Abstract
Objective
Some studies report that initial anxiety is associated with equivocal or negative effects in depression treatment. In contrast, at least four studies of cognitive behavioral therapy (CBT) report that anxiety predicts greater or more rapid change in depression. Further exploration is needed to clarify the relationship between initial anxiety and depression change. Questions include the relationship between anxiety and patterns of change and time to relapse, as well the specificity effects to CBT.
Method
The study assessed the relation of Beck Anxiety Inventory anxiety scores to early rapid change and overall change in Beck Depression Inventory-II depression scores during acute depression treatment. Participants were 178 individuals enrolled in a randomized controlled trial of CBT versus medications (ADM) for moderate to severe depression. They were 58% female and 83% Caucasian, with an average age of 40 (SD = 11.5). Thirty four percent (34%) were married or cohabitating. Hierarchical linear models including quadratic growth parameters were used to model change. The relation of anxiety to the probability of post-treatment relapse was also examined.
Results
Findings indicate that higher levels of anxiety predict early rapid change, but not overall change, in both CBT and ADM. However, patients with higher levels of intake anxiety evidenced increased risk for relapse after CBT.
Conclusions
Early rapid change predicted by anxiety occurs across different treatment conditions, but this early rapid response is not indicative of positive overall outcome in all cases. These findings might indicate that anxiety predicts a response to non-specific “common factors” of treatment.
Keywords: depression, anxiety, CBT, antidepressant medications, rate of change
The predictive relationship between pretreatment anxiety and the course of symptom change in depression treatment has received increasing attention in the literature (Forand et al., 2011; Kashdan & Roberts, 2011; Smits, Minhajuddin & Jarrett, 2009; Smits, Minhajuddin, Thase & Jarrett, 2012). Anxiety commonly co-occurs with depression and is associated with greater symptom severity, impairment, and dysfunction (Fava et al. 2004; Brown, Schulberg, Madonia, Shear, & Houck, 1996). Because the pathology of depression with concurrent anxiety is believed to be more complex, some have suggested it requires specialized interventions (e.g., Kush, 2004; Papakostas et al., 2010). However, while many studies report negative or equivocal effects of anxiety on change in medication or psychotherapy (Fava et al., 2004; Howland et al., 2009; Smits, Minhajuddin & Jarrett, 2009; Gibbons & DeRubeis, 2008), a few studies of cognitive behavioral therapy (CBT) for depression find, surprisingly, that anxiety predicts increased rapidity of early change as well as greater overall change (Forand et al., 2011; Kashdan & Roberts, 2011; Rohde et al., 2001; Smits, Minhajuddin, Jarrett & Thase, 2012). In the current study, we investigate further the association between anxiety and change in depression in a sample of outpatients who were given CBT for depression, and we extend this investigation to a sample of patients who were given antidepressant medications.
Anxiety and Treatment of Depression
Antidepressant medication
In medication treatment, most studies find that anxiety is predictive of poorer outcomes. However, results depend to a certain extent on how anxiety is conceptualized and measured. When anxiety is defined as the presence of comorbid anxiety disorders, it has been associated with longer time to response and remission (Howland et al., 2009), as well as “treatment resistance,” defined as nonresponse to two consecutive adequate trials of ADM (Sourey et al., 2007). Similarly, “anxious depression,” defined by a cutoff on the anxiety and somatization items on the Hamilton Rating Scale for Depression (Hamilton, 1960), has been associated with longer time to and lower rates of remission in some samples (Fava et al., 2004, Fava et al., 2008). When anxiety severity has been conceptualized as a continuous variable, poorer outcomes have not always been evident. Frank et al. (2011) found that panic-agoraphobia symptoms and social anxiety symptoms predicted a longer time to remission in both interpersonal therapy and medication treatment. In contrast, Fournier et al. (2009) found no relationship between anxiety severity and change over time in CBT or medications for depression.
Psychotherapy
In contrast to studies of antidepressant medications, studies of the relationship between anxiety and change during psychotherapy have produced more inconsistent findings. One study found that comorbid anxiety disorders predicted greater end of treatment depression in systemic-behavioral family therapy and nondirective supportive therapy for adolescent depression (Brent et al., 1998). However, comorbid anxiety diagnoses have evidenced little or no predictive relation to end of CBT for depression in Brent et al. (1998) and in three other reports (McEvoy & Nathan, 2007; Persons et al., 2006; Smits, Minhajuddin & Jarrett, 2009). With regard to continuously measured anxiety, higher levels of panic-agoraphobic symptoms predicted worse response to IPT in Frank et al. (2000), but no relationship between variation in continuously measured anxiety symptoms and change was observed in a study of CBT (Gibbons & DeRubeis, 2008).
Notably, in at least four studies of CBT for depression, the presence of anxiety prior to the initiation of treatment predicted greater or more rapid change in depression. In CBT group therapy for adolescents, Rohde et al. (2001) found that comorbid anxiety disorder predicted greater baseline severity, but also greater reductions in depression from pre to post treatment. Three other studies assessed the relationship between anxiety and depression change over time using hierarchical linear models. In a study of group CBT for depression, comorbid social anxiety disorder predicted greater change in depressive symptoms over the course of treatment (Kashdan & Roberts, 2011). In particular, the authors noted that that the social anxiety group experienced more rapid gains in early treatment sessions. In a large study of CBT for depression, Smits, Minhajuddin, Jarrett and Thase (2012) found some evidence that anxious depression predicted greater initial severity and a lower probability of response, but also greater overall change in depression (although this latter finding only emerged in clinician-rated depression scales). Finally, in two naturalistic samples of CBT for depression, Forand et al. (2011) found that initial level of anxiety measured by the Beck Anxiety Inventory (Beck, Epstein, Brown, & Steer, 1988) was associated with greater change in depression over the full course of treatment (Study 1) as well as more rapid change early in treatment (Study 2).
Clarifying the Role of Anxiety in Depression Change
These findings are provocative; however, it is difficult to reconcile the normally deleterious effects of anxiety with a supposed beneficial treatment effect. Moreover, when viewed as a whole, the literature provides no clear answer with respect to the effect of anxiety on change in depression. These discrepant findings are likely in part attributable to differences in treatment, as well as differences in the measurement of anxiety (e.g., diagnoses vs. cutoff scores vs. continuous measures) and the measurement of outcome (e.g., time to response vs. probability of response vs. change in depression).
