Abstract
Purpose
Visual field progression can be determined by evaluating the visual field by serial examinations (longitudinal analysis), or by a change in classification derived from comparison to age-matched normal data in single examinations (cross-sectional analysis). We determined the agreement between these two approaches in data from the Ocular Hypertension Treatment Study (OHTS).
Methods
Visual field data from 3088 eyes of 1570 OHTS participants (median follow-up 7 yrs, 15 tests with static automated perimetry) were analysed. Longitudinal analyses were performed with change probability with total and pattern deviation, and cross-sectional analysis with Glaucoma Hemifield Test, Corrected Pattern Standard Deviation, and Mean Deviation. The rates of Mean Deviation and General Height change were compared to estimate the degree of diffuse loss in emerging glaucoma.
Results
The agreement on progression in longitudinal and cross-sectional analyses ranged from 50% to 61% and remained nearly constant across a wide range of criteria. In contrast, the agreement on absence of progression ranged from 97% to 99.7%, being highest for the stricter criteria. Analyses of pattern deviation were more conservative than total deviation, with a 3 to 5 times lesser incidence of progression. Most participants developing field loss had both diffuse and focal change.
Conclusions
Despite considerable overall agreement, between 40 to 50% of eyes identified as having progressed with either longitudinal or cross-sectional analyses were identified with only one of the analyses. Because diffuse change is part of early glaucomatous damage, pattern deviation analyses may underestimate progression in patients with ocular hypertension.
Keywords: glaucoma, progression, visual field, change probability, ocular hypertension
Introduction
The Ocular Hypertension Treatment Study (OHTS) demonstrated that treatment to lower intraocular pressure delays or prevents the development of glaucoma in ocular hypertension. In participants randomised to receive treatment, the 5-year incidence of glaucoma was 4.4%, approximately half of that observed in those who did not receive treatment (9.5%).1, 2
In the OHTS, one endpoint for the development of glaucoma was the occurrence of reproducible visual field loss.3 Initially, all participants had normal visual fields, defined by a Glaucoma Hemifield Test (GHT)4 and Corrected Pattern Standard Deviation (CPSD) within normal limits.3, 5 If, during the follow-up, either the GHT or the CPSD were outside normal limits in three consecutive tests, visual field progression was suspected, and the participant’s visual fields were referred to the endpoint committee to confirm that progression attributable to glaucoma had occurred.6 GHT and CPSD summarize results from a single visual field examination by comparing the data to those of healthy subjects.7 Because GHT and CPSD are based on a comparison with normative data at a single point in time, this is a cross-sectional analysis, even though 3 consecutive visual fields may be required to confirm an abnormality. A different approach of measuring progression is to determine whether there is a significant change within the patient’s visual field over time,8, 9 and this is referred to as longitudinal analysis. Several types of longitudinal analyses have been described to analyse either the entire follow-up (trend analysis, by linear regression),10–13 or the baseline and a single follow-up examination (event analysis, by Glaucoma Change Probability analysis).13–15 Owing to the large range of normal values, a visual field may show clear evidence of change with longitudinal analysis, while remaining within the normal limits of a cross-sectional analysis. Therefore, it is possible that longitudinal analyses reveal disease-related changes in different eyes than the cross-sectional analyses.
The primary objective of this report was to investigate the agreement between longitudinal and cross- sectional progression analyses in participants of the OHTS. A second goal was to establish how a progression analysis applied in the Early Manifest Glaucoma Trial (EMGT)16 to patients with established glaucoma performs in patients with ocular hypertension. These questions have important implications on how patients with ocular hypertension should be followed in clinical practice, and on the design of research studies that use visual field progression as an outcome measure.
