Abstract
Physician practice variation may be a barrier to informing hematopoietic cell transplant (HCT) recipients about fertility preservation (FP) options. We surveyed HCT physicians in the United States to evaluate FP knowledge, practices, perceptions and barriers. Of the 1035 physicians invited, 185 completed a 29-item web-survey. Most respondents demonstrated knowledge of FP issues and discussed and felt comfortable discussing FP. However, only 55% referred patients to an infertility specialist. Most did not provide educational materials to patients and only 35% felt that available materials were relevant for HCT. Notable barriers to discussing FP included perception that patients were too ill to delay transplant (63%), patients were already infertile from prior therapy (92%) and time constraints (41%). Pediatric HCT physicians and physicians with access to an infertility specialist were more likely to discuss FP and to discuss FP even when prognosis was poor. On analyses that considered physician demographics, knowledge and perceptions as predictors of referral for FP, access to an infertility specialist and belief that patients were interested in FP were observed to be significant. We highlight variation in HCT physician perceptions and practices regarding FP. Physicians are generally interested in discussing fertility issues with their patients but lack educational materials.
Keywords: Hematopoietic cell transplantation, autologous, allogeneic, fertility preservation, infertility, pregnancy, practice patterns
INTRODUCTION
Hematopoietic cell transplantation (HCT) has been associated with relatively high rates of infertility in both men and women.1-8 However, fertility preservation (FP) among HCT recipients presents several challenges and practice variation among transplant physicians may be a barrier. Provider negative perceptions of the importance of fertility and low rates of discussion or referrals for FP have been reported to be among the barriers to FP in cancer patients and likely apply to physicians caring for HCT recipients.9-13 Additional physician factors include specialty, age, knowledge and attitudes toward FP, and comfort with the topic. In addition, several patient factors such as prognosis, insurance status, availability of resources, and cost of procedures may also influence physician perceptions. HCT may have to be pursued urgently as patients frequently have diseases that are at high risk for relapse and physicians may not consider FP as a priority or may not feel that a patient has time to delay transplant to pursue FP. Finally, physicians may be reluctant to discuss FP with patients who have poor prognosis. In a survey of United States (US) oncologists, Quinn et al found that only 47% of respondents routinely referred cancer patients of childbearing age to a reproductive endocrinologist, a practice recommended in the 2006 American Society of Clinical Oncology (ASCO) guidelines for oncologists.10 To better understand physician perceptions and practice patterns regarding fertility after HCT, we conducted a national survey of adult and pediatric HCT physicians in the US. This study fills the gap in knowledge about provider specific barriers to FP in HCT recipients.
METHODS
Survey Instrument
We adapted a questionnaire that has been previously validated and used to assess oncologists’ perceptions and practice patterns regarding FP among cancer patients.10, 14, 15 With permission and participation of the authors, the survey was modified to address similar issues among HCT physicians. The final instrument (Supplement) maintained the broad survey components and content areas that were established by extensive preliminary studies. These domains included: (1) FP knowledge; (2) practice behaviors regarding FP; (3) barriers to FP; (4) FP attitudes and perceptions; and (5) demographic and practice information.
The survey instrument was piloted among 14 physicians from 6 transplant centers who were not associated with the study to obtain feedback on clarity and interpretation of questions and to estimate the time required to complete the survey. The final survey instrument consisted of 29-items and took 5-10 minutes to complete. The responses were generally on a Likert scale indicating degree of agreement with a list of statements (strongly agree to strongly disagree). Respondents were asked to respond based on their experience with HCT recipients who could now or later get pregnant or father a child (patient age 0-45 years).
Survey Administration
The study was conducted under guidance of the Institutional Review Board of the National Marrow Donor Program. Transplant centers that participate in the Center for International Blood and Marrow Transplant Research (CIBMTR) observational research database provide a list of names and email addresses of transplant physicians who practiced in their facility. This included all US centers performing allogeneic and autologous HCT and the majority of centers performing autologous HCT only. We used this list to invite 1035 transplant physicians to participate in the survey. Identifying information on survey invitees (name and email address) was not available to the study team – this information was available to research staff from the CIBMTR who were not involved with the study and were responsible for sending survey invites, tracking responses and sending reminders to non-respondents. Hence, survey responses were anonymous to the study team and the respondents could not be identified in the final dataset available for analysis. No incentive was provided for participation. Survey invites were sent via email with a link to the survey website. Two subsequent followup email reminders were sent 4 weeks apart.
Statistical Analysis
We used center volume to classify transplant center size. One question each asked respondents to report the average annual number of autologous and allogeneic HCT at their center (<20, 20-50, 51-100, 101-200 and >200). Based on the distribution of responses to both questions, we classified centers as small (≤50 autologous HCT and <20 allogeneic HCT/year), medium (did not meet criteria for small or large size centers), and large (>100 autologous or >50 allogeneic HCT/year).
For descriptive purposes, we combined “Strongly agree” and “Agree” responses and “Always” and “Often” responses into one category. Similarly, we grouped “Strongly disagree” and “Disagree” responses and “Rarely” and “Never” responses.