With respect to the operationalization of anxiety, the most powerful test of anxiety’s relationship with depression change must account for both the continuous nature of anxiety (Barlow, 2002) and its substantial overlap with depression (Forand et al., 2011). Depressed individuals often have substantial levels of anxiety that nonetheless do not meet criteria for a diagnosable anxiety disorder (Fava et al., 2004). Using categorical definitions of anxiety might obscure subsyndromal variation in anxiety symptoms that could be related to change or outcome (Forand et al., 2011). Using the presence of comorbid anxiety disorders as a measure of anxiety might also be problematic, because the type and severity of anxiety symptoms varies within and across diagnostic categories (Barlow, 2002). Because anxiety disorders are a heterogeneous collection of symptoms, an observed relationship between anxiety disorder and change is difficult to interpret. Dimensional scores allow the assessment of all levels of anxiety independent of potentially arbitrary categories, and therefore might be preferable to diagnoses and cutoff scores for assessing the relation between anxiety and change.
With respect to the measurement of change, evidence for a positive effect of anxiety has emerged primarily from studies that model change in depression over time. Variation in patterns of change, including increased early rapid change, have been found to predict both shorter and longer term outcomes (Stassen, Angst, Hell, Scharfetter & Szegedi, 2007; Hayes et al., 2007; Tang & DeRubeis, 1999), and person level characteristics have in turn been found to predict these patterns (Cohen et al., 2008; Forand et al., 2011; Gunthert et al., 2005). Information relevant to treatment processes might be revealed by examining the effect of anxiety on these patterns. Furthermore, despite evidence that anxiety improves short-term outcomes, few studies have assessed the effect of pretreatment anxiety on longer-term outcomes, such as the probability of relapse. Pretreatment anxiety is known to predict a greater chance of relapse after treatment (O'Leary, Hickey, Lagendijk & Webb, 2010), thus a full understanding of the effect of anxiety on change requires an extension to post-treatment outcomes.
The Current Study
The current study attempted to replicate and extend the investigation of Forand et al. (2011). Consistent with Forand et al., we assessed the effect of continuously measured anxiety on both early rapid change in depression and change in depression across the entire treatment period, as measured by the BDI-II. We also considered the effect of comorbid anxiety disorders on these indices of change. We then extended these investigations to a sample of outpatients treated with antidepressant medications. Finally, we determined whether anxiety at pre-treatment predicts post-treatment outcome by assessing its relationship with time to relapse.
Methods
Participants and Treatment
Sample characteristics, treatment protocols, and main outcomes of this research have been reported elsewhere (DeRubeis et al., 2005; Hollon et al., 2005). The trial was approved by institutional review boards and all participants provided written informed consent prior to participating. The sample consisted of 180 individuals randomized to cognitive behavioral therapy (CBT; n=60), and pharmacotherapy with paroxetine, which could be augmented with lithium or desipramine after 8 weeks (ADM, n=120). All treatment was conducted at the University of Pennsylvania in Philadelphia, PA and Vanderbilt University in Nashville, TN. Participants all had Structured Clinical Interview for DSM–IV (First, Spitzer, Gibbon, & Williams, 2001) diagnosed major depression, and scored at or above 20 on two successive interviews on the 17-item Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) given 1 week apart. Individuals were excluded if they had a history of Bipolar I disorder, active substance abuse, psychosis, previous failed response to study medications, borderline personality disorder, antisocial personality disorder, schizotypal personality disorder, or a primary Axis I disorder other than MDD. Written informed consent was obtained from all participants prior to entering the acute phase of the study. Patients were 58% female and 83% Caucasian, with an average age of 40 (SD = 11.5). Approximately one third (34%) were married or cohabitating.
CBT was conducted by six therapists with 5–21 years of experience following the guidelines laid out in Beck, Rush, Shaw, and Emery (1979). Antidepressant management was provided according to the guidelines specified by Fawcett, Epstein, Fiester, Elkin, & Autry (1987). Active treatments continued for 16 weeks. Nine (9) CBT and 13 ADM patients dropped out during acute treatment. Responders at end of treatment (week 16) were patients who had (a) HRSD ≤ 12 at week 16 and either HRSD≤ 14 at week 14 or HRSD ≤ 12 at week 10 and week 12, or (b) HRSD ≤ 12 at weeks 12, 14 and 18. CBT and ADM both achieved response rates of 58%. After acute treatment, ADM responders were randomized to one year of continuation ADM treatment or pill placebo. CBT responders were allowed three booster sessions scheduled at least 1 month apart during the continuation period.
Measures
Dependent variables
Beck Depression Inventory-II (BDI-II)
The BDI-II (Beck, Steer & Brown, 1996) is a widely used and well-validated 21-item self-report measure of depression. Following Forand et al. (2011), it was used in the present investigation as the primary measure of intake and weekly depression. The BDI-II was completed by patients at intake and weeks 1, 2, 3, 4, 6, 8, 10, 12, 14, and 16. At intake, Cronbach’s α in the current sample was .96.
Depressive Relapse/Recurrence
Relapse (or recurrence) criteria were met if a responder (a) scored a 14 on HRSD for 2 consecutive weeks or (b) met the diagnostic criteria for major depressive disorder for 2 consecutive weeks. The relapse rate of CBT responders (31.4%) was similar to that of ADM responders who remained on medication (41.2%) and significantly lower than that of ADM responders whose medication was discontinued (57.1%).
Independent variables
Beck Anxiety Inventory (BAI)
The BAI (Beck, Epstein, Brown & Steer, 1988) is a commonly used and well-validated 21-item self-report measure of anxiety. It was the measure of anxiety symptom severity at intake and the end of treatment. At intake, Cronbach’s α in the current sample was .93. Total scores on the BDI-II and BAI were prorated when items were missing.
Comorbid Anxiety Diagnoses
Anxiety disorders were diagnosed via the Structured Clinical Interview for DSM–IV (First, Spitzer, Gibbon, & Williams, 2001). Anxiety disorders were coded dichotomously, with the presence of one or more comorbid anxiety disorder coded as “1”, and the absence of any anxiety disorder as “0”.
