P value close to the prespecified level for study termination) but also on the basis of the results of the intention-to-treat analysis and the observation of a strong positive association between the amount of time spent wearing the brace and the rate of success. The data and safety monitoring board instructed the study team to perform a data lock on all outcomes up to and including the date of the board meeting. The analyses presented in this article were performed with the use of the resulting data set.
CHARACTERISTICS OF THE PATIENTS
Of 1183 patients screened, 1086 met the inclusion criteria and made a decision concerning study participation (Fig. 1). A total of 383 patients (35%) provided assent, with written informed consent provided by a parent or guardian. These patients then either underwent randomization (155 patients [40%]) or declined randomization and instead chose their treatment (228 [60%]). The 383 patients with informed consent and the 703 who declined participation were similar with respect to age and sex distribution, but in the group with informed consent there was a slightly higher percentage of blacks and a slightly lower percentage of patients with a single lumbar curve or both a thoracic and a thoracolumbar curve (Table S4 in the Supplementary Appendix).
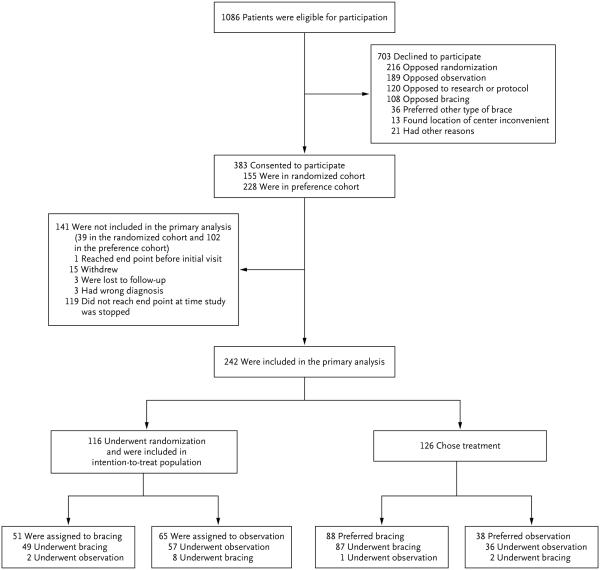
Figure 1. Study Enrollment and Treatment of the Patients.
Between March 2007 and February 2011, a total of 1086 patients underwent screening. Of the 242 patients included in the primary analysis, 116 patients underwent randomization and were included in the intention-to-treat population. A total of 126 patients declined randomization and chose their preferred treatment. Patients were permitted to change treatment groups on request.
PRIMARY ANALYSIS
A total of 242 patients were included in the primary analysis: 116 patients (48%) in the randomized cohort and 126 (52%) in the preference cohort (Table 1). The two cohorts differed significantly at baseline with respect to sex distribution, the interval between the diagnosis of scoliosis and trial enrollment, the person who first noticed the scoliosis, and the largest degree of apical vertebral rotation (Table S5 in the Supplementary Appendix).
Table 1.
