Abstract
Background
The American Heart Association’s 2020 Strategic Impact Goals target a 20% relative improvement in overall cardiovascular health with the use of 4 health behavior (smoking, diet, physical activity, body mass) and 3 health factor (plasma glucose, cholesterol, blood pressure) metrics. We sought to define current trends and forward projections to 2020 in cardiovascular health.
Methods and Results
We included 35 059 cardiovascular disease–free adults (aged ≥20 years) from the National Health and Nutrition Examination Survey 1988–1994 and subsequent 2-year cycles during 1999–2008. We calculated population prevalence of poor, intermediate, and ideal health behaviors and factors and also computed a composite, individual-level Cardiovascular Health Score for all 7 metrics (poor=0 points; intermediate=1 point; ideal=2 points; total range, 0–14 points). Prevalence of current and former smoking, hypercholesterolemia, and hypertension declined, whereas prevalence of obesity and dysglycemia increased through 2008. Physical activity levels and low diet quality scores changed minimally. Projections to 2020 suggest that obesity and impaired fasting glucose/diabetes mellitus could increase to affect 43% and 77% of US men and 42% and 53% of US women, respectively. Overall, population-level cardiovascular health is projected to improve by 6% overall by 2020 if current trends continue. Individual-level Cardiovascular Health Score projections to 2020 (men=7.4 [95% confidence interval, 5.7–9.1]; women=8.8 [95% confidence interval, 7.6–9.9]) fall well below the level needed to achieve a 20% improvement (men=9.4; women=10.1).
Conclusions
The American Heart Association 2020 target of improving cardiovascular health by 20% by 2020 will not be reached if current trends continue.
Keywords: cardiovascular disease risk factors, epidemiology, risk factors, trends
The American Heart Association (AHA) 2020 Strategic Impact Goals target a 20% relative improvement in overall cardiovascular health in all Americans with the use of 4 health behavior (smoking, diet, physical activity, body weight) and 3 health factor (plasma glucose, cholesterol, blood pressure) metrics.1 The 2020 goals were conceptualized on the basis of 3 key concepts of health promotion and disease prevention: (1) effectiveness of primordial prevention; (2) life course nature of cardiovascular disease (CVD) development and CVD risk factors; and (3) balance between population- and individual-level prevention.1 A higher number of health behaviors and factors at ideal levels is associated with substantially lower cardiovascular event rates in short- and long-term follow-up.1,2 However, given the very low prevalence of individuals with ideal cardiovascular health,3 a 20% relative improvement would have a small absolute effect on the population. Concurrent shifts from poor to intermediate levels of health behaviors and factors will also be needed to realize substantial improvements across the spectrum of cardiovascular health. The 20% target was deemed aggressive yet achievable by consensus.1
Current trends of these composite cardiovascular health metrics are unclear. Decreases in smoking4 and exposure to secondhand smoke5 have slowed. Nationally representative data continue to suggest poor dietary quality for most of the population,6 but increases in obesity prevalence may be slowing.7 Trends in physical activity are mixed,4 but diabetes mellitus prevalence rates are rising.4 Total cholesterol levels are decreasing, in part because of a doubling in the use of lipid-lowering drugs.8 Despite population-level increases in body weight, mean blood pressure and blood pressure control are improving.9
We therefore sought to evaluate recent trends in composite cardiovascular health metrics and to estimate future levels of cardiovascular health behaviors and factors among adults in the United States to determine whether the AHA 2020 goals will be met if current trends continue.
Methods
We used data from noninstitutionalized, nonpregnant, nonlactating adults aged ≥20 years in each age, sex, and race/ethnicity group as appropriate who were free from CVD and participated in the Third National Health and Nutrition Examination Survey (NHANES III, 1988–1994) and subsequent 2-year cycles (1999 –2000, 2001–2002, 2003–2004, 2005–2006, 2007–2008). Methods of measurement of each health behavior and health factor have been reported previously and are described in the online-only Data Supplement.10 We defined CVD as any self-reported history of myocardial infarction, angina, stroke, or heart failure. We calculated prevalence estimates from 1988 to 2008 of ideal, intermediate, and poor levels of the 7 cardiovascular health behaviors and health factors, as defined by the AHA 2020 Impact Goals (Table 1).1
Table 1.
Definitions of Cardiovascular Health Metrics, as Defined by the American Heart Association’s 2020 Strategic Impact Goals Committee
| Level of Cardiovascular Health | |||
|---|---|---|---|
| Metric | Poor | Intermediate | Ideal |
| Smoking | Current smoker | Quit smoking <12 mo | Never smoker or quit smoking ≥12 mo |
| Diet* | Diet score=0–1 | Diet score=2–3 | Diet score=4–5 |
| Physical activity† | No physical activity | 1–149 min/wk of moderate intensity, 1–74 min/wk of vigorous intensity, or 1–149 min/wk moderate plus vigorous intensity activity (whereby time in vigorous activity is doubled) | ≥150 min/wk of moderate intensity, ≥75 min/wk of vigorous intensity, or ≥150 min/wk of moderate plus vigorous intensity activity (in which time in vigorous activity is doubled) |
| Body weight | BMI ≥30 kg/m2 | BMI 25–29.9 kg/m2 | BMI <25 kg/m2 |
| Glucose/diabetes mellitus | FPG ≥126 mg/dL or diagnosed diabetes mellitus with HbA1c ≥7% | FPG 100–125 mg/dL or diagnosed diabetes mellitus with HbA1c <7% | FPG <100 mg/dL |
| Cholesterol | Total cholesterol ≥240 or treated total cholesterol >200 mg/dL | Total cholesterol 200–239 or treated total cholesterol <200 mg/dL | Total cholesterol <200 mg/dL |
| BP | Treated BP >140/>90 and SBP ≥140 or DBP ≥90 mm Hg | SBP 120–139 or DBP 80–89 or treated BP <140/<90 mm Hg | BP <120/<80 mm Hg |
BMI indicates body mass index; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; BP, blood pressure; SBP, systolic blood pressure; and DBP, diastolic blood pressure.
