Abstract
Purpose
To examine the effects of Reiki as an adjuvant therapy to opioid therapy for postoperative pain control in pediatric patients.
Methods
This was a double-blind, randomized controlled study of children undergoing dental procedures. Participants were randomly assigned to receive either Reiki therapy or the control therapy (sham Reiki) preoperatively. Postoperative pain scores, opioid requirements, and side effects were assessed. Family members were also asked about perioperative care satisfaction. Multiple linear regressions were used for analysis.
Results
Thirty-eight children participated. The blinding procedure was successful. No statistically significant difference was observed between groups on all outcome measures.
Implications
Our study provides a successful example of a blinding procedure for Reiki therapy among children in the perioperative period. This study does not support the effectiveness of Reiki as an adjuvant therapy to opioid therapy for postoperative pain control in pediatric patients.
Keywords: Pain, postoperative; Reiki therapy; Pain management; Analgesics, opioid
1. Background
A significant number (38–95%) of children experience postoperative pain and discomfort following dental procedures, as reported either by children themselves or from parental observation [1–4]. The use of Complementary and Alternative Medicine among adults and children for pain management is increasing, and the use of these therapies is governed by patients’ or their families’ desires to follow a more integrative approach to medical care [5–7]. The current pilot study aimed to evaluate whether Reiki therapy is beneficial in postoperative pain management as an adjuvant to opioid therapy in pediatric patients undergoing either elective dental procedures, including restorative and extraction work, or palatoplasty with or without bilateral myringotomy.
Reiki therapy is a biofield energy healing modality [8] defined by the National Center for Complementary and Alternative Medicine as “a health practice in which practitioners place their hands lightly on or just above the person, with the goal of facilitating the person's own healing response.” [9] According to the Reiki paradigm, surgery disrupts a patient's energy flow and energy patterns, thus resulting in a greater vulnerability to pain and discomfort due to a blockage of the energy center [10]. A Reiki practitioner places his or her hands in a series of positions on or above the recipient's body to realign and strengthen the energy flow by transmitting “Reiki” (a form of universal life energy) into the body [11] and consequently influencing the body's physical and psychological functioning as well as its spiritual well-being [8].
Previous studies have indicated that Reiki therapy supports opioid therapy in relieving pain by reducing pain intensity and improving quality of life among cancer patients [12,13]. Reiki therapy also has had a positive impact on the management of pain, anxiety, and depression in chronically ill patients [14]. The possibility of incorporating Reiki therapy following surgery has been explored [15]. Among patients undergoing dental procedures, a significant reduction in pain perception and experience has been demonstrated in a study of patients undergoing removal of impacted teeth [16]. The available data on adults regarding the efficacy of Reiki therapy for pain management suggests that a potential may exist for the pediatric population. Unfortunately, the available evidence evaluating the therapeutic role of Reiki therapy, especially among pediatric patients, is scarce and fraught with poor methodological design [17,18]. Considering the noninvasive nature of Reiki therapy and its potential to provide comfort and relaxation, it may be a valuable adjuvant therapy among the pediatric population [5].
2. Methods
The study took place at Seattle Children's Hospital. Seattle Children's Hospital serves a diverse population drawn from a five-state region. Reiki therapy is not the standard of care at Seattle Children's Hospital; however, the hospital does not preclude providing Reiki therapy in addition to standard analgesic therapy. The children who were enrolled in this study and randomized to the intervention group received Reiki therapy that was a noninvasive comfort therapy with the potential to promote the body's ability to self-heal and enhance endogenous analgesia. This study was approved by the Seattle Children's Hospital Institutional Review Board.
2.1. Design
A single-site, double-blind, randomized controlled study investigating the effects of Reiki therapy on postoperative pain management in children was conducted. This study aimed to evaluate the effects of an intervention (Reiki) on pain scores, analgesic medication requirements, side effects, and family satisfaction related to perioperative care compared with the control treatment (sham Reiki).