Demographic and Clinical Characteristics at Baseline in the Primary-Analysis Population.*
| Characteristic | Study Cohort | As-Treated Group | ||
|---|---|---|---|---|
| Randomized Cohort (N = 116) |
Preference Cohort (N = 126) |
Observation (N = 96) |
Bracing (N = 146) |
|
| Age — yr | 12.7±1.1 | 12.6±1.1 | 12.7±1.2 | 12.7±1.0 |
| Female sex — no. (%) | 101 (87) | 120 (95) | 86 (90) | 135 (92) |
| Race — no. (%)† | ||||
| Black | 15 (13) | 7 (6) | 11 (11) | 11 (8) |
| White | 88 (76) | 101 (80) | 73 (76) | 116 (79) |
| Other | 9 (8) | 8 (6) | 9 (9) | 8 (5) |
| Unknown or not reported | 4 (3) | 10 (8) | 3 (3) | 11 (8) |
| Standing height — cm | 154.4±11.6 | 156.2±7.7 | 153.6±10.6 | 156.5±9.1 |
| SRS curve classification — no. (%) | ||||
| Thoracic | 25 (22) | 34 (27) | 21 (22) | 38 (26) |
| Thoracolumbar | 17 (15) | 15 (12) | 13 (14) | 19 (13) |
| Lumbar | 3 (3) | 6 (5) | 4 (4) | 5 (3) |
| Double major | 38 (33) | 31 (25) | 32 (33) | 37 (25) |
| Double thoracic | 6 (5) | 16 (13) | 7 (7) | 15 (10) |
| Thoracic and thoracolumbar | 20 (17) | 13 (10) | 13 (14) | 20 (14) |
| Triple | 7 (6) | 11 (9) | 6 (6) | 12 (8) |
| Cobb angle of the largest curve — degrees‡ | 30.5±6.0 | 30.3±6.1 | 30.3±6.5 | 30.5±5.8 |
| Risser grade — no./total no. (%)‡§ | ||||
| 0 | 70/115 (61) | 72/125 (58) | 60/94 (64) | 82/146 (56) |
| 1 | 25/115 (22) | 39/125 (31) | 19/94 (20) | 45/146 (31) |
| 2 | 17/115 (15) | 10/125 (8) | 12/94 (13) | 15/146 (10) |
| 3 | 2/115 (2) | 3/125 (2) | 3/94 (3) | 2/146 (1) |
| 4 | 1/115 (1) | 0/125 | 0/94 | 1/146 (1) |
| 5 | 0/115 | 1/125 (1) | 0/94 | 1/146 (1) |
| Coronal balance — cm¶ | 1.6±1.06 | 1.4±1.06 | 1.4±1.0 | 1.6±1.1 |
| Sagittal balance — cm∥ | 3.1±2.8 | 3.0±2.1 | 3.2±2.6 | 3.0±2.0 |
| Kyphosis — degrees | 34.8±11.9 | 33.3±12.7 | 34.6±12.4 | 33.6±12.3 |
| Lordosis — degrees | 59.9±12.3 | 60.2±12.1 | 60.1±12.4 | 59.8±12.1 |
| PedsQL score** | 82.2±14.1 | 84.9±13.4 | 83.3±13.3 | 83.8±14.1 |
Plus−minus values are means ±SD. There were no significant between-group differences at baseline, except for the comparisons of sex in the two study cohorts (P = 0.02) and standing height in the as-treated groups (P=0.03). Data were missing for the following characteristics: Risser grade (for 1 patient in the randomized cohort, 1 in the preference cohort, and 2 in the observation group), coronal balance (for 5 patients in the randomized cohort, 8 patients in the preference cohort, 2 in the observation group, and 11 in the bracing group), sagittal balance (for 10 in the randomized cohort, 21 in the preference cohort, 12 in the observation group, and 19 in the bracing group), kyphosis (for 6 in the randomized cohort, 7 in the preference cohort, 4 in the observation group, and 9 in the bracing group), lordosis (for 6 in the randomized cohort, 7 in the preference cohort, 5 in the observation group, and 8 in the bracing group), and Pediatric Quality of Life Inventory (PedsQL) score (for 6 in the preference cohort, 2 in the observation group, and 4 in the bracing group). SRS denotes Scoliosis Research Society.
Race was self-reported. The “other” category included American Indian, Alaskan Native or First Nations, Asian, and Native Hawaiian or Pacific Islander.
Radiographic measurements were from the centralized reading center. The readers identified 21 patients with radiographic measurements that did not meet the eligibility criteria (1 patient is included in more than one group listed here): a Cobb angle of less than 20 degrees in 3 patients (1 in the randomized cohort, 2 in the preference cohort, 1 in the observation group, and 2 in the bracing group), a Cobb angle of more than 40 degrees in 10 (7 in the randomized cohort, 3 in the preference cohort, 6 in the observation group, and 4 in the bracing group), a Risser grade of 3 or more in 7 (3 in the randomized cohort, 4 in the preference cohort, 3 in the observation group, and 4 in the bracing group), and an unclassifiable Risser grade in 2 (1 in the randomized cohort, 1 in the preference cohort, and 2 in the observation group).