Diet score (scale: 0–5) was calculated on the basis of 1 point for each of 5 components, including ≥4.5 cups per day of fruits/vegetables, ≥2 servings of fish per week (3.5-oz servings), <1500 mg/d of sodium, ≤450 kcal (36 oz) per week of sweets/sugar-sweetened beverages, and ≥3 servings per day of whole grains (1.1 g of fiber in 10 g of carbohydrate; 1-oz equivalent servings).
Leisure-time physical activity.
Statistical Analyses
All analyses were performed with the use of SAS version 9.1 (SAS Institute, Cary, NC) with the complex sampling design taken into account. We used the standard 2000 US population to adjust the data for age using 3 age strata (20 –39, 40–59, and ≥60 years). To estimate time trends from 1988 to 2008 and average annual change in cardiovascular health factors and behaviors, we performed weighted linear regression using estimated mean values or percentages as dependent variables and survey time as independent variables. We fitted weighted linear regression models with prevalence as the dependent variables and survey time as independent variables. The β coefficients indicate the average annual change in the prevalence. On the basis of the findings, we projected the future situation of year 2020 assuming that trends would continue to change at a similar rate. We calculated prediction intervals on the basis of SE of the predicted prevalence estimates. Reciprocals of variances were used as weights. We projected estimates to 2020 by assuming that trends would continue in a manner similar to those observed over the past 2 decades in a linear fashion. Because the methodology used to measure diet and physical activity had changed from NHANES III to the 1999–2008 cycles, we excluded NHANES III dietary and physical activity data and only included 1999–2008 data. Likewise, because the methodology used to measure physical activity changed between the 2005–2006 and 2007–2008 cycles, we excluded 2007–2008 cycle physical activity data. We performed a sensitivity analysis by including individuals with CVD, and the overall prevalence trends and 2020 projections were not substantively different (<3% absolute difference in all 2020 projections including individuals with prevalent CVD).
We projected the situation for 2020 by assuming that trends would continue to change at a similar rate. We considered alternative statistical methods such as linear models with a quadratic term for time to assess nonlinear trends, but the results differed little from standard linear models with the sole exception of blood pressure trends in women. The majority of our final estimated models had coefficients of determination (R2) values of 0.80 and better. Results from log-linear and logit models were nearly identical to the results from linear models. In addition, the projected 2020 estimates for blood pressure in women with a model with a quadratic term were substantially lower than a realistic value. Thus, we chose to use the linear models for simplicity. Estimates with a coefficient of variation >30% were considered unreliable.11 Data are presented as mean and 95% confidence interval (CI). A P value <0.05 defined statistical significance.
We compared these estimates based on current trends with a 20% improvement in cardiovascular health metrics from 2006 to 2020 because the AHA used 2006 as a reference point. A 20% improvement in cardiovascular health was defined as the average of a 20% relative decrease in the prevalence of poor cardiovascular health metrics and a 20% relative increase in the prevalence of ideal cardiovascular health across the 7 metrics. This method minimizes the likelihood of demonstrating an improvement in cardiovascular health that is driven solely by a reduction in poor health, which could be due to higher death rates in that group. Categories of ideal, intermediate, and poor levels of each metric are exclusive from each other. Thus, the prevalence estimates across different categories of each item (poor smoking, intermediate smoking, and ideal smoking, for example) sum to 100% by definition. For projections to 2020, we created estimates by first accounting for changes in ideal and poor levels of each metric and created estimates for intermediate levels on the basis of the remaining prevalence.
To capture individual-level changes in cardiovascular health factors and behaviors, we created a composite, individual-level Cardiovascular Health Score based on the individual-level composite of all 7 cardiovascular health behaviors and health factors (poor=0 points; intermediate=1 point; ideal=2 points; total scale: 0–14 points). This score is not a risk prediction tool but helps to assess individual-level trends amid population-level trends in cardiovascular health. We assessed changes in the score from 1999 to 2006 and performed forward projections to 2020 in a similar manner. We did not calculate Cardiovascular Health Scores for NHANES III and for the 2007–2008 cycle because of methodological differences in diet and physical activity data collection from 1999 to 2006.
Results
Among 79 932 participants who attended interviews and examination measurements from 1988 to 2008, we analyzed data from up to 35 059 participants. Reasons for exclusion were as follows: age <20 years (n=38 666; 48.4%), women pregnant or lactating (n=1628; 2.0%), and prior CVD, defined as prior myocardial infarction, angina, stroke, or heart failure (n=4579; 5.7%) (Figure I in the online-only Data Supplement). Participants’ mean age was 44.4 years, and 51% were women.
Prevalence estimates for adults categorized as poor, intermediate, and ideal for cardiovascular health components in 1988–1994 and 2007–2008 are displayed by sex in Tables 2 and 3. In addition, β coefficients and SEs from weighted linear regression models, representing trends for each metric by including data from all NHANES samples, and coefficients of determination (R2) are displayed.
Table 2.