Physician demographic characteristics and survey responses were summarized using frequencies and proportions. Bivariate analyses were performed to assess the association of likelihood of referring patients to an infertility specialist with physician characteristics and FP knowledge and perceptions. This was based on response to the question “I refer patients who have questions about fertility to an infertility specialist or reproductive endocrinologist”. Physicians who responded “Always” or “Often” to this question were compared with physicians who responded “Sometimes”, “Rarely” or “Never”. Physician factors considered for this analysis included: gender, year of graduation from medical school, size of transplant center, availability of infertility specialist, and whether respondent had previously taken care of patients who reported pregnancy after HCT. In addition to physician factors, we considered responses to questions on ‘fertility preservation knowledge’ as predictive factors for referral to an infertility specialist (response of ‘Strongly agree” or “Agree” to 4 or 5/5 questions in this section). We also considered “Strongly agree” or “Agree” response to one question under “fertility preservation attitudes and perceptions’ section (“patients are interested in learning about the effects of transplant on their fertility”) as a predictive factor for referral. All analyses were conducted using SAS statistical software (version 9.2, SAS Institute, Cary, NC). All P values are two sided with a statistical significance level set at 0.05.
RESULTS
Respondent Demographics
The overall response rate for our survey was 18% (185/1035). Table 1 shows the characteristics of survey respondents. Half of respondents (50%) practiced at large centers (>100 autologous or >50 allogeneic HCT annually). Access to an infertility specialist within their own center was available to 58% of respondents while another 25% reported access to an infertility specialist at another institution in their community. Physicians with access to an infertility specialist were significantly more likely to be practicing at a large transplant center (60% vs. 8% of those without access, P < 0.001).
Table 1.
Demographic characteristics of physicians who responded to the survey
| Characteristic | N (%) |
|---|---|
| Sample size | 185 |
|
| |
| Race/ethnicity | |
| Hispanic or Latino | 7 (4) |
| Not Hispanic or Latino | 163 (88) |
| Declined | 15 (8) |
|
| |
| Race | |
| White | 135 (73) |