The Risser grade is a measure of the amount of ossification and eventual fusion of the iliac apophysis reflecting skeletal maturity.14 Grades range from 0 to 5, with higher grades indicating greater maturity.
Coronal balance measures the offset of the top of the spine relative to the sacrum in the coronal plane.
Sagittal balance measures the offset of the top of the spine relative to the sacrum in the sagittal plane.
Scores on the PedsQL range from 0 to 100, with higher scores indicating better quality of life.
A total of 146 patients (60%) received a brace, and 96 (40%) underwent observation only. The two study groups were generally similar with respect to baseline characteristics, except that the patients in the bracing group were taller on average than those in the observation group (156.5 cm vs. 153.6 cm, P = 0.03). The propensity-score model included baseline height, Cobb angle of the largest curve, age, and status with respect to randomization. The average duration of follow-up was 21.3 months in the observation group and 24.2 months in the bracing group (P = 0.01).
The rate of treatment success was 72% in the bracing group and 48% in the observation group (Table 2). With adjustment for the propensity-score quintile and duration of follow-up, the odds ratio for a successful outcome associated with bracing was 1.93 (95% CI, 1.08 to 3.46). Additional details of the propensity-score modeling are provided in the Supplementary Appendix.
Table 2.
Odds Ratio for a Successful Outcome of Bracing as Compared with Observation.*
| Analysis* | Observation | Bracing | Odds Ratio (95% CI) |
|---|---|---|---|
| no./total no. (%) | |||
| Primary analysis | 46/96 (48) | 105/146 (72) | 1.93 (1.08–3.46)† |
| Intention-to-treat analysis | 27/65 (42) | 38/51 (75) | 4.11 (1.85–9.16) |
Successful outcome was defined as skeletal maturity without curve progression to 50 degrees or more. The primary analysis included data from patients in the as-treated groups. The intention-to-treat analysis included data only from patients who had undergone randomization.
The analysis was adjusted for propensity-score quintile and duration of follow-up.
INTENTION-TO-TREAT ANALYSIS
A total of 51 patients (44%) in the randomized cohort were assigned to bracing. There were no significant differences at baseline between the bracing and observation groups, except for the degree of lordosis (P = 0.02) (Table 3, and Table S6 in the Supplementary Appendix).
Table 3.
Demographic and Clinical Characteristics at Baseline in the Intention-to-Treat Population.
| Characteristic | Observation (N = 65) |
Bracing (N = 51) |
|---|---|---|
| Age — yr | 12.7±1.2 | 12.6±1.1 |
| Female sex — no. (%) | 56 (86) | 45 (88) |
| Race — no. (%) | ||
| Black | 11 (17) | 4 (8) |
| White | 47 (72) | 41 (80) |
| Other | 5 (8) | 4 (8) |
| Unknown or not reported | 2 (3) | 2 (4) |
| Standing height — cm | 153.8±12.0 | 155.3±11.1 |
| SRS curve classification — no. (%) | ||
| Thoracic | 15 (23) | 10 (20) |
| Thoracolumbar | 7 (11) | 10 (20) |
| Lumbar | 2 (3) | 1 (2) |
| Double major | 24 (37) | 14 (27) |
| Double thoracic | 4 (6) | 2 (4) |
| Thoracic and thoracolumbar | 10 (15) | 10 (20) |
| Triple | 3 (5) | 4 (8) |
| Cobb angle of the largest curve — degrees† |
31.3±6.7 | 29.4±4.7 |
| Risser grade — no./total no. (%)† | ||
| 0 | 41/64 (64) | 29/51 (57) |
| 1 | 14/64 (22) | 11/51 (22) |
| 2 | 7/64 (11) | 10/51 (20) |
| 3 | 2/64 (3) | 0/51 |
| 4 | 0/64 | 1/51 (2) |
| Coronal balance — cm | 1.6±1.0 | 1.7±1.1 |
| Sagittal balance — cm | 3.3±2.6 | 2.9±2.1 |
| Kyphosis — degrees | 34.3±11.7 | 35.2±12.5 |
| Lordosis — degrees | 57.3±12.9 | 62.8±10.8 |
| PedsQL score | 83.0±13.2 | 81.2±15.2 |
There were no significant between-group differences at baseline, except for the degree of lordosis (P=0.02). Data were missing for the following characteristics: Risser grade (for one patient in the observation group), coronal balance (for two patients in the observation group and three in the bracing group), sagittal balance (for five in the observation group and five in the bracing group), kyphosis (for two in the observation group and four in the bracing group), and lordosis (for three in the observation group and three in the bracing group).