Prevalence Estimates (95% CI) and 2020 Projections of Poor, Intermediate, and Ideal Levels of Cardiovascular Health Components for US Men: NHANES (1988 –2008)
| NHANES III (1988 –1994) |
2007–2008 | β (SE) | P | R2 | 2020 Projection (95% CI) |
|
|---|---|---|---|---|---|---|
| Smoking | ||||||
| Poor | 30.8 (27.9–33.8) | 25.6 (21.1–30.2) | −0.29 (0.08) | 0.02 | 0.77 | 22.5 (16.5–28.5) |
| Intermediate | 1.9 (1.0–2.9) | 2.7 (1.4–4.0) | 0.08‡§ (0.04) | 0.07 | 0.59 | 4.5 (1.5–7.5) |
| Ideal | 67.3 (64.3–70.2) | 71.7 (67.7–75.6) | 0.21 (0.08) | 0.05 | 0.65 | 73.0 (66.7–79.3) |
| Healthy diet* | ||||||
| Poor | 82.5 (78.3–86.6) | 81.6 (78.7–84.5) | 0.03§ (0.15) | 0.85 | 0.02 | 82.0 (72.5–91.6) |
| Intermediate | 17.2 (13.2–21.3) | 17.8 (14.6–21.0) | −0.07§ (0.16) | 0.71 | 0.05 | 16.8 (7.2–26.5) |
| Ideal | 0.3 (0–0.8) | 0.6 (0–1.2) | 0.04‡ (0.01) | 0.04 | 0.81 | 1.2 (0.3–2.1) |
| Physical activity† | ||||||
| Poor | 36.8 (31.3–42.2) | 30.4 (24.0–36.9) | −0.80§ (0.69) | 0.36 | 0.40 | 17.3 (0–65.0) |
| Intermediate | 18.4 (14.4–22.3) | 20.2 (15.6–24.8) | 0.44§ (0.23) | 0.19 | 0.65 | 26.6 (10.3–42.9) |
| Ideal | 44.8 (38.4–51.3) | 49.4 (43.5–55.2) | 0.33§ (0.79) | 0.72 | 0.10 | 56.1 (0–100) |
| Body weight | ||||||
| Poor | 19.9 (17.5–22.1) | 31.6 (27.3–36.0) | 0.83 (0.07) | <0.01 | 0.97 | 43.4 (37.9–49.4) |
| Intermediate | 41.2 (37.9–44.1) | 40.2 (35.8–44.5) | −0.05§ (0.07) | 0.48 | 0.12 | 39.8 (34.5–45.0) |
| Ideal | 38.9 (36.0–42.4) | 28.2 (25.1–31.3) | −0.75 (0.07) | <0.01 | 0.96 | 16.8 (11.7–21.8) |
| Glucose/diabetes mellitus | ||||||
| Poor | 5.5 (4.1–7.0) | 11.1 (8.0–14.3) | 0.27‡ (0.08) | 0.03 | 0.65 | 13.6 (4.9–22.3) |
| Intermediate | 26.6 (23.2–29.6) | 50.5 (45.1–55.9) | 1.33 (0.28) | <0.01 | 0.85 | 63.1 (37.8–88.3) |
| Ideal | 67.9 (64.8–71.2) | 38.4 (32.7–44.0) | −1.60 (0.34) | <0.01 | 0.85 | 23.3 (0–53.7) |
| Cholesterol | ||||||
| Poor | 18.6 (15.9–20.8) | 13.8 (10.8–16.8) | −0.30 (0.05) | <0.01 | 0.88 | 10.0 (5.7–14.3) |
| Intermediate | 34.9 (31.9–37.5) | 39.6 (34.3–44.8) | 0.31 (0.08) | 0.02 | 0.80 | 43.5 (37.3–49.7) |
| Ideal | 46.5 (43.8–50.0) | 46.6 (41.6–51.7) | −0.01§ (0.12) | 0.92 | 0.01 | 46.5 (37.0–55.8) |
| Blood pressure | ||||||
| Poor | 21.0 (18.3–23.5) | 15.7 (12.8–18.5) | −0.35 (0.03) | <0.01 | 0.96 | 11.2 (8.3–14.2) |
| Intermediate | 46.0 (42.6–49.0) | 48.6 (44.2–53.0) | 0.11§ (0.11) | 0.40 | 0.18 | 48.7 (39.8–57.7) |
| Ideal | 33.0 (30.6–35.9) | 35.7 (31.8–39.6) | 0.21§ (0.1.0) | 0.10 | 0.53 | 40.1 (29.6–50.4) |
CI indicates confidence interval; NHANES, National Health and Nutrition Examination Survey.
NHANES III data replaced with NHANES 1999–2000 data, given different methods used.
NHANES III and NHANES 2007–2008 data replaced with NHANES 1999–2000 and 2005–2006 data, respectively, given different methods used.
Coefficient of variation >0.3.
P>0.05 for the null hypothesis that β = 0; all others, P<0.05.
Table 3.