Methods
Dataset
This report includes data obtained within the OHTS through July, 2003. The OHTS was a multi-center randomized clinical trial, conducted in accord with the principles of the Declaration of Helsinki, to determine the efficacy and safety of ocular hypotensive therapy in preventing or delaying the development of glaucoma in patients with ocular hypertension.3
All eligible participants had ocular hypertension and were monitored with static automated perimetry program 30-2 of the Humphrey Field Analyzer (Carl Zeiss Meditec Inc, Dublin, California) with the Full Threshold strategy. For the purpose of this report, only eyes with 2 normal baseline visual fields and at least 3 follow-up examinations were included. To be classified as normal, baseline fields had to have a GHT classification of “within normal limits,” as well as CPSD and Mean Deviation (MD) within normal limits (p>10%).
A total of 3088 eyes of 1570 participants met these criteria. There were a mean of 15 (interquartile range, 5–18) visual field examinations per eye, obtained over a mean follow-up period of 6.7 (interquartile range, 6.3–7.5) years. We elected not to exclude visual fields for non-reliability on the basis fixation losses, false-positive, or false-negative responses. Therefore, a small proportion (461 of 44302, or 1%) of visual fields retained for this analysis had failed to meet the OHTS reliability criteria.17
Analyses
Cross-sectional analyses
In the OHTS, visual field progression was suspected if the GHT classification became “outside normal limits” or “general reduction of sensitivity” in three consecutive examinations, or if the CPSD became abnormal (p<5%) in three consecutive examinations. The same index had to be involved, and the spatial pattern of the defect had to be consistent across the three examinations.6 For brevity, we will refer to this as the “OHTS criterion”. To be clear, meeting the OHTS criterion by itself had not constituted an endpoint in OHTS; rather, it established a “suspicion of glaucomatous visual field progression” and triggered subsequent review by the Endpoint Committee, which by consensus determined if the eye had unequivocally developed glaucoma. For this reason, not all eyes fulfilling the “OHTS criterion” were confirmed as having a glaucomatous change by the Endpoint Committee.
There is no reference standard for what degree or type of visual field change constitutes a definite increment of glaucomatous damage, making it difficult to determine empirically the sensitivity and specificity of progression analyses. To arrive at a meaningful assessment of the agreement between the two different types of analysis, independent of the trade-off between sensitivity and specificity governed by a particular criterion, we elected to equalise the progression rates of the longitudinal and cross-sectional analyses.
To vary the number of eyes classified as progressing with the cross-sectional approach, we established a range of criteria that were similar to the OHTS criterion, but identified progression in a smaller or larger number of eyes. A cross-sectional score was assigned as follows. For each test, GHT classifications of “borderline”, “outside normal limits”, or “general reduction in sensitivity” were assigned a score of 1. Each of the MD and CPSD indices with significant p-values at <5% or <10% were assigned a score of 1, and at p<2% each were assigned a score of 2. For each test, the scores were summed with the results of the previous 2 tests, such that each test was given a score ranging from 0 to 15. By varying the criterion, a more than 10-fold variation in progression rates with cross-sectional analyses could be achieved.
Longitudinal analyses
Change probability analyses of progression were performed to measure visual field change over time.13 These analyses compare the deviation at each test location of the follow-up field to the average value obtained at two baseline examinations. Test locations at which the deviation is outside the 5th percentile of retest variability established in a group of stable glaucoma patients are flagged for likely deterioration, and progressive change in a visual field is determined based on the number of locations that show deterioration in 3 consecutive examinations. These analyses were performed with total and pattern deviation values using custom-written software previously described.13 The pattern deviation analyses are equivalent to the Guided Progression Analysis (GPA) of the Statpac software (Carl Zeiss Meditec Inc, Dublin, California),15, 18 while the total deviation analyses are equivalent to the older Glaucoma Change Probability analysis.7 The criteria of the longitudinal analyses were varied by adjusting the number of test locations which had to show significant change in 3 consecutive examinations.
Agreement between longitudinal and cross-sectional analyses
We assessed the agreement between longitudinal and cross-sectional analyses with total deviation change analysis and cross-sectional score as described above. Criteria were selected such that approximately the same number of eyes was classified as having progressed with each type of analysis. Three criteria (liberal, moderate, and conservative) were established in this manner. Agreement rates between longitudinal and cross-sectional analyses for progressing and non-progressing eyes were determined 19 and visualized by area-proportional Venn diagrams.