2.2. Participants
Eligible participants were children aged 9 months to 4 years who were scheduled for elective dental work, including restorative and extraction procedures, or for palatoplasty surgery without need for a bone graft. The dental procedure patients were discharged home the same day, while the palatoplasty patients were routinely admitted to the hospital for 1–2 postoperative days. The palatoplasty patients were often scheduled simultaneously for the bilateral myringotomy tube or ear tube placements, since ear infections are commonly associated with cleft palate. Combining the two procedures avoids patient exposure to multiple anesthetics and multiple hospital visits. Fluency in English for at least one of the parents or legal guardians was a requirement for inclusion in the study. Patients who were given regional blocks for anesthesia during surgery were excluded from the study.
2.3. Procedures
Study participants were identified by review of the Seattle Children's Hospital operating room schedule. Eligibility for the study was determined by a member of the research team, based on review of the patient's chart, or in collaboration with the surgery and anesthesia team. Once the patient's eligibility was determined, a member of the research team then discussed the study with the patient and family. Following the guidelines set out by the Seattle Children's Hospital and the Pediatric Committee on Bioethics regarding consent to participate in research for children less than 7 years of age, signed parental consent was obtained and the parents’ had an opportunity to ask questions related to study participation [19].
The participants who met the inclusion criteria and had parents’ signed consent to participate were randomly assigned to one of two groups: (a) to receive preoperative Reiki therapy or (b) to receive preoperative sham Reiki therapy. To allow randomization without great distortion in each group, a randomization design with balanced permuted blocks of 10 that were stratified by surgical procedure (cleft palate 60% and dental procedures 40%) were created and distributed sequentially.
Practitioners of both Reiki and sham Reiki were present outside the examination room when a study participant was scheduled to receive therapy. A member of the research team gave the practitioners an envelope with the randomization assignment for the study participant. This research team member then left the area, and the practitioners opened the randomization envelope to determine who would enter the participant's room to provide the therapy (Reiki or sham Reiki).
The Reiki therapy was performed in an exam room at the surgery center. The duration of the therapy was 20–30 min. Once the therapy was complete, the participants waited in the exam room until their surgery was ready to commence, at which point they were brought to the operating room. The participants received a standard anesthetic and standard intraoperative pain management during their surgery.
Postoperatively, participants’ pain scores were recorded both by a blinded observer and by their assigned nurse, who was also blinded to group assignment. Any medications administered in the postoperative period, and any side effects related to treatment experienced by the participant, were recorded by the research team member from a review of participants’ charts. These data were collected at any time within 15 min of the participant's arrival in the Post Anesthesia Care Unit (PACU), and subsequently at 30, 60, 120, and 180 min or at the time of discharge home, whichever occurred first. A brief family questionnaire was also administered 24 h after surgery either by telephone or in person.
2.4. Intervention
Reiki practitioners (a maximum of three) and sham Reiki practitioners (members of the research team not trained in Reiki) were employed for this study. The Reiki practitioners each had a Reiki Master degree certificate. To eliminate perceptible differences, and to keep the procedure consistent throughout the study period, we conducted a training session to prepare the practitioners (Reiki and sham Reiki) for the study. The standard script (conversation) with participants and families, centering and balancing of the Reiki practitioners, use of intention, hand positions on the patient's body, and duration of the therapy at each position (head, shoulders, chest, abdomen, knees, and feet) were standardized and discussed with all of the practitioners prior to starting participant enrollment.
Participants were brought, with their parents or caregivers, to an examination room in the surgery center where they would routinely be housed prior to any surgery. The participant could be in either a parent or caregiver's lap or on the bed for the Reiki or sham Reiki therapy. A “Do Not Disturb” sign was placed on the door to the exam room for the duration of the therapy, and no one else was allowed in the room during this time. A practitioner introduced him- or herself and explained the purpose of the visit using a standardized script. Once permitted to proceed, the practitioner placed his or her hands on standard positions on the participant's body systematically as determined per protocol. Parents and care-givers were blinded to the nature of the Reiki therapy administered. Once the therapy was complete, the practitioner left the room, recorded the data, sealed it in an envelope, placed it in a predetermined place, and left the premises. The participant waited in the exam room until it was time to proceed to the operation room for surgery.