Prevalence Estimates (95% CI) and 2020 Projections of Poor, Intermediate, and Ideal Levels of Cardiovascular Health Components for US Women: NHANES (1988 –2008)
| NHANES III (1988 –1994) |
2007–2008 | β (SE) | P | R2 | 2020 Projection (95% CI) |
|
|---|---|---|---|---|---|---|
| Smoking | ||||||
| Poor | 25.3 (22.6–27.8) | 19.9 (16.0–23.8) | −0.33 (0.05) | <0.01 | 0.90 | 15.9 (11.6–20.6) |
| Intermediate | 1.2 (0.6–2.0) | 2.7 (1.4–4.0) | 0.11‡ (0.02) | <0.01 | 0.90 | 4.2 (2.3–6.3) |
| Ideal | 73.5 (70.6–76.2) | 77.4 (73.1–81.6) | 0.22 (0.05) | <0.01 | 0.85 | 79.9 (76.0–83.6) |
| Healthy diet* | ||||||
| Poor | 71.2 (66.4–75.9) | 70.7 (67.0–74.3) | 0.03§ (0.19) | 0.86 | 0.01 | 71.2 (58.8–83.6) |
| Intermediate | 27.8 (23.2–32.6) | 27.9 (24.5–31.3) | −0.08§ (0.17) | 0.67 | 0.07 | 26.9 (14.9–38.9) |
| Ideal | 0.90 (0.01–1.85) | 1.4 (0.4–0.4) | 0.04‡ (0.02) | 0.09 | 0.67 | 1.9 (0.8–2.8) |
| Physical activity† | ||||||
| Poor | 42.2 (37.1–47.4) | 31.7 (26.6–36.7) | −1.70§ (0.47) | 0.07 | 0.87 | 4.8 (0–41.0) |
| Intermediate | 20.4 (14.8–25.9) | 25.3 (21.3–29.4) | 0.76§ (0.41) | 0.21 | 0.64 | 40.2 (7.4–73.0) |
| Ideal | 37.4 (30.5–44.3) | 43.0 (38.1–47.8) | 0.77§ (0.26) | 0.09 | 0.82 | 55.0 (35.5–74.6) |
| Body weight | ||||||
| Poor | 25.2 (22.2–27.5) | 34.1 (29.6–38.6) | 0.63 (0.09) | <0.01 | 0.92 | 42.2 (33.3–51.0) |
| Intermediate | 25.8 (23.5–28.1) | 29.2 (25.0–38.6) | 0.15§ (0.10) | 0.22 | 0.34 | 29.9 (20.9–38.9) |
| Ideal | 49.0 (46.2–52.4) | 36.7 (32.5–40.9) | −0.78 (0.13) | <0.01 | 0.90 | 27.9 (15.5–40.3) |
| Glucose/diabetes mellitus | ||||||
| Poor | 4.6 (3.3–5.8) | 6.3 (3.8–8.8) | 0.10‡§ (0.05) | 0.11 | 0.50 | 8.3 (2.2–14.4) |
| Intermediate | 16.5 (14.0–18.8) | 36.6 (30.9–42.2) | 0.91 (0.24) | 0.02 | 0.78 | 44.3 (21.9–66.8) |
| Ideal | 78.9 (76.2–81.8) | 57.1 (51.2–63.1) | −1.07 (0.25) | 0.01 | 0.82 | 47.4 (24.2–70.5) |
| Cholesterol | ||||||
| Poor | 21.1 (18.6–23.5) | 14.9 (11.7–18.0) | −0.40 (0.06) | <0.01 | 0.92 | 10.0 (5.3–14.8) |
| Intermediate | 31.3 (28.1–34.0) | 39.0 (35.8–42.3) | 0.48 (0.08) | <0.01 | 0.90 | 44.5 (37.8–51.1) |
| Ideal | 46.1 (44.8–50.9) | 47.6 (42.2–50.0) | −0.08§ (0.08) | 0.36 | 0.21 | 45.5 (39.2–52.0) |
| Blood pressure | ||||||
| Poor | 16.9 (14.8–19.0) | 12.8 (10.3–15.4) | −0.21§ (0.14) | 0.22 | 0.34 | 11.7 (0–23.8) |
| Intermediate | 30.2 (27.5–32.6) | 35.9 (31.6–40.3) | 0.33 (0.06) | <0.01 | 0.85 | 39.4 (33.9–44.8) |
| Ideal | 52.9 (50.6–55.5) | 51.2 (47.3–55.2) | −0.18§ (0.12) | 0.20 | 0.36 | 48.9 (36.7–61.0) |
CI indicates confidence interval; NHANES, National Health and Nutrition Examination Survey.
NHANES III data replaced with NHANES 1999–2000 data, given different methods used.
NHANES III and NHANES 2007–2008 data replaced with NHANES 1999–2000 and 2005–2006 data, respectively, given different methods used.
Coefficient of variation >0.3.
P>0.05 for the null hypothesis that β = 0; all others, P<0.05.
Prevalence of current smoking, physical activity (1999–2006 only), high cholesterol, and high blood pressure (ie, poor levels of these metrics) all decreased from 1988 to 2008, although trends in physical activity and in high blood pressure in women were not statistically significant, whereas a corresponding increase in ideal smoking status (never smoker or quit >12 months) was observed. However, there was not a significant increase in the prevalence of individuals with ideal levels of physical activity, cholesterol, or blood pressure. Conversely, obesity and dysglycemia increased substantially in both sexes from 1988 to 2008. Furthermore, there was a minimal increase in healthy diet score in men and no change in women during the period of observation (1999–2008).
Projected prevalence trends to 2020 (95% CIs) for ideal, intermediate, and poor cardiovascular health metrics, with the assumption that current trends continue, are also presented in Tables 2 and 3. Current smoking decreased significantly from 1998 to 2008 in both men and women, with projected prevalence in 2020 reaching 23% in men and 16% in women. Prevalence of former smokers who had quit <12 months ago (intermediate cardiovascular health) increased in both groups as well and is projected to be 4.5% and 4.3% in men and women, respectively, in 2020. Among current smokers, the mean number of cigarettes per day was lower in both men and women and in all age groups (Figure II in the online-only Data Supplement).
The prevalence of ideal healthy diet score=4 or 5 increased minimally from 0.3% to 0.6% in men (P=0.04) and from 0.9% to 1.4% in women (P=0.02) between 1999 and 2008. The projected prevalence of ideal healthy diet score will reach only 1.2% in men and 1.9% in women by 2020. The mean healthy diet score was minimally increased between 1999 and 2008 in men (from 0.78 to 0.84 healthy diet components; P=0.04) and in women (from 1.04 to 1.10; P=0.33). The healthy diet scores were slightly higher for adults aged ≥60 years in both men and women from 2000 to 2006, but these differences were small and are projected to narrow further by 2020 (Figure III in the online-only Data Supplement).
Physical inactivity prevalence declined nonsignificantly from 1999 to 2006 in both men (from 37% to 30%; P=0.40) and women (from 42% to 32%; P=0.87). Corresponding increases in the prevalence of intermediate and ideal physical activity levels were also not statistically significant in either sex. Projections to 2020 appear unreliable given fewer time periods and the wide variance of this measure. The median number of minutes of activity per week was <150 minutes in all age and sex groups from 2000 to 2006 (Figure IV in the online-only Data Supplement).