Data Analytic Strategy
We conducted two main sets of analyses. The first of these concerned the pattern of change during depression treatment. Data consisted of repeated symptom measurements nested within individuals, and were modeled using hierarchical linear models (HLM). In these models, depression scores over the course of treatment were modeled as a function of a three growth parameters: intercept, linear slope, and quadratic slope. The linear component of the model represents the person-specific instantaneous rate of change at week 8, and the quadratic component represents the acceleration in the person-specific growth trajectory (Raudenbush & Bryk, 2002). To reduce multicollinearity between the linear and quadratic slopes, the linear term is centered at week 8 (midway through treatment), and this centered term is squared to create the quadratic term (Forand et al., 2011; Gunthert et al., 2005). At the between-subjects level, person-specific slopes and intercepts are treated as randomly varying across subjects, and are modeled as a function of intake anxiety and depression. Between-person effects are represented as cross level interactions. Measures of intake anxiety and depression were centered at their grand mean. All models were calculated with full maximum likelihood estimation procedures, and the degrees of freedom for hypothesis tests were estimated with the Kenward–Roger approximation (Kenward & Roger, 1997). These analyses included data from all participants, including dropouts, and are thus full intent to treat analyses.
The second set of analyses concerned the relationship between measures of symptom severity and time to relapse, which was estimated using Cox proportional hazards models (Cox & Oakes, 1984). In models predicting relapse, observations of patients who dropped out, deviated from their prescribed medication regimen, or received outside treatment prior to relapse or recurrence were censored at the point of the deviation. All analyses were performed using SAS Version 9.2 (SAS Institute, Cary, NC).
Results
Two participants, one in each of the two conditions, were missing BDI-II scores at intake, bringing the total n’s in CBT to 59 and ADM to 119. Means (SD) for the intake BDI-II were 30.9 (10.0) in the CBT condition and 30.9 (9.6) in the ADM condition. For the BAI they were 14.6 (9.0) in the CBT condition and 15.4 (9.9) in the ADM condition. The correlation between the BDI-II and the BAI at intake was r = .42. In the CBT condition, 52.5% of the sample had a comorbid anxiety disorder, and in the ADM condition the rate of comorbid anxiety disorders was 51.3%. Rates of individual anxiety diagnoses can be seen in Table 1. Of the scheduled 1,958 measurements of the BDI-II over the course of treatment, 1,547 were collected, indicating that 79.0% of possible measurements were available. A visual inspection of the BDI-II scores plotted against time in the CBT and ADM conditions revealed curvilinear patterns, with more rapid change occurring earlier in each treatment. These patterns suggested that quadratic growth models were appropriate for modeling the data.
Table 1.
Anxiety Disorders in CBT and ADM
| CBT (n = 59) | ADM (n = 119) | |||
|---|---|---|---|---|
| n | % | n | % | |
| Specific Phobia | 9 | 15.3 | 20 | 16.8 |
| Social Anxiety | 14 | 23.7 | 30 | 25.2 |
| GAD | 6 | 10.2 | 15 | 12.6 |
| Panic Disorder | 3 | 5.1 | 4 | 3.4 |
| Panic Disorder with Agoraphobia | 7 | 11.9 | 7 | 5.9 |
| PTSD | 13 | 22.0 | 16 | 13.5 |
| Anxiety NOS | 2 | 3.4 | 3 | 2.5 |
| Any anxiety disorder | 31 | 52.5 | 61 | 51.2 |
Replication in Cognitive Behavioral Therapy
An unconditional model, in which weekly BDI-II scores were modeled as a function of Time (the linear change term) and Time2 (the quadratic change term), was estimated in the CBT condition. The results revealed significant linear (b = −0.88, 95% CI [−1.08, −0.69], t= − 9.13(51.4), p < .001) and quadratic (b = 0.04, 95% CI [0.01, 0.06], t= 2.98(52.9), p < .01) patterns of change. An inspection of the variance components revealed sufficient between-person variability in slopes and intercepts to justify modeling them as a function of between-person predictors. A preliminary model including the terms Site, Site × Time and Site × Time2 was run to determine the need to control for site effects. As none of these terms reached significance, Site was not included as a predictor.
We next assessed the effect of intake anxiety on change while controlling for the effect of intake depression. The terms Intake BAI, Intake BAI × Time, Intake BAI × Time2, Intake BDIII, Intake BDI-II × Time, and Intake BDI-II × Time2 were entered into the model. Full results can be seen in Table 2. Intake BDI-II was a significant predictor of the intercept, with greater intake scores predicting greater depression at week 8 (b = 0.56, 95% CI [0.25, 0.88], t= 3.59(57.3), p < .001). With regard to linear slopes, neither the Intake BAI × time nor the Intake BDI-II × Time term was significant, indicating that intake depression and anxiety were not related to overall change in depression. Interactions with the quadratic term showed that intake depression had no relationship with early rapid change, however the Intake BAI × Time2 interaction was significant (b = .003, 95% CI [0.0003, 0.006], t= 2.28(56.6), p < .05). This result indicated that intake anxiety, controlling for intake depression, was associated with more rapid early change in depression symptoms. The Intake BAI × Time2 interaction accounted for 15% of the variance in quadratic slopes. A comparison between the deviance statistics (−2 log likelihood) of this model and a model that excluded the term BAI × Time2 revealed that the full model was a significantly better fit to the data (χ2 = 5.1(1), p < .05).
Table 2.