Comparison between total deviation and pattern deviation analyses
In the Early Manifest Glaucoma Trial (EMGT), change probability analyses were performed with pattern deviation rather than total deviation values to guard against the influence of diffuse visual field loss from developing cataract. We therefore compared the incidence of progression between total and pattern deviation analyses, with criteria of ≥2, ≥3, ≥5 and ≥8 test locations with significant change in 3 consecutive examinations. To determine the role of diffuse visual field loss, changes over time of the MD were compared to those of the General Height (GH) of the visual field. The GH is defined as the 85th percentile of the ranked total deviation values and is an index of sensitivity at the “least damaged” points in the visual field. This index is used for the calculation of the pattern deviation values, and changes in the GH reflect diffuse changes in the visual field.
Results
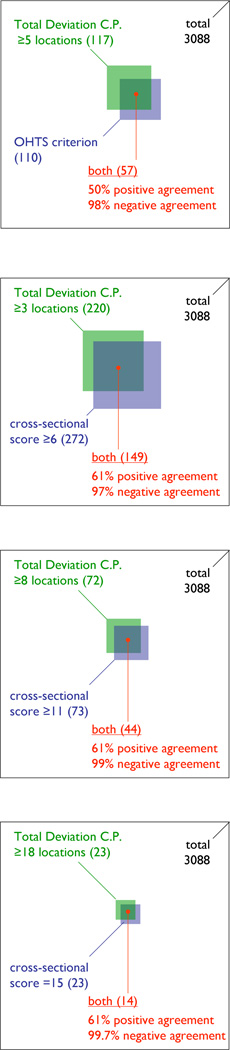
Of the 3088 eyes included in the study, 110 (3.6%) eyes met the OHTS criterion for suspected visual field progression. With the total deviation change probability analysis, this number was matched closest by a criterion of 5 test locations which detected progression in 117 eyes. The analyses agreed on the presence of progression in 57 eyes, and on its absence in 2918 eyes, giving rise to proportions of positive and negative agreement of 50% and 98%, respectively (Table 1, left column).
Table 1.
Agreement between longitudinal and cross-sectional analyses of visual field progression. The longitudinal analyses were performed with total deviation change probability.
| OHTS criterion | liberal | moderate | conservative | |
|---|---|---|---|---|
|
criterion of longitudinal analysis eyes classified as having progressed / total |
≥5 locations* 117 / 3088 |
≥3 locations 220 / 3088 |
≥8 locations 72 / 3088 |
≥18 locations 18 / 3088 |
|
criterion of cross-sectional analysis eyes classified as having progressed / total |
OHTS criterion 110 / 3088 |
score ≥ 6 272 / 3088 |
score ≥ 11 73 / 3088 |
score = 15 23 /3088 |
| eyes classified as progressed with both methods /total | 57 / 3088 | 149 /3088 | 44 / 3088 | 14 /3088 |
| proportion of positive agreement | 50% | 61% | 61% | 61% |
| proportion of negative agreement | 98% | 97% | 99% | 99.7% |
| Fig 1a | Fig 1b | Fig 1c | Fig 1d |
Criterion that provided the closest equivalence in numbers of progressive cases to the cross-sectional analysis of OHTS criterion. The OHTS used only cross-sectional criteria and had no longitudinal criteria.
The proportion of positive agreement between longitudinal and cross-sectional analyses remained similar across a wide range of criteria (Table 1, Fig 1). A less conservative criterion (total deviation change in ≥ 3 locations, and a cross-sectional score ≥ 6) identified progression in over 10 times as many eyes as a more conservative criterion (total deviation change in ≥ 18 locations, and a cross-sectional score = 15), but the proportion of positive agreement was identical (61%) for the liberal, moderate and conservative criteria.
