Abstract
Objective
The aim of this study was to evaluate long-term changes in the pharyngeal airway dimensions after functional appliance treatment in adolescents with skeletal Class II malocclusions.
Methods
Pharyngeal airway dimensions were compared between subjects with skeletal Class II malocclusions (n = 24; mean age: 11.6 ± 1.29 years) treated with a Class II bionator and age-matched control subjects with skeletal Class I occlusions (n = 24; mean age: 11.0 ± 1.21 years) using a series of lateral cephalograms obtained at the initial visit (T0), after treatment (T1), and at the completion of growth (T2).
Results
The length of the nasopharyngeal region was similar between adolescents with skeletal Class I and Class II malocclusions at all time points, while the lengths of the upper and lower oropharyngeal regions and the pharyngeal airway areas were significantly smaller in the skeletal Class II adolescents before treatment when compared to the control adolescents (p < 0.05). However, following treatment with a functional appliance, the skeletal Class II adolescents had increased pharyngeal airway dimensions, which became similar to those of the control subjects.
Conclusions
Functional appliance therapy can increase the pharyngeal airway dimensions in growing adolescents with skeletal Class II malocclusions, and this effect is maintained until the completion of growth.
Keywords: Pharyngeal airway, Functional appliance, Skeletal Class II, Lateral cephalogram
INTRODUCTION
Patients with skeletal Class II malocclusions and retrusive mandibles can have breathing problems.1 In an analysis using cone-beam computed tomography imaging, children classified with skeletal Class II malocclusions and retrusive mandibles also had smaller pharyngeal airway dimensions than children with skeletal Class I malocclusions.2 Without therapeutic intervention, voluntary anterior-posterior compensation does not occur with normal growth of the mandible.3-5 Therefore, children with skeletal Class II malocclusions may have a higher probability of maintaining the skeletal phenotype, even after growth, as they have smaller pharyngeal airway dimensions than children with Class I malocclusions.
The pharyngeal airway is divided into the nasopharynx, oropharynx, and laryngeal pharynx, among which the nasopharynx and oropharynx play an important role in respiration. The adenoids can be found within the nasopharyngeal region, and their enlargement may induce mouth breathing due to a reduction in the dimension of the nasopharyngeal airway.6 Narrow pharyngeal airway dimensions in the oropharyngeal area also cause breathing problems and may lead to a reduction in growth hormone levels in growing children and obstructive sleep apnea in adults.7,8
With abnormal breathing, a growing child may show problems with maxillofacial growth, such as a vertical facial pattern, skeletal Class II malocclusion, and posterior crossbite.9 However, the jaw bones have been verified to grow normally once the respiratory functions are recovered by removing the factors that infringe breathing.10
Although many studies have demonstrated the skeletal effects of Class II functional appliances, reports on the effect of functional appliances on the soft tissues and muscles around the maxillofacial region are limited.11 In a study by Ozbek et al.,12 the oropharynx increased in subjects with skeletal Class II malocclusions after treatment with Harvold-type activators; however, the observation period of less than 2 years was relatively short. Hanggi et al.13 reported a short-term increase and a long-term (up to 12.0 years) maintenance of the pharyngeal airway dimension after activator treatment in subjects with skeletal Class II malocclusions during growth. However, in this study, headgear and functional appliances were simultaneously used, and specific evaluation regarding growth, such as the use of hand-wrist radiographs, did not occur.
Thus, the objective of this study was to evaluate the short-term and long-term changes in pharyngeal airway dimensions in adolescents with skeletal Class II malocclusions treated only with functional appliances.
MATERIALS AND METHODS
Subjects
The treatment records of adolescents with skeletal Class II malocclusions were retrieved from the Department of Orthodontics at Gangnam Severance Dental Hospital located in Seoul, Korea, with the approval of the institutional review board retrospectively (No. 3-2013-0105). The inclusion criteria were as follows:
Adolescents who had not yet reached peak growth with a skeletal maturity indicator (SMI) <5, as evaluated by hand-wrist radiographs.14
Diagnosed with skeletal Class II malocclusion and retrusive mandible, including an A point-Nasion-B point angle (ANB) >5°, Sella-Nasion-B point angle (SNB) < 77°, and overjet > 5 mm. Treated with a Class II bionator with good compliance to treatment.
