Abstract
Colonoscopy is the preferred modality for colon cancer screening. A successful colonoscopy requires proper bowel preparation. Adequate bowel preparation continues to remain a limiting factor. One hundred thirty-three patients scheduled for an outpatient colonoscopy were prospectively randomized in a single-blinded manner to video or nonvideo group. In addition to written bowel preparation instructions, patients in the video group viewed a brief instructional video. Quality of colon preparation was measured using the Ottawa Bowel Preparation Quality scale, while patient satisfaction with preparation was evaluated using a questionnaire. Statistical analyses were used to evaluate the impact of the instructional colonoscopy video. There were significant differences in the quality of colonoscopy preparation between the video and the nonvideo groups. Participants who watched the video had better preparation scores in the right colon (P=0.0029), mid-colon (P=0.0027), rectosigmoid (P=0.0008), fluid content (P=0.03) and aggregate score (median score 4 versus 5; P=0.0002). There was no difference between the two groups with regard to patient satisfaction. Income, education level, sex, age and family history of colon cancer had no impact on quality of colonoscopy preparation or patient satisfaction. The addition of an instructional bowel preparation video significantly improved the quality of colon preparation.
Keywords: Bowel preparation, Colon, Colonoscopy, Colon cancer screening, Videos
Abstract
La coloscopie est la modalité favorisée pour dépister le cancer du côlon. Pour réussir une coloscopie, il faut bien préparer l’intestin, ce qui continue de demeurer un facteur contraignant. Cent trente-trois patients qui devaient subir une coloscopie ambulatoire ont été répartis au hasard à simple insu sur une base prospective entre un groupe qui visionnait une vidéo et un groupe qui ne la visionnait pas. En plus de directives écrites sur la préparation intestinale, les patients du premier groupe ont vu une courte vidéo de directives. Les chercheurs ont mesuré la qualité de la préparation du côlon au moyen de l’échelle de qualité de la préparation intestinale d’Ottawa et ont évalué la satisfaction des patients à l’aide d’un questionnaire. Ils ont recouru à des analyses statistiques pour évaluer les effets de la vidéo de directives sur la coloscopie. Ils ont remarqué des différences significatives de la qualité de la préparation à la coloscopie entre le groupe ayant vu la vidéo et le groupe ne l’ayant pas vue. Les participants du premier groupe présentaient de meilleurs indices de préparation du côlon droit (P=0,0029), du milieu du côlon (P=0,0027), du rectosigmoïde (P=0,0008), du contenu liquidien (P=0,03) et un meilleur indice global (indice médian de 4 par rapport à 5; P=0,0002). Les chercheurs n’ont constaté aucune différence entre les deux groupes en matière de satisfaction des patients. Le revenu, le niveau d’instruction, le sexe, l’âge et les antécédents familiaux de cancer du côlon n’avaient pas d’effet sur la qualité de la préparation à la coloscopie ou sur la satisfaction des patients. L’ajout d’une vidéo de directives sur la préparation intestinale améliorait la qualité de la préparation du côlon de manière significative.
Colonoscopy is the preferred modality for colon cancer screening. A successful colonoscopy requires proper preprocedure bowel preparation to ensure complete visualization of the colonic mucosa. Despite improvements in bowel purgatives, inadequate bowel cleansing remains a significant barrier to a successful colonoscopy (1) because 10% to 20% of all colonoscopies in the United States (US) fail due to suboptimal preparation (1–5). Furthermore, inadequate bowel preparation not only increases procedural duration and the need for repeat colonoscopies (4,6–8), but a 45% reduction in polyp detection rates were observed in colonoscopies with suboptimal bowel preparation (7,8). Ultimately, the economic impact of inadequate bowel preparation is significant, with incomplete procedures resulting in 12% to 22% higher estimated costs (1,6–9). Therefore, studies examining factors that affect bowel preparation are needed to improve procedural outcomes while reducing the need for repeat colonoscopies and its economic burden.
A landmark study by Ness et al (10) provided a list of factors that lead to poor bowel preparation. Poor bowel preparation has been attributed to factors such as inpatient status, chronic constipation, tricyclic antidepressants, male sex and later colonoscopy starting time. More recent studies have demonstrated that low socioeconomic status (11), increased body mass index and abdominal girth (12), and opioid dependence (13) are additional factors that affect the quality of bowel preparation. Furthermore, noncompliance with bowel preparation due to poor comprehension of the complex bowel preparation instructions may also contribute to inadequate bowel preparation (1,6). However, studies focusing on patient education to improve the quality and adequacy of colonoscopy preparation have been inconsistent and with varying results (1–3,7,14–16).
