Abstract
The use of endoscopic ultrasonography has allowed for improved detection and pathologic analysis of fine needle aspirate material for pancreatic lesion diagnosis. The molecular analysis of KRAS has further improved the clinical sensitivity of preoperative analysis. For this reason, the use of highly analytical sensitive and specific molecular tests in the analysis of material from fine needle aspirate specimens has become of great importance. In the present study, 60 specimens from endoscopic ultrasonography fine needle aspirate were analyzed for KRAS exon 2 and exon 3 mutations, using three different techniques: Sanger sequencing, allele specific locked nucleic acid PCR and Next Generation sequencing (454 GS-Junior, Roche). Moreover, KRAS was also tested in wild-type samples, starting from DNA obtained from cytological smears after pathological evaluation. Sanger sequencing showed a clinical sensitivity for the detection of the KRAS mutation of 42.1%, allele specific locked nucleic acid of 52.8% and Next Generation of 73.7%. In two wild-type cases the re-sequencing starting from selected material allowed to detect a KRAS mutation, increasing the clinical sensitivity of next generation sequencing to 78.95%. The present study demonstrated that the performance of molecular analysis could be improved by using highly analytical sensitive techniques. The Next Generation Sequencing allowed to increase the clinical sensitivity of the test without decreasing the specificity of the analysis. Moreover we observed that it could be useful to repeat the analysis starting from selectable material, such as cytological smears to avoid false negative results.
Introduction
Pancreatic ductal adenocarcinoma (PDAC) represents the fourth-highest cause of cancer death in the United States with the lowest survival rate among the most common cancers (∼6%) [1]. Several imaging techniques have been developed to improve early diagnosis of pancreatic masses, such as multi-detector-row computed tomography (MDCT), transcutaneous ultrasonography (TUS), magnetic resonance imaging (MRI), endoscopic ultrasonography (EUS), endoscopic retrograde cholangiopancreatography (ERCP) and positron emission tomography (PET) scanning [2]–[4]. Among these techniques, endoscopic ultrasonography guarantees the highest-resolution imaging of the pancreas, allowing for the detection of small masses [5], of lymph node involvement [2] and of vascular tumor infiltration [3]. The introduction of the EUS-guided fine needle aspiration (EUS-FNA) in the clinical practice has supported clinicians in the preoperative diagnosis of pancreatic tumors helping to correctly and promptly selecting patients eligible for a curative surgical intervention or for other treatment [4], [6], [7].
Although EUS-FNA shows high diagnostic clinical sensitivity and specificity, a subset of cases are characterized by limited cellularity or inadequate material for cytologic evaluation [8]. Other than these “unsatisfactory” specimens, inconclusive cytologic cases include those samples described as “suspicious of malignancy” or with “presence of atypical cells” which also represent a significant problem for clinicians and pathologists. The combination of cytologic evaluation and molecular analysis, especially in inconclusive cases, has enhanced the diagnostic power of the EUS-FNA technique [9]–[12].
Mutant KRAS has been reported in >90% of cases of pancreatic ductal adenocarcinoma [13] and in 30 to 45% of cases of intraductal papillary mucinous neoplasm (IPMN), a pre-malignant distinct pathological entity which is thought to be a precursor of PDAC [14]–[17]. KRAS mutations were not detected in acinar carcinomas of the pancreas, in pancreatic neuroendocrine tumors (pNET) or in solid pseudopapillary tumors (SPPT) [18]–[20].
KRAS mutations represent an early genetic event in PDAC pathogenesis and, as regards solid lesions, it is considered a tumor marker for pancreatic adenocarcinoma [21]–[23]. The detection of KRAS mutations in a pancreactic lesion sample is useful to confirm the preoperative diagnosis or to suggest the presence of malignancy in those cases where EUS-FNA cytology is inconclusive [11], [22], [24], [25]. Moreover it has been observed that KRAS point mutations could also occur in chronic pancreatitis and are associated with evolution towards pancreatic cancer [26], [27]. Several techniques could be used for KRAS mutation analysis, including Single-Strand Conformation Polymorphism (SSCP) [9], Restriction Fragment Length Polymorphism (RFLP) assays [28], [29], Enriched-PCR and enzyme Linked Mini-sequence Assay (ELMA-PCR) [30], clamping Peptide Nucleic Acids PCR (PNA-PCR) [31], Allele Specific Locked Nucleic Acid PCR (ASLNAqPCR) [32] and Sanger sequencing [15], [28]. Considering that cytological material obtained from EUS-FNA is often composed of heterogeneous cell populations, it is crucial to make use of accurate and high analytical sensitive molecular tests to detect even a small proportion of mutated cells in a background of wild-type ones [33].
In this work we analyzed the KRAS gene mutational status in 60 consecutive cases of pancreatic lesions starting from material directly collected with EUS-FNA and using three different molecular techniques. We compared Sanger sequencing (considered the gold standard technique for DNA sequence analysis) with two highly analytical sensitive and semi-quantitative techniques: ASLNAqPCR [32] and 454 Next Generation Sequencing (454 GS-Junior platform, Roche). The aim of the present study was to evaluate if a highly analytical sensitive technique could provide more accurate results (meaning fewer false negative and fewer false positive results) in the routine analysis of KRAS in pancreatic lesions. Moreover, considering that usually in pancreatic specimens only mutations in KRAS exon 2 are investigated [15], [20], [28], [34], we tested if it could be useful to analyze also KRAS exon 3 mutations. Finally, taking into consideration that evaluation of cellular composition is not possible from EUS-FNA material directly collected into a tube (“direct” EUS-FNA), we re-tested KRAS starting from cytologic smears and compared the two results, one obtained by targeting selected cells with cytologic atypia and the other directly obtained from EUS-FNA specimens.
Materials and Methods
Selection of Cases
Sixty samples of EUS-FNA obtained from pancreatic lesions were analyzed. According to ecoendoscopy they were classified as solid (31 cases) or cystic (29 lesions) lesions of the pancreas. Patients were 23 male and 37 female, ages ranging from 17 to 84 (mean 66 yrs).
EUS-FNA was performed using a linear echoendoscope (Fujinon, Inc., Saitama, Japan), the aspirated material was smeared on microscope slides for on-site examination or immediately fixed in 95% ethanol for Papanicolaou staining; the remaining material was partly placed in a tube containing 4% formaldehyde solution for cell block preparation and partly in a tube containing 100% ethanol for KRAS analysis (“direct” EUS-FNA material). Cases were diagnosed on preoperative evaluation according to standard criteria as unsatisfactory (C1), negative for malignancy (C2), atypical cells present (C3), suspicious for malignancy (C4) or positive for malignancy (C5) [35]. Regarding the unsatisfactory samples, we decided to distinguish them as C1c if the EUS-FNA was performed on a cystic lesion or C1s if EUS-FNA was performed on solid lesion. We considered C1s, C3 and C4 as inconclusive diagnoses.
Since KRAS mutational analysis is part of the routine diagnostic workup of patients with pancreatic lesions the need for ethic committee’s approval was not necessary for this study, in accordance with medical ethical guidelines of the Azienda Unità Sanitaria Locale di Bologna. Accordingly to these guidelines, a comprehensive written informed consent was signed for the procedure (endoscopic ultrasound fine needle aspiration) that produced the tissue samples. All information regarding the human material was managed using anonymous numerical codes. All samples were handled in compliance with the Helsinki declaration (http://www.wma.net/en/30publications/10policies/b3/).