Presence of serial lateral cephalograms before treatment (T0), after functional appliance treatment (T1), and at the completion of growth (T2).
Presence of hand-wrist radiographs to evaluate growth, as well as for comparison to the lateral cephalograms at T0 and T2.
A skeletal midline deviation > 2 mm.
A total of 24 subjects were included in the bionator group (mean age: 11.6 ± 1.29 years), and the mean treatment period with a Class II bionator was around 2 years.
For the control group, age-matched subjects (mean age: 11.0 ± 1.21 years) who were diagnosed as skeletal Class I (0° < ANB < 4°) with minor dental crowding and had serial lateral cephalograms (T0; T1, taken 2 years after T0; and T2) along with matching hand-wrist radiographs were selected. The subjects' demographic features are shown in Table 1.
Table 1.
Mean age (year) and number of subjects
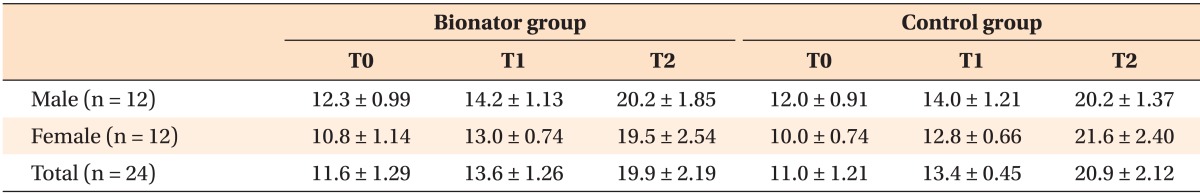
Values are presented as mean ± standard deviation.
T0, Before treatment; T1, after functional appliance treatment in the bionator group and after an observation period of the same length in the control group; T2, completion of growth.
Measurements
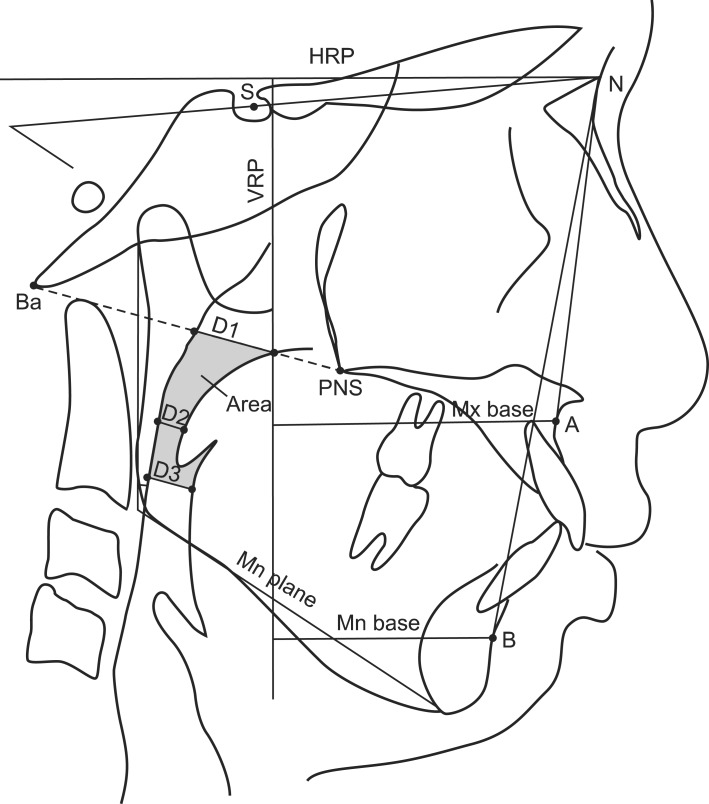
The software program, V-Ceph 6.0 (Osstem Implant Co. Ltd., Seoul, Korea), was used to perform five linear and four angular measurements. A line was reconstructed 7° upward from the Sella-Nasion line at Nasion and was defined as the horizontal reference plane (HRP); a line perpendicular to the HRP and tangent to the anterior wall of Sella was defined as the vertical reference plane (VRP) (Figure 1).15
Figure 1.