The aim of the present study was to evaluate the impact of a brief informational colonoscopy video on the quality of colonic bowel preparation and patient satisfaction with the colonoscopy procedure. A brief bowel preparation video containing pictorial demonstrations, subtitles and simplified instructions was created. The video emphasized the importance of adhering to the instructions for proper bowel preparation. The video was shown to patients before undergoing a colonoscopy. The primary end point was to compare the quality of bowel preparation between patients who watched the video and those who did not watch the video.
Therefore, we designed colonoscopy bowel preparation instructions in a simplified script with pictures and subtitles, with an emphasis on the importance of adhering to the instructions for proper bowel preparation. We then filmed a 5 min bowel preparation video explaining the colonoscopy preparation instructions using the SUPREP Bowel Prep Kit (sodium sulfate, potassium sulfate, and magnesium sulfate oral solution, Braintree Laboratories, USA). The aim of our study was to evaluate the impact of a brief informational colonoscopy video on the quality of colonic bowel preparation and patient satisfaction.
METHODS
The present study was a single-blinded, randomized, multicentre prospective trial evaluating the impact of a supplementary bowel preparation instructional video on the quality of colonoscopy preparation and patient satisfaction. The study protocol and informed consent were approved by the Institutional Review Board at Southern Regional Medical Center, Riverdale, Georgia (USA). The study was conducted from June 6, 2011 to June 6, 2012, with participants enrolled at two outpatient endoscopy centres (GI Endoscopy Center and Locust Grove Endoscopy Center, both in Georgia).
Study population
Study patients included men and women >18 years of age whose primary language was English, had computer access and were willing to provide informed consent to participate in the study. Patients could have any indication for the procedure except for inflammatory bowel disease. All enrolled patients were scheduled for a morning session (before 13:00) outpatient colonoscopy. The SUPREP kit was the standard bowel preparation in the study. Patients with any previous colon surgery, inflammatory bowel disease, gastric surgery, gout, renal impairment, seizures and cardiac arrhythmias that were contraindications to the bowel preparation were excluded.
Study design
After scheduling for outpatient colonoscopy, the performing physician or a member of the research team inquired whether the patient was interested in volunteering to participate in the study. The consent form was then reviewed in detail with the patient and questions were answered by a member of the research team. Patients who provided consent and met all eligibility criteria were randomly assigned to a group (video or novideo group). A single-blinded randomization was performed via sealed and numbered envelopes. Envelopes were distributed to the patients in numerical order based on when they consented and were deemed eligible for the study. The performing physician, members of the research team and nurses were blinded to the allocation. All envelopes contained the instructional brochure in the appropriate primary language, English. The sealed envelopes also included a study ticket assigning them to the appropriate group (video or nonvideo). In addition, patients assigned to the video group had additional instructions including the Internet website to view the colonoscopy preparation instructional video. The bowel preparation video was uploaded to a website that allows the posting of videos for public viewing. Password protection was used to limit access to the bowel preparation instructional video, with the password provided to only patients included in the video group. The video included instructions with pictures and subtitles to supplement the standard written instructions for the preparation process. It also included a photograph of optimal and poor preparation for patients to visually understand the clinical significance of bowel preparation. All participants were required to complete the standard split-dose bowel preparation regimen with SUPREP Bowel Prep Kit 5 h before the scheduled procedure. On the morning of the procedure before undergoing a colonoscopy, all patients received a five-page multiple-choice questionnaire. The form included questions evaluating satisfaction with the preparation process, adverse reactions, educational level, income level, demographic information (age, race/ethnicity, sex), previous colonoscopies and family history of colon cancer. Furthermore, the questionnaire confirmed that patients viewed the video and completed the preparation process.