Radiographic measurements were from the centralized reading center. The readers identified 12 patients with radiographic measurements that did not meet the eligibility criteria: a Cobb angle of less than 20 degrees in 1 patient in the observation group, a Cobb angle of more than 40 degrees in 7 in the observation group, a Risser grade of 3 or more in 3 (2 patients in the observation group and 1 in the bracing group), and an unclassifiable Risser grade in 1 in the observation group.
The rate of treatment success was 75% among patients randomly assigned to bracing, as compared with 42% among those randomly assigned to observation (unadjusted odds ratio for successful outcome with bracing, 4.11; 95% CI, 1.85 to 9.16) (Table 2). The number needed to treat in order to prevent one case of curve progression warranting surgery was 3.0 (95% CI, 2.0 to 6.2), and the reduction in relative risk with bracing was 56% (95% CI, 26 to 82).
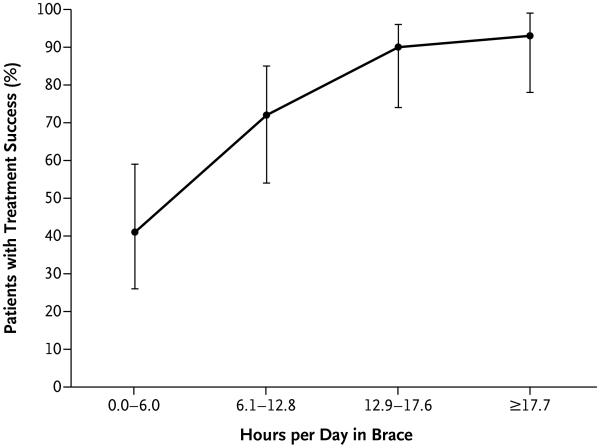
BRACE DOSE–RESPONSE RELATIONSHIP
The majority of patients assigned to bracing (68%) were treated with a customized Boston-type thoracolumbosacral orthosis. Temperature data were available for 116 patients (from both the randomized and preference cohorts). During the first 6 months, patients wore the brace for a mean (±SD) of 12.1±6.5 hours per day (range, 0 to 23.0). The quartile of duration of brace wear was positively associated with the rate of success (P<0.001). The lowest quartile of wear (mean hours per day, 0 to 6.0) was associated with a success rate (41%) similar to that in the observation group in the primary analysis (48%), whereas brace wear for an average of at least 12.9 hours per day was associated with success rates of 90 to 93% (Fig. 2).
Figure 2. Rate of Treatment Success According to Average Hours of Daily Brace Wear.
During the first 6 months, patients wore the brace for a mean (±SD) of 12.1±6.6 hours per day (range, 0 to 23.0). Duration of brace wear was positively associated with the rate of success (P<0.001 by the chi-square test). The lowest quartile of wear (mean hours per day, 0 to 6.0) was associated with a success rate of 42%, whereas brace wear for an average of at least 12.9 hours per day was associated with success rates of 90 to 93%. I bars indicate 95% confidence intervals.