DNA Extraction and KRAS Analysis
DNA from direct EUS-FNA material or cytological smears was extracted using MasterPure DNA Purification Kit (Epincentre, Madison WI, USA) according to manufacturer’s instruction. DNA from cytoblocks was extracted using High Pure PCR Template Preparation Kit (Roche Diagnostic, Manheim, Germany). Cytological smears were considered evaluable for analysis if at least a hundred of neoplastic cells were present in the slide. The smears were scanned as virtual slides for archiving (ScanScope CS2 Digital Slide Scanner, Aperio, CA, USA) prior to dissecting.
KRAS mutational analysis was performed using three different techniques: Sanger sequencing, Allele Specific Locked Nucleic Acid PCR (ASLNAqPCR) and 454 Next Generation Sequencing (454-NGS).
Sanger sequencing
DNA was amplified using previously described primers [32], purified and sequenced for KRAS exon 2 and exon 3, according manufacturer’s protocol. Sequencing was carried out according to standard procedures using a CEQ2000 XL automatic DNA sequencer (Beckman Coulter, Inc., Fullerton, CA, U.S.A). Strands were analyzed using forward and reverse primers.
Allele specific locked nucleic acid PCR
Mutations in exon 2 were analyzed using ASLNAqPCR optimized for the 7 most common KRAS mutations (G12A, G12C, G12D, G12R, G12S, G12V and G13D) as previously described [32]. The percentage of mutated alleles was calculating according to the following formula [33]:
where R is the “Ratio”, Ct refers to the threshold cycle and Mut and WT refer to mutated and wild-type alleles, respectively. The analytical sensitivity of ASLNAqPCR is below 1%, as previously reported [32].
454 Next-generation sequencing
Sequence analysis of KRAS exon 2 and exon 3 was performed with the 454 GS-Junior Next Generation Sequencer platform (Roche Diagnostics, Mannheim, Germany), according to manufacturers’ instructions. Each target sequence was read at least 300 times (“reads”). KRAS primers were specific for exon 2 (Fw 5′-GGCCTGCTGAAAATGACTGAA-3′; Rv 5′-TGTATCAAAGAATGGTCCTGCAC-3′) and exon 3 (5′-TCTTGGATATTCTCGACACAGCA-3′; 5′-TGCATGGCATTAGCAAAGAC-3′). A sample was considered to be mutated for KRAS only if mutation was present in at least 1% of the consensual reads and in at least 10 of the total reads, according to the 454-NGS analytical sensitivity previously reported [36] and also as determined by serial dilution of KRAS mutated cell lines (OCUT-1) (data not shown).
Follow Up and Final Diagnosis
To determine the performance of the three different techniques, sequencing data were compared with the histological diagnosis for patients that underwent surgery. For patients that were not operated on, sequencing data were compared with a final endpoint based on a combination of clinicopathologic features and follow-up information.
According to final end-point, we distinguished three different categories of lesions: i) benign lesions, ii) adenocarcinomatous lesions (including precursor lesions of adenocarcinoma); iii) not-adenocarcinomatous lesions.
We considered non-neoplastic cysts, pseudocysts and pancreatitis as benign lesions; the inoperable neoplasias with poor progression, PDAC and intraductal papillary mucinous neoplasms (IPMN, both Branch Duct - BD-IPMN - and Main Duct - MD-IPMN) were considered as adenocarcinomatous/preneoplastic lesions; neuroendocrine (pNET) and solid pseudopapillary tumors (SPPT) were considered as not-adenocarcinomatous lesions.
Statistical Measures of Performance
We considered a result as true positive (TP), false positive (FP), true negative (TN) or false negative (FN) as follows. TP were cases when showed a mutation in KRAS and which were PDAC, inoperable neoplasias or IPMN according to final end-point. FP were cases in which a mutation was found but with a “benign” endpoint or else diagnosed as SPPT or pNET. TN were cases that resulted wild-type and with a “benign” endpoint or with an endpoint of neuroendocrine or pseudopapillary neoplasia. FN were cases with a wild-type KRAS but were PDAC/inoperable neoplasias or IPMN at the final end-point.
Test clinical sensitivity (SEN), specificity (SPEC), negative predictive value (NPV), positive predictive value (PPV), accuracy (ACC) and false discovery rate (FDR) were calculated as previously described [32]. Comparisons between clinical sensitivities were performed according to recommendations previously described [37]. Results with a p-value of <0.05 were considered to be statistically significant.
Results
Cytologic results and features, final end-point and KRAS molecular analysis are summarized in Tables 1 and 2.
Table 1. Percentage of mutated KRAS samples according to preoperative cytology evaluation.
| Cytology Diagnosis (number of cases) | KRAS mutated samples | |||||
| 454 NGS (%) | End-point of mutated samples | ASLNA (%) | End-point of mutated samples | Sanger sequencing (%) | End-point of mutated samples | |
| C1 (20) | 8 (40.0) | 6 IPMN (4 BD, 2 MD), 2 NA | 4 (20.0) | 2 IPMN (BD), 2 NA | 4 (20.0) | 3 IPMN (2 BD, 1 MD), 1 NA |
| C1c (17) | 8 (47.1) | 4 (23.5) | 4 (23.5) | |||
| C1s (4) | 0 (0) | 0 (0) | 0 (0) | |||
| C2 (4) | 0 (0) | 0 (0) | 0 (0) | |||
| C3 (2) | 1 (50.0) | Mal. Inop. Neoplasia | 1 (50.0) | 1 Mal. Inop. Neoplasia | 1 (50.0) | 1 Mal. Inop. Neoplasia |
| C4 (9) | 7 (77.8) | 5 PDAC, 1 IPMN (BD), 1Mal. Inop. Neoplasia | 6 (66.7) | 4 PDAC, 1 Mal. Inop.Neoplasia, 1 IPMN (BD) | 5 (55.6) | 3 PDAC, 1 Mal. Inop. Neoplasia, 1 IPMN (BD) |
| C5 (20) | 11 (55.0) | 9 PDAC, 2 Mal. Inop. Neoplasia | 10 (50.0) | 8 PDAC, 2 Mal. Inop.Neoplasia | 6 (30.0) | 5 PDAC, 1 Mal. Inop. Neoplasia |
| C5 PDAC (13) | 11 (84.6) | 10 (76.9) | 6 (46.2) | |||
| C5 Not PDAC. (7) | 0 (0) | 0 (0) | 0 (0) | |||
| NA (5) | 4 (80.0) | 3 IPMN (2 BD, 1 MD), 1 NA | 3 (60.0) | 2 IPMN (1 BD, 1 MD), 1 NA | 1 (20.0) | 1 IPMN (BD) |
| TOTAL (60) | 31 (51.7) | 24 (40.0) | 17 (28.3) | |||
ASLNAqPCR, Allele Specific Locked Nucleic Acid qPCR; NGS, Next Generation Sequencing; PDAC, Pancreatic Ductal AdenoCarcinoma; Not PDAC, malignant neoplasia but not Pancreatic Ductal Adenocarcinoma; NA, cytology not available.
Table 2. Percentage of mutated KRAS samples according to different techniques per final end-point.
| Number of KRAS mutated samples using: | |||
| Final End-Point | 454 NGS (%) | ASLNAqPCR (%) | Sanger (%) |
| Adenocarcinomatous and pre-neoplastic lesions (n = 38) | 28 (73.7) | 21 (55.3) | 16 (42.1) |
| PDAC (n = 20) | 14 (70) | 12 (60) | 8 (40) |
| IPMN (n = 12) | 10 (83.3) | 5 (41.7) | 5 (41.7) |
| Inop. Neoplasia (n = 6) | 4 (66.7) | 4 (66.7) | 3 (50) |
| Not-adenocarcinomatous lesions (n = 7) | 0 (0) | 0 (0) | 0 (0) |
| pNET (n = 5) | 0 (0) | 0 (0) | 0 (0) |
| SPPT (n = 2) | 0 (0) | 0 (0) | 0 (0) |
| Benign Lesions (n = 12) | 0 (0) | 0 (0) | 0 (0) |
| NA (n = 3) | 3 (100) | 3 (100) | 1 (33.3) |
PDAC, Pancreatic Ductal AdenoCarcinoma; IPMN, Intraducatal Pancreatc Mucinous Neoplasia; Inop. Neoplasia, Malignant inoperable neoplasia; pNET, pancreatic NeuroEndocrine Tumor; SPPT, Solid PseudoPapillary Tumor; NA, end-point not available.