| Asian | 30 (16) |
| More than one race | 2 (1) |
| Declined | 18 (10) |
|
| |
| Gender | |
| Male | 116 (63) |
| Female | 53 (29) |
| Declined | 16 (9) |
|
| |
| Year of medical school graduation | |
| 1965-1969 | 3 (2) |
| 1970-1979 | 33 (18) |
| 1980-1989 | 54 (29) |
| 1990-1999 | 56 (30) |
| 2000-2004 | 16 (9) |
| Declined | 23 (12) |
|
| |
| Patient age treated | |
| Adult only | 113 (61) |
| Pediatric only | 36 (20) |
| Both adult and pediatric | 17 (9) |
| Declined | 19 (10) |
|
| |
| Center size (based on self-reported transplant volume/year) | |
| Small | 23 (12) |
| Medium | 51 (28) |
| Large | 93 (50) |
| Declined | 18 (10) |
|
| |
| Access to an infertility specialist or reproductive endocrinologist | |
| Yes, within respondents institution | 107 (58) |
| Yes, in another institution in respondents community | 47 (25) |
| No | 13 (7) |
| Declined | 18 (10) |
|
| |
| Median number of HCT recipients that respondent has cared for who reported getting pregnant or fathering a child (range) | 3 (0-30) |
We did not collect demographic characteristics of survey non-respondents and hence could not compare them with that of respondents. However, we contrasted characteristics of our cohort with information available through the American Society for Blood and Marrow Transplantation BMT Physician Survey that was conducted in 2010 (personal communication with Robert Krawisz). This survey reported that 70% of US transplant physicians were male (vs. 63% in our study), 14% took care of pediatric patients (vs. 14% in our study), and 38% had completed training in blood and marrow transplantation prior to 1990 (vs. 49% of our study respondents had graduated from medical school prior to 1990).
Survey Responses
Figure 1 summarizes survey responses. Figures 2 and 3 highlight reported practice behaviors and barriers to FP based on practice type and access to infertility specialist.
Figure 1.
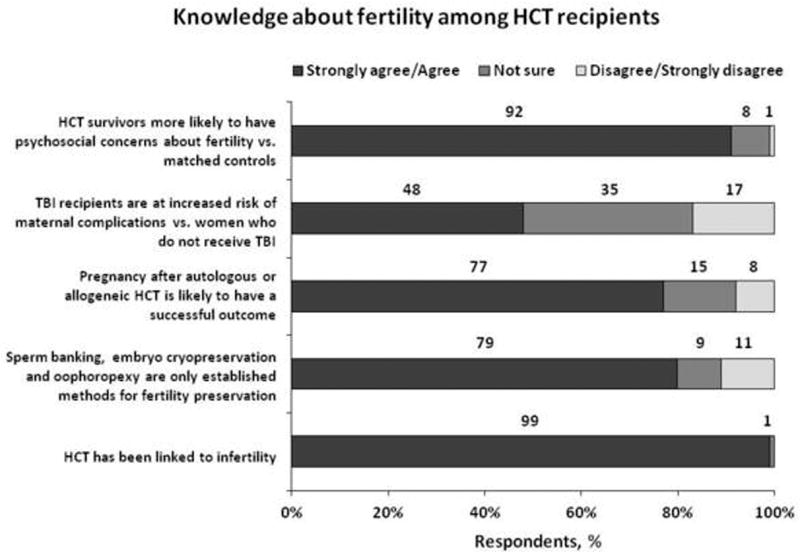
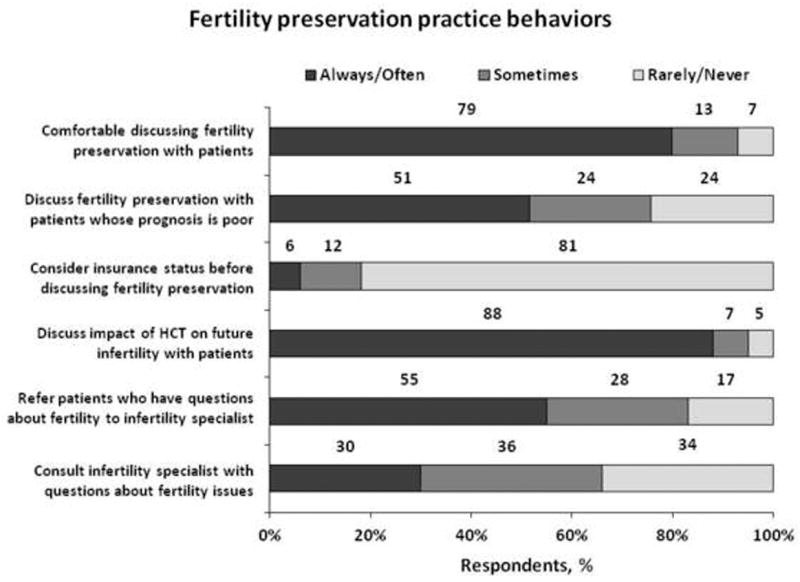
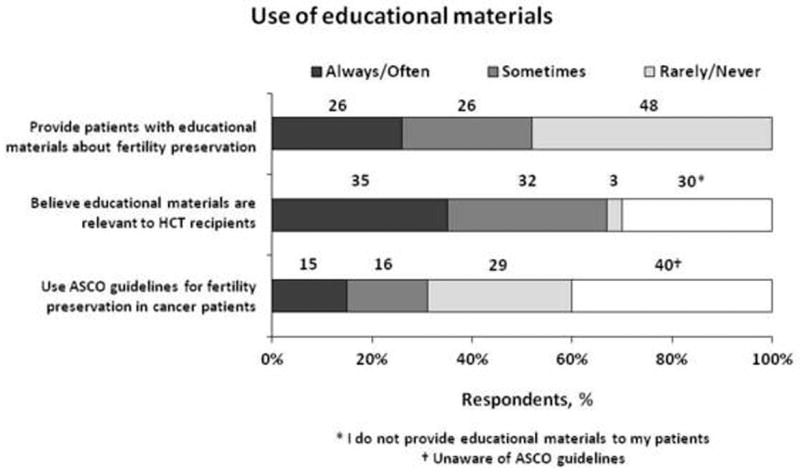
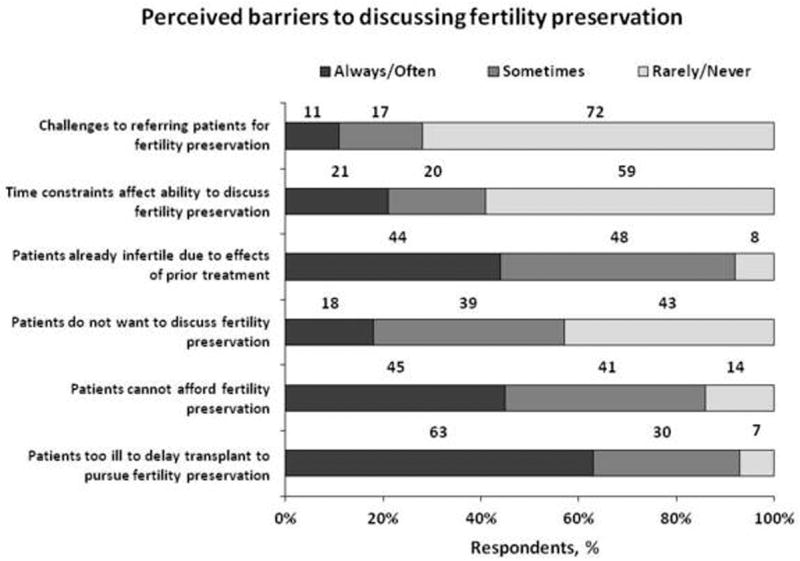
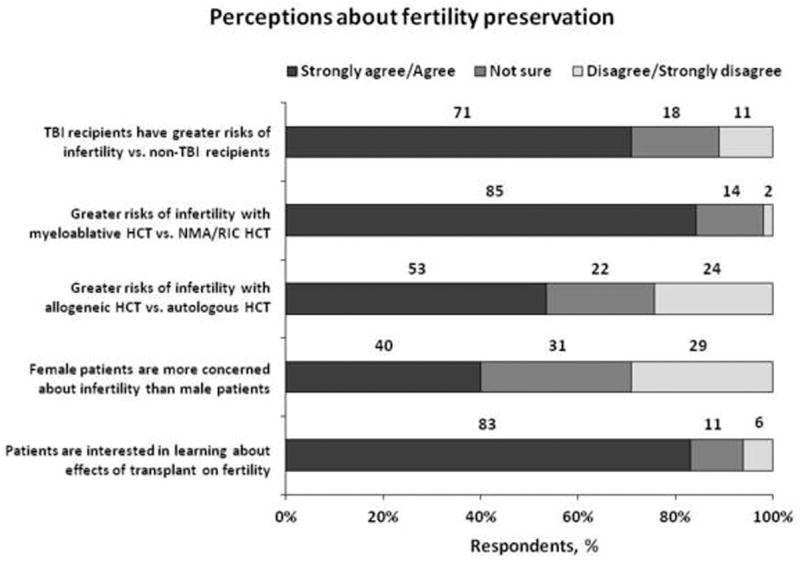
Physician responses to survey on fertility preservation perceptions and practice behaviors showing: (a) knowledge about fertility among HCT recipients, (b) fertility preservation practice behaviors, (c) use of educational materials, (d) perceived barriers to discussing fertility preservation and (e) perceptions about fertility preservation
Figure 2.