Measurements of linear, angular, and pharyngeal airway dimensions. HRP, horizontal reference plane; VRP, vertical reference plane; S, Sella; N, Nasion; Ba, Basion; PNS, posterior nasal spine; A, A point; B, B point; D1, the length at which the PNS-Ba line intersects the pharyngeal airway; D2, the narrowest distance between the soft palate and the posterior pharyngeal wall; D3, the narrowest distance between the base of tongue and the posterior pharyngeal wall; Area, the area between D1 and D3.
Mx base and Mn base indicate A point and B point perpendicular distances to VRP, respectively. Mn plane indicates Gonion-Menton line.
To determine the angular measurements, we performed the following calculations: The perpendicular distance from A point to the VRP was defined as the length of the maxillary basal bone (Mx base), and the perpendicular distance from B point to the VRP was defined as the length of the mandibular basal bone (Mn base). Mx-Mn was defined as the difference in length between the Mx base and the Mn base. For angular measurements, SNA, SNB, ANB, gonial angle, and mandibular plane angle (Mn plane angle) were measured.
For the pharyngeal airway measurements, we utilized the following: D1, D2, and D3. The D1 measurement corresponded to the length at which the PNS-Ba line intersected the pharyngeal airway. Meanwhile, D2 referred to the length of the upper oropharyngeal region and was measured at the narrowest distance between the soft palate and posterior pharyngeal wall. D3 indicated the length of the lower oropharyngeal region and was measured at the narrowest distance between the base of tongue and the posterior pharyngeal wall.13,16 The pharyngeal airway area was measured as the area between D1 and D3 (Figure 1).
Statistical analysis
The IBM SPSS Statistics 19.0 for Windows (IBM Co., Armonk, NY, USA) was used for statistical analysis. The Wilcoxon rank sum test was used for gender comparison of the pharyngeal airway measurements at T0. Two-sample t-test was conducted to compare measurements between the bionator and control group. Paired t-test was used to compare changes in the pharyngeal airway dimensions within the groups during each observation period (T1-T0, T2-T1, and T2-T0). A two-sample t-test was conducted to compare intergroup differences in changes in pharyngeal airway dimensions. The interaction effect was calculated by using a linear mixed model in order to identify the relationship between the skeletal measurements and pharyngeal airway measurements. One operator examined all measurements. To evaluate the intra-operator reliability, the same operator reanalyzed 30 randomly selected cephalometric tracings in a two-week interval. The intraclass correlation coefficient showed a high reliability (> 0.95).
RESULTS
Comparison of pharyngeal airway dimensions between the genders before treatment (Table 2)
Table 2.
Comparison of pharyngeal airway dimensions between male and female subjects before treatment
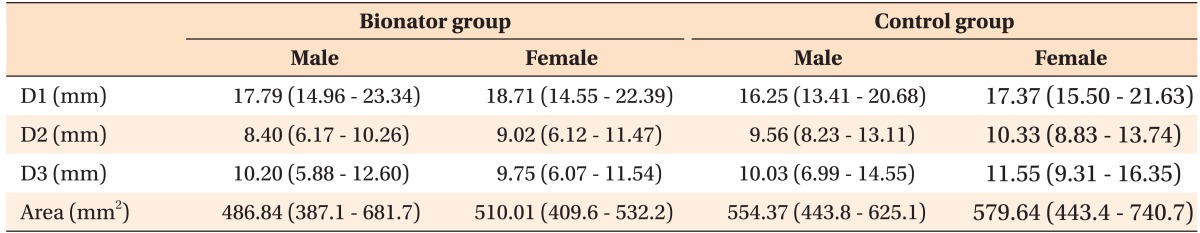
Values are presented as median (minimum - maximum).
All data is not statistically significant.
See Figure 1 for the landmarks and the measurements.
At T0, there was no significant difference in the pharyngeal airway dimension measurements between males and females (p > 0.05).
Comparison of skeletal and pharyngeal airway dimensions between the bionator and control group (Table 3)
Table 3.