Patients then underwent a colonoscopy with one of five American Board of Internal Medicine-certified gastroenterologists with experience performing >2000 procedures. The performing physicians and nursing staff were blinded to the group the patient was assigned to. Finally, the gastroenterologist completed a procedure assessment form immediately after the colonoscopy to evaluate the bowel preparation. The quality of bowel preparation was evaluated using the Ottawa Bowel Preparation Quality Scale (Ottawa scale) (17), a validated bowel preparation scale. The Ottawa scale is an instrument requiring the endoscopist to rate cleansing in three segments (right colon, mid colon and rectosigmoid colon) on a scale of 0 to 4, with 0 indicating perfect cleansing, and overall fluid quantity on a scale of 0 to 2, with 0 indicating no fluid in the colon (17). The individual scores were then summed to create a total aggregate score, with lower scores indicating better preparation (17). To maintain precision in evaluating colon preparation and reduce interobserver variability, all performing gastroenterologists completed an Ottawa scale workshop before study enrollment. During the workshop, the Ottawa scale was reviewed with education provided to the gastroenterologists assisting with the study. The workshop also included a series of colon photographs with a short quiz and discussion among the group of gastroenterologists to ensure uniformity and precision in the score.
End points
The primary end point of the study was to evaluate the quality of bowel preparation using the Ottawa bowel preparation scale. Secondary end points assessed included patient satisfaction, demographic information (race/ethnicity, sex, age), educational level, income, family history of colon cancer and previous colonoscopy.
Statistical analysis
Patient characteristics, individual components of the Ottawa scale, and patient satisfaction between the video and nonvideo groups were compared using the χ2 test or Fisher’s exact test. Fisher’s exact test was used when the variables being compared had exactly two categories or when there were small expected cell counts. The Mann-Whitney U test was used to compare the overall score calculated for the Ottawa scale between the two groups. The Spearman’s rank order correlation procedure was used to determine whether there was a correlation between various variables. SAS version 9.3 (SAS Institute, USA) was used for all analyses. Two-tailed tests were used and P<0.05 was considered to be statistically significant.
RESULTS
A total of 147 patients were initially enrolled in the study. Fourteen patients were excluded due to not completing the patient questionnaire or incomplete Ottawa scale, resulting in 133 patients being included in the analyses. Of the 133 patients included in the analyses, 67 were in the video group and 66 were in the nonvideo group. Of the 67 who were assigned to the video group, 79% were satisfied with the video on a scale of 1 to 5, with 1 representing unsatisfied and 5 representing satisfied. Thirty-two (47.76%) patients viewed the video only once, twenty-six (38.81%) watched it twice, six (8.96%) watched it three times and three (4.48%) watched it more than three times. Ninety-five per cent reported they would recommend the video to another person scheduled for a colonoscopy and 64% reported they learned additional information from the video.
Patient characteristics were compared between the video and nonvideo groups in Table 1. There was no significant difference in race or having a family member diagnosed with colorectal cancer before 60 years of age. There were statistically significant differences between the two groups in age (P=0.022), income level (P=0.0021) and level of formal education (P=0.0035). There were no differences between the two groups with respect to sex (P=0.081), race (P=0.33), or history of previous colonoscopies (P=0.061). However, 61% of the video group had not undergone any previous colonoscopies compared with 44% in the nonvideo group. There were more patients in the nonvideo group who had undergone two, three or more than three colonoscopies than in the video group. Of the total cohort of patients, only three patients (one in the video group and two in the nonvideo group) reported being given the SUPREP kit for a previous colonoscopy. Of those who had undergone a previous colonoscopy, there was a nonsignificant trend when assessing whether the previous experiences with colonoscopies were more satisfying (P=0.081). Only three (11.54%) patients in the video group and 10 (27.03%) in the nonvideo group reported that their previous colonoscopies were more satisfying. Fifteen (57.69%) patients in the video group and 23 (62.16%) in the nonvideo group reported that their previous experiences were not more satisfying. Eight (30.77%) patients in the video group and four (10.81%) in the nonvideo group reported that this question was not applicable.
TABLE 1.