Mean body mass index and obesity rates increased substantially from 20% in NHANES III to 32% by 2007–2008 in men and are projected to reach 43% by 2020 if current trends continue. Similar trends were observed in women, in whom 2020 prevalence projections of obesity reach 42%. There was a corresponding rise in mean body mass index and decrease in the prevalence of ideal body mass index <25 kg/m2 (Figure V in the online-only Data Supplement).
Trends in dysglycemia prevalence rates were similar. Diabetes mellitus prevalence and impaired fasting glucose increased in both men and women. The 2020 projected prevalence of diabetes mellitus is 14% in men and 8% in women, and <50% of women and <25% of men will have ideal fasting plasma glucose levels (<100 mg/dL). Among individuals with diabetes mellitus, hemoglobin A1c values are projected to decrease (from 7.5% to 7.2% from 2008 to 2020) in men but remain stable in women (Figure VI in the online-only Data Supplement). Among individuals without diabetes mellitus, the mean fasting plasma glucose increased to 104 mg/dL in men and 99 mg/dL in women in 2008, with 2020 projections reaching 108 mg/dL and 101 mg/dL, respectively, if current trends continue (Figure VII in the online-only Data Supplement).
The mean total cholesterol fell from 204 to 196 mg/dL in men and 206 to 199 mg/dL in women from 1998 to 2008. By 2020, mean total cholesterol is projected to decrease in both men (to 191 mg/dL) and women (to 194 mg/dL) (Figure VIII in the online-only Data Supplement). The corresponding prevalence of high cholesterol (≥240 mg/dL) decreased from 19% to 14% in men (P<0.01) and from 21% to 15% in women (P<0.01) from 1988 to 2008. However, the prevalence of individuals with intermediate cholesterol increased significantly. This group includes individuals with untreated levels of 200 to 239 mg/dL and those with total cholesterol <200 mg/dL on medical therapy (Figures IX and X in the online-only Data Supplement).
The prevalence of high blood pressure decreased from 21% to 16% in men (P<0.01) and from 17% to 13% in women (P=0.22), with a significant increase in the prevalence of intermediate levels of untreated blood pressure (120 – 139 mm Hg systolic or 80–89 mm Hg diastolic) or blood pressure treated to <140/<90 mm Hg in women but not men. Mean systolic blood pressure is projected to be 119 mm Hg in men and women by 2020. Older adults (≥60 years) had declines in mean systolic blood pressure, whereas middle-aged adults (40–59 years) and younger adults (20–39 years) did not (Figure XI in the online-only Data Supplement). Decreases in mean systolic blood pressure over time were most pronounced among groups using blood pressure-lowering agents, in whom systolic blood pressure was lower across all ages during all cycles (Figures XII and XIII in the online-only Data Supplement).
Projections in Cardiovascular Health: Will a 20% Improvement Be Achieved by 2020?
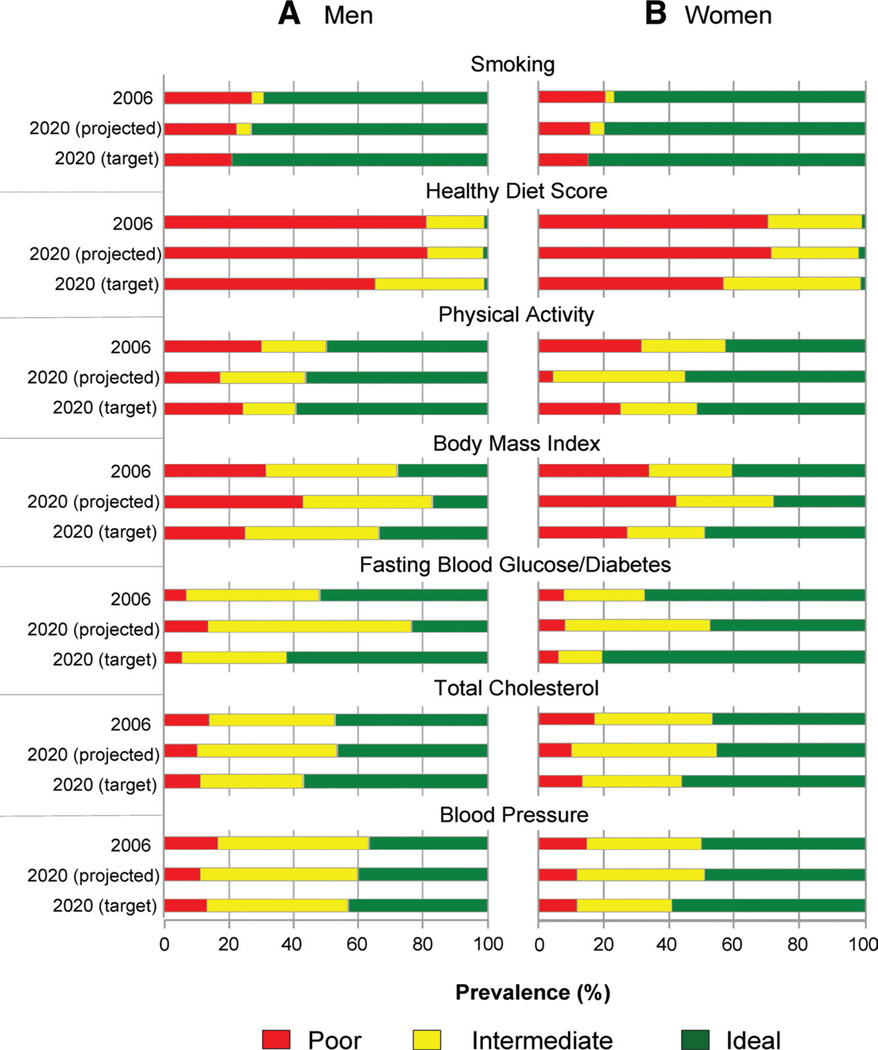
Figure 1 shows the prevalence of ideal (green), intermediate (yellow), and poor (red) cardiovascular health metrics in 2006 (AHA 2020 Impact Goals baseline year) and 2020 projections with the assumption that current trends continue. Additionally, Figure 1 provides 2020 targets for each cardiovascular health metric, with the assumption of a 20% relative increase in ideal cardiovascular health prevalence metrics and a 20% relative decrease in poor cardiovascular health prevalence metrics for men and women.