Comparison of measurements between the control and bionator groups
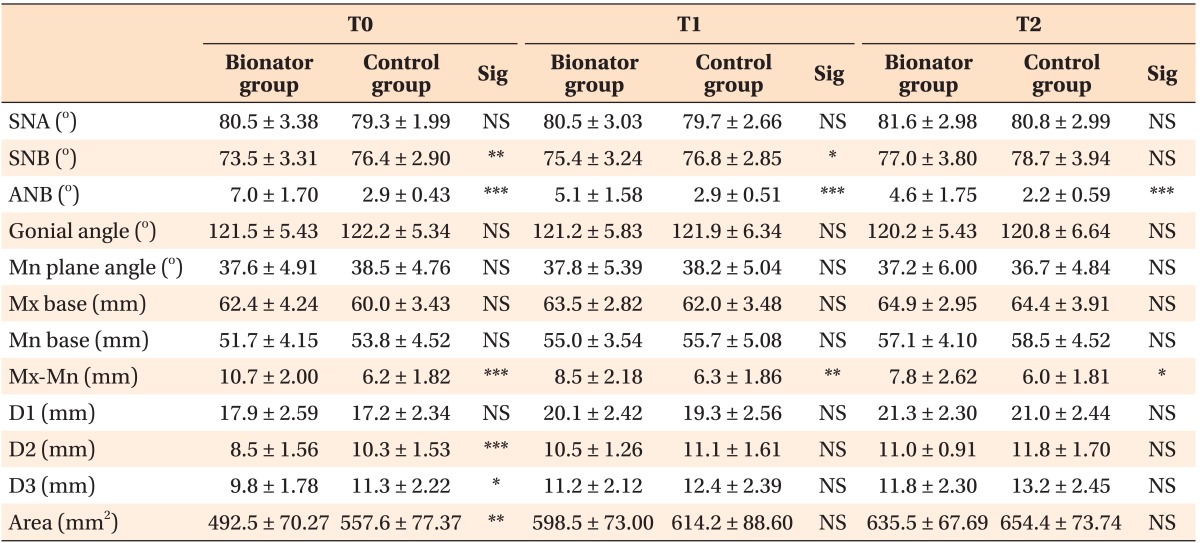
Values are presented as mean ± standard deviation.
Sig, Significance; NS, not significant; *p < 0.05; **p < 0.01; ***p < 0.001.
T0, Initial; T1, right after functional appliance treatment in the bionator group and after the same duration in the control group; T2, growth completion; SNA, Sella-Nasion-A point angle; SNB, Sella-Nasion-B point angle; ANB, A point-Nasion-B point angle.
See Figure 1 for the landmarks and the measurements.
In the bionator group, ANB decreased from 7.0 ± 1.70° before treatment (T0) to 5.1 ± 1.58° after functional appliance treatment (T1). Additionally, in the bionator group, the difference in length between the basal bones of the upper and lower jaws (Mx-Mn) also decreased from 10.7 ± 2.00 mm (T0) to 8.5 ± 2.18 mm (T1) with functional appliance treatment. The ANB and Mx-Mn of the control group was relatively stable from T0 to T1.
In terms of the pharyngeal airway, D1 was similar between the bionator and control groups at T0 (p > 0.05). However, D2, D3, and pharyngeal airway area (Area) were significantly smaller in the bionator group when compared to those of the control group at T0 (p < 0.05). Following the use of a functional appliance (T1) and also after the completion of growth (T2), D1, D2, D3, and Area in the bionator group reached similar levels to those of the control group (p > 0.05).
Changes in the pharyngeal airway measurements during each observation period (Table 4)
Table 4.
Changes in pharyngeal airway dimensions in the bionator and control groups
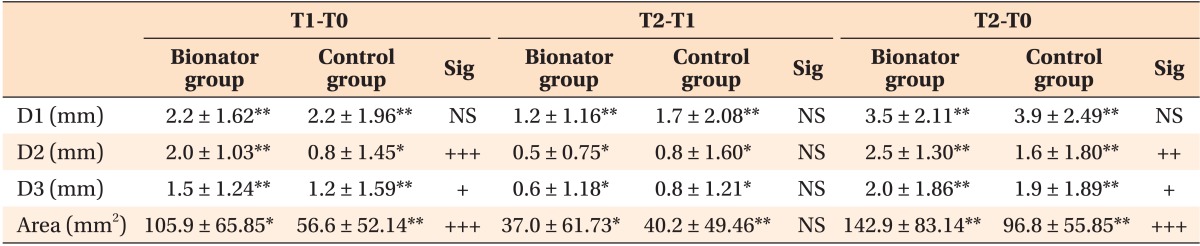
Values are presented as mean ± standard deviation.