HLM Results
| ba | St. Error | DF | t | p | |
|---|---|---|---|---|---|
| CBT | |||||
| Intercept | 17.060 | 1.231 | 57.7 | 13.85 | *** |
| Intake BDI-II | 0.562 | 0.157 | 57.3 | 3.59 | *** |
| Intake BAI | −0.205 | 0.135 | 57 | −1.52 | |
| Time | −0.907 | 0.094 | 51.4 | −9.62 | *** |
| Time2 | 0.034 | 0.012 | 55.2 | 2.79 | ** |
| Intake BDI-II × Time | −0.020 | 0.012 | 51.3 | −1.67 | |
| Intake BDI-II × Time2 | −0.002 | 0.002 | 56.7 | −1.05 | |
| Intake BAI × Time | −0.006 | 0.010 | 50.5 | −0.60 | |
| Intake BAI × Time2 | 0.003 | 0.001 | 56.6 | 2.28 | * |
| ADM | |||||
| Intercept | 13.769 | 1.056 | 141 | 13.03 | *** |
| Intake BDI-II | 0.366 | 0.095 | 105 | 3.84 | ** |
| Intake BAI | −0.185 | 0.107 | 105 | −1.73 | |
| Time | −0.947 | 0.089 | 113 | −10.62 | *** |
| Time2 | 0.090 | 0.011 | 92.4 | 8.06 | *** |
| Intake BDI-II × Time | −0.031 | 0.007 | 112 | −4.47 | ** |
| Intake BDI-II × Time2 | −0.001 | 0.001 | 108 | −0.40 | |
| Intake BAI × Time | 0.011 | 0.008 | 107 | 1.48 | |
| Intake BAI × Time2 | 0.004 | 0.001 | 106 | 3.03 | * |
Note. Intake BDI-II = intake Beck Depression Inventory-II, Intake BAI = intake Beck Anxiety Inventory, Time = linear slope, Time2 = quadratic slope.
Values represent unstandardized betas. The intercept represents estimated depression at week 8. For significant interactions with Time, negative values indicate a prediction of greater overall change. For significant interactions with Time2, positive values indicate greater rapid early change.
p < .05,
p < .01,
p < .001
To determine whether comorbid anxiety disorders predicted early change in depression, a similar model was run, this time with comorbid anxiety disorder (yes, no) in place of intake BAI. The presence of a comorbid anxiety disorder was not associated with the intercept, the linear slope, or the quadratic slope (all p’s > .50).
Extension to Antidepressant Medications
We next assessed the relationship between anxiety and patterns of change in the ADM condition (N=119). An unconditional model revealed significant linear (b = −1.11, 95% CI [−1.24, −0.97], t= −16.32(106), p < .001), and quadratic patterns of change (b = 0.09, 95% CI [0.07, 0.11], t= 7.52(105), p < .001), and variance components indicated sufficient between-person variability to model slopes as a function of between-person predictors. A model including Site revealed a significant Site × Time interaction, indicating that participants at Vanderbilt experienced greater overall change in depression during medication treatment than participants at Penn. This interaction term was retained in subsequent models.
The next model included Intake BAI, Intake BDI-II, and their interactions with Time and Time2. See Table 2 for the full results. As with the CBT condition, the results showed that Intake BDI-II was a significant predictor of the intercept, with greater intake scores predicting greater depression at week 8 (b = 0.37, 95% CI [0.18, 0.56], t= 3.84(105), p < .001). With regard to linear slopes, the Intake BDI-II × Time term was significant (b = −0.03, 95% CI [−0.05, −0.02], t=−4.47(112), p < .001), indicating that greater intake depression was associated with greater overall change in depression. A test of the interaction of intake BDI-II with the quadratic term was not significant, indicating little or no influence on early rapid change. However, similar to the CBT condition, Intake BAI × Time2 interaction was significant (b = 0.004, 95% CI [0.0001, 0.007], t= 3.03(106), p < 0.01), again indicating that intake anxiety, independent of depression, was associated with more rapid early change in depression symptoms. The Intake BAI × Time2 interaction accounted for 13% of the variance in quadratic slopes. A comparison between the deviance statistics (−2 log likelihood) of this model and a model that excluded the term BAI × Time2 revealed that the full model was a significantly better fit to the data (χ2 = 8.1(1), p < .01). We noted that the effect of anxiety on quadratic slope was similar across CBT and ADM treatments. Indeed, when the samples were combined and treatment interactions were entered into the model, the Treatment × BAI × Time2 interaction was not significant.
The model with comorbid anxiety disorders (yes, no) indicated that the presence of a comorbid anxiety disorder was not associated with either the linear or the quadratic slope (all p’s > .60).
To help rule out the effect of shared method variance between the BDI-II and BAI, we also constructed models using the rater-administered Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) as a measure of intake and change in depression. Results were similar to those using the BDI-II. In both the CBT and ADM conditions, anxiety was associated with increased early rapid change (CBT: b = 0.001, 95% CI [0.00002, 0.004], t = 2.04(106), p < 0.05; ADM: b = 0.002, 95% CI [0.0005, 0.004], t = 2.61(106), p < 0.05), but unassociated with overall change. This finding helps rule out a measurement artifact as a possible explanation for the observed effects.