2.5. Outcome measures
Age-appropriate pain scores were collected using the Face, Legs, Activity, Cry, Consolability (FLACC) scale. The FLACC scale is appropriate for preverbal children who are in pain from surgery [20]; it also has demonstrated reliability and validity [21]. Analgesic medication requirements and the incidence of side effects related to analgesic medication were also collected from participants’ charts. The total requirement of opioid analgesic used was scaled to morphine equivalents to calculate the opioid dose normalized by weight. Side effects were scored on a scale of 0–3 (0 = no side effects; 1 = single side effect but no intervention needed; 2 = more than one side effect but no intervention needed; 3 = side effects requiring an intervention).
Parents or caregivers completed a brief investigator-developed survey about their experience with Reiki and their satisfaction related to pain management and quality of care in the perioperative period. This satisfaction survey used a Likert-scale rating (5 = strongly agree and 1 = strongly disagree).
2.6. Statistical analysis
Descriptive statistics were used to summarize the demographic, anesthetic, and outcome variables at baseline, stratified by treatment group. The major outcome measures were cumulative and daily opioid usage, pain scores, and parent satisfaction scores. The effect of Reiki therapy on the outcome measures was analyzed by multiple linear regression models. The model used mean pain scores in the first 30 min, and cumulative opioid usage in the first 30 min normalized by weight, and the models adjusted for procedure type (dichotomized to dental procedure and palatoplasgy), gender, and age (for opioid usage model). Statistical analysis was completed using R 2.15.3 (R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria, 2013).
3. Results
3.1. Baseline participant characteristics
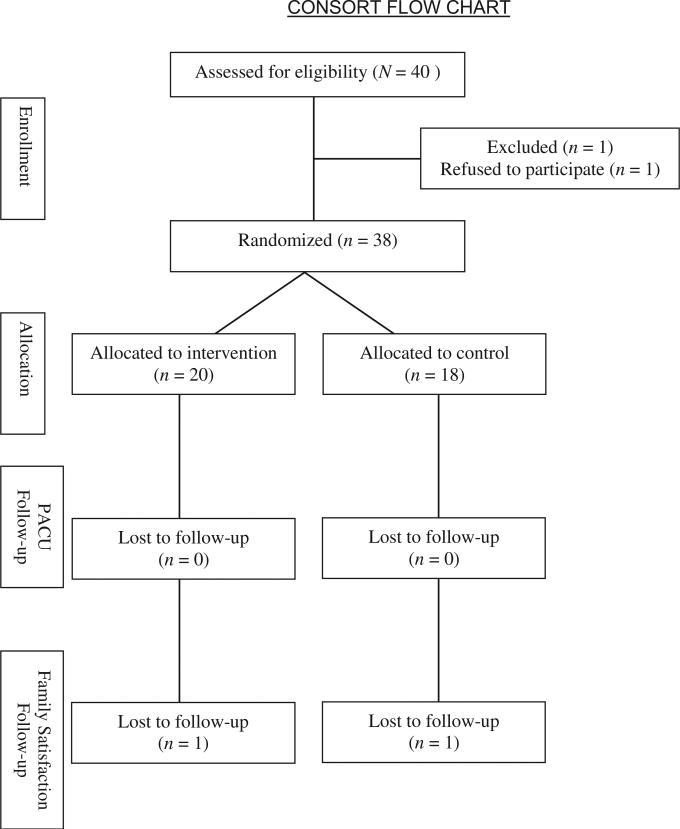
Thirty-eight participants were enrolled in this study (Fig. 1). The mean age was 25.6 months (range = 9–48 months), and 42% of the participants were male. The distribution of procedures showed that 65% of the participants had the palatoplasty procedure (18% had palatoplasty only and 47% had palatoplasty with bilateral myringotomy), and 35% of the participants had dental procedures (26% had restorative work, and 9% had dental extraction). The mean anesthesia duration was 157 min (SD = 53). Table 1 shows participants’ demographic data, procedure, and anesthesia distribution by group. The two groups did not differ significantly on the variables measured at baseline.
Fig. 1.
Consort flow chart.
Table 1.