Sig, Significance; NS, not significant; comparisons within each group.
*p < 0.05; **p < 0.01; ***p < 0.001; comparisons between the bionator and control groups. +p < 0.05; ++p < 0.01; +++p < 0.001.
T0, Initial; T1, right after functional appliance treatment in the bionator group and after the same duration in the control group; T2, growth completion.
See Figure 1 for the landmarks and the measurements.
Pharyngeal airway measurements significantly increased throughout the observation period (T1-T0, T2-T1, and T2-T0) for both the bionator and control groups (p < 0.05). However, the increase from T0 to T1 was significantly larger in the bionator group than in the control group, except for D1 (p < 0.05). The pharyngeal airway dimensions increased during the posttreatment observation period (T2-T1) and were similar in both groups. For the overall changes from T0 to T2, the bionator group had significantly greater changes in D2, D3, and Area compared to those of the control group (p < 0.05).
Interaction effects between the skeletal measurements and pharyngeal airway measurements (Table 5)
Table 5.
Interaction effects between the skeletal measurements and pharyngeal airway dimensions
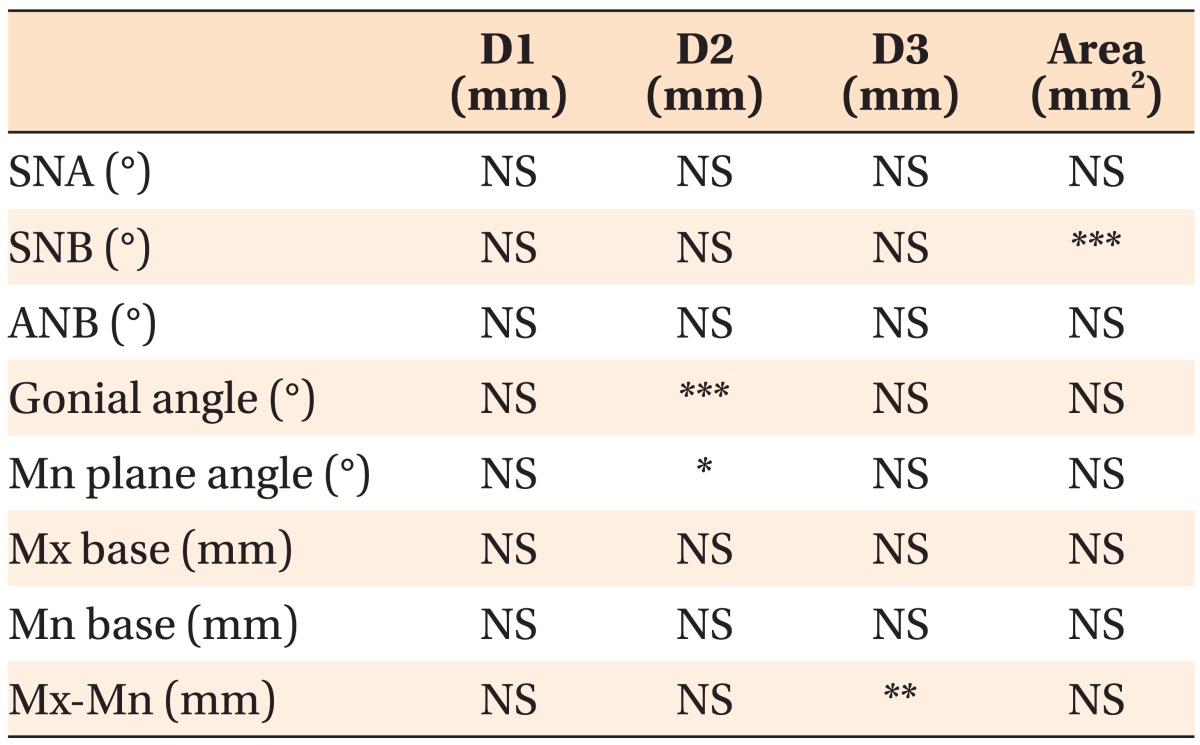
NS, Not significant; *p < 0.05; **p < 0.01; ***p < 0.001.
See Figure 1 for the landmarks and the measurements.