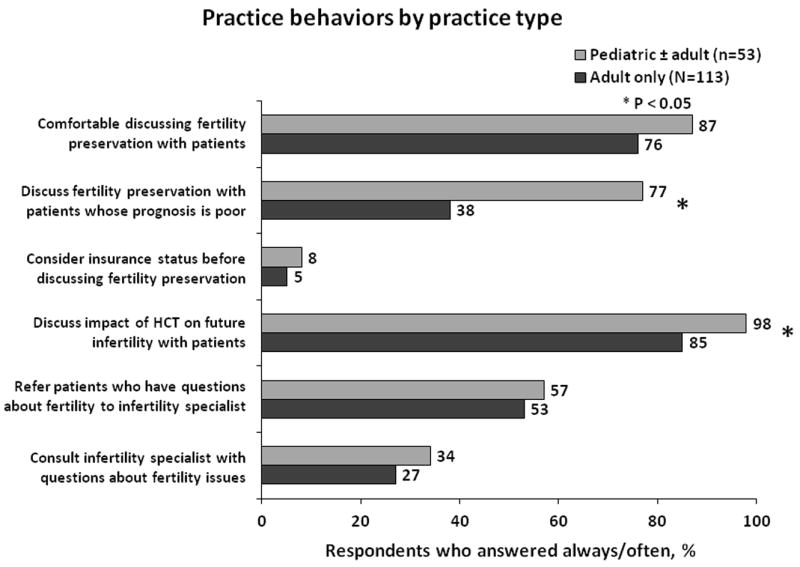
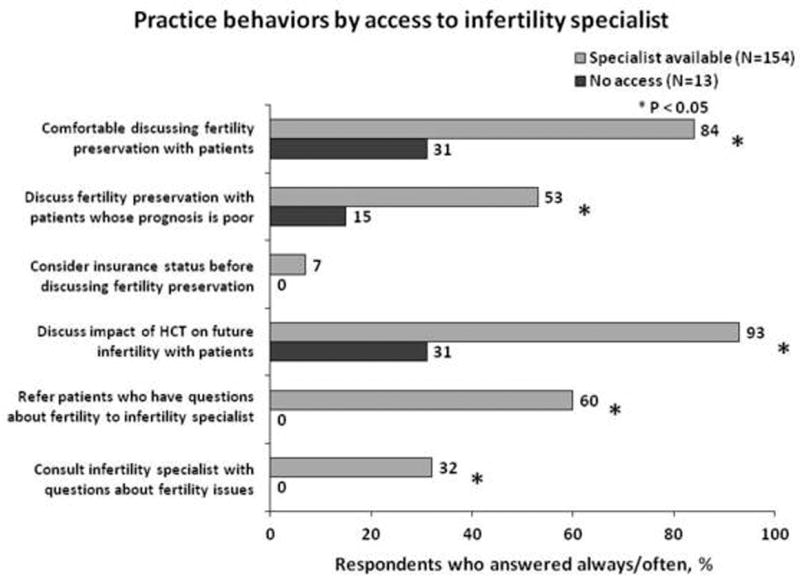
Reported fertility preservation practice behaviors for HCT recipients by physician practice type (adult HCT only vs. pediatric ± adult HCT) and access to an infertility specialist at the same institution or within their community
Figure 3.
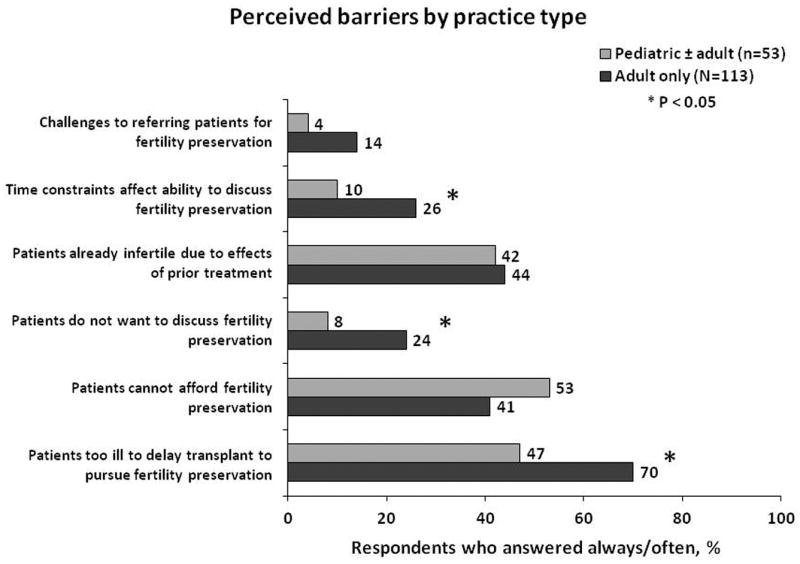
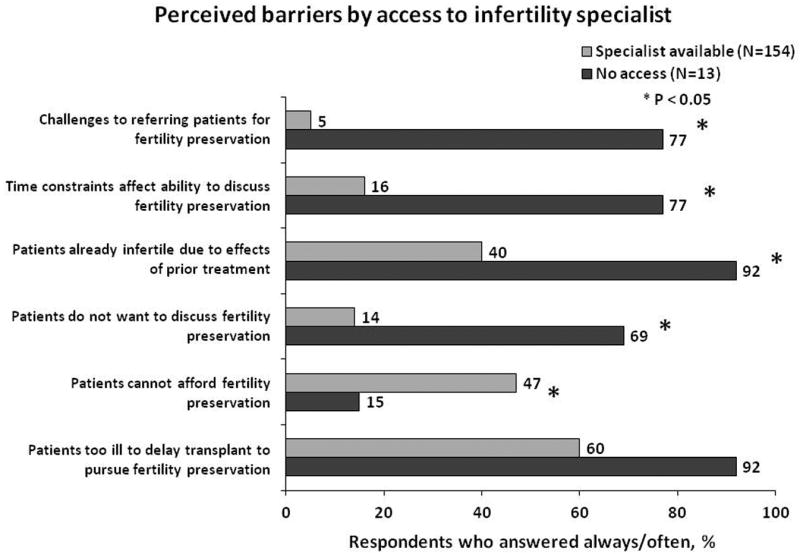
Perceived barriers to discussing fertility preservation with HCT recipients by physician practice type (adult HCT only vs. pediatric ± adult HCT) and access to an infertility specialist at the same institution or within their community
Fertility preservation knowledge
The vast majority of respondents recognized that HCT has been linked to infertility and demonstrated recognition of present standard-of-care options for FP. Responses did not vary by gender or by patient population treated. Physicians who had access to an infertility specialist were more likely to recognize that psychosocial fertility-related distress occurs among transplant recipients (93% with access vs. 69% with no access; P=0.01).
Fertility preservation practice behaviors
Most respondents discussed the impact of transplant on future fertility and felt comfortable discussing fertility issues, although only half of respondents discussed FP with patients whose prognosis was poor. Most did not consult an infertility specialist with questions about FP and only half referred their patients. Educational materials on FP were generally not provided and only 35% felt that available materials were relevant to HCT recipients. Importantly, 40% of transplant physicians were unaware of ASCO fertility guidelines,1 and another 29% said they ‘rarely’ or ‘never’ used these guidelines.
No notable differences in practice behaviors were observed by physician gender; except that a higher proportion of women physicians discussed FP with patients whose prognosis was poor (66% vs. 43% male physicians, P=0.02). We noted differences in practice behaviors among respondents who cared for adult recipients only compared to those who cared for pediatric recipients. While 98% of pediatric transplant physicians discussed FP with their patients, only 85% of adult physicians did (P=0.02). Pediatric providers were far more likely to discuss FP even when prognosis was poor (77% vs. 38% for adult physicians, P<0.0001). The most striking differences were noted based on access to an infertility specialist. Transplant physicians with access to an infertility specialist were significantly more likely both to consult (32% vs. 0%, P<0.0001) and to refer (60% vs. 0%, P<0.0001) patients to an infertility specialist, felt more comfortable in discussing FP with their patients (84% vs. 31%, P<0.0001), and were more likely to discuss FP when prognosis was poor (53% vs. 15%, p = 0.001). Additionally, providers with access to infertility specialists were more likely to provide educational materials (29% vs. 0%, P<0.0001) and were aware of the ASCO fertility guidelines (85% vs. 36%, P=0.009).