Patient demographics and intraoperative data.
| Reiki (n = 20) | Sham Reiki (n = 18) | p-Value | |
|---|---|---|---|
| Mean age (yr) (range) | 28.6 (9–48) | 22.3 (4–48) | .45 |
| Gender (male/female) | 9/11 | 7/11 | NS |
| Mean weight (SD) (kg) | 12.7 (3.4) | 13.1 (6.8) | NS |
| Procedure | |||
| Palatoplasty | 4 | 3 | NS |
| Palatoplasty with BM | 8 | 10 | NS |
| Restorative | 7 | 3 | NS |
| Extraction | 1 | 2 | NS |
| Mean anesthesia duration (min) | 150 (48) | 166 (64) | NS |
| Intraoperative opioid dose (mg/kg) | 2.1 | 3.1 | <.01 |
NS = Not Significant.
3.2. Blinding
The blinding process was successful, as demonstrated by the parents’ or caregivers’ judgment of the type of Reiki therapy (true vs. sham) their children received. Sixteen parents (42%) reported “don't know,” and 12 parents (32%) reported a different type of Reiki therapy than what their child had actually received during the study.
3.3. Outcome measures
Pain scores and opioid requirement decreased after 30 min postoperatively, and the number of participants also decreased after 30 min due to early discharge; therefore, mean pain scores during the first 30 min and cumulative opioid usage in the first 30 min normalized by weight were used in the regression model. There was no statistically significant difference between the intervention and control groups on the major variables. The side effects reported included 1 child in the control group who experienced itching (side effect score = 1) and 1 child in the intervention group who experienced oxygen desaturation (side effect score = 3). There were no statistically significant differences in family satisfaction scores between the two groups.
4. Discussion
This is one of the few double-blind, randomized controlled studies looking into the effect of Reiki as an adjuvant to opioid therapy for pain control in children. We successfully developed a blinding procedure that eliminates the intention of the researchers, as well as a sham Reiki procedure that was identical to outside observers as true Reiki therapy. The success of the blinding process in our study is demonstrated by comparing the parents’ and caregivers’ inability to accurately identify the type of Reiki therapy (true vs. sham) that their children received. Parents who accompanied participants were relevant proxies since the participants of our study were very young children. One other study, Bowden and colleagues [22], has reported a blinding procedure. In that study, the participants were blinded to whether or not they were in a Reiki group, but the investigator, who was also a Reiki Master and provided Reiki to the participants, was not blinded. Thus, one cannot eliminate the possible influence of unintentional verbal and physical clues on the study results.
Reiki as an adjuvant therapy for postoperative pain control has been studied in three randomized controlled trials. An early randomized, double-blind, crossover design study by Wirth, Brelan, Levine, and Rodriquez [16] suggested that a combination of two kinds of biofield energy therapies (Reiki and LeShan healing) performed after unilateral operative extraction of the lower third molar for 6 h resulted in statistically significant difference in both level of pain intensity and degree of pain relief experienced for postoperative hours 4 through 9. Another randomized clinical trial studied the effect of Reiki on pain and anxiety among women who had undergone abdominal hysterectomies [23], and suggested that perioperative Reiki resulted in a significant decrease in pain scores at 24 h postoperatively, among the Reiki group; there was no difference between groups at 48 and 72 h postoperatively. More recently, a large, randomized, sham Reiki controlled trial evaluated the effect of Reiki as an adjuvant treatment for fibromyalgia patients [24]. Reiki therapy did not add additional benefit in all the outcome measures including pain intensity, physical and mental functioning, medication use, and health provider visits [24]. The mixed results of studies exploring the effect of Reiki therapy may relate to lack scientific rigor [17,18].
Our current pilot study extends the body of evidence about the effectiveness of Reiki therapy to a pediatric population in a study that also employed a rigorous study design. This study included children aged 9 months to 4 years who were scheduled for procedures in the head and neck area (palatoplasty and elective dental procedures). We found that the group receiving presurgery Reiki therapy did not differ in postoperative pain scores, opioid requirements, incidence of side effects, or family satisfaction based on their assignment to true or sham Reiki therapy preoperatively.
The limitations of our study include the small sample size and the heterogeneous dental procedures. These factors limit the interpretation of the study results, since pain results from the procedures differed. Additionally, we did not include measures to assess neuroendocrine or immune changes or changes in the participant's energy field.