The interaction effects between the skeletal measurements (SNA, SNB, ANB, gonial angle, Mn plane angle, Mx base, Mn base, and Mx-Mn) and pharyngeal airway measurements (D1, D2, D3, and Area) were examined using a linear mixed model. Gonial angle (p < 0.001) and Mn plane angle (p < 0.05) showed significant relationships with D2, while SNB showed a significant relationship with Area (p < 0.001). Mx-Mn also exhibited a significant relationship with D3 (p < 0.01).
DISCUSSION
This study showed that adolescents with skeletal Class II malocclusions treated with functional appliances experienced increased pharyngeal airway dimensions and that such changes were maintained throughout growth until the completion of growth.
According to our results, there was no significant difference in the nasopharyngeal region (D1) from T0 to T2 between the two groups. This is probably because the nasopharyngeal region is directly influenced by the size of the adenoids and is not changed by orthopedic treatment.17 The adenoids reach their greatest size at the age of 10 years in boys and 9 years in girls and then gradually decrease thereafter.18 However, in this study, the mean age of the male subjects at T0 was 12.0 years and 12.3 years in the control and bionator groups, respectively, while the mean age of the female subjects at T0 was 10.0 years and 10.8 years in the control and bionator groups, respectively. Furthermore, reports have indicated that adolescents experience a reduction in adenoid size19,20 which could explain the increase in D1 in both the bionator and control groups during the treatment period and also during the posttreatment period.
In the oropharyngeal region, the narrowest part of the cross section is considered clinically important in terms of airflow and oxygen saturation.21 Therefore, in this study, the narrowest distances from the posterior soft palate to the posterior pharyngeal wall and the narrowest distance from the posterior tongue base to the posterior pharyngeal wall were used as measurements for the upper and lower oropharyngeal regions, respectively. From a comparison of the bionator and control groups, adolescents with skeletal Class II malocclusions had significantly smaller oropharyngeal regions when compared to adolescents with skeletal Class I malocclusions at the initial visit (p < 0.05). Previous studies demonstrated similar results in skeletal Class II subjects with significantly smaller pharyngeal airway dimensions in the oropharynx than skeletal Class I subjects, in both adults and children.22,23 This is probably because pharyngeal airway dimensions become narrower due to posterior positioning of the tongue and soft palate in subjects with retrognathic mandibles.12
After functional appliance treatment, pharyngeal airway dimensions corresponding to the oropharynx increased in skeletal Class II subjects and reached similar dimensions to that of the skeletal Class I subjects. This indicates that during functional appliance treatment the increase in the pharyngeal airway dimensions exceeded the increase normally seen with growth. In addition, there was no difference in measurements after the termination of growth between the two groups, suggesting that the increase in the pharyngeal airway dimension can be maintained until the termination of growth. Stretching of the tongue and the suprahyoid muscles can accompany the mandibular advancement seen with functional appliance treatment, which in turn leads to an increased pharyngeal airway dimension and therefore improved respiration.24
The upper oropharyngeal region was reported to increase by about 0.5 mm during growth.13 In this study, the increase in the upper oropharyngeal region was about 0.8 mm in the skeletal Class I subjects, while the skeletal Class II subjects treated with functional appliances showed an increase that was more than twice as large at 2.0 mm during the same period. With respect to the lower oropharyngeal region, the mean lower oropharyngeal dimension of the skeletal Class II subjects was 11.8 mm after the completion of growth in this study, corresponding well to the previously reported normal range of 10 - 12 mm.25
Considering the relationship between skeletal measurements and pharyngeal airway measurements, a significant interaction effect was detected between SNB and the pharyngeal airway area (p < 0.001). Gonial angle and mandibular plane angle only showed a significant interaction effect in the upper oropharyngeal region (p < 0.05). Therefore, it can be hypothesized that the vertical facial pattern influences the upper oropharyngeal region. In addition, a difference in the basal bone length between the upper and lower jaws (Mx-Mn) showed a significant interaction effect with the lower oropharyngeal region (p < 0.01). Additional studies with a larger sample size could provide insight into the specific interactions between skeletal measurements and pharyngeal airway dimensions.