Barriers to fertility preservation
Many transplant physicians felt that patients were too ill to delay transplant for pursuit of FP options but generally recognized that patients did wish to discuss this topic. The majority felt that their patients were already infertile due to prior treatment. Barriers to FP included lack of access to infertility specialist, time constraints affecting ability to discuss fertility issues, ability of patients to afford FP and insurance coverage for FP (Table 2).
Table 2.
Primary perceived barriers to discussing fertility preservation with HCT recipients
| Characteristic | Responses* (%) |
|---|---|
| My typical patient is too ill to delay treatment | 102 (55%) |
| Insurance does not cover fertility preservation | 64 (35%) |
| Patients cannot afford fertility preservation | 61 (33%) |
| Time constraints limit fertility preservation discussion | 50 (27%) |
| Do not have sufficient knowledge to discuss fertility preservation | 30 (16%) |
| Do not have information to give to patients about fertility preservation | 28 (15%) |
| Patients do not want to discuss fertility preservation | 25 (14%) |
| There is no place/person to refer my patients | 22 (12%) |
| No barriers | 29 16%) |
Respondents could choose multiple responses
We observed no differences in reported barriers by physician gender. However, when considering practice type, pediatric practitioners were less likely to feel that their patients were too ill to delay transplant for FP (47% vs. 70% for adult providers, P=0.02), were less likely to feel that their patients were not interested in discussing fertility issues (8% vs. 24%, P=0.04) and were less likely to report that time constraints affected their ability to discuss FP (10% vs. 26%, P=0.003). Once again, the greatest differences were observed by access to an infertility specialist. Those with access were less likely perceive that patients do not want to discuss fertility (14% vs. 69% without access, P< 0.0001), report that their patients were already infertile due to prior therapy (40% vs. 92%, P<0.0001), report that lack of infertility specialists was a barrier (5% vs. 77%, P<0.0001), and perceive time constraints limited their ability to discuss fertility issues (16% vs. 77%, P<0.0001).