Figure 1.
Prevalence of ideal (green), intermediate (yellow), and poor (red) cardiovascular health metrics in 2006 (AHA 2020 Impact Goals baseline year) and 2020 projections with the assumption that current trends continue. 2020 targets for each cardiovascular health metric are shown, with the assumption of a 20% relative increase in ideal cardiovascular health prevalence metrics and a 20% relative decrease in poor cardiovascular health prevalence metrics for men and women. A, men; B, women.
Projected decreases in the prevalence of poor cardiovascular health will meet the 20% improvement if current trends continue for smoking, physical activity, blood pressure, and cholesterol. However, fewer and more modest increases in the prevalence of ideal cardiovascular health metrics are projected for smoking, diet, and physical activity. Overall, we estimate a 6.04% relative improvement in the prevalence of overall cardiovascular health on the basis of current trends using the methods outlined by the AHA. This would be well short of the AHA target.
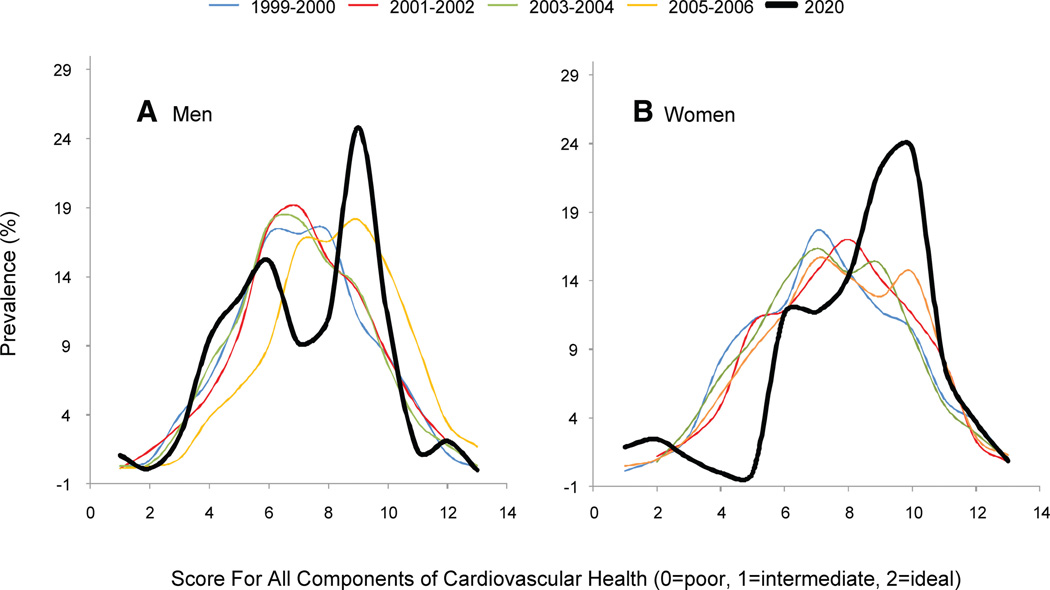
Cardiovascular Health Score
Figure 2 shows the distributions of the individual-based Cardiovascular Health Score over 5 NHANES cycles from 1999 to 2006. The highest overall mean score occurred during the 2005–2006 cycle (yellow curves). Furthermore, from 1999 to 2006, mean Cardiovascular Health Scores did not change significantly for men (from 7.9 to 7.8 points; P=0.48) or women (from 8.2 to 8.4 points; P=0.46). If these current trends continue to 2020, the mean scores are projected to be 7.4 (95% CI, 5.7–9.1) for men and 8.8 (95% CI, 7.6 –9.9) for women. These estimates are substantially lower than the target scores necessary to achieve a 20% relative improvement in individual-level cardiovascular health (9.4 for men; 10.1 for women).
Figure 2.
Distributions of the individual-based Cardiovascular Health Score over 5 National Health and Nutrition Examination Survey cycles from 1999 to 2006. A, men; B, women.
Discussion
Summary of Results
From 1988 to 2008, significant declines in the prevalence of smoking, high cholesterol, and high blood pressure (in men) have been offset by substantial increases in the prevalence of obesity and dysglycemia. Healthy diet scores have changed minimally, and physical inactivity has trended lower, albeit not significantly. The declines in high cholesterol and high blood pressure are not matched with a concomitant increase in the prevalence of ideal cholesterol and blood pressure levels, suggesting that individuals are moving toward intermediate levels of each health factor, a stratum that includes individuals treated to cholesterol and/or blood pressure target.
Worrying increases in body mass index and dysglycemia are matched by a concomitant decrease in the prevalence of normal-weight and euglycemic adults, consistently suggesting adverse population-level shifts in each metric. Our projections may overestimate the future prevalence of impaired fasting glucose (intermediate cardiovascular health) because some individuals will likely develop diabetes mellitus by crossing the 126 mg/dL fasting plasma glucose threshold and will not contribute to these projected mean values.