Figure 1.
a) Agreement between longitudinal (total deviation change probability [C.P.], green square) and cross-sectional analyses (OHTS criterion, blue square) of visual field progression. The area of each square, and their overlap, is proportional to the number of eyes classified as having progressed with each method (in brackets).The total deviation criterion (5 locations) has been selected to provide the best possible match to the incidence of change with the OHTS criterion. The large square (black) is proportional to the total number of eyes (3088):
b) Agreement between longitudinal (total deviation, green square) and cross-sectional (blue square) analyses of visual field progression with liberal criteria approximately matched for incidence of progression
c) Agreement between longitudinal (total deviation, green square) and cross-sectional (blue square) analyses of visual field progression with moderate criteria approximately matched for incidence of progression.
d) Agreement between longitudinal (total deviation, green square) and cross-sectional (blue square) analyses of visual field progression with conservative criteria approximately matched for incidence of progression.
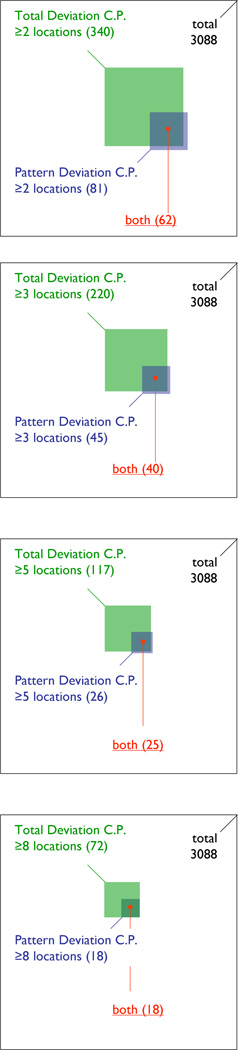
Analyses of pattern deviation classified considerably fewer eyes as having progressed compared to total deviation. For example, with a criterion of ≥ 3 locations, total deviation analyses identified progression in 220 eyes, while pattern deviation analyses identified progression in only 45 eyes. Almost all eyes identified with pattern deviation analyses were identified with total deviation analyses (Table 2, Fig 2).
Table 2.
Agreement between total and pattern deviation analyses of change probability. The table gives the number of eyes with significant change in 3 consecutive examinations in ≥2, ≥3, ≥5, and ≥8 test locations, out of the total of 3088 analyzed eyes.
| criterion | ≥ 2 locations | ≥ 3 locations | ≥ 5 locations | ≥ 8 locations |
|---|---|---|---|---|
|
eyes classified as having progressed by total deviation change probability |
340 | 220 | 117 | 72 |
|
eyes classified as having progressed by pattern deviation change probability |
81 | 45 | 26 | 18 |
|
eyes classified as having progressed by both total and pattern deviation change probability |
62 | 40 | 25 | 18 |
| Fig 2a | Fig 2b | Fig 2c | Fig 2d |
Figure 2.
Agreement between total deviation (green squares) and pattern deviation (blue squares) change probability (C.P.) analyses of visual field progression. The area of each square, and the overlap, is proportional to the number of eyes classified as having progressed with each method (in brackets). The large square (black) symbolizes the total number of eyes (3088).
a) Results with criteria of ≥2 locations with significant change in 3 consecutive tests
b) Results with criteria of ≥3 locations with significant change in 3 consecutive tests
c) Results with criteria of ≥5 locations with significant change in 3 consecutive tests
d) Results with criteria of ≥8 locations with significant change in 3 consecutive tests.