Cytologic Evaluation (Table 1)
Material for cytologic evaluation was available for 55 cases. According to preoperative cytology diagnosis, specimens were classified as follows: unsatisfactory (C1, 20 cases), negative for malignancy (C2, 4 cases), atypical cells present (C3, 2 cases), suspicious for malignancy (C4, 9 cases), positive for malignancy (C5, 20 cases). Among the latter, 13 were PDAC, 5 were pNET and 2 were SPPT. The samples diagnosed as C1 were considered C1c (17 cases) if the EUS-FNA material was obtained from a cystic lesion or C1s (3 cases) if it was evaluated from a solid lesion. A virtual slide of one of the specimens analyzed is available at the following address: http://vetrinodigitale.ausl.bo.it/spectrum_Login.php (username and password are available upon request).
KRAS Sequencing in Direct EUS-FNA Material (Tables 1–2)
Sanger sequencing
Using Sanger sequencing, 17 of 60 samples (28.3%) showed a mutation in KRAS exon 2 (15 of 60 cases, 25%) or in the exon 3 (2 of 60 cases, 3.3%) (Figures 1–2).
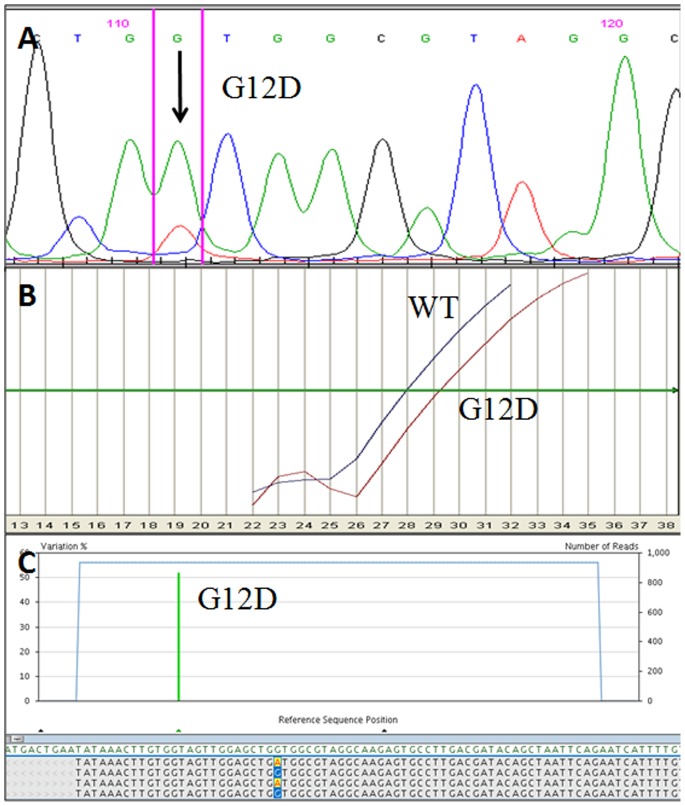
Figure 1. Example of molecular results in a KRAS exon 2 mutated sample.
A) Electropherogram obtained using Sanger sequencing. The KRAS G12D mutation is identified by the smaller peak pointed by the arrow. B) Using ASLNAqPCR results the KRAS G12D mutation is identified by the right curve (G12D). The left curve indicates the wild-type allele (WT). C) Profile obtained using 454-NGS, the KRAS G12D mutation is identified by the vertical green bar. The percentage of mutated alleles is indicated on the left y axis while the total number of reads on the right one.
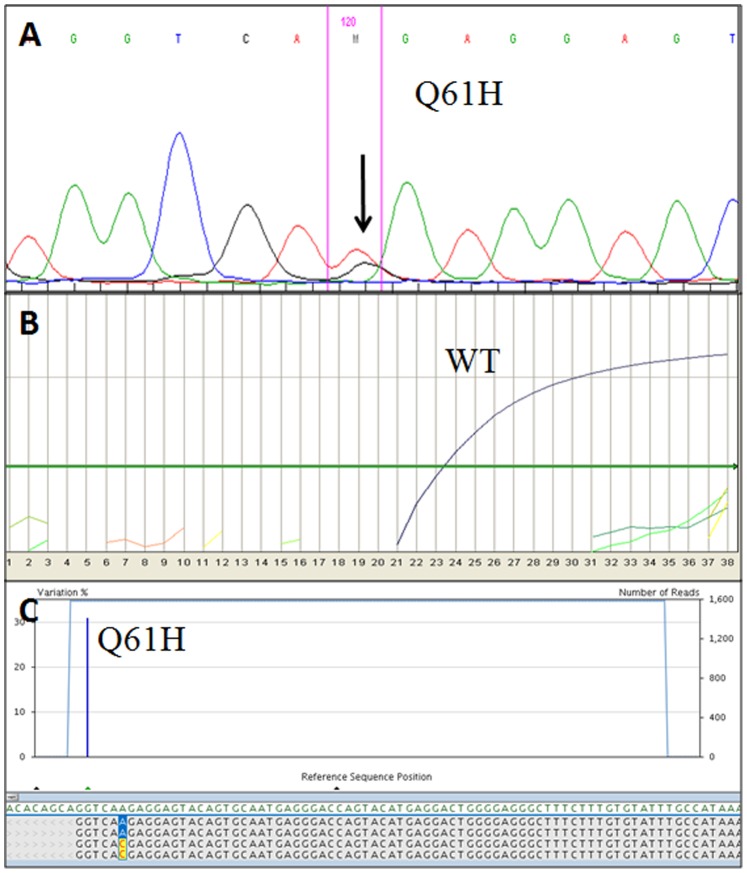
Figure 2. Example of molecular results in a KRAS exon 3 mutated sample (case #37, Table 4).
A) Electropherogram obtained using Sanger sequencing. The KRAS Q61H mutation is identified by the smaller pick pointed by the arrow. B) No KRAS mutation was detected using ASLNAqPCR results: only the curve corresponding to the wild-type allele is visible (WT). C) Profile obtained using 454-NGS, the KRAS Q61H mutation is identified by the vertical blue bar. The percentage of mutated alleles is indicated on the left y axis while the total number of reads on the right one.
In particular these latter cases were a C1 cystic lesion (mutated for Q61H) and a C4 suspected for malignancy (mutated for Q61L) which were respectively a BD-IPMN with low-grade dysplasia and a PDAC upon follow-up. In two cases, double mutations in KRAS exon 2 were observed (see “Multiple KRAS mutations” paragraph).
As summarized in Table 1, KRAS mutations were found in the 20.0% of inadequate samples (C1), in one of the two cases (50.0%) with atypical cells (C3), in the 55.6% of the cases suspect for malignant neoplasia (C4) and in the 30.0% of samples diagnosed as C5. All C2 cases showed no mutations in the KRAS gene and they were benign cysts (3 cases) or pancreatitis (one case) on follow-up. One of five cases with no available material for cytological evaluation was mutated for KRAS and it was a BD-IPMN on follow-up.
Considering the final endpoint, using Sanger sequencing we detected a KRAS mutation in 42.1% of adenocarcinomatous and pre-neoplastic lesions (in 40% of PDAC, 41.7% of IPMNs and in the 50% of inoperable neoplasms), while no KRAS mutations were observed in not adenocarcinomatous or in benign lesions (Table 2).