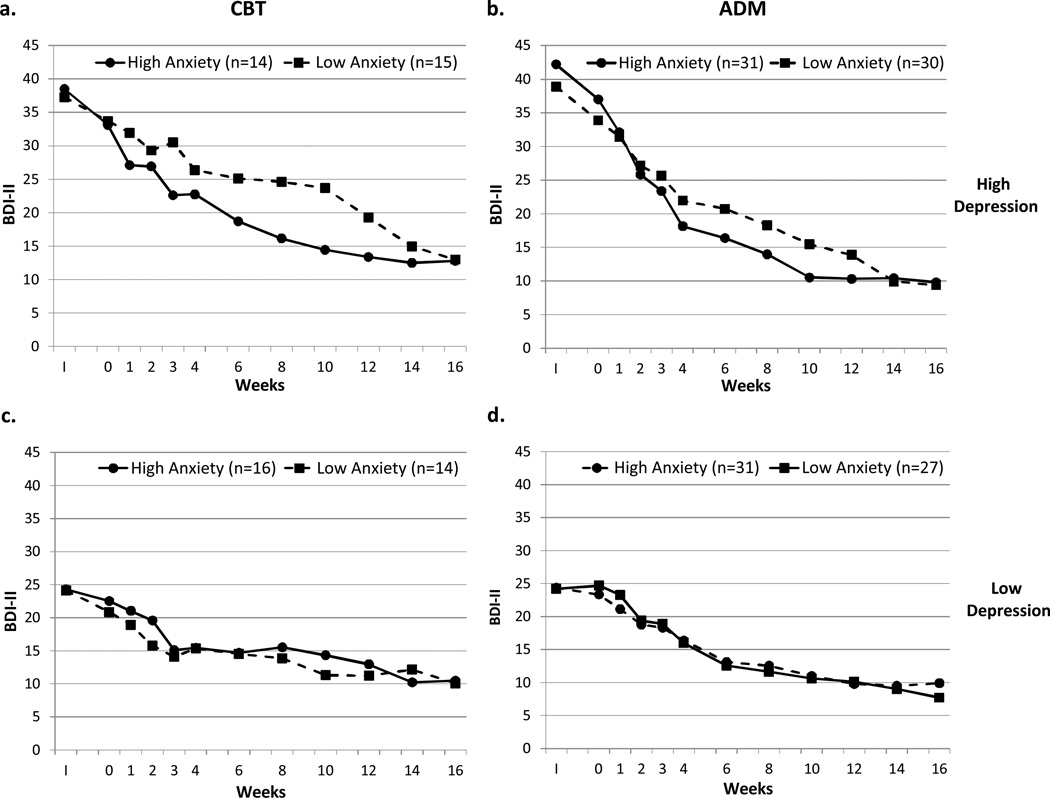
Graphs depicting the effect of anxiety on change can be seen in Figure 1. To enhance the visualization of the effect of anxiety on change independent of the severity of initial depression, we split each treatment condition into high and low depression groups at their medians. Within each of these groups, we performed a median split on anxiety and plotted depression change for the resulting high and low anxiety groups. This created two graphs in each treatment condition: high vs. low anxiety in high depression and high vs. low anxiety in low depression. Two features are evident in these graphs. First, the increased rapidity of early change predicted by anxiety is clearly visible in the high depression groups in both CBT and ADM conditions (top row). However, there are only minimal differences in early change evident in the low depression groups (bottom row), suggesting that the effect of anxiety on early rapid change is mostly confined to higher levels of depression severity. Second, as indicated by the models, the high anxiety groups do not experience greater overall depression change than the low anxiety groups. Although the high depression/high anxiety groups evidenced a more rapid early decrease in depression, they did not maintain this advantage over the full course of treatment. Rather, the high depression/high anxiety groups “leveled off” about halfway through treatment while the high depression/low anxiety group continued to improve at a steady rate.
Figure 1.
Change in Depression in CBT and ADM for High and Low Intake Anxiety Plotted for High Intake Depression (top row) and Low Intake Depression (bottom row)
Note. a. CBT High Depression: High Anxiety vs. Low Anxiety, b. ADM High Depression: High Anxiety vs. Low Anxiety, c. CBT Low Depression: High Anxiety vs. Low Anxiety, d. ADM Low Depression: High Anxiety vs. Low Anxiety. I = intake assessment. Missing data were interpolated using adjacent data points. High and Low Depression groups (top and bottom rows) were created via a median split. High and Low Anxiety groups (solid and dashed lines) were created via a median split within each depression group.
Prediction of Relapse
Our next set of analyses assessed the relationship between anxiety and time to relapse. Separate Cox regression models were run for each continuation condition (discontinued CBT with booster sessions: CBT; continued ADM: ADM-ADM; and discontinued ADM with placebo: ADM-PBO). To account for residual depressive symptom severity, which is a known risk factor for relapse (McGrath et al., 2006; Paykel et al., 1995), the BDI-II obtained at the end of treatment was included in the models. Results showed that intake anxiety, controlling for intake depression (BDI-II), did not predict time to relapse in ADM-ADM (p = .91) or ADMPBO conditions (p = .62). However, in the CBT condition, intake anxiety predicted decreased time to relapse (hazard ratio: 1.08, 95% CI [1.02, 1.15], χ2 = 6.1(1), p < .05).
Time to relapse for individuals above the median in intake anxiety was M = 34.5 (SD = 15.8) weeks, compared to M = 38.4 (SD = 15.9) weeks for individuals below the median. The presence of an anxiety disorder was not related to relapse in any of the conditions (all p’s > .21). Results were unchanged for prediction relapse when HRSD scores were used as the measure of intake and end of treatment depression.
Discussion
This study replicated and extended previous findings that suggested that the presence of high levels of anxiety fostered rapid or greater improvement in CBT for depression. In a sample of individuals treated with CBT, we found that pre-treatment anxiety was positively associated with increased early rapid change in depression. This finding replicated the results of Forand et al’s (2011) Study 2. Perhaps surprisingly, in light of reports that the presence of anxiety predicts inferior response in medication treatments, higher levels of anxiety also predicted increased early rapid change in individuals who received antidepressant medications. Change trajectories tended to “level off” in anxious individuals over the second half of treatment, however, resulting in no differences in overall change as a function of pretreatment anxiety.
Contrary to these initial positive effects of anxiety on depression change, we also found that greater intake anxiety predicted a decreased time to symptom return after successful treatment with CBT. Thus the combination of findings observed is somewhat surprising: high levels of anxiety in CBT appear related to both a positive outcome (early rapid change) and a negative outcome (decreased time to relapse) apparently within the same individuals.
These findings add to the growing body of literature on the effect of anxiety on change during treatment for depression. Previous authors have found that anxiety disorders (Kashdan & Roberts, 2011; Rohde et al., 2001), “anxious depression” (Smits, Minhajuddin, Jarrett & Thase, 2012), and anxiety symptoms (Forand et al., 2011) each predict increased depression reduction. In the current study, early rapid change was predicted by continuously measured anxiety symptoms – and severe anxiety symptoms in particular – but comorbid anxiety disorders were unrelated to change. Anxiety disorders are heterogeneous with respect to the presence and severity of anxiety symptoms (Barlow, 2002). Because of this, it is difficult to interpret a relationship between their presence of one or more anxiety disorders and depression reduction. In contrast, the BAI is known to predominantly measure the severity of physiological arousal and panic-like symptoms (Cox, Cohen, Direnfeld, & Swinson, 1996), suggesting that this group of symptoms is specifically important to the prediction of early change.