QUALITY OF LIFE AND ADVERSE EVENTS
The average PedsQL scores22 for patients included in the primary and intention-to-treat analyses did not differ significantly between the bracing and observation groups at baseline (Tables 1 and 3) or at the final follow-up assessment (mean scores in the primary analysis, 82.0 and 81.9, respectively; P = 0.97; mean scores in the intention-to-treat analysis, 79.1 and 81.2, respectively; P = 0.45) (Tables S7 and S8 in the Supplementary Appendix). There were no significant differences between the bracing and observation groups in the primary analysis with respect to the percentage of patients with any adverse event (P = 0.32) or the percentage of patients reporting back pain, the most common adverse event (P = 0.29). There was one serious adverse event, a hospitalization for anxiety and depression in a patient who wore a brace. Adverse events involving the skin under the brace were reported in 12 of the 146 patients (8%) who wore a brace.
DISCUSSION
In adolescents with idiopathic scoliosis who were considered to be at high risk for curve progression that would eventually warrant surgery, bracing was associated with a significantly greater likelihood of reaching skeletal maturity with a curve of less than 50 degrees, as compared with observation alone. A significant benefit of bracing was observed in both the randomized and the as-treated populations. We also found a significant association between the average hours of daily brace wear and the likelihood of a successful outcome. These findings corroborate those of previous prospective observational studies, which have shown a significantly lower rate of surgery among patients who wore a brace than among those who were untreated12 and a strong brace dose–response relationship.30
The rates of treatment failure in both groups in the randomized cohort were higher than expected, at 25% with bracing and 58% with observation; we hypothesized that the rates would be 15% and 30%, respectively. In previous studies, the rates of progression warranting surgery have varied widely, ranging from 0 to 79% after bracing 4,12,31 and from 10 to 38% in untreated patients.12,32-34 This variation could be due to differences in case mix, inconsistent indications for surgery, differences in the quality of the brace and in patient compliance with brace wear, and nonblinded outcome evaluation.
Strengths of this study include the objective monitoring of the time spent wearing the brace; blinded, independent determination of the outcome; the diversity of participating sites; and the a priori determination of the magnitude of risk reduction that was considered necessary by patients in order for them to choose bracing. The independent, blinded documentation of the outcome of a large group of untreated patients can serve as a benchmark in future studies of treatment for this condition.
BRAIST began as a randomized trial, but we were aware at the inception of the study that the majority of families would decline participation in order to pursue their own treatment preferences.26 Therefore, the relatively low enrollment rate and the need to include the preference cohort were not unexpected but resulted in a primary analysis that was an as-treated assessment rather than an intention-to-treat assessment. Potential bias due to nonrandom treatment assignment in this analysis is expected to be minimized, but is not eliminated, by the use of propensity-score adjustment. In addition, the brace dose–response analysis may be confounded by factors such as curve type, curve flexibility, and characteristics of the brace. The observation that the intention-to-treat analysis yielded results that were similar to those of the as-treated analysis provides strong support for the conclusion that bracing reduces the risk of curve progression and the need for surgery.
Our findings have direct clinical applicability because they are derived from assessment of a group of patients for whom bracing would have been recommended in a typical orthopedic practice but in the absence of rigorous supporting data. It is also relevant that, in the primary analysis, 48% of the patients in the observation group had a successful outcome, as did 41% of the patients in the bracing group who spent little time actually wearing the brace. As others have suggested,12,35 current bracing indications may be too broad, resulting in unnecessary treatment for many patients. It is important to identify patients at high risk for clinically significant curve progression who are also most likely to benefit from bracing.
In conclusion, bracing significantly decreased the progression of high-risk curves to the threshold for surgery in patients with adolescent idiopathic scoliosis. Longer hours of brace wear were associated with greater benefit.
Supplementary Material
Acknowledgments
Supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R21AR049587 and R01AR052113, to Dr. Weinstein), the Children’s Miracle Network (to Dr. Weinstein), the Canadian Institutes of Health Research (FRN-81050, to Dr. Wright), the Shriners Hospitals for Children (79125, to Dr. Dobbs), the University of Rochester, and the Children’s Mercy Hospitals and Clinics.