Future research is still needed to explore the mechanism of Reiki therapy. An earlier study [25] indicated that Reiki works by affecting the neuroendocrine immune system; biochemical changes in terms of immune responsivity were also reported [22,26]. Despite the absence of scientific verification regarding the presence of biofield energy, anecdotal reports and proponents suggest that biofield therapy is clinically effective for relieving various symptoms, including physical pain, and for supporting well-being, but not to treat particular illnesses [8]. Many studies suggest that future studies may develop tools to directly measure the changes in subtle elements of the human energy field induced by Reiki therapy [27].
5. Conclusion
Our randomized controlled trial of Reiki therapy for postoperative pain among children suggests that young patients undergoing palatoplasty and elective dental procedures found no evidence of benefit from a single session of preoperative Reiki in terms of reducing pain intensity, analgesic requirements, incidence of side effects, and perioperative family satisfaction. Future studies employing homogeneous groups of procedures, with larger sample sizes might help provide further evidence.
Acknowledgments
Role of the funding source
Research reported in this publication was supported by intramural funding from Seattle Children's Hospital and by the National Cancer Institute of the National Institutes of Health under award number R42 CA141875.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Seattle Children's Hospital.
Footnotes
Conflict of interest statement
The authors declare that they have no conflicts of interest of any kind.
References
- 1.Staman NM, Townsend JA, Hagan JL. Observational study: discomfort following dental procedures for children. Pediatr Dent. 2013;35(1):52–4. [PubMed] [Google Scholar]
- 2.Mayeda C, Wilson S. Complications within the first 24 hours after dental rehabilitation under general anesthesia. Pediatr Dent. 2009;31(7):513–9. [PubMed] [Google Scholar]
- 3.Ashkenazi M, Blumer S, Eli I. Post-operative pain and use of analgesic agents in children following intrasulcular anaesthesia and various operative procedures. Br Dent J. 2007;202(5):E13. doi: 10.1038/bdj.2007.81. http://dx.doi.org/10.1038/bdj.2007.81 [discussion 276-7] [DOI] [PubMed] [Google Scholar]
- 4.Needleman HL, Harpavat S, Wu S, Alfred EN, Berde C. Postoperative pain and other sequelae of dental rehabilitations performed on children under general anesthesia. Pediatr Dent. 2008;30(2):111–21. [PubMed] [Google Scholar]
- 5.Kundu A, Dolan-Oves R, Dimmers MA, Towle CB, Doorenbos AZ. Reiki training for caregivers of hospitalized pediatric patients: a pilot program. Complement Ther Clin Pract. 2013;19(1):50–4. doi: 10.1016/j.ctcp.2012.08.001. http://dx.doi.org/10.1016/j.ctcp.2012.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelner M, Wellman B. Health care and consumer choice: medical and alternative therapies. Soc Sci Med. 1997;45(2):203–12. doi: 10.1016/s0277-9536(96)00334-6. [DOI] [PubMed] [Google Scholar]
- 7.Giordano J, Boatwright D, Stapleton S, Huff L. Blinding boundaries: steps toward an integration of complementary and alternative medicine into mainstream practice. J Altern Complement Med. 2002;8(6):897–906. doi: 10.1089/10755530260511892. [DOI] [PubMed] [Google Scholar]
- 8.Miles P, True G. Reikidreview of a biofield therapy history, theory, practice, and research. Altern Ther Health Med. 2003;9(2):62–72. [PubMed] [Google Scholar]
- 9.National Center for Complementary and Alternative Medicine . US Department of Health and Human Services, National Institutes of Health; Bethesda (MD): 2006. [2013 Jul 25]. Reiki: an introduction [Internet]. Available from: http://nccam.nih.gov/health/reiki/introduction.htm [updated 2013 Apr] [Google Scholar]