Patient characteristics
| Characteristics | Video group (n=67) | Nonvideo group (n=66) | P* |
|---|---|---|---|
| Sex | 0.081 | ||
| Male | 35 (52.24) | 24 (36.36) | |
| Female | 32 (47.76) | 42 (63.64) | |
| Age, years | 0.022 | ||
| <22 | 2 (2.99) | 1 (1.52) | |
| 22–42 | 8 (11.94) | 11 (16.67) | |
| 43–63 | 52 (77.61) | 38 (57.58) | |
| 64–84 | 5 (7.46) | 16 (24.24) | |
| >84 | 0 (0.00) | 0 (0.00) | |
| Race | 0.33 | ||
| Asian | 2 (2.99) | 2 (3.03) | |
| African American | 29 (43.28) | 36 (54.55) | |
| Hispanic | 0 (0.00) | 2 (3.03) | |
| Native American | 0 (0.00) | 0 (0.00) | |
| Caucasian | 35 (52.24) | 25 (37.88) | |
| Other | 1 (1.49) | 1 (1.52) | |
| Annual income level, $ | 0.0021 | ||
| <25,000 | 6 (8.96) | 24 (36.36) | |
| 25,000–75,000 | 35 (52.24) | 26 (39.39) | |
| >75,000–100,000 | 16 (23.88) | 11 (16.67) | |
| >100,000 | 10 (14.93) | 5 (7.58) | |
| Education level | 0.0035 | ||
| <High school | 1 (1.49) | 12 (18.18) | |
| High school | 23 (34.33) | 28 (42.42) | |
| College | 35 (52.24) | 18 (27.27) | |
| Graduate | 7 (10.45) | 6 (9.09) | |
| Postgraduate | 1 (1.49) | 2 (3.03) | |
| Previous colonoscopies, n | 0.061 | ||
| 0 | 41 (61.19) | 29 (43.94) | |
| 1 | 20 (29.85) | 18 (27.27) | |
| 2 | 3 (4.48) | 10 (15.15) | |
| 3 | 1 (1.49) | 4 (6.06) | |
| >3 | 2 (2.99) | 5 (7.58) | |
| Family member diagnosed with colorectal cancer before | 0.48 | ||
| 60 years of age | |||
| Yes | 9 (13.43) | 12 (18.18) | |
| No | 58 (86.57) | 54 (81.82) | |
Data presented as n (%) unless otherwise indicated.
χ2 test used for income and education level, Fisher’s exact test used for all other variables
There was a statistically significant difference between the two groups with regard to quality of colonoscopy preparation (Table 2 and Figures 1A to 1D). Using the individual components of the Ottawa scale, the video group had better ratings for cleanliness for the right colon, mid colon and rectosigmoid, and also fluid content. There was a statistically significant difference in the total composite score between the two groups (P=0.0002). The median score for the video group was 4, and the median score for the nonvideo group was 5.
TABLE 2.
Ottawa Bowel Preparation Quality Scale
| Segment (score) | Video group (n=67) | Nonvideo group (n=66) | P* |
|---|---|---|---|
| Right colon† | 0.0029 | ||
| Excellent (0) | 27 (40.30) | 13 (19.70) | |
| Good (1) | 31 (46.27) | 29 (43.94) | |
| Fair (2) | 8 (11.94) | 14 (21.21) | |
| Poor (3) | 1 (1.49) | 3 (4.55) | |
| Inadequate (4) | 0 (0.00) | 7 (10.61) | |
| Mid colon† | 0.0027 | ||
| Excellent (0) | 29 (43.28) | 12 (18.18) | |
| Good (1) | 26 (38.81) | 31 (46.97) | |
| Fair (2) | 11 (16.42) | 14 (21.21) | |
| Poor (3) | 1 (1.49) | 3 (4.55) | |
| Inadequate (4) | 0 (0.00) | 6 (9.09) | |
| Rectosigmoid† | 0.0008 | ||
| Excellent (0) | 24 (35.82) | 8 (12.12) | |
| Good (1) | 33 (49.25) | 37 (56.06) | |
| Fair (2) | 10 (14.93) | 12 (18.18) | |
| Poor (3) | 0 (0.00) | 4 (6.06) | |
| Inadequate (4) | 0 (0.00) | 5 (7.58) | |
| Fluid† | 0.030 | ||
| Small (0) | 17 (25.37) | 9 (13.64) | |
| Moderate (1) | 39 (58.21) | 34 (51.52) | |
| Large (2) | 11 (16.42) | 23 (34.85) | |
| Total score‡ | 0.0002 | ||
| Median (IQR) | 4.00 (1–4) | 5.00 (3–7) |
Fisher’s exact test used for right colon, mid colon and rectosigmoid components due to small expected cell counts, χ2 test used for fluid content, Mann-Whitney U test used for total score;
Data presented as n (%) for right colon, mid colon, rectosigmoid and fluid components, and median and interquartile range (IQR) reported for total score;
Total score = composite of right colon, mid colon, rectosigmoid and fluid: lower scores = better, higher scores = worse)
Figure 1).