Fertility preservation attitudes and perceptions
Transplant physicians recognize that patients are interested in learning about the impact of transplant on their fertility. A greater proportion of respondents felt that risks of infertility were higher among recipients of total body irradiation, myeloablative conditioning and allogeneic HCT. There were no notable differences by gender or by practice type. Physicians with access to an infertility specialist were more likely to perceive patients were interested in learning about fertility (88% vs. 23% with no access, P<0.0001).
Factors Predictive for Consultation or Referral to Infertility Specialist
Table 3 lists survey responses and characteristics of physicians who consulted or referred their patients to an infertility specialist. Physicians who reported that they “Rarely” or “Never” consulted or referred were more likely to report specific perceived barriers to FP (e.g., patients not interested, referral challenges and time constraints). Physician gender, practice type or center size was similar among respondents who did and did not consult or refer patients to infertility specialists. Physicians who graduated from medical school prior to 1990 were more likely to consult or refer. Finally, access to an infertility specialist was an important determinant of whether physicians consulted or referred their patients for FP.
Table 3.
Fertility preservation barriers reported and characteristics of physicians who consulted or referred their patients to an infertility specialist
| Characteristic | Consult infertility specialist, %†
|
P-value | Refer to infertility specialist, %†
|
P-value | ||||
|---|---|---|---|---|---|---|---|---|
| Always/often | Sometimes | Rarely/never | Always/often | Sometimes | Rarely/never | |||
| N | 54 | 64 | 62 | 98 | 50 | 31 | ||
|
| ||||||||
| Barriers* | ||||||||
|
| ||||||||
| Patients too ill to delay transplant | 47 | 64 | 76 | 0.008 | 55 | 69 | 77 | 0.14 |
|
| ||||||||
| Patient cannot afford fertility preservation | 45 | 48 | 43 | 0.64 | 48 | 43 | 37 | 0.39 |
|
| ||||||||
| Patients do not want to discuss fertility preservation | 6 | 13 | 34 | 0.0003 | 13 | 12 | 45 | 0.0001 |
|
| ||||||||
| Patients already infertile | 39 | 33 | 60 | 0.03 | 38 | 47 | 61 | 0.16 |
|
| ||||||||
| No place to refer patients | 4 | 2 | 26 | <0.0001 | 3 | 4 | 45 | <0.0001 |
|
| ||||||||
| Time constraints | 4 | 18 | 37 | 0.001 | 12 | 18 | 53 | <0.0001 |
|
| ||||||||
| Insurance does not cover fertility preservation | 55 | 40 | 38 | 0.03 | 45 | 45 | 37 | 0.09 |
|
| ||||||||
| Physician characteristics | ||||||||
|
| ||||||||
| Gender | 0.45 | 0.90 | ||||||
| Male | 73 | 63 | 71 | 70 | 66 | 70 | ||
| Female | 27 | 37 | 29 | 30 | 34 | 30 | ||
|
| ||||||||
| Year of medical school graduation | 0.02 | 0.05 | ||||||
| Prior to 1990 | 62 | 65 | 44 | 62 | 56 | 37 | ||
| 1990 and later | 38 | 35 | 56 | 38 | 44 | 63 | ||
|
| ||||||||
| Practice type | 0.59 | 0.53 | ||||||
| Adult patients only | 63 | 69 | 72 | 67 | 65 | 77 | ||
| Pediatric ± adult patients | 37 | 31 | 28 | 33 | 35 | 23 | ||
|
| ||||||||
| Center size | 0.59 | 0.17 | ||||||
| Small | 8 | 14 | 18 | 12 | 9 | 28 | ||
| Medium | 33 | 28 | 32 | 30 | 30 | 31 | ||
| Large | 59 | 58 | 50 | 58 | 61 | 41 | ||
|
| ||||||||
| Access to infertility specialist | <0.0001 | <0.0001 | ||||||
| Yes, in my institution | 80 | 64 | 52 | 69 | 70 | 41 | ||
| Yes, in another institution in my community | 20 | 36 | 27 | 31 | 26 | 21 | ||
| No | 0 | 0 | 21 | 0 | 4 | 38 | ||
“Always” or “Often” responses are shown
Column percent; P-value compares “Always/often”, “Sometimes” and “Rarely/never”
We conducted bivariate analyses that considered physician characteristics, knowledge about fertility issues in HCT recipients, and their perception about whether HCT recipients were interested in learning about effects of transplant on fertility. Two factors were significantly associated with referral to infertility specialist – access to an infertility specialist (0 referrals among physicians with no access, P<0.001) and physicians belief that patients were interested in learning about the effects of transplant on fertility (OR 6.07, 95% CI: 1.25-25.60, P=0.02).
DISCUSSION
This is the first study to provide important information about the knowledge, attitudes, practices and referral patterns of adult and pediatric HCT physicians regarding FP among transplant recipients. Several important themes emerge from our analysis. First, most transplant physicians were knowledgeable and comfortable discussing fertility issues relevant to their patients. This is in contrast to general oncologists where discussion rates are lower.10, 13 However, awareness and use of formal guidelines, educational materials, and resources for both physicians and patients were lacking. These rates were similar to those found among general oncologists who treat adults but lower than those found among a survey of pediatric oncologists.10, 16 A need for physician and patient resources specific for HCT recipients was identified, as many physicians felt that FP guidelines and materials for cancer patients were not relevant to HCT recipients.