Implications
Our estimated 6% relative improvement in cardiovascular health from 2006 to 2020 is far short of the AHA’s 2020 Impact Goals’ target of improving cardiovascular health by 20%. Furthermore, we project no changes in the mean individual Cardiovascular Health Score for both men and women. In addition to worsening cardiovascular health metrics, current trends will likely lead to stagnating age-adjusted fatal and nonfatal CVD event rates in the context of rising healthcare costs on the basis of unfavorable coronary heart disease mortality trends among Americans aged 35 to 54 years.12 The AHA has recently estimated that between 2010 and 2030, direct costs for CVD (including hypertension, coronary heart disease, heart failure, stroke, and all other CVD) will increase from $273 billion to $818 billion, and indirect costs will rise from $172 billion to $276 billion, unless substantial changes to prevent and control CVD are adopted.13
The optimal combination of primordial,14 primary, and secondary prevention approaches—realized through a mixture of medical and public health/policy interventions—will be critical for any high-functioning health system to reduce the prevalence of poor cardiovascular health metrics. The goals of this approach are to (1) provide high-quality, equitable management of individuals with risk factors and disease and (2) shift individuals from intermediate to ideal levels or, optimally, to maintain ideal health cardiovascular metrics throughout the lifespan. This has been shown to lead to greater longevity and health,15 compression of morbidity,16 dramatically low lifetime risks for CVD (which account for competing risks),17 and remarkably lower healthcare utilization and costs (annual, lifetime, and last year of life).18 Given these compelling findings, the improvement in cardiovascular health through quantifiable metrics has received increasing attention, including being part of Healthy People 2020 as a named objective.19
Potential Targets for Intervention
These results reinforce the central importance of comprehensive tobacco control policies as well as the prevention and management of obesity through diet, exercise, and judicious use of therapies for weight loss to improve cardiovascular health in adults. Although declines in tobacco consumption are encouraging, tobacco remains the leading cause of preventable death and disability, including a substantial burden of non-CVD such as lung cancer and chronic lung disease. The downstream impact of obesity on other cardiovascular health metrics such as dysglycemia, blood pressure, and possibly cholesterol suggests that reversal of body weight trends will have substantial benefits across the spectrum of cardiovascular health.
The World Health Organization has also prioritized tobacco control and healthier diet policies, suggesting several population-level “best buy” policy options for noncommunicable, chronic disease prevention that are relevant to cardiovascular health in the United States and the AHA’s 2020 Impact Goals. These include the following: (1) public smoking bans, (2) tobacco advertising restrictions, (3) increased tobacco excise taxes (especially relevant at the state level given the wide variation across the United States20), (4) reduced salt in the food supply, (5) replacement of trans fats with polyunsaturated fats, and (6) mass media campaigns to promote healthy diets and physical activity.21 In concert with policy changes, more rigorous improvements in individual lifestyle behaviors and factors and medical treatment and control (including combination therapy for high-risk individuals) are needed to help shift individuals from poor to intermediate to ideal cardiovascular health.19
Strengths/Limitations
The strengths of our results include its large, nationally representative sample size and 20-year measurement period. However, our study has limitations. First, measures of diet and physical activity are prone to sampling variability, as noted by the wide CIs for these estimates, and misclassification due to self-reporting. In addition, we relied on fewer NHANES cycles for trend tests and 2020 projections for diet and physical activity. Our estimates for diet and physical activity may be unstable and should be interpreted cautiously. Second, future trends may not be linear, as we have assumed. For example, recent obesity increases may be plateauing; conversely, recent cholesterol and blood pressure declines may also be plateauing, which may contribute to the flattening coronary heart disease mortality rates in young men and women in the United States, United Kingdom, and elsewhere.12,22 Finally, we created a simple composite Cardiovascular Health Score to examine individual-level cardiovascular health. This score weighs the presence of all intermediate or poor levels of the 7 metrics equally. Prior studies indicate that some adverse health factors, such as current smoking or diabetes mellitus, may be associated with greater relative risks for cardiovascular events than other factors. However, the present score is not intended as a measure to estimate risk; rather, it serves as a means for monitoring the distribution (poor, intermediate, or ideal) of all 7 metrics at the individual level across the population. Furthermore, Folsom et al2 recently demonstrated that there were roughly equal stepwise decreases in hazards for cardiovascular events for each additional single health behavior or health factor present at ideal levels.
Conclusions
If current trends continue, overall cardiovascular health is projected to improve by only 6% from 2006 to 2020, far below the AHA 2020 Strategic Impact Goals target of 20%. This projection reflects modest, further declines in tobacco consumption, high cholesterol, and high blood pressure, offset by increases in obesity and dysglycemia. Continued individual-level primary and secondary preventive measures should be complemented by an increased national commitment to promote primordial prevention. The potential reductions in CVD burden if the AHA 2020 Strategic Impact Goals target of 20% improvement in overall cardiovascular health were achieved could be substantial, rapid, and associated with substantial cost savings.23–26
Supplementary Material
CLINICAL PERSPECTIVE.
The American Heart Association’s Strategic Planning Task Force set forth the goal of improving the cardiovascular health of all Americans by 20% by 2020. To assess progress toward this goal, 7 health metrics were defined: smoking, diet, physical activity, body weight, blood glucose, blood pressure, and cholesterol. In this investigation, we asked, “If current trends in these metrics continue, will this goal be reached?” We evaluated past trends by using data from the 1998–2008 National Health and Nutrition Examination Survey (NHANES) examination cycles and created best-fit linear regression models and linear forward projections to 2020. We also created an individual-level Cardiovascular Health Score to evaluate individual-level changes in cardiovascular health amid larger population trends. Our results suggest that if current trends continue, changes in the individual-level Cardiovascular Health Score will be minimal and that the overall cardiovascular health of the US population will improve by only 6% by 2020; this progress is far short of the American Heart Association’s target of 20% improvement. This projection reflects modest further declines in tobacco use and improved control of high cholesterol and high blood pressure that are offset by increases in obesity and dysglycemia prevalence. In conclusion, continued individual-level primary and secondary preventive measures should be complemented by an increased national commitment to policies promoting prevention of the development of abnormal risk factor levels from childhood onward. If the American Heart Association target of 20% improvement in overall cardiovascular health were achieved, the potential reductions in cardiovascular disease burden could be substantial, rapid, and associated with substantial cost savings.