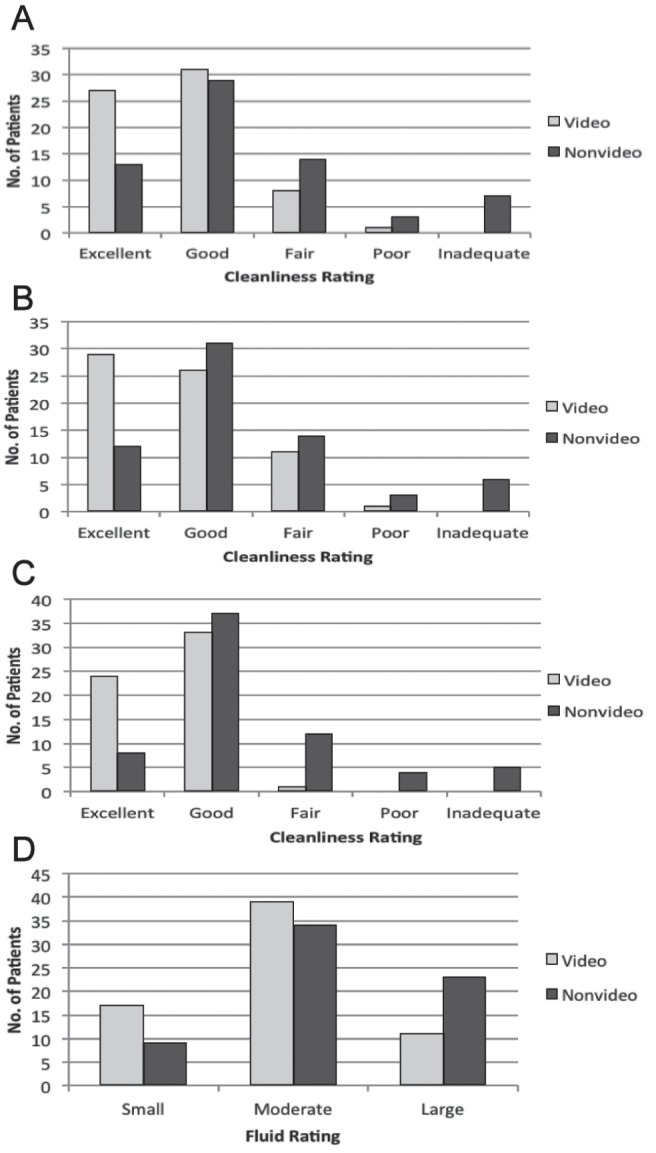
Ottawa Bowel Preparation Scale. A Right colon assessment according to group. B Mid colon assessment according to group. C Recto-sigmoid assessment according to group. D Fluid assessment according to group. No Number
Race had no impact on the total or segmental components of the Ottawa scale when examining all race categories. When examining only the main categories of Caucasian and African American, there was a significant difference between the two categories for fluid content (P=0.0091), indicating Caucasians had better ratings for this component. Eighteen (30.0%) Caucasians had a small amount of fluid compared with seven (10.77%) African Americans. Ten (16.67%) Caucasians had a large amount of fluid compared with 22 (33.85%) African Americans. Sex and history of a family member undergoing colon cancer had no impact on quality of colonoscopy preparation (components of the Ottawa scale or total score). There was no significant correlation between quality of colonoscopy preparation (components of Ottawa scale and total score) and income level, education level or age.
There was no significant difference between the two groups with regard to patient satisfaction. Seventy-five per cent of patients in the video group and 68% in the nonvideo group rated their satisfaction with the preparation process at 5 (five-point scale with 1 = unsatisfied and 5 = satisfied). Race, sex and history of a family member undergoing colon cancer had no impact on patient satisfaction. There was no significant correlation between patient satisfaction and quality of colonoscopy preparation (components of Ottawa scale and total score), income level, education level or age.
DISCUSSION
Bowel preparation has been a limiting factor in the utility of a colonoscopy as a diagnostic and therapeutic modality. Our study demonstrated significant improvements in the quality of colonic preparation with a supplemental educational video to assist with the complex bowel preparation process. We found that patients who viewed a brief instructional video containing bowel preparation instructions had significantly improved colonic preparation quality as measured using the Ottawa scale.