We identified several physician reported barriers that hinder discussions with patients about FP. Many physicians felt that transplant usually has to be pursued urgently and delaying transplant to pursue FP may not be in the best interest of the patient and that pre-transplant therapies can cause infertility. This concern is valid for many patients who have high-risk diseases that require urgent HCT and even though FP is discussed, there may not be sufficient time to pursue FP or FP methods may prove to be ineffective. Other perceptions that may serve as barriers to discussing FP were identified, including inability to afford FP by patients, lack of insurance coverage for FP, lack of patient interest in discussing FP and lack of sufficient knowledge to discuss FP. Insufficient time to discuss fertility issues was noted as a barrier by some. Availability of HCT specific physician and patient educational resources may mitigate some of these barriers. In addition, models of care may be considered where discussion about FP could be conducted by another provider from the transplant center (e.g., mid-level providers or social workers).
An important determinant in discussing fertility with patients undergoing transplant is having access to an infertility specialist. Transplant physicians without access to these specialists were far more likely to underestimate the psychosocial impact of infertility and to believe that patients do not wish to discuss fertility. They were significantly less likely to consult and to refer to infertility specialists, and were even less aware of guidelines, educational materials, and resources available to assist them and their patients. Our findings behoove transplant physicians to reach out to and foster collaborative relationships with their colleagues who are experts in FP to facilitate appropriate and timely care of HCT recipients who are interested in FP. In addition, general adult and pediatric oncologists may not always discuss and pursue FP with their patients.10, 13, 16 Education and outreach to oncologists would also facilitate appropriate and timely interventions for FP prior to a patient referral for HCT.
We also observed significant differences between adult treating and pediatric transplant physicians’ knowledge, attitudes, and practices. Most notably, pediatric providers were more likely to discuss infertility with patients who had poor prognosis and were less likely to feel that their patients were too sick to discuss FP or that time constraints limited this conversation. However, practice type was not associated with likelihood of consultation or referral to infertility specialist.
In their survey of US oncologists, Quinn et al observed that referrals for FP were more likely among female physicians, physicians with favorable attitudes about FP, and physicians whose patients routinely asked about FP.10 We also found that the likelihood of referral was higher among physicians who felt that their patients were interested in learning about fertility and FP. Physician characteristics such as gender, practice type, year of medical school graduation or transplant center size were not found to be predictive of referral to infertility specialist in multivariate analyses.
Some limitations of our study have to be considered. The response rate to our survey was lower than what has been reported for email/web physician surveys not providing an incentive (typically 25-40%).17, 18 Furthermore, physicians who elected to participate may be relatively more knowledgeable about survivorship and fertility issues, and thus this sample may not be representative of the transplant community and the barriers to FP may even be greater among transplant physicians in general. This bias may also explain the high proportion of respondents who felt comfortable discussing and actually discussed FP with their patients. On the same note, physicians might overestimate their frequency of discussing impact of HCT on fertility.19 Also, our findings are specific to physicians practicing in the US and different medical, cultural and economical factors may influence FP practices for physicians who practice in other countries.
In conclusion, our study highlights the variation in practices and perceptions about FP among US adult and pediatric HCT physicians and identifies barriers to having physician-patient discussions about the impact of HCT on fertility. We also identify a need to develop educational materials and guidelines for physicians that may facilitate the discussion of FP with their patients.
Supplementary Material
Acknowledgments
Support
The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement U24-CA76518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U01HL069294 from NHLBI and NCI; a contract HHSH234200637015C with Health Resources and Services Administration (HRSA/DHHS); two Grants N00014-06-1-0704 and N00014-08-1-0058 from the Office of Naval Research; and grants from Allos, Inc.; Amgen, Inc.; Angioblast; Anonymous donation to the Medical College of Wisconsin; Ariad; Be the Match Foundation; Blue Cross and Blue Shield Association; Buchanan Family Foundation; CaridianBCT; Celgene Corporation; CellGenix, GmbH; Children’s Leukemia Research Association; Fresenius-Biotech North America, Inc.; Gamida Cell Teva Joint Venture Ltd.; Genentech, Inc.; Genzyme Corporation; GlaxoSmithKline; HistoGenetics, Inc.; Kiadis Pharma; The Leukemia & Lymphoma Society; The Medical College of Wisconsin; Merck & Co, Inc.; Millennium: The Takeda Oncology Co.; Milliman USA, Inc.; Miltenyi Biotec, Inc.; National Marrow Donor Program; Optum Healthcare Solutions, Inc.; Osiris Therapeutics, Inc.; Otsuka America Pharmaceutical, Inc.; RemedyMD; Sanofi; Seattle Genetics; Sigma-Tau Pharmaceuticals; Soligenix, Inc.; StemCyte, A Global Cord Blood Therapeutics Co.; Stemsoft Software, Inc.; Swedish Orphan Biovitrum; Tarix Pharmaceuticals; Teva Neuroscience, Inc.; THERAKOS, Inc.; and Wellpoint, Inc. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, or any other agency of the U.S. Government.
Footnotes
Financial Disclosures: None of the authors have any relevant financial conflicts of interest to disclose.