Acknowledgments
Sources of Funding
Drs Huffman and Shay were supported by a National Heart, Lung, and Blood Institiute–sponsored cardiovascular epidemiology and prevention training grant during part of this work (5 T32 HL069771-08). All data used in this study were collected by the National Center for Health Statistics, Centers for Disease Control and Prevention. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
The online-only Data Supplement is available with this article at http://circ.ahajournals.org/lookup/suppl/doi:10.1161/CIRCULATIONAHA.111.070722/-/DC1.
Disclosures
None.
References
- 1.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s Strategic Impact Goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 2.Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57:1690–1696. doi: 10.1016/j.jacc.2010.11.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bambs C, Kip KE, Dinga A, Mulukutla SR, Aiyer AN, Reis SE. Low prevalence of “ideal cardiovascular health” in a community-based population: the Heart Strategies Concentrating On Risk Evaluation (Heart SCORE Study) Circulation. 2011;123:850–857. doi: 10.1161/CIRCULATIONAHA.110.980151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.CDC/NCHS. Early release of selected estimates based on data from the 2010 National Health Interview Survey. [Accessed June 24, 2011]; http://www.cdc.gov/nchs/nhis/released201106.htm#6.
- 5.Chen CI, Burton T, Baker CL, Mastey V, Mannino D. Recent trends in exposure to secondhand smoke in the United States population. BMC Public Health. 2010;10:359. doi: 10.1186/1471-2458-10-359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dietary Guidelines for Americans, 2010. 7th ed. Washington, DC: US Government Printing Office; 2010. US Department of Agriculture and US Department of Health and Human Services. [Google Scholar]
- 7.Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303:235–241. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 8.Cohen JD, Cziraky MJ, Cai Q, Wallace A, Wasser T, Crouse JR, Jacobson TA. 30-year trends in serum lipids among United States adults: results from the National Health and Nutrition Examination Survey II, III, and 1999–2006. Am J Cardiol. 2010;106:969–975. doi: 10.1016/j.amjcard.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 9.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 10.CDC/NCHS. National Health and Nutrition Examination Survey. [Accessed June 28, 2011]; http://www.cdc.gov/nchs/nhanes.htm.
- 11.Analytic and Reporting Guidelines: The National Health and Nutrition Examination Survey (NHANES) Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 12.Ford ES, Capewell S. Coronary heart disease mortality among young adults in the US from 1980 through 2002: concealed leveling of mortality rates. J Am Coll Cardiol. 2007;50:2128–2132. doi: 10.1016/j.jacc.2007.05.056. [DOI] [PubMed] [Google Scholar]
- 13.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, Finkelstein EA, Hong Y, Johnston SC, Khera A, Lloyd-Jones DM, Nelson SA, Nichol G, Orenstein D, Wilson PW, Woo YJ. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 14.Strasser T. Reflections on cardiovascular diseases. Interdisciplinary Sci Rev. 1978;3:225–230. [Google Scholar]
- 15.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, Dyer AR, Liu K, Greenland P. Low risk-factor profile and long-term cardiovascular and noncardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA. 1999;282:2012–2018. doi: 10.1001/jama.282.21.2012. [DOI] [PubMed] [Google Scholar]
- 16.Daviglus ML, Liu K, Pirzada A, Yan LL, Garside DB, Feinglass J, Guralnik JM, Greenland P, Stamler J. Favorable cardiovascular risk profile in middle age and health-related quality of life in older age. Arch Intern Med. 2003;163:2460–2468. doi: 10.1001/archinte.163.20.2460. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd-Jones DM, Leip EP, Larson MG, D’Agostino RB, Beiser A, Wilson PW, Wolf PA, Levy D. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113:791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 18.Daviglus ML, Liu K, Greenland P, Dyer AR, Garside DB, Manheim L, Lowe LP, Rodin M, Lubitz J, Stamler J. Benefit of a favorable cardiovascular risk-factor profile in middle age with respect to Medicare costs. N Engl J Med. 1998;339:1122–1129. doi: 10.1056/NEJM199810153391606. [DOI] [PubMed] [Google Scholar]
- 19.Healthy People 2020 objectives. [Accessed June 24, 2011]; http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=21.
- 20.Schroeder SA, Warner KE. Don’t forget tobacco. N Engl J Med. 2010;363:201–204. doi: 10.1056/NEJMp1003883. [DOI] [PubMed] [Google Scholar]
- 21.Global Status Report on Non-Communicable Diseases. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 22.O’Flaherty M, Bishop J, Redpath A, McLaughlin T, Murphy D, Chalmers J, Capewell S. Coronary heart disease mortality among young adults in Scotland in relation to social inequalities: time trend study. BMJ. 2009;339:b2613. doi: 10.1136/bmj.b2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Institute for Health and Clinical Excellence. Prevention of cardiovascular disease at population level, 2010. [Accessed June 23, 2011]; http://guidance.nice.org.uk/ph25. [Google Scholar]
- 24.Barton P, Andronis L, Briggs A, McPherson K, Capewell S. Effectiveness and cost effectiveness of cardiovascular disease prevention in whole populations: modelling study. BMJ. 2011;343:d4044. doi: 10.1136/bmj.d4044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Capewell S, Ford ES, Croft JB, Critchley JA, Greenlund KJ, Labarthe DR. Cardiovascular risk factor trends and potential for reducing coronary heart disease mortality in the United States of America. Bull World Health Organ. 2010;88:120–130. doi: 10.2471/BLT.08.057885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Capewell S, O’Flaherty M. Rapid mortality falls after risk-factor changes in populations. Lancet. 2011;378:752–753. doi: 10.1016/S0140-6736(10)62302-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.