ASLNAqPCR
Using ASLNAqPCR analysis, 24 of 60 samples (40.0%) showed a mutation in KRAS exon 2 (Figure 1, Table 1). All mutations in KRAS exon 2 detected by Sanger sequencing were also detected by ALSNAqPCR (Figures 1A–1B). In five cases, double mutations in KRAS exon 2 were observed (see “Multiple KRAS mutations” paragraph).
No KRAS exon 3 (codon 61) mutations were detected by ASLNAqPCR because this technique is designed only for the 7 most common mutations in KRAS codon 12–13 [32].
As summarized in Table 1, KRAS mutations were found in the 20.0% of inadequate samples (C1), in one of the two cases (50.0%) with atypical cells (C3), in the 66.7% of the cases suspect for malignant neoplasia (C4) and in ten cases diagnosed as malignant neoplasia (C5). All the C2 cases showed no KRAS mutations. Three cases with no available material for cytological evaluation were mutated for KRAS. Upon follow-up two were IPMN, one BD-IPMN and one MD-IPMN with moderate dysplasia. No further information was available in the third case).
Considering the final endpoint, using ASLNAqPCR we detected a KRAS mutation in the 56.8% of adenocarcinomatous and pre-neoplastic lesions (in the 60% of PDAC, 41.7% of IPMNs and in the 66.7% of inoperable neoplasias. No KRAS mutations were observed in not adenocarcinomatous or in benign lesions (Table 2).
454 Next-generation sequencing
Using 454-NGS, 31 of 60 samples (51.7%) showed a mutation in KRAS exon 2 (24 of 60, 40%) and/or in KRAS exon 3 (10 of 60, 16.7%) (Figures 1–2). Raw data are available upon request.
All mutations in KRAS exon 2 detected by Sanger sequencing and ALSNAqPCR were also detected using 454-NGS (Figures 1 A–C).
In 7 cases (four C1c, one C4, one C5; in one case no material was available for cytologic evaluation) only a KRAS exon 3 (codon 61) substitution was found, while in 3 cases (two C4 and one C5) a KRAS exon 3 substitution was found in association with a mutation in KRAS exon 2 (see “Multiple KRAS mutations” paragraph). All mutations in KRAS exon 3 detected by Sanger sequencing were also detected using 454-NGS.
KRAS mutations were found the 40.0% of inadequate samples (C1), in one of the two cases (50.0%) with atypical cells (C3), in the 77.8% of cases suspect for malignant neoplasia (C4) and in eleven cases diagnosed as malignant neoplasia (C5) (Table 1). All the C2 cases showed no mutations in the KRAS gene. Four cases with no available material for cytologic evaluation were mutated for KRAS and upon follow-up three were IPMN (two BD-IPMN and one MD-IPMN with moderate dysplasia). No further information was available in the third case (Table 1).
Considering the final endpoint, using 454-NGS we detected a KRAS mutation in the 75.7% of adenocarcinomatous and pre-neoplastic lesions (in the 70% of PDAC cases, in the 83.3% of IPMNs and in the 66.7% of inoperable neoplasias). No KRAS mutations were observed in not adenocarcinomatous or in benign lesions (Table 2).
Multiple KRAS Mutations
Using Sanger sequencing double mutations of the KRAS gene exon 2 were observed in two cases (one C4 and one C5) that were PDAC upon follow-up (Table 3). ASLNAqPCR allowed to detect multiple mutations in 5 of 24 mutated cases (one C4 and two C5; in two cases cytologic evaluation was not available). These five cases were one IPMN and five PDAC upon follow-up (Table 3). Finally, next generation sequencing analysis allowed to observe multiple mutation of KRAS gene in 7 of 31 mutated cases (two C4 and three C5; in two cases no cytology material was available). In 3 of these 31 mutated cases, mutations in KRAS exon 2 and in KRAS exon 3 were observed. Upon follow-up, these seven cases were one IPMN and six PDAC (Table 3).
Table 3. Multiple KRAS mutations according to different techniques.
| Technique (#sample) | Mutations | Final End-Point |
| Sanger sequencing | ||
| #4 | G12D/G12V | PDAC |
| #53 | G12D/G12V | PDAC |
| ASLNAqPCR | ||
| #4 | G12D/G12V | PDAC |
| #5 | G12D/G12V | PDAC |
| #22 | G12D/G12V | IPMN |
| #26 | G12C/G12V | NA |
| #53 | G12C/G12D/G12R/G12V | PDAC |
| 454 NGS | ||
| #4 | G12D/G12V | PDAC |
| #5 | G12D/G12V | PDAC |
| #6 | G12V/Q61H | PDAC |
| #22 | G12D/G12V | IPMN |
| #26 | G12C/G12V | NA |
| #53 | G12C/G12D/G12R/G12V/Q61H | PDAC |
| #54 | G12D/Q61H | PDAC |
PDAC, Pancreatic Ductal AdenoCarcinoma; IPMN, Intraducatal Pancreatc Mucinous Neoplasia; NA, end-point not available.
Discrepant KRAS Results between Sanger Sequencing, ASLNAqPCR and 454-NGS
Results of discrepant cases are summarized in Table 4.
Table 4. Discrepant results obtained with the three techniques.
| Cytological (preoperative) Diagnosis (# of consecutive case) | KRAS mutational status | Final End-Point | ||
| 454 NGS (% ofmutated reads) | ASLNAqPCR (Ratio) | Sanger sequencing | ||
| C1 | ||||
| #31 | Q61H (4.3) | WT | WT | BD-IPMN |
| #37 | Q61H (31.0) | WT | Q61H | MD-IPMN |
| #42 | G12V (2.7) | G12V (0.02) | WT | NA |
| #44 | Q61L (3.0) | WT | WT | BD-IPMN |
| #46 | Q61R (1.1) | WT | WT | MD-IPMN |
| C4 | ||||
| #52 | Q61L (22.0) | WT | Q61L | PDAC |
| #57 | G12D (6.5) | G12D (0.03) | WT | PDAC |
| #60 | G12R (12.0) | G12R (0.06) | WT | PDAC |
| C5 | ||||
| #8 | G12D (19.3) | G12D (0.01) | WT | PDAC |
| #9 | Q61H (15) | WT | WT | PDAC |
| #10 | G12V (1.5) | G12V (0.08) | WT | PDAC |
| #11 | G12V (1.0) | G12V (0.02) | WT | PDAC |
| #14 | G12D (3.0) | G12D (0.02) | WT | Malignant Inop. Neop1 |
| NA | ||||
| #21 | G12V (3.7) | G12V (0.02) | WT | MD-IPMN |
| #25 | Q61H (1.4) | WT | WT | BD-IPMN |
| #26 | G12C&G12V (2.6&2.0) | G12C&G12V (0.02&0.01) | WT | NA |
Malignant Inop. Neop, Malignant Inoperable Neoplasia, patient did not undergo surgery, FU determined according to clinical data. FU, Follow-Up; NGS, Next Generation Sequencing; ASLNAqPCR, Allele Specific Locked Nucleic Acid qPCR; WT, Wild-Type; PDAC, Pancreatic Ductal AdenoCarcinoma; IPMN, Intraductal papillary mucinous neoplasm; BD, Branch Duct; MD, Main Duct; NA, follow-up not available.
In 16 cases discordant results in KRAS mutational status were obtained using at least one of the three different techniques (Table 4). Upon cytologic evaluation, 5 of 16 cases were diagnosed as malignant (C5) and 3 as suspect for malignancy (C4). In 5 cases the samples were cyst content material considerate inadequate for cytologic diagnosis (C1c). In three cases no material was available for cytologic examination.