Preparation instructions are often discussed in the outpatient clinic as early as eight weeks before the scheduled colonoscopy; patients may forget key components of the bowel preparation process, which can result in suboptimal bowel preparation. However, providing a supplemental Internet video that may be accessed at any time to review the key components of bowel preparation process can be beneficial to answer any remaining questions and increase compliance with bowel preparation and enhance colonic preparation. In the present study, 64% of patients in the video group indicated they learned additional information from the video, and 95% of patients in the video group reported they would recommend a friend to view the instructional video before the scheduled procedure. Perhaps the improvement in colonic bowel cleansing in the video group resulted from a better understanding of precolonoscopy bowel preparation instructions and led to a greater compliance with the instructions. Despite the majority of patients in the video group (61%) not having had any previous experience with a colonoscopy, the supplemental video group had better colonic cleansing and lower Ottawa scale scores in all locations of the colon. Conversely, despite the fact that a majority (56%) of the patients in the nonvideo group had previous experience undergoing a colonoscopy, their overall Ottawa scale scores were significantly higher than the video group.
In our study, regardless of the study group, race did not affect the total Ottawa scale score but did have a statistically significant impact on the fluid content score. Our study revealed that Caucasians had better scores with less fluid in the colon. However, given that the present analysis was not a multicentre study, the demographics of the local community and race of enrolled patients were limiting factors in our study. The majority of patients enrolled in the present study were Caucasian and African American, with other races representing only 4.48% in the video group and 7.58% in the nonvideo group. Furthermore, we had no Native Americans enrolled in either group. A multicentre centre, possibly at a tertiary care centre, would be useful to truly evaluate the impact of race on bowel preparation.
Patient satisfaction, a secondary end point, was not statistically different between the video and nonvideo groups. The majority of the patients in the video group (75%) and nonvideo (68%) group were satisfied with the bowel preparation. The instructional video may not have impacted satisfaction because it did not modify the bowel preparation process but rather provided patients in the video group with supplemental instructions for greater adherence to the instructions for bowel preparation.
Education and income level did not result in any differences in quality of colonoscopy preparation in the video group and nonvideo group. However, our study was limited to the local enrolled population surrounding metropolitan Atlanta, Georgia. The majority of enrolled study patients had high school and college education, but almost 20% of the total study population had an education level of less than high school. Perhaps, a future study can focus on patients with low education, a group that may experience greater benefit from a supplemental educational resource such as an instructional colonoscopy video. The understanding of colonic preparation may have a greater impact on bowel preparation quality in patients with limited understanding due to a lack of formal education.
Our report is the first published study to evaluate the impact of a SUPREP instructional video on colonic preparation and satisfaction. There have been previous studies evaluating educational resources, with conflicting results on colonic bowel preparation. There were some limitations to our study. First, it was a community-based, single-centre, private practice study with enrolled patients representing the local suburban Atlanta population. Second, enrollment occurred at several offices, with some variation in the population. Finally, our study only evaluated preparation quality and satisfaction with a single preparation (SUPREP Kit) and did not compare other available preparation products and processes.
Further multicentre studies at tertiary care centres with different preparation processes may be useful to evaluate the impact of a supplemental educational video on bowel preparation and satisfaction. However, our study clearly demonstrates a measurable benefit from a supplemental colonoscopy instructional video that is a low-cost and risk-free intervention.
Footnotes
DISCLOSURES: An educational grant was provided for the study from Braintree Laboratories Inc, USA.