These results also advance our understanding of how anxiety might influence the specific shape of change trajectories. Prior to this research, most studies that have found positive associations between anxiety and change were concerned with the relationship between anxiety and overall depression outcome. Their analyses appropriately focused on predictors of linear change (Kashdan & Roberts, 2011; Rohde et al., 2001; Smits, Minhajuddin, Jarrett & Thase, 2012). In contrast, studies concerned with the shape of change, which include the current study and its predecessor (Forand et al., 2011), have each used a modeling approach that allows both linear and curvilinear components of change to vary as a function of pretreatment anxiety. Kashdan and Roberts (2011) included a quadratic slope in their models to account for curvilinear change, and also report that the increased linear change predicted by social anxiety disorder was mostly accounted for by rapid reductions in depression symptoms in early sessions. However, because they did not model the effect of anxiety on curvilinear change specifically, it is unclear how this determination was made. Thus the diversity of early findings in this area is likely is attributable at least in part to the modeling approach selected by the authors. It is premature to conclude that the effect of anxiety on change has been localized to the relationship between anxious arousal on early rapid improvement, to the exclusion of other possible relationships. However, if researchers had employed the methods similar to the current study, it is possible that a relationship between anxiety and early rapid change (instead of linear change) would have emerged. Because curvilinear change is common in depression treatment (Ilardi & Craighead, 1994; Stassen et al., 2007), authors investigating predictors of change are encouraged to consider predictors of both early curvilinear and overall trajectories.
Our methods for assessing change might also account for an apparent discrepancy between our results in ADM and findings from previous studies showing that anxiety predicted worse medication outcomes. In these studies, investigators have typically chosen as their dependent variable probability of response or time to response (Fava et al., 2004; Fava et al., 2008; Howland et al., 2009; Sourey et al., 2007). These methods are not intended to examine variations in patterns of change, and thus it is possible that the relationship between these outcomes and anxiety differ. On the other hand, our findings are not necessarily inconsistent with the finding that anxiety predicts a longer time to response (Fava et al., 2008; Howland et al., 2009). Because anxious individuals do not maintain their rapid rate of improvement in our sample, it is possible that the depressive symptoms of anxious individuals reach a “plateau” before individuals meet criteria for response. As this is one of the first studies to assess the relationship between anxiety and trajectories of change in ADM, further research is needed to clarify the relationship between anxiety and these various measures of outcome in this treatment.
Possible Mechanisms
Two tentative conclusions are implied by our findings: (a) the effect of anxiety on early rapid response is a common feature of treatment response in depression, unrelated to treatment modality and (b) the apparently positive initial effects on change in CBT can be illusory, as anxiety may portend poorer later outcomes in this treatment. A hypothesis that accounts for these findings must integrate the apparently contradictory effects of anxiety on outcome in across two mechanistically different treatments for depression. Previous authors have suggested that the positive effect of anxiety on depression reduction is due to a synergistic interaction between CBT techniques and anxiety (Forand et al., 2011; Kashdan & Roberts, 2011). However, the presence of the positive short-term effect in ADM and the indication that inferior long-term outcomes are predicted by higher anxiety in CBT suggest that an anxiety-related enhancement of CBT processes is unlikely.
One plausible account of the observed findings is that individuals with high levels of anxiety might have responded rapidly to warmth, positive regard, or other so called “common factors” of treatment. As is visible in Figure 1, the greatest effect of anxiety on early rapid change can be observed in individuals who have the most severe depression and most severe anxiety. BAI scores at the level of those observed in this group have been associated with intense panic-like symptoms (Cox, Cohen, Direnfeld, & Swinson, 1996). Individuals in this state are likely eager for relief, and might be particularly receptive to expressions of warmth, understanding, and efforts to promote hope. In other words, treatment might be “soothing” to a highly distressed person, and precipitate a rapid early response. Indeed, others have suggested that much of rapid early response is attributable to non-specific factors, both in CBT and ADM treatment (Ilardi & Craighead, 1994; Quitkin, Rabkin, Ross, & Stewart, 1984; Stewart et al., 1998). If individuals are responding to positivity and warmth by their therapist and improving rapidly, they might also have little opportunity or motivation to learn CBT skills that protect against depressive relapse (Strunk, DeRubeis, Chiu, & Alvarez, 2007). In this way, anxiety might interfere with treatment processes in CBT, a supposition that is supported by the findings of a previous study (Gibbons & DeRubeis, 2008). Another possibility is that individuals with significant anxiety require CBT skills directed at the reduction of anxiety, such as relaxation or exposure, to reduce their vulnerability to depressive relapse. These skills are less likely to be taught in CBT for depression, and thus individuals might remain vulnerable, particularly if they experience a return or worsening of anxiety symptoms.
The possibility of a rapid but non-enduring response calls into question the prospect of using the rapidity of response itself as an early marker for positive treatment outcomes, an idea proposed by previous researchers (e.g., Tadić et al., 2010). The current results suggest that not all rapid responses are indicative of positive long-term outcomes. Clinicians observing rapid responses in the context of high initial anxiety are therefore advised to be cautious about the durability of this response, and consider providing continued monitoring and relapse prevention interventions (Jarrett et al., 2001). This mechanism is speculative, however, and future research on the specific effect of anxiety on CBT treatment is needed to test this possibility.
Limitations and Future Directions
The current study has several limitations. Our modeling approach did not allow the assessment of change trajectories that deviate from a quadratic pattern, such as depression spikes (Hayes et al., 2007). It is possible that variations in these trajectories also contain important information related to the effect of anxiety. Furthermore, our study focused primarily on self-report measures of anxiety and depression. At least one previous study found that the method used to measure depression affected the relationship between anxiety and depression change (Smits, Minhajuddin, Jarrett, & Thase, 2012). Although results were largely similar when we used rater-administered scales, we cannot rule out method variance as a contributor to the observed results. Our results might also not be generalizable to populations with different characteristics than the current sample. Finally, it is unclear why anxiety predicted relapse in CBT and not after medication treatment. Further studies are needed to understand this relationship in different treatment modalities.
Future studies might also seek to understand differences in the process of recovery between individuals with different levels of anxiety, especially given that anxiety might be related to treatment-interfering processes in CBT (Gibbons & DeRubeis, 2008). Finally, it is clear from the current study that detailed investigations into trajectories of change can reveal important information about individual differences in response to treatment. Continued work in this area is likely to advance our understanding of how treatments for depression work beyond what can be understood through simple predictions of end of treatment response.
Acknowledgments
This research was supported by National Institute of Mental Health Grants MH55877 (R10), MH55875 (R10), MH01697 (K02), and MH01741 (K24). GlaxoSmith-Kline (Brentford, United Kingdom) provided medications and pill placebos for the trial.