We thank the many patients and families who participated in this trial and the research coordinators and staff at the participating institutions.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the official views of any of the funding institutions.
No potential conflict of interest relevant to this article was reported.
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Nachemson AL, Lonstein JE, Weinstein SL. Scoliosis Research Society; Denver: 1982. Report of the Prevalence and Natural History Committee of the Scoliosis Research Society. [Google Scholar]
- 2.Weinstein SL. Ponseti IV. Curve progression in idiopathic scoliosis. J Bone Joint Surg Am. 1983;65:447–55. [PubMed] [Google Scholar]
- 3.HCUP Kids’ Inpatient Database (KID) Healthcare Cost and Utilization Project (HCUP) Agency for Health-care Research and Quality; Rockville, MD: 2009. ( http://www.hcup-us.ahrq.gov/kidoverview.jsp) [Google Scholar]
- 4.Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976) 2007;32(Suppl):S91–S100. doi: 10.1097/BRS.0b013e318134ead9. [DOI] [PubMed] [Google Scholar]
- 5.Dolan LA, Weinstein SL. Best treatment for adolescent idiopathic scoliosis: what do current reviews tell us? In: Wright JG, editor. Evidence-based orthopaedics: the best answers to clinical questions. Saunders; Philadelphia: 2009. [Google Scholar]
- 6.Focarile FA, Bonaldi A, Giarolo MA, Ferrari U, Zilioli E, Ottaviani C. Effectiveness of nonsurgical treatment for idiopathic scoliosis: overview of available evidence. Spine (Phila Pa 1976) 1991;16:395–401. doi: 10.1097/00007632-199104000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Lenssinck ML, Frijlink AC, Berger MY, Bierman-Zeinstra SM, Verkerk K, Verhagen AP. Effect of bracing and other conservative interventions in the treatment of idiopathic scoliosis in adolescents: a systematic review of clinical trials. Phys Ther. 2005;85:1329–39. [PubMed] [Google Scholar]
- 8.Negrini S, Minozzi S, Bettany-Saltikov J, et al. Braces for idiopathic scoliosis in adolescents. Cochrane Database Syst Rev. 2010;1:CD006850. doi: 10.1002/14651858.CD006850.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Rowe DE, Bernstein SM, Riddick MF, Adler F, Emans JB, Gardner-Bonneau D. A meta-analysis of the efficacy of nonoperative treatments for idiopathic scoliosis. J Bone Joint Surg Am. 1997;79:664–74. doi: 10.2106/00004623-199705000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Screening for idiopathic scoliosis in adolescents . Preventive Services Task Force; Rockville, MD: Jun, 2004. ( http://www.uspreventiveservicestaskforce.org/uspstf/uspsaisc.htm) [Google Scholar]
- 11.Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg Am. 1995;77:815–22. doi: 10.2106/00004623-199506000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine (Phila Pa 1976) 2007;32:2198–207. doi: 10.1097/BRS.0b013e31814b851f. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Design of the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST) Spine. 2013 Sep 10; doi: 10.1097/01.brs.0000435048.23726.3e. (Epub ahead of print) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Risser JC. The classic: the iliac apophysis: an invaluable sign in the management of scoliosis — 1958. Clin Orthop Relat Res. 2010;468:643–53. doi: 10.1007/s11999-009-1095-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976) 2005;30:2068–75. doi: 10.1097/01.brs.0000178819.90239.d0. [DOI] [PubMed] [Google Scholar]
- 16.The Terminology Committee of the Scoliosis Research Society A glossary of scoliosis terms. Spine. 1976;1:57–8. [Google Scholar]
- 17.Dolan LA, Weinstein SL, Adams BS. Presented at the Annual Meeting of the Pediatric Orthopaedic Society of North America. Waikaloa, HI: May 3–7, 2010. Temperature as a diagnostic test for compliance with a thoracolumbosacral orthosis. (poster) [Google Scholar]