References
- 1.Lee SJ, Schover LR, Partridge AH, Patrizio P, Wallace WH, Hagerty K, et al. American Society of Clinical Oncology recommendations on fertility preservation in cancer patients. J Clin Oncol. 2006;24(18):2917–31. doi: 10.1200/JCO.2006.06.5888. [DOI] [PubMed] [Google Scholar]
- 2.Carter A, Robison LL, Francisco L, Smith D, Grant M, Baker KS, et al. Prevalence of conception and pregnancy outcomes after hematopoietic cell transplantation: report from the Bone Marrow Transplant Survivor Study. Bone Marrow Transplant. 2006;37(11):1023–9. doi: 10.1038/sj.bmt.1705364. [DOI] [PubMed] [Google Scholar]
- 3.Gulati SC, Van Poznak C. Pregnancy after bone marrow transplantation. J Clin Oncol. 1998;16(5):1978–85. doi: 10.1200/JCO.1998.16.5.1978. [DOI] [PubMed] [Google Scholar]
- 4.Hammond C, Abrams JR, Syrjala KL. Fertility and risk factors for elevated infertility concern in 10-year hematopoietic cell transplant survivors and case-matched controls. J Clin Oncol. 2007;25(23):3511–7. doi: 10.1200/JCO.2007.10.8993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salooja N, Szydlo RM, Socie G, Rio B, Chatterjee R, Ljungman P, et al. Pregnancy outcomes after peripheral blood or bone marrow transplantation: a retrospective survey. Lancet. 2001;358(9278):271–6. doi: 10.1016/s0140-6736(01)05482-4. [DOI] [PubMed] [Google Scholar]
- 6.Sanders JE, Hawley J, Levy W, Gooley T, Buckner CD, Deeg HJ, et al. Pregnancies following high-dose cyclophosphamide with or without high-dose busulfan or total-body irradiation and bone marrow transplantation. Blood. 1996;87(7):3045–52. [PubMed] [Google Scholar]
- 7.Loren AW, Chow E, Jacobsohn DA, Gilleece M, Halter J, Joshi S, et al. Pregnancy after hematopoietic cell transplantation: a report from the late effects working committee of the Center for International Blood and Marrow Transplant Research (CIBMTR) Biol Blood Marrow Transplant. 17(2):157–66. doi: 10.1016/j.bbmt.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Borgmann-Staudt A, Rendtorff R, Reinmuth S, Hohmann C, Keil T, Schuster FR, et al. Fertility after allogeneic haematopoietic stem cell transplantation in childhood and adolescence. Bone Marrow Transplant. 2012;47(2):271–6. doi: 10.1038/bmt.2011.78. [DOI] [PubMed] [Google Scholar]
- 9.Scanlon M, Blaes A, Geller M, Majhail NS, Lindgren B, Haddad T. Patient satisfaction with physician discussions of treatment impact on fertility, menopause and sexual health among pre-menopausal women with cancer. J Cancer. 2012;3:217–25. doi: 10.7150/jca.4408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quinn GP, Vadaparampil ST, Lee JH, Jacobsen PB, Bepler G, Lancaster J, et al. Physician referral for fertility preservation in oncology patients: a national study of practice behaviors. J Clin Oncol. 2009;27(35):5952–7. doi: 10.1200/JCO.2009.23.0250. [DOI] [PubMed] [Google Scholar]
- 11.Schover LR, Brey K, Lichtin A, Lipshultz LI, Jeha S. Oncologists’ attitudes and practices regarding banking sperm before cancer treatment. J Clin Oncol. 2002;20(7):1890–7. doi: 10.1200/JCO.2002.07.174. [DOI] [PubMed] [Google Scholar]
- 12.Knapp CA, Quinn GP. Healthcare provider perspectives on fertility preservation for cancer patients. Cancer Treat Res. 2010;156:391–401. doi: 10.1007/978-1-4419-6518-9_30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kohler TS, Kondapalli LA, Shah A, Chan S, Woodruff TK, Brannigan RE. Results from the survey for preservation of adolescent reproduction (SPARE) study: gender disparity in delivery of fertility preservation message to adolescents with cancer. Journal of assisted reproduction and genetics. 2011;28(3):269–77. doi: 10.1007/s10815-010-9504-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quinn GP, Vadaparampil ST, Gwede CK, Miree C, King LM, Clayton HB, et al. Discussion of fertility preservation with newly diagnosed patients: oncologists’ views. J Cancer Surviv. 2007;1(2):146–55. doi: 10.1007/s11764-007-0019-9. [DOI] [PubMed] [Google Scholar]
- 15.Vadaparampil S, Quinn G, King L, Wilson C, Nieder M. Barriers to fertility preservation among pediatric oncologists. Patient education and counseling. 2008;72(3):402–10. doi: 10.1016/j.pec.2008.05.013. [DOI] [PubMed] [Google Scholar]
- 16.Forman EJ, Anders CK, Behera MA. A nationwide survey of oncologists regarding treatment-related infertility and fertility preservation in female cancer patients. Fertil Steril. 2010;94(5):1652–6. doi: 10.1016/j.fertnstert.2009.10.008. [DOI] [PubMed] [Google Scholar]
- 17.Martins Y, Lederman RI, Lowenstein CL, Joffe S, Neville BA, Hastings BT, et al. Increasing response rates from physicians in oncology research: a structured literature review and data from a recent physician survey. Br J Cancer. 2012;106(6):1021–6. doi: 10.1038/bjc.2012.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.VanGeest JB, Johnson TP, Welch VL. Methodologies for improving response rates in surveys of physicians: a systematic review. Eval Health Prof. 2007;30(4):303–21. doi: 10.1177/0163278707307899. [DOI] [PubMed] [Google Scholar]
- 19.Hohmann C, Borgmann-Staudt A, Rendtorff R, Reinmuth S, Holzhausen S, Willich SN, et al. Patient counselling on the risk of infertility and its impact on childhood cancer survivors: results from a national survey. Journal of psychosocial oncology. 2011;29(3):274–85. doi: 10.1080/07347332.2011.563344. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