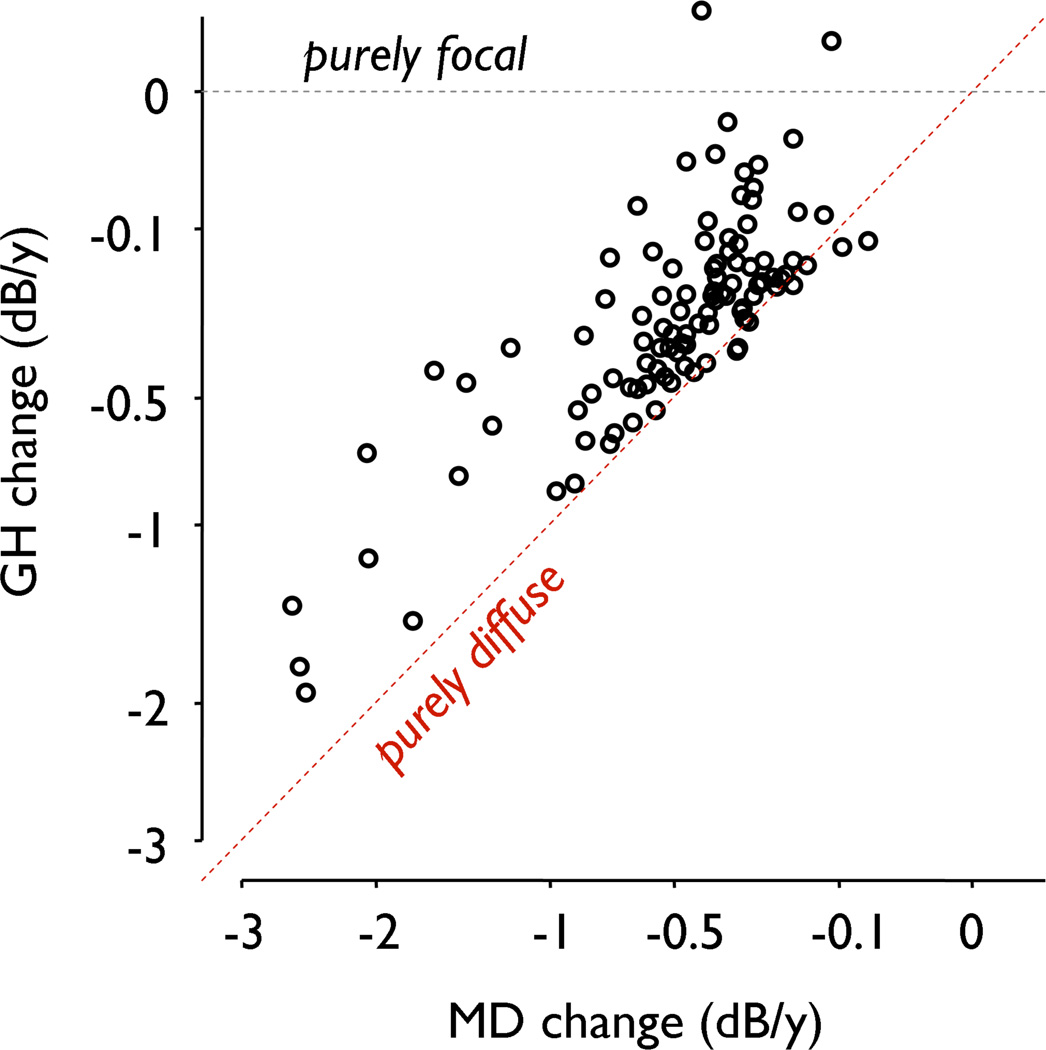
To investigate the large differences between total and pattern deviation analyses, we compared the rates of change of the MD and GH indices in all eyes in which the endpoint committee had ascertained a glaucomatous endpoint, either by visual field or optic disc change (Fig. 3). With purely focal visual field change, the MD would show a negative slope while the slope of the GH would be close to zero. In contrast, with purely diffuse visual field change the slopes of MD and GH would both be negative and similar to each other. This analysis showed that most eyes with glaucomatous endpoints exhibited diffuse as well as focal visual field changes.
Figure 3.
Changes in visual field General Height (GH) and Mean Deviation (MD) in eyes that developed glaucoma. Changes were established as the slope (by linear regression) of GH and MD (dB) with follow-up time (y). Eyes with purely focal change would show a change in MD but not in GH (dashed horizontal line), while eyes with purely diffuse change would show approximately equal slopes with both indices (dashed diagonal line). Most eyes showed focal as well as diffuse changes. For clarity, points are shown only if either MD or GH slope had a p-value <0.1 (n=108), omitting 63 with confirmed glaucomatous endpoints but no statistical trend in either GH nor MD. Axes are on a square-root scale to emphasize mid-range values.