C1 cases
In one sample a mutation in KRAS exon 2 gene was detected using 454-NGS and ASLNAqPCR, but not with Sanger sequencing (#42, Table 4). No follow up was available for this case. In one sample a mutation in KRAS exon 3 was detected both with 454-NGS and Sanger sequencing (#37, Table 4); it was a MD-IPMN (with low-grade dysplasia) according to histological evaluation. In the three remaining cases (#31, #44 and #46, Table 4) a mutation in KRAS exon 3 was detected only using 454-NGS and all three cases were IPMN (two BD-IPMN and one MD-IPMN) after post-operative histologic evaluation (Figures 2 A–C).
C4 cases
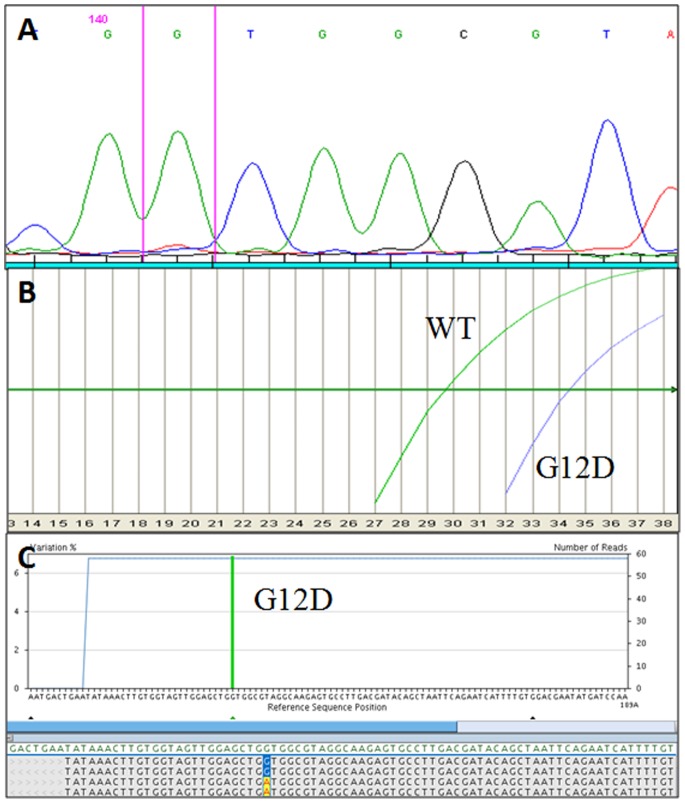
In two C4 samples (#57 and #60, Table 4) a mutation in KRAS exon 2 gene was detected using 454-NGS and ASLNAqPCR, but not with Sanger sequencing (Figures 3 A–C). All cases were pancreatic ductal adenocarcinoma (PDAC) after post-operative histologic evaluation. In one case (#52, Table 4) a mutation in KRAS exon 3 was detected both with 454-NGS and Sanger sequencing but not using ASLNAqPCR. It was a PDAC according to histological evaluation.
Figure 3. Example of molecular results in a KRAS exon 2 mutated sample (case #57, Table 4) with discordant results between the three techniques.
A) Electropherogram obtained using Sanger sequencing. The mutation is not identified. B) Using ASLNAqPCR the KRAS G12D mutation is identified by the right curve (G12D). The left curve indicates the wild-type allele (WT). The ratio between the two curves corresponds to ∼6% of mutated alleles. C) Profile obtained using 454-NGS, the KRAS G12D mutation is identified by the vertical green bar. The percentage of mutated alleles is indicated on the left y axis while the total number of reads on the right one.
C5 cases
In four C5 cases (#8, #10, #11 and #14, Table 4) a mutation in KRAS exon 2 gene was detected using 454-NGS and ASLNAqPCR, but not with Sanger sequencing. All cases were malignant carcinoma upon follow-up: three were diagnosed as pancreatic ductal adenocarcinoma (PDAC) after post-operative histologic evaluation, one case did not undergo surgery and was considered a malignant primary pancreatic neoplasm, based on clinical findings. In one case (#9, Table 4) a mutation in KRAS exon 3 was detected only with 454-NGS and was found to be a PDAC after post-operative histologic evaluation.
Cases with cytologic evaluation not available
All three samples with no cytologic evaluation and discrepant KRAS results were from cystic lesions. In two cases (#21 and #26, Table 4) at least one mutation in KRAS exon 2 gene was detected using 454-NGS and ASLNAqPCR, but not using Sanger sequencing. According to follow-up, one case (#21, Table 4) was a MD-IPMN (with moderate dysplasia). In the other no follow-up information was available. In the third case (#25, Table 4) a mutation in KRAS exon 3 was detected only with 454-NGS and the lesion was diagnosed as BD-IPMN after post-operative histologic evaluation.
According to the percentage of mutated reads (454-NGS) and ratio values (ASLNAqPCR) all the mutations in KRAS exon 2 detected using 454-NGS and ASLNAqPCR but not using Sanger sequencing were below the Sanger analytical sensitivity threshold (∼20% of mutated alleles, corresponding to ∼40% of mutated cells, considering the mutation heterozygous) (Table 4). The five mutations detected in KRAS exon 3 only by 454-NGS were all below the Sanger sequencing analytical sensitivity threshold (Table 4). On the contrary, the two KRAS exon 3 mutations detected both using 454-NGS and Sanger sequencing were observed in more than 20% of the total reads (Table 4).
KRAS Mutational Status in Cytologic Smears
Considering that it was not possible to determine the proportion or the presence of neoplastic cells in EUS-FNA material directly collected into a tube, we decided to re-analyze the samples not mutated for KRAS starting from cytological smears or cyto-blocks. The slides suitable for the manual dissection of neoplastic cells were selected by a pathologist and the representative area was marked. Residual material for molecular analysis was available for 24 of 29 patients that were wild-type for KRAS according all three techniques. On cytologicic evaluation, these 24 samples were diagnosed as: C1 in ten cases, C2 in 3 cases, C3 in one case, C4 in two cases and C5 in 8 cases (Table 5). In the 13 cases evaluated as unsatisfactory (C1c or C1s) or negative for malignancy (C2) the re-analysis was not performed. Due to the higher clinical sensitivity of NGS (see “Statistical measures of performance” paragraph) the analysis was repeated only using 454-NGS.
Table 5. Molecular results of KRAS analysis in material obtained from cytological smears.
| Number of consecutive analyzed Cases | Pre-operative Diagnosis | KRAS status onFNA material | KRAS status on cytological smear/cytoblock (% of mutated reads) | Final End-Point |
| #1 | C5 | WT | G12C (1.3) | PDAC |
| #3 | C5 | WT | WT | Malignant Inop. Neop.1 |
| #7 | C5 | WT | WT | pNET |
| #15 | C5 | WT | WT | pNET |
| #16 | C5 | WT | WT | pNET |
| #17 | C5 | WT | WT | pNET |
| #50 | C5 | WT | WT | SPPT |
| #51 | C5 | WT | WT | SPPT |
| #19 | C4 | WT | WT | PDAC |
| #55 | C4 | WT | WT | Malignant Inop. Neop.1 |
| #432 | C3 | WT | G12V (1.7) | PDAC |
FNA, Fine Needle Aspiration; FU, Follow-Up; PDAC, Pancreatic Ductal AdenoCarcinoma; pNET, pancreatic NeuroEndocrine Tumor; SPPT, Solid PseudoPapillary Tumor.
Malignant Inop. Neop, Malignant Inoperable Neoplasia, no histological evaluation was possible.
A digital slide of this sample is available at the following address http://vetrinodigitale.ausl.bo.it/spectrum_Login.php.