REFERENCES
- 1.Calderwood AH, Lai EJ, Fix OK, Jacobson BC. An endoscopist-blinded, randomized, controlled trial of a simple visual aid to improve bowel preparation for screening colonoscopy. Gastrointest Endosc. 2011;73:307–14. doi: 10.1016/j.gie.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 2.Tae JW, Lee JC, Hong SJ, et al. Impact of patient education with cartoon visual aids on the quality of bowel preparation for colonoscopy. Gastroint Endosc. 2012;76:804–11. doi: 10.1016/j.gie.2012.05.026. [DOI] [PubMed] [Google Scholar]
- 3.Abuksis G, Mor M, Segal N, et al. A patient education program is cost-effective for preventing failure of endoscopic procedures in a gastroenterology department. Am J Gastroenterol. 2001;96:1786–90. doi: 10.1111/j.1572-0241.2001.03872.x. [DOI] [PubMed] [Google Scholar]
- 4.Froehlich F, Wietlisbach V, Gonvers JJ, Burnand B, Vader JP. Impact of colonic cleansing on quality and diagnostic yield of colonoscopy: The European Panel of Appropriateness of Gastrointestinal Endoscopy European multicenter study. Gastrointest Endosc. 2005;61:378–84. doi: 10.1016/s0016-5107(04)02776-2. [DOI] [PubMed] [Google Scholar]
- 5.Harewood GC, Sharma VK, de Garmo P. Impact of colonoscopy preparation quality on detection of suspected colonic neoplasia. Gastrointest Endosc. 2003;58:76–9. doi: 10.1067/mge.2003.294. [DOI] [PubMed] [Google Scholar]
- 6.Smith SG, von Wagner C, McGregor LM, et al. The influence of health literacy on comprehension of a colonoscopy preparation information leaflet. Dis Colon Rectum. 2012;55:1074–80. doi: 10.1097/DCR.0b013e31826359ac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spiegel BM, Talley J, Shekelle P, et al. Development and validation of a novel patient educational booklet to enhance colonoscopy preparation. Am J Gastroenterol. 2011;106:875–83. doi: 10.1038/ajg.2011.75. [DOI] [PubMed] [Google Scholar]
- 8.Rex DK, Imperiale TF, Latinovich DR, Bratcher LL. Impact of bowel preparation on efficiency and cost of colonoscopy. Am J Gastroenterol. 2002;97:1696–700. doi: 10.1111/j.1572-0241.2002.05827.x. [DOI] [PubMed] [Google Scholar]
- 9.Byrne MF. The curse of poor bowel preparation for colonoscopy. Am J Gastroenterol. 2002;97:1587–90. doi: 10.1111/j.1572-0241.2002.05855.x. [DOI] [PubMed] [Google Scholar]
- 10.Ness RM, Manam R, Hoen H, Chalasani N. Predictors of inadequate bowel preparation for colonoscopy. Am J Gastroenterol. 2001;96:1797–802. doi: 10.1111/j.1572-0241.2001.03874.x. [DOI] [PubMed] [Google Scholar]
- 11.Lebwohl B, Kastrinos F, Glick M, Rosenbaum AJ, Wang T, Neugut AI. The impact of suboptimal bowel preparation on adenoma miss rates and the factors associated with early repeat colonoscopy. Gastrointest Endosc. 2011;73:1207–14. doi: 10.1016/j.gie.2011.01.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu KL, Rayner CK, Chuah SK, Chiu KW, Lu CC, Chiu YC. Impact of low-residue diet on bowel preparation for colonoscopy. Dis Colon Rectum. 2011;54:107–12. doi: 10.1007/DCR.0b013e3181fb1e52. [DOI] [PubMed] [Google Scholar]
- 13.Verma S, Fogel J, Beyda DJ, Bernstein B, Notar-Francesco V, Mohanty SR. Chronic methadone use, poor bowel visualization and failed colonoscopy: A preliminary study. World J Gastroenterol. 2012;18:4350–6. doi: 10.3748/wjg.v18.i32.4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Modi C, Depasquale JR, Digiacomo WS, et al. Impact of patient education on quality of bowel preparation in outpatient colonoscopies. Qual Primary Care. 2009;17:397–404. [PubMed] [Google Scholar]
- 15.Shaikh AA, Hussain SM, Rahn S, Desilets DJ. Effect of an educational pamphlet on colon cancer screening: A randomized, prospective trial. Eur J Gastroenterol Hepatol. 2010;22:444–9. doi: 10.1097/MEG.0b013e328333fca6. [DOI] [PubMed] [Google Scholar]
- 16.Rosenfeld G, Krygier D, Enns RA, Singham J, Wiesinger H, Bressler B. The impact of patient education on the quality of inpatient bowel preparation for colonoscopy. Can J Gastroenterol. 2010;24:543–6. doi: 10.1155/2010/718628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rostom A, Jolicoeur E. Validation of a new scale for the assessment of bowel preparation quality. Gastrointest Endosc. 2004;59:482–6. doi: 10.1016/s0016-5107(03)02875-x. [DOI] [PubMed] [Google Scholar]