Discussion
In patients who develop glaucoma from ocular hypertension, both longitudinal and cross-sectional approaches of detecting progression have a sound rationale. However, while the properties of both approaches have been investigated in healthy subjects and in patients with glaucoma, 13, 16, 20 they have not previously been compared in patients with ocular hypertension. In a previous study, we demonstrated the high specificity of change probability analysis, based either on total or pattern deviation, in a group of glaucoma patients and healthy subjects followed for up to 13 years.13 With the EMGT criterion, for example, the 5-year “progression” rate in healthy subjects was between 1 and 2%. Findings of progression with these analyses, therefore, constitute a credible signal that real change has taken place.
The primary aim of this report was to investigate the agreement between longitudinal and cross- sectional analyses of visual field progression in patients with ocular hypertension and to establish whether these analyses detect progression in different eyes. Our findings indicate that almost all eyes classified as stable with one type of analysis were also classified as stable with the other, while only 50%-60% of the eyes classified as having changed with either longitudinal or cross-sectional analyses were identified by both approaches. The finding of close agreement on the absence of progression (>97%) was expected, given the low incidence of glaucoma and the application of highly specific tests for progression. Even with the liberal criteria, most eyes did not show progression with either longitudinal or cross-sectional analyses.
However, the modest proportion of agreement on the presence of progression (50–61%) means that many eyes were identified as having changed with one analysis but not the other. One plausible explanation for this finding is that the two types of analysis identify different aspects of visual field change. For example, the longitudinal analyses performed in this study identified localized changes at individual test locations, while the cross-sectional analyses of GHT and CPSD operated on hemifield sectors and the global visual field, respectively. The spatial pattern of visual field change and its bearing on analyses of progression are topics of ongoing study, but a key message of the current report is that longitudinal analyses may be an important complement to cross-sectional analyses of visual field progression when patients with ocular hypertension are followed in clinical practice.
Because the recent clinical trials in glaucoma have all used different analyses, and different criteria, for establishing endpoints of visual field progression, it is difficult to compare progression across these studies. The EMGT approach has previously been investigated by several groups, and is now incorporated into the Guided Progression Analysis of the HFA Statpac software.21 When we applied the EMGT criteria16 to the participants of the OHTS, pattern deviation analyses were considerably more conservative than those with total deviation, and the differences were larger than those reported in patients with established glaucoma.13, 22 To explain these unexpectedly large differences between total and pattern deviation analyses, we compared the rates of MD and GH change over time. In almost all participants who developed glaucoma, changes in GH occurred alongside changes in MD, indicating that purely focal progression in glaucoma is rare, at least when glaucomatous damage first emerges in patients with high intraocular pressure.
Since pattern deviation analyses discount any diffuse changes of the visual field, they underestimate the overall amount of glaucoma-related change. Exclusive reliance on pattern deviation analyses may therefore underestimate the true incidence of early glaucomatous progression.
With visual field progression, there is no independent reference standard for what magnitude or type of change best separates true progression from variability. Sensitive criteria will identify most eyes with genuine worsening of the disease but will also misidentify cases where no such change had really taken place (lower specificity). More conservative criteria provide greater specificity to true change but will miss a greater number of eyes with more subtle progression. Each progression criterion provides a unique trade-off between sensitivity and specificity, and the choice of a particular criterion depends largely on the setting in which it is to be applied. Frequency of examinations, quality of the data, and the incidence of progression all differ between clinical practice, epidemiological studies, and treatment trials, and no single progression criterion is likely to be equally useful across the large spectrum of circumstances and requirements. However, the overall agreement between longitudinal and cross-sectional analyses in this report remained consistent over an approximately 10-fold variation in progression rates, and our finding that longitudinal and cross-sectional criteria identify progression in different subsets of eyes is therefore relevant to a wide range of clinical settings in which patients with ocular hypertension might be followed.