Two further mutations in the KRAS gene were observed in material obtained from cytologic smears. A KRAS G12V mutation was observed in a sample with “atypical cells” (C3) upon cytologic evaluation (#43 Table 5). This case was a PDAC according to post-operative histologic evaluation. A KRAS G12C mutation was detected in a sample with a “malignant” cytologic diagnosis (C5) (#1 Table 5) that was an adenocarcinoma after post-operative histologic evaluation. The remaining cases were wild-type for KRAS, even after the analysis was repeated on material dissected from the cytology specimen. According to follow-up these cases were PDAC (one case), pNET (4 cases), SPPT (2 cases). Two were inoperable malignant neoplasms (Table 5).
Statistical Measures of Performance
As shown in Table 6, when the analysis of KRAS (exon 2 and exon 3) was performed on direct FNA the 454-NGS, ASLNAqPCR and Sanger sequencing had 100% specificity. If only KRAS exon 2 was analyzed, the clinical sensitivity of 454-NGS (52.78%) was higher (p<0.001) than Sanger sequencing (44.19%) and comparable with that of ASLNAqPCR (52.78%). Clinical sensitivity (73.68%, p<0.001), negative predicted value (65.52%) and accuracy (82.46%) of 454-NGS were higher if KRAS exon 3 was also analyzed (Table 6).
Table 6. Statistical performance of KRAS molecular analysis using the three different techniques.
| KRAS Ex 2 | KRAS Ex 2 and Ex 3 | |||||
| Performance | 454 NGS | ASLNA | Sanger | 454 NGS | ASLNA | Sanger |
| SPEC (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| SENSIT (%) | 52.78 | 52.78 | 44.19 | 73.68 | 52.78 | 42.11 |
| PPV (%) | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 | 100.00 |
| NPV (%) | 55.26 | 55.26 | 36.84 | 65.52 | 55.26 | 46.34 |
| ACC (%) | 70.18 | 70.18 | 57.89 | 82.46 | 70.18 | 70.18 |
| FDR (%) | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
Ex, Exon; NGS, Next Generation Sequencing; ASLNA, Allele Specific Locked Nucleic Acid qPCR; Sanger, Sanger sequencing; SPEC, Specificity; SENS, Clinical Sensitivity; PPV, Positive Predictive Value; NPV; Negative Predictive Value; ACC; Accuracy; FDR, False Discovery Rate. In bold the higher value per each parameter.
The repeated analysis using 454-NGS of KRAS wild-type samples starting from DNA obtained from cytologic specimens led to increases in clinical sensitivity (78.95%, p<0.05), negative predictive value (70.37%) and accuracy (85.96%) (Table 7).
Table 7. Statistical performance of KRAS molecular analysis using 454-NGS starting only from FNA material or adding the results obtained in DNA extracted from cytologic smears (in bold).
| 454 NGS performances | KRAS analysis only on direct EUS-FNA sample | KRAS analysis performed also on cells scraped from the cytologic smears or cytoblocks |
| SPEC (%) | 100.00 | 100.00 |
| SENS (%) | 73.68 | 78.95 |
| PPV (%) | 100.00 | 100.00 |
| NPV (%) | 65.52 | 70.37 |
| ACC (%) | 82.46 | 85.96 |
| FDR (%) | 0.00 | 0.00 |
SPEC, Specificity; SENS, Clinical Sensitivity; PPV, Positive Predictive Value; NPV; Negative Predictive Value; ACC; Accuracy; FDR, False Discovery Rate.
Discussion
Detection of KRAS mutations can be used to improve the pre-operative diagnosis of pancreatic EUS-FNA samples. For this reason it is of crucial importance to perform the analysis with highly specific and analytical sensitive techniques. Sanger sequencing has been widely used for KRAS analysis, but the low analytical sensitivity (∼20% of mutated alleles) of the method can lead to false negative results [32] if compared with highly sensitive methods. Mutation specific assays, as ASLNAqPCR, notably improve the analytical sensitivity of KRAS molecular analysis, allowing to recognize 1% of mutated alleles [32]. However, these assays are designed only for particular “hot-spot” KRAS mutations (e.g. in KRAS exon 2). They can therefore underestimate the number of mutated samples, an example being those specimens with substitutions in KRAS exon 3 that are not usually targeted by mutation specific assays. Next generation sequencing merges the high analytical sensitivity of mutation specific assays with the broader capabilities of direct sequencing methods like Sanger, that not being mutation specific also allows the detection of unusual or unexpected mutations. Our data demonstrate that 454-NGS has a higher clinical sensitivity (73.68%) than ASLNAqPCR (52.78%, p<0.001) and Sanger sequencing (42.11%, p<0.001) in KRAS mutation detection of pancreatic lesions starting from EUS-FNA material. Mutations in specimens with a low proportion of mutated alleles (<20%, corresponding to <40% of cells considering the mutation heterozygous) were detected only using 454-NGS and ASLNAqPCR (if the mutation was present in exon 2) or only using 454-NGS (if the mutation was in KRAS exon 3). These results are fully compatible with the fact that that Sanger sequencing can detect a mutation only if it is present in more than 40% of the cells.
Our analysis of KRAS using highly analytical sensitive techniques such as ASLNAqPCR or 454-NGS not only increases the clinical sensitivity of the test but also maintains a very high level of specificity (100%).
Even if KRAS exon 2 mutations were still the majority (40% of all analyzed cases using NGS), mutations of KRAS exon 3 were also observed many samples (16.7% using NGS). Using Sanger sequencing our percentage of KRAS exon 3 mutated cases was about 3%, similar to that generally reported in the literature [38]). In three cases the KRAS exon 3 mutation would not have affected the molecular diagnosis, considering that the mutation was found in association with another KRAS mutation in exon 2. However, in seven cases the mutation in KRAS exon 3 was the only alteration found. All these seven cases would have been considered wild-type for KRAS although, on follow-up, five were IPMN and two were PDAC. For this reason, the detection of additional mutation in KRAS exon 3 provides very useful diagnostic information. Moreover, when both KRAS exon 2 and exon 3 were analyzed, the clinical sensitivity of 454-NGS was higher (73.68%) than when only KRAS exon 2 was investigated (52.78%).
IPMN is a spectrum of neoplasms in the pancreatic duct epithelium characterized by cystic dilation of the main pancreatic ducts and/or of their branches. IPMN is considered to be a precursor of PDAC. It has been proposed that the process of IPMN follows an adenoma - carcinoma sequence and that the time of progression to malignancy is about 5 years [39]. Since the process is slow, a correct diagnosis of IPMN provides the opportunity to cure the patient, before an invasive preoperative adenocarcinoma develops.
The results presented here indicate not only that IPMN are frequently mutated for KRAS (83.3% in our series, consistent with other studies that analyze only KRAS exon 2 in IPMN [14], [15], [40]), but also that they are commonly mutated in KRAS exon 3 (41.7%).
Analysis of KRAS starting from direct EUS-FNA material allows to obtain good quality DNA for molecular analysis that is therefore available at the same time of the cytologic evaluation. In samples with unsatisfactory cytology (e.g. cyst content material, C1c), the analysis of KRAS from EUS-FNA material directly collected into a tube is the only way to evaluate the mutational status of the gene. However, it is important to note that the direct analysis of EUS-FNA does not allow for the determination of the presence or the proportion of neoplastic cells in the specimen. Since this type of analysis is “blind”, DNA could originate from a population of cells not representative of the lesion, resulting in false negative results.
For this reason, in samples directly collected in a tube with a wild-type KRAS result it is important to repeat the analysis after the dissection of diagnostic material from the corresponding cytology specimen (smear or cytoblock) if there are atypical cells in the cytology preparation. In fact, in our series two cases found to be wild-type for KRAS starting from direct EUS-FNA material resulted mutated after the analysis was repeated on cells scraped from the cytologic smears. Both cases were diagnosed as adenocarcinoma after postoperative histologic evaluation.