We thank our colleagues for making this research possible. Paula R. Young and Margaret L. Lovett served as the two study coordinators. Jay D. Amsterdam, Richard C. Shelton, John P. O’Reardon, Ronald M. Salomon, and the late Martin Szuba served as study pharmacotherapists. Steven D. Hollon, Robert J. DeRubeis, Cory P. Newman, Karl N. Jannasch, Frances Shusman, and Sandra Seidel served as the cognitive therapists. Jan Fawcett provided consultation on the implementation of clinical management pharmacotherapy. Aaron T. Beck, Judith Beck, Christine Johnson, and Leslie Sokol provided consultation on the implementation of cognitive therapy. Madeline M. Gladis and Kirsten L. Haman oversaw the training of the clinical interviewers. David Appelbaum, Laurel L. Brown, Richard C. Carson, Barrie Franklin, Nana A. Landenberger, Jessica Londa-Jacobs, Julie L. Pickholtz, Pamela Fawcett-Pressman, Sabine Schmid, Ellen D. Stoddard, Michael Suminski, and Dorothy Tucker served as the clinical interviewers. Joyce L. Bell, Brent B. Freeman, Cara C. Grugan, Nathaniel R. Herr, Mary B. Hooper, Miriam Hundert, Veni Linos, and Tynya Patton provided research support.
Footnotes
The data presented in this article were collected as part of a clinical trial conducted between 1998 and 2003. The findings described have not been published elsewhere; however, subsets of the findings were presented at the 2011 Meeting of the North American Society for Psychotherapy Research, Banff, Canada, and at the 2011 Convention of the Association for Behavioral and Cognitive Therapies, Toronto, Canada.
No authors have relevant conflicts of interest to disclose.
References
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd ed. New York: The Guilford Press; 2002. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. Vol 56(6) 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. 1979. [Google Scholar]
- Brent DA, Kolko DJ, Birmaher B, Baugher M, Bridge J, Roth C, Holder D. Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(9):906–914. doi: 10.1097/00004583-199809000-00010. [DOI] [PubMed] [Google Scholar]
- Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. The American Journal of Psychiatry. 1996;153(10):1293–1300. doi: 10.1176/ajp.153.10.1293. [DOI] [PubMed] [Google Scholar]
- Cohen LH, Gunthert KC, Butler AC, Parrish BP, Wenze SJ, Beck JS. Negative affective spillover from daily events predicts early response to cognitive therapy for depression. Journal of Consulting and Clinical Psychology. Vol 76(6) 2008;76:955–965. doi: 10.1037/a0014131. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Cohen E, Direnfeld DM, Swinson RP. Does the Beck Anxiety Inventory measure anything beyond panic attack symptoms? Behaviour Research and Therapy. 1996;34(11–12):949–954. doi: 10.1016/s0005-7967(96)00037-x. [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Amsterdam JD, Shelton RC, Young PR, Salomon RM, O’Reardon JP, et al. Cognitive therapy vs medications in the treatment of moderate to severe depression. Archives of General Psychiatry. 2005;62(4):409–416. doi: 10.1001/archpsyc.62.4.409. [DOI] [PubMed] [Google Scholar]
- Fava M, Alpert JE, Carmin CN, Wisniewski SR, Trivedi MH, Biggs MM, Rush JA. Clinical correlates and symptom patterns of anxious depression among patients with major depressive disorder in STAR*D. Psychological Medicine. 2004;34(7):1299–1308. doi: 10.1017/s0033291704002612. [DOI] [PubMed] [Google Scholar]
- Fava M, Rush AJ, Alpert JE, Balasubramani GK, Wisniewski SR, Carmin CN, Trivedi MH. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. The American Journal of Psychiatry. 2008;165(3):342–351. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Epstein P, Fiester SJ, Elkin I, Autry JH. Clinical management-- imipramine/placebo administration manual. NIMH Treatment of Depression Collaborative Research Program. Psychopharmacology Bulletin. 1987;23(2):309–324. [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition With Psychotic Screen. New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Forand NR, Gunthert KC, Cohen LH, Butler AC, Beck JS. Preliminary evidence that anxiety is associated with accelerated response in cognitive therapy for depression. Cognitive Therapy and Research. Vol 35(2) 2011;35:151–160. [Google Scholar]
- Fournier JC, DeRubeis RJ, Shelton RC, Hollon SD, Amsterdam JD, Gallop R. Prediction of response to medication and cognitive therapy in the treatment of moderate to severe depression. Journal of Consulting and Clinical Psychology. 2009;77(4):775–787. doi: 10.1037/a0015401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Cassano GB, Rucci P, Thompson WK, Kraemer HC, Fagiolini A, Houck PR. Predictors and moderators of time to remission of major depression with interpersonal psychotherapy and SSRI pharmacotherapy. Psychological Medicine. 2011;41(1):151–162. doi: 10.1017/S0033291710000553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank E, Shear MK, Rucci P, Cyranowski JM, Endicott J, Fagiolini A, Cassano GB. Influence of panic-agoraphobic spectrum symptoms on treatment response in patients with recurrent major depression. The American Journal of Psychiatry. 2000;157(7):1101–1107. doi: 10.1176/appi.ajp.157.7.1101. [DOI] [PubMed] [Google Scholar]
- Gibbons CJ, DeRubeis RJ. Anxiety symptom focus in sessions of cognitive therapy for depression. Behavior Therapy. Vol 39(2) 2008;39(2008):117–125. doi: 10.1016/j.beth.2007.05.006. [DOI] [PubMed] [Google Scholar]
- Gunthert KC, Cohen LH, Butler AC, Beck JS. Predictive Role of Daily Coping and Affective Reactivity in Cognitive Therapy Outcome: Application of a Daily Process Design to Psychotherapy Research. Behavior Therapy. Vol 36(1) 2005;36:77–88. [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Laurenceau J-P, Feldman G, Strauss JL, Cardaciotto L. Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. Vol 27(6) 2007;27:715–723. doi: 10.1016/j.cpr.2007.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon SD, DeRubeis RJ, Shelton RC, Amsterdam JD, Salomon RM, O’Reardon JP, Gallop R. Prevention of relapse following cognitive therapy vs medications in moderate to severe depression. Archives of General Psychiatry. 2005;62(4):417–422. doi: 10.1001/archpsyc.62.4.417. [DOI] [PubMed] [Google Scholar]