In summary, there was reasonable agreement between longitudinal and cross-sectional analyses of progression in the participants of OHTS when the criterion for each was adjusted to identify the same number of progressive eyes. However, a substantial number of eyes were identified as having changed with only one analysis but not the other, and longitudinal analyses of visual field progression should therefore be used alongside single field analyses when patients at risk of developing glaucoma are followed over time. Finally, reliance solely on pattern deviation analyses to detect progression may significantly underestimate the true incidence of emerging glaucoma in eyes with ocular hypertension.
Acknowledgments
grant support & disclosures
National Eye Institute and National Center on Minority Health and Health Disparities, National Institutes of Health, Bethesda, Maryland (grant nos.: EY 09307, EY 09341); Merck Research Laboratories, Whitehouse Station, New Jersey; and unrestricted grants to the several participating institutions from Research to Prevent Blindness, Inc., New York, New York.
Footnotes
Disclosure: Dr. Anderson is a consultant for Carl Zeiss Meditec, Dublin, CA.
Contributor Information
Paul H Artes, Email: paul@dal.ca.
Balwantray C Chauhan, Email: bal@dal.ca.
John L Keltner, Email: jlkeltner@ucdavis.edu.
Kim E Cello, Email: kecello@ucdavis.edu.
Chris A Johnson, Email: chris-a-johnson@uiowa.edu.
Douglas R Anderson, Email: danderson@med.miami.edu.
Mae O Gordon, Email: mae@vrcc.wustl.edu.
Michael A Kass, Email: kass@vision.wustl.edu.
References
- 1.Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002 Jun;120(6):701–713. doi: 10.1001/archopht.120.6.701. discussion 829-730. [DOI] [PubMed] [Google Scholar]
- 2.Palmberg P. Answers from the ocular hypertension treatment study. Arch Ophthalmol. 2002 Jun;120(6):829–830. doi: 10.1001/archopht.120.6.829. [DOI] [PubMed] [Google Scholar]
- 3.Gordon MO, Kass MA. The Ocular Hypertension Treatment Study: design and baseline description of the participants. Arch Ophthalmol. 1999 May;117(5):573–583. doi: 10.1001/archopht.117.5.573. [DOI] [PubMed] [Google Scholar]
- 4.Asman P, Heijl A. Glaucoma Hemifield Test. Automated visual field evaluation. Archives of Ophthalmology. 1992;110(6):812–819. doi: 10.1001/archopht.1992.01080180084033. [DOI] [PubMed] [Google Scholar]
- 5.Johnson CA, Keltner JL, Cello KE, et al. Baseline visual field characteristics in the ocular hypertension treatment study. Ophthalmology. 2002 Mar;109(3):432–437. doi: 10.1016/s0161-6420(01)00948-4. [DOI] [PubMed] [Google Scholar]
- 6.Keltner JL, Johnson CA, Quigg JM, Cello KE, Kass MA, Gordon MO. Confirmation of visual field abnormalities in the Ocular Hypertension Treatment Study. Ocular Hypertension Treatment Study Group. Arch Ophthalmol. 2000 Sep;118(9):1187–1194. doi: 10.1001/archopht.118.9.1187. [DOI] [PubMed] [Google Scholar]
- 7.Heijl A, Lindgren G, Lindgren A. Extended empirical statistical package for evaluation of single and multiple fields in glaucoma: Statpac 2. Perimetry Update. 1990;1:303–315. [Google Scholar]
- 8.Spry PGD, Johnson CA. Identification of Progressive Glaucomatous Visual Field Loss. Survey of Ophthalmology. 2002;47(2):158–173. doi: 10.1016/s0039-6257(01)00299-5. [DOI] [PubMed] [Google Scholar]