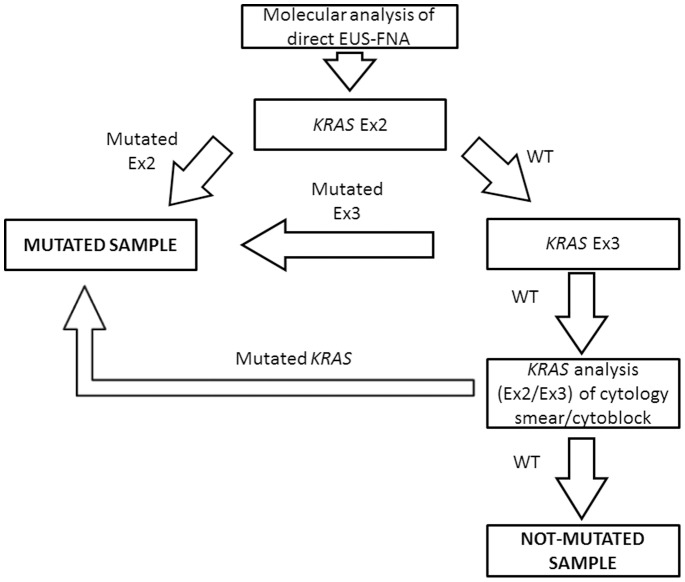
We propose an algorithm for KRAS analysis of pancreatic lesions (Figure 4). Next generation sequencing is more labor intensive and time-consuming that mutation specific techniques, as ASLNAqPCR. The turn-around time of 454-NGS depends on the throughput of the laboratory and batches of at least 100 amplicons (targeting the same or different exons) have to be run to lower the cost of the sequence to ∼20€ per amplicon. One hundred amplicons correspond to the analysis of 50 cases if both KRAS exons 2 and 3 are analyzed, for a total cost of ∼40€ per patient.
Figure 4. Proposed algorithm for the detection of KRAS mutations in EUS-FNA material from pancreatic lesions.
Ex, Exon; WT, Wild-Type.
To reduce turnaround time, the KRAS analysis could be performed by initially studying only KRAS exon 2, using a highly analytical sensitive mutation-specific method that is not time-consuming (less than 2 working days, including DNA extraction). This molecular analysis is carried out in conjunction and at the same time of the cytologic evaluation. If the sample is not mutated, KRAS analysis should be expanded to include KRAS exon 3, using a highly analytical sensitive direct sequencing technique such as pyrosequencing or Next Generation sequencing. If the sample is still not mutated for KRAS and the cytologic smear shows atypical, suspicious or malignant cells, KRAS analysis should be repeated starting from cells dissected from the cytology smear or cytoblock (Figure 4).
The algorithm we propose allowed us to reach a clinical sensitivity of ∼80% and a remarkable negative predictive value of ∼70%, if cases that were wild type for KRAS starting from material directly collected with EUS-FNA were re-analyzed on selected material dissected from the cytology smear or cytoblock. We want to point out that this high clinical sensitivity was achieved without any false positive result, with a 100% of specificity.
Four routine clinical test it is desirable, if not mandatory, to perform DNA analysis only after careful morphologic evaluation of the cytologic or histologic material submitted for molecular diagnosis. In fact, a negative KRAS result on a sample that consists of non-neoplastic cells or that is inadequate must be considered non-informative for clinical purposes. The results obtained in the present study stress the importance of morphologic evaluation of the material analyzed to detect KRAS mutations.
Finally, the analysis of KRAS with a semi-quantitative method (454-NGS or ASLNAqPCR), performed on material of well-known cellular composition, allows to clarify if mutations (single or multiple) are present in a small percentage of tumor cells (sub-clones) or in the vast majority of them as in the case of all “driver” mutations [33]. This type of evaluation is obviously not possible starting from direct EUS-FNA material.
In conclusion, our study underlines the importance of using a highly analytical sensitive technique for KRAS – as well as for any other molecular marker - mutation analysis to support the pathologist in the diagnosis of pancreatic lesions, as also recently shown in a meta-analysis by Fuccio et al. [42]. In this series Next Generation Sequencing has allowed us to reach a very high clinical sensitivity without getting false positive results. Highly analytical sensitive KRAS mutation analysis can prevent repeat biopsies and thus improve patient care while reducing costs [41], [42]. Considering the high prevalence of KRAS codon 6 mutation, particularly in IPMN, the analysis KRAS exon 3 should be performed in all pancreatic lesions.
Finally, analysis of wild-type KRAS samples should be repeated starting from cells dissected from selected cytology specimens (smears or cytoblocks), since direct EUS-FNA material can provide false negative results.
Funding Statement
This study was supported in part by an Italian Government MURST grant (Grant no.20093XZC57_003) to GT. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. No additional external funding was received for this study.
References
- 1. Siegel R, Ward E, Brawley O, Jemal A (2011) Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin 61: 212–236. [DOI] [PubMed] [Google Scholar]
- 2. De Angelis C, Repici A, Carucci P, Bruno M, Goss M, et al. (2007) Pancreatic cancer imaging: the new role of endoscopic ultrasound. JOP 8: 85–97. [PubMed] [Google Scholar]
- 3. Miura F, Takada T, Amano H, Yoshida M, Furui S, et al. (2006) Diagnosis of pancreatic cancer. HPB (Oxford) 8: 337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Saftoiu A, Vilmann P (2009) Role of endoscopic ultrasound in the diagnosis and staging of pancreatic cancer. J Clin Ultrasound 37: 1–17. [DOI] [PubMed] [Google Scholar]
- 5. Petrone MC, Arcidiacono PG (2008) Role of endosocopic ultrasound in the diagnosis of cystic tumours of the pancreas. Dig Liver Dis 40: 847–853. [DOI] [PubMed] [Google Scholar]
- 6. Iqbal S, Friedel D, Gupta M, Ogden L, Stavropoulos SN (2012) Endoscopic-ultrasound-guided fine-needle aspiration and the role of the cytopathologist in solid pancreatic lesion diagnosis. Patholog Res Int 2012: 317167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Turner BG, Brugge WR (2010) Diagnostic and therapeutic endoscopic approaches to intraductal papillary mucinous neoplasm. World J Gastrointest Surg 2: 337–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Varadarajulu S, Fockens P, Hawes RH (2012) Best practices in endoscopic ultrasound-guided fine-needle aspiration. Clin Gastroenterol Hepatol 10: 697–703. [DOI] [PubMed] [Google Scholar]
- 9. Dillon DA, Johnson CC, Topazian MD, Tallini G, Rimm DL, et al. (2000) The utility of Ki-ras mutation analysis in the cytologic diagnosis of pancreatobiliary neoplasma. Cancer J 6: 294–301. [PubMed] [Google Scholar]
- 10. Reicher S, Boyar FZ, Albitar M, Sulcova V, Agersborg S, et al. (2011) Fluorescence in situ hybridization and K-ras analyses improve diagnostic yield of endoscopic ultrasound-guided fine-needle aspiration of solid pancreatic masses. Pancreas 40: 1057–1062. [DOI] [PubMed] [Google Scholar]
- 11. Khalid A, Nodit L, Zahid M, Bauer K, Brody D, et al. (2006) Endoscopic ultrasound fine needle aspirate DNA analysis to differentiate malignant and benign pancreatic masses. Am J Gastroenterol 101: 2493–2500. [DOI] [PubMed] [Google Scholar]
- 12. Kato K, Kamada H, Fujimori T, Aritomo Y, Ono M, et al. (2012) Molecular Biologic Approach to the Diagnosis of Pancreatic Carcinoma Using Specimens Obtained by EUS-Guided Fine Needle Aspiration. Gastroenterol Res Pract 2012: 243524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hruban RH, Bishop Pitman M, Klimstra DS (2007) Tumors of the pancreas. Washington DC: American Registry of Pathology and AFIP.