- 18.Helfenstein A, Lankes M, Ohlert K, et al. The objective determination of compliance in treatment of adolescent idiopathic scoliosis with spinal orthoses. Spine (Phila Pa 1976) 2006;31:339–44. doi: 10.1097/01.brs.0000197412.70050.0d. [DOI] [PubMed] [Google Scholar]
- 19.Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B. 2005;14:320–4. doi: 10.1097/01202412-200509000-00002. [DOI] [PubMed] [Google Scholar]
- 20.Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am. 2008;90:540–53. doi: 10.2106/JBJS.G.00004. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Burwinkle TM, Seid M, Skarr D. The PedsQL 4.0 as a pediatric population health measure: feasibility, reliability, and validity. Ambul Pediatr. 2003;3:329–41. doi: 10.1367/1539-4409(2003)003<0329:tpaapp>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 22.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Landgraf J, Abetz L, Ware J. The Health Institute, New England Medical Center; Boston: 1996. The CHQ user’s manual. [Google Scholar]
- 24.Petersen A, Schulenberg J, Abramowitz R, Offer D, Jarcho H. A self-image questionnaire for young adolescents (SIQYA): reliability and validity. J Youth Adolesc. 1984;13:93–111. doi: 10.1007/BF02089104. [DOI] [PubMed] [Google Scholar]
- 25.Sanders JO, Harrast JJ, Kuklo TR, et al. The Spinal Appearance Questionnaire: results of reliability, validity, and responsiveness testing in patients with idiopathic scoliosis. Spine (Phila Pa 1976) 2007;32:2719–22. doi: 10.1097/BRS.0b013e31815a5959. [DOI] [PubMed] [Google Scholar]
- 26.Dolan LA, Sabesan V, Weinstein SL, Spratt KF. Preference assessment of recruitment into a randomized trial for adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2008;90:2594–605. doi: 10.2106/JBJS.G.01460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 28.Lan KKG, DeMets DL. Changing frequency of interim analysis in sequential monitoring. Biometrics. 1989;45:1017–20. [PubMed] [Google Scholar]
- 29.O’Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35:549–56. [PubMed] [Google Scholar]
- 30.Katz DE, Herring JA, Browne RH, Kelly DM, Birch JG. Brace wear control of curve progression in adolescent idiopathic scoliosis. J Bone Joint Surg Am. 2010;92:1343–52. doi: 10.2106/JBJS.I.01142. [DOI] [PubMed] [Google Scholar]
- 31.Janicki JA, Poe-Kochert C, Armstrong DG, Thompson GH. A comparison of the thoracolumbosacral orthoses and Providence orthosis in the treatment of adolescent idiopathic scoliosis: results using the new SRS inclusion and assessment criteria for bracing studies. J Pediatr Orthop. 2007;27:369–74. doi: 10.1097/01.bpb.0000271331.71857.9a. [DOI] [PubMed] [Google Scholar]
- 32.Fernandez-Feliberti R, Flynn J, Ramirez N, Trautmann M, Alegria M. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop. 1995;15:176–81. [PubMed] [Google Scholar]
- 33.Goldberg CJ, Dowling FE, Hall JE, Emans JB. A statistical comparison between natural history of idiopathic scoliosis and brace treatment in skeletally immature adolescent girls. Spine (Phila Pa 1976) 1993;18:902–8. doi: 10.1097/00007632-199306000-00015. [DOI] [PubMed] [Google Scholar]
- 34.Goldberg CJ, Moore DP, Fogarty EE, Dowling FE. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine (Phila Pa 1976) 2001;26:42–7. doi: 10.1097/00007632-200101010-00009. [DOI] [PubMed] [Google Scholar]
- 35.Sanders JO, Newton PO, Browne RH, Herring AJ. Bracing in adolescent idiopathic scoliosis, surrogate outcomes, and the number needed to treat. J Pediatr Orthop . 2012;32(Suppl 2):S153–S157. doi: 10.1097/BPO.0b013e31825199e5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.