- Howland RH, Rush AJ, Wisniewski SR, Trivedi MH, Warden D, Fava M, Davis LL, Berman SR. Concurrent anxiety and substance use disorders among outpatients with major depression: clinical features and effect on treatment outcome. Drug and Alcohol Dependence. 2009;99(1–3):248–260. doi: 10.1016/j.drugalcdep.2008.08.010. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, Craighead WE. The role of nonspecific factors in cognitive-behavior therapy for depression. Clinical Psychology: Science and Practice. Vol 1(2) 1994;1:138–156. [Google Scholar]
- Jarrett RB, Kraft D, Doyle J, Foster BM, Eaves GG, Silver PC. Preventing recurrent depression using cognitive therapy with and without a continuation phase: a randomized clinical trial. Archives of General Psychiatry. 2001;58(4):381–388. doi: 10.1001/archpsyc.58.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashdan TB, Roberts JE. Comorbid social anxiety disorder in clients with depressive disorders: predicting changes in depressive symptoms, therapeutic relationships, and focus of attention in group treatment. Behaviour Research and Therapy. 2011;49(12):875–884. doi: 10.1016/j.brat.2011.10.002. [DOI] [PubMed] [Google Scholar]
- Kenward MG, Roger JH. Small sample inference for fixed effects from restricted maximum likelihood. Biometrics. 1997;53(3):983–997. [PubMed] [Google Scholar]
- Kush FR. An operationalized cognitive therapy approach with mixed anxiety and depression. Psychotherapy: Theory. 2004;41(41):266–275. [Google Scholar]
- McEvoy PM, Nathan P. Effectiveness of cognitive behavior therapy for diagnostically heterogeneous groups: a benchmarking study. Journal of Consulting and Clinical Psychology. 2007;75(2):344–350. doi: 10.1037/0022-006X.75.2.344. [DOI] [PubMed] [Google Scholar]
- McGrath PJ, Stewart JW, Quitkin FM, Chen Y, Alpert JE, Nierenberg AA, Fava M, Petkova E. Predictors of relapse in a prospective study of fluoxetine treatment of major depression. The American Journal of Psychiatry. 2006;163(9):1542–1548. doi: 10.1176/ajp.2006.163.9.1542. [DOI] [PubMed] [Google Scholar]
- O’Leary D, Hickey T, Lagendijk M, Webb M. Onset of remission and relapse in depression: testing operational criteria through course description in a second Dublin cohort of first-admission participants. Journal of Affective Disorders. 2010;125(1–3):221–226. doi: 10.1016/j.jad.2010.02.107. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Ramana R, Cooper Z, Hayhurst H, Kerr J, Barocka A. Residual symptoms after partial remission: an important outcome in depression. Psychological Medicine. 1995;25(6):1171–1180. doi: 10.1017/s0033291700033146. [DOI] [PubMed] [Google Scholar]
- Persons JB, Roberts NA, Zalecki CA, Brechwald WAG. Naturalistic outcome of case formulation-driven cognitive-behavior therapy for anxious depressed outpatients. Behaviour Research and Therapy. 2006;44(7):1041–1051. doi: 10.1016/j.brat.2005.08.005. [DOI] [PubMed] [Google Scholar]
- Quitkin FM, Rabkin JG, Ross D, Stewart JW. Identification of true drug response to antidepressants. Use of pattern analysis. Archives of General Psychiatry. 1984;41(8):782–786. doi: 10.1001/archpsyc.1984.01790190056007. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. London: Sage; 2002. [Google Scholar]
- Rohde P, Clarke GN, Lewinsohn PM, Seeley JR, Kaufman NK. Impact of comorbidity on a cognitive-behavioral group treatment for adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(7):795–802. doi: 10.1097/00004583-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Smits JAJ, Minhajuddin A, Jarrett RB. Cognitive therapy for depressed adults with comorbid social phobia. Journal of Affective Disorders. 2009;114(1–3):271–278. doi: 10.1016/j.jad.2008.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souery D, Oswald P, Massat I, Bailer U, Bollen J, Demyttenaere K, Mendelwicz J. Clinical factors associated with treatment resistance in major depressive disorder: results from a European multicenter study. The Journal of Clinical Psychiatry. 2007;68(7):1062–1070. doi: 10.4088/jcp.v68n0713. [DOI] [PubMed] [Google Scholar]
- Stassen HH, Angst J, Hell D, Scharfetter C, Szegedi A. Is there a common resilience mechanism underlying antidepressant drug response? Evidence from 2848 patients. The Journal of Clinical Psychiatry. 2007;68(8):1195–1205. doi: 10.4088/jcp.v68n0805. [DOI] [PubMed] [Google Scholar]
- Stewart JW, Quitkin FM, McGrath PJ, Amsterdam J, Fava M, Fawcett J, Roback P. Use of pattern analysis to predict differential relapse of remitted patients with major depression during 1 year of treatment with fluoxetine or placebo. Archives of General Psychiatry. 1998;55(4):334–343. doi: 10.1001/archpsyc.55.4.334. [DOI] [PubMed] [Google Scholar]
- Strunk DR, DeRubeis RJ, Chiu AW, Alvarez J. Patients’ competence in and performance of cognitive therapy skills: Relation to the reduction of relapse risk following treatment for depression. Journal of Consulting and Clinical Psychology. Vol 75(4) 2007;75:523–530. doi: 10.1037/0022-006X.75.4.523. [DOI] [PubMed] [Google Scholar]
- Tadić A, Helmreich I, Mergl R, Hautzinger M, Kohnen R, Henkel V, Hegerl U. Early improvement is a predictor of treatment outcome in patients with mild major, minor or subsyndromal depression. Journal of Affective Disorders. Vol 120(1–3) 2010;120(2010):86–93. doi: 10.1016/j.jad.2009.04.014. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ. Sudden gains and critical sessions in cognitive-behavioral therapy for depression. Journal of Consulting and Clinical Psychology. 1999;67(6):894–904. doi: 10.1037//0022-006x.67.6.894. [DOI] [PubMed] [Google Scholar]