- 14. Schonleben F, Qiu W, Bruckman KC, Ciau NT, Li X, et al. (2007) BRAF and KRAS gene mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/IPMC) of the pancreas. Cancer Lett 249: 242–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Schonleben F, Qiu W, Remotti HE, Hohenberger W, Su GH (2008) PIK3CA, KRAS, and BRAF mutations in intraductal papillary mucinous neoplasm/carcinoma (IPMN/C) of the pancreas. Langenbecks Arch Surg 393: 289–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Klimstra DS (2010) Intraductal Pancreatic Tumors; 2010; Washington DC.
- 17.Lauwers GY, Carneiro F, Graham DY (2010) Classification of Tumours of the Digestive System. Lyon: IARC.
- 18. Corbo V, Tortora G, Scarpa A (2012) Molecular pathology of pancreatic cancer: from bench-to-bedside translation. Curr Drug Targets 13: 744–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hruban RH, Adsay NV (2009) Molecular classification of neoplasms of the pancreas. Hum Pathol 40: 612–623. [DOI] [PubMed] [Google Scholar]
- 20. Matthaei H, Norris AL, Tsiatis AC, Olino K, Hong SM, et al. (2012) Clinicopathological characteristics and molecular analyses of multifocal intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 255: 326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Ottenhof NA, de Wilde RF, Maitra A, Hruban RH, Offerhaus GJ (2011) Molecular characteristics of pancreatic ductal adenocarcinoma. Patholog Res Int 2011: 620601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tada M, Komatsu Y, Kawabe T, Sasahira N, Isayama H, et al. (2002) Quantitative analysis of K-ras gene mutation in pancreatic tissue obtained by endoscopic ultrasonography-guided fine needle aspiration: clinical utility for diagnosis of pancreatic tumor. Am J Gastroenterol 97: 2263–2270. [DOI] [PubMed] [Google Scholar]
- 23. Hong SM, Park JY, Hruban RH, Goggins M (2011) Molecular signatures of pancreatic cancer. Arch Pathol Lab Med 135: 716–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khalid A, Dewitt J, Ohori NP, Chen JH, Fasanella KE, et al. (2011) EUS-FNA mutational analysis in differentiating autoimmune pancreatitis and pancreatic cancer. Pancreatology 11: 482–486. [DOI] [PubMed] [Google Scholar]
- 25. Goggins M (2007) Identifying molecular markers for the early detection of pancreatic neoplasia. Semin Oncol 34: 303–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Arvanitakis M, Van Laethem JL, Parma J, De Maertelaer V, Delhaye M, et al. (2004) Predictive factors for pancreatic cancer in patients with chronic pancreatitis in association with K-ras gene mutation. Endoscopy 36: 535–542. [DOI] [PubMed] [Google Scholar]
- 27. Kamisawa T, Takuma K, Tabata T, Egawa N, Yamaguchi T (2011) Long-term follow-up of chronic pancreatitis patients with K-ras mutation in the pancreatic juice. Hepatogastroenterology 58: 174–176. [PubMed] [Google Scholar]
- 28. Bournet B, Souque A, Senesse P, Assenat E, Barthet M, et al. (2009) Endoscopic ultrasound-guided fine-needle aspiration biopsy coupled with KRAS mutation assay to distinguish pancreatic cancer from pseudotumoral chronic pancreatitis. Endoscopy 41: 552–557. [DOI] [PubMed] [Google Scholar]
- 29. Maluf-Filho F, Kumar A, Gerhardt R, Kubrusly M, Sakai P, et al. (2007) Kras mutation analysis of fine needle aspirate under EUS guidance facilitates risk stratification of patients with pancreatic mass. J Clin Gastroenterol 41: 906–910. [DOI] [PubMed] [Google Scholar]
- 30. Tada M, Tateishi K, Kawabe T, Sasahira N, Isayama H, et al. (2002) Quantity of mutant K-ras gene in pancreatic secretions for diagnosis of pancreatic carcinoma with different assays: analysis of 100 patients. Clin Chim Acta 324: 105–111. [DOI] [PubMed] [Google Scholar]
- 31. Dabritz J, Hanfler J, Preston R, Stieler J, Oettle H (2005) Detection of Ki-ras mutations in tissue and plasma samples of patients with pancreatic cancer using PNA-mediated PCR clamping and hybridisation probes. Br J Cancer 92: 405–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Morandi L, de Biase D, Visani M, Cesari V, De Maglio G, et al. (2012) Allele specific locked nucleic acid quantitative PCR (ASLNAqPCR): an accurate and cost-effective assay to diagnose and quantify KRAS and BRAF mutation. PLoS One 7: e36084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Visani M, de Biase D, Baccarini P, Fabbri C, Polifemo AM, et al.. (2013) Multiple KRAS Mutations in Pancreatic Adenocarcinoma: Molecular Features of Neoplastic Clones Indicate the Selection of Divergent Populations of Tumor Cells. Int J Surg Pathol. [DOI] [PubMed]
- 34. Panarelli NC, Sela R, Schreiner AM, Crapanzano JP, Klimstra DS, et al. (2012) Commercial molecular panels are of limited utility in the classification of pancreatic cystic lesions. Am J Surg Pathol 36: 1434–1443. [DOI] [PubMed] [Google Scholar]
- 35.Chhieng DC, Stelow EB (2007) Pancreatic cytopathology; Rosental DL, editor: Springer.
- 36. Altimari A, de Biase D, De Maglio G, Gruppioni E, Capizzi E, et al. (2013) 454 next generation-sequencing outperforms allele-specific PCR, Sanger sequencing, and pyrosequencing for routine KRAS mutation analysis of formalin-fixed, paraffin-embedded samples. Onco Targets Ther 6: 1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hawass NE (1997) Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol 70: 360–366. [DOI] [PubMed] [Google Scholar]
- 38. Oliveira-Cunha M, Hadfield KD, Siriwardena AK, Newman W (2012) EGFR and KRAS mutational analysis and their correlation to survival in pancreatic and periampullary cancer. Pancreas 41: 428–434. [DOI] [PubMed] [Google Scholar]
- 39. Traverso LW, Moriya T, Hashimoto Y (2012) Intraductal papillary mucinous neoplasms of the pancreas: making a disposition using the natural history. Curr Gastroenterol Rep 14: 106–111. [DOI] [PubMed] [Google Scholar]
- 40. Sessa F, Solcia E, Capella C, Bonato M, Scarpa A, et al. (1994) Intraductal papillary-mucinous tumours represent a distinct group of pancreatic neoplasms: an investigation of tumour cell differentiation and K-ras, p53 and c-erbB-2 abnormalities in 26 patients. Virchows Arch 425: 357–367. [DOI] [PubMed] [Google Scholar]
- 41. Buttitta F, Felicioni L, Del Grammastro M, Filice G, Di Lorito A, et al. (2012) Effective assessment of egfr mutation status in bronchoalveolar lavage and pleural fluids by next-generation sequencing. Clin Cancer Res 19: 691–698. [DOI] [PubMed] [Google Scholar]
- 42.Fuccio L, Hassan C, Laterza L, Correale L, Pagano N, et al.. (2013) The role of K-ras gene mutation analysis in EUS-guided FNA cytology specimens for the differential diagnosis of pancreatic solid masses: a meta-analysis of prospective studies. Gastrointest Endosc. [DOI] [PubMed]