- 9.Smith SD, Katz J, Quigley HA. Analysis of progressive change in automated visual fields in glaucoma. Invest Ophthalmol Vis Sci. 1996;37(7):1419–1428. [PubMed] [Google Scholar]
- 10.Wild JM, Hutchings N, Hussey MK, Flanagan JG, Trope GE. Pointwise univariate linear regression of perimetric sensitivity against follow-up time in glaucoma. Ophthalmology. 1997;104(5):808–815. doi: 10.1016/s0161-6420(97)30229-2. [DOI] [PubMed] [Google Scholar]
- 11.Gardiner SK, Crabb DP. Examination of Different Pointwise Linear Regression Methods for Determining Visual Field Progression. Investigative Ophthalmology & Visual Science. 2002;43(5):1400. [PubMed] [Google Scholar]
- 12.McNaught AI, Crabb DP, Fitzke FW, Hitchings RA. Visual field progression: Comparison of Humphrey Statpac and pointwise linear regression analysis. Graefe's Archive for Clinical and Experimental Ophthalmology. 1996;234(7):411–418. doi: 10.1007/BF02539406. [DOI] [PubMed] [Google Scholar]
- 13.Artes PH, Nicolela MT, LeBlanc RP, Chauhan BC. Visual Field Progression in Glaucoma: Total Versus Pattern Deviation Analyses. Investigative Ophthalmology & Visual Science. 2005;46(12):4600–4606. doi: 10.1167/iovs.05-0827. [DOI] [PubMed] [Google Scholar]
- 14.Morgan RK, Feuer WJ, Anderson DR. Statpac 2 glaucoma change probability. Archives of Ophthalmology. 1991;109(12):1690–1692. doi: 10.1001/archopht.1991.01080120074029. [DOI] [PubMed] [Google Scholar]
- 15.Bengtsson B, Lindgren A, Heijl A, Lindgren G, Asman P, Patella M. Perimetric probability maps to separate change caused by glaucoma from that caused by cataract. Acta Ophthalmol Scand. 1997;75(2):184–188. doi: 10.1111/j.1600-0420.1997.tb00121.x. [DOI] [PubMed] [Google Scholar]
- 16.Heijl A, Leske MC, Bengtsson B, Bengtsson B, Hussein M. Measuring visual field progression in the Early Manifest Glaucoma Trial. Acta Opthalmologica Scandinavica. 2003;81(3):286. doi: 10.1034/j.1600-0420.2003.00070.x. [DOI] [PubMed] [Google Scholar]
- 17.Keltner JL, Johnson CA, Cello KE, et al. Visual field quality control in the Ocular Hypertension Treatment Study (OHTS) J Glaucoma. 2007 Dec;16(8):665–669. doi: 10.1097/IJG.0b013e318057526d. [DOI] [PubMed] [Google Scholar]
- 18.Budenz D. [ Date last accessed September 18, 2009];New Developments in Monitoring for Glaucoma Progression with Visual Fields. 2005 http://www.hbrentals-stream.com/events/zeiss/20051015-233024-1/msh.htm.
- 19.Cicchetti DV, Feinstein AR. High agreement but low kappa: II. Resolving the paradoxes. J Clin Epidemiol. 1990;43(6):551–558. doi: 10.1016/0895-4356(90)90159-m. [DOI] [PubMed] [Google Scholar]
- 20.Heijl A, Bengtsson B. Early visual field defects in glaucoma: a study of eyes developing field loss. Glaucoma: Decision Making in Therapy. Milan: Springer Verlag. 1996:75–78. [Google Scholar]
- 21.Meditec C-Z. HFA II-i with Guided Progression Analysis - Sample Cases. http://www.zeiss.de/C125679E00525939/EmbedTitelIntern/HFA_GPA_sample_cases/$File/HFA_GPA_sample_cases.pdf.
- 22.Katz J. A Comparison of the Pattern-and Total Deviation-Based Glaucoma Change Probability Programs. Investigative Ophthalmology & Visual Science. 2000;41(5):1012–1016. [PubMed] [Google Scholar]