- 10.Behar M. Reiki: bridging traditional and complementary healing techniques. OT Pract. 1997;2(2):22–3. [Google Scholar]
- 11.Fazzino DL, Griffin MT, McNulty RS, Fitzpatrick JJ. Energy healing and pain: a review of the literature. Holist Nurs Pract. 2010;24(2):79–88. doi: 10.1097/HNP.0b013e3181d39718. http://dx.doi.org/10.1097/HNP.0b013e3181d39718. [DOI] [PubMed] [Google Scholar]
- 12.Olson K, Hanson J, Michaud M. A phase II trial of Reiki for the management of pain in advanced cancer patients. J Pain Symptom Manage. 2003;26(5):990–7. doi: 10.1016/s0885-3924(03)00334-8. [DOI] [PubMed] [Google Scholar]
- 13.Olson K, Hanson J. Using Reiki to manage pain: a preliminary report. Cancer Prev Control. 1997;1(2):108–13. [PubMed] [Google Scholar]
- 14.Dressen LJ, Singg S. Effects of Reiki on pain and selected affective and personality variables of chronically ill patients. Subtle Energies Energy Med. 1998;9(1):51–82. [Google Scholar]
- 15.Alandydy P. Using Reiki to support surgical patients. J Nurs Care Qual. 1999;13(4):89–91. doi: 10.1097/00001786-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Wirth DP, Brelan DR, Levine RJ, Rodriquez CM. The effect of complementary healing therapy on postoperative pain after surgical removal of impacted third molar teeth. Complement Ther Med. 1993;1(3):133–8. [Google Scholar]
- 17.Lee MS, Pittler MH, Ernst E. Effects of Reiki in clinical practice: a systematic review of randomised clinical trials. Int J Clin Pract. 2008;62(6):947–54. doi: 10.1111/j.1742-1241.2008.01729.x. [DOI] [PubMed] [Google Scholar]
- 18.vanderVaart S, Gijsen VM, de Wildt SN, Koren G. A systematic review of the therapeutic effects of Reiki. J Altern Complement Med. 2009;15(11):1157–69. doi: 10.1089/acm.2009.0036. [DOI] [PubMed] [Google Scholar]
- 19.Committee on Bioethics Informed consent, parental permission, and assent in pediatric practice. Pediatrics. 1995;95:314–7. [PubMed] [Google Scholar]
- 20.Manworren RC, Hynan LS. Clinical validation of FLACC: preverbal patient pain scale. Pediatr Nurs. 2003;29(2):140–6. [PubMed] [Google Scholar]
- 21.Crellin D, Sullivan TP, Babl FE, O'Sullivan R, Hutchinson A. Analysis of the validation of existing behavioral pain and distress scales for use in the procedural setting. Paediatr Anaesth. 2007;17(8):720–33. doi: 10.1111/j.1460-9592.2007.02218.x. [DOI] [PubMed] [Google Scholar]
- 22.Bowden D, Goddard L, Gruzelier J. A randomised controlled single-blind trial of the effects of Reiki and positive imagery on well-being and salivary cortisol. Brain Res Bull. 2010;81(1):66–72. doi: 10.1016/j.brainresbull.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Vitale AT, O'Connor PC. The effect of Reiki on pain and anxiety in women with abdominal hysterectomies: a quasi-experimental pilot study 2006. Holist Nurs Pract. 2007;20(6):263–72. [PubMed] [Google Scholar]
- 24.Assefl N, Bogart A, Goldberg J, Buchwald D. Reiki for the treatment of fibromyalgia: a randomized controlled trial. J Altern Complement Med. 2008;14(9):1115–22. doi: 10.1089/acm.2008.0068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mansour AA, Beuche M, Laing G, Leis A, Nurse J. A study to test the effectiveness of placebo Reiki standardization procedures. J Altern Complement Med. 1999;5(2):153–64. doi: 10.1089/acm.1999.5.153. [DOI] [PubMed] [Google Scholar]
- 26.Mackay N, Hansen S, McFarlane O. Autonomic nervous system changes during Reiki treatment: a preliminary study. J Altern Complement Med. 2004;10(6):1077–81. doi: 10.1089/acm.2004.10.1077. [DOI] [PubMed] [Google Scholar]
- 27.Snyder M, Lindquist R. Complementary and alternative therapies in nursing. 6th ed. Springer Publishing Company; New York: 2009. [Google Scholar]