In this study, ANB and Mx-Mn differences in the bionator group during treatment were improved by 1.9° and 2.2 mm, respectively. Such increases did not demonstrate any relapses until the termination of appliance treatment. After functional appliance treatment, an increase in the pharyngeal airway dimension can be seen as a result of the combination of treatment effects and normal pharyngeal airway growth.17 Therefore, future studies comparing untreated and treated adolescents with skeletal Class II malocclusions would be helpful in evaluating pure treatment effects.
Lateral cephalograms have been used in many studies to analyze pharyngeal airway dimensions. Even though lateral cephalograms only provide two-dimensional information and three-dimensional images are more informative, regular imaging using three-dimensional techniques in growing adolescents is not necessary for orthodontic treatment purposes. A small increase in the sagittal plane may lead to greater changes in the pharyngeal airway dimensions, which could then improve airflow.13
In growing adolescents, treatment with functional appliances allows harmonious craniofacial development through changes in the hard and soft tissues, accompanied by increases in pharyngeal airway dimensions.
CONCLUSION
Growing adolescents with skeletal Class II malocclusions treated with functional appliances demonstrated an increase in pharyngeal airway dimensions of the oropharyngeal region, and such changes were consistently maintained even after the completion of growth. Therefore, through appropriate therapeutic intervention, an improvement in the skeletal relationship can help obtain an additional advantage with respect to pharyngeal airway dimensions, as well as improve the facial profile and dentoalveolar relationship.
Footnotes
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Li Y. Early orthodontic treatment of skeletal Class II malocclusion may be effective to prevent the potential for OSAHS and snoring. Med Hypotheses. 2009;73:594–595. doi: 10.1016/j.mehy.2009.05.041. [DOI] [PubMed] [Google Scholar]
- 2.Kim YJ, Hong JS, Hwang YI, Park YH. Three-dimensional analysis of pharyngeal airway in preadolescent children with different anteroposterior skeletal patterns. Am J Orthod Dentofacial Orthop. 2010;137:306.e1–306.e11. doi: 10.1016/j.ajodo.2009.10.025. [DOI] [PubMed] [Google Scholar]
- 3.Subtelny JD. To treat or not to treat. Int Dent J. 1973;23:292–303. [PubMed] [Google Scholar]
- 4.Bishara SE, Hoppens BJ, Jakobsen JR, Kohout FJ. Changes in the molar relationship between the deciduous and permanent dentitions: a longitudinal study. Am J Orthod Dentofacial Orthop. 1988;93:19–28. doi: 10.1016/0889-5406(88)90189-8. [DOI] [PubMed] [Google Scholar]
- 5.You ZH, Fishman LS, Rosenblum RE, Subtelny JD. Dentoalveolar changes related to mandibular forward growth in untreated Class II persons. Am J Orthod Dentofacial Orthop. 2001;120:598–607. doi: 10.1067/mod.2001.119801. [DOI] [PubMed] [Google Scholar]
- 6.Proffit WR, Fields HW, Sarver DM. Contemporary orthodontics. 5th ed. St. Louis: Elsevier; 2012. pp. 141–145. [Google Scholar]
- 7.Späth-Schwalbe E, Hundenborn C, Kern W, Fehm HL, Born J. Nocturnal wakefulness inhibits growth hormone (GH)-releasing hormone-induced GH secretion. J Clin Endocrinol Metab. 1995;80:214–219. doi: 10.1210/jcem.80.1.7829614. [DOI] [PubMed] [Google Scholar]
- 8.Born J, Muth S, Fehm HL. The significance of sleep onset and slow wave sleep for nocturnal release of growth hormone (GH) and cortisol. Psychoneuroendocrinology. 1988;13:233–243. doi: 10.1016/0306-4530(88)90021-2. [DOI] [PubMed] [Google Scholar]
- 9.Agren K, Nordlander B, Linder-Aronsson S, Zettergren-Wijk L, Svanborg E. Children with nocturnal upper airway obstruction: postoperative orthodontic and respiratory improvement. Acta Otolaryngol. 1998;118:581–587. doi: 10.1080/00016489850154766. [DOI] [PubMed] [Google Scholar]
- 10.Williams EF, 3rd, Woo P, Miller R, Kellman RM. The effects of adenotonsillectomy on growth in young children. Otolaryngol Head Neck Surg. 1991;104:509–516. doi: 10.1177/019459989110400415. [DOI] [PubMed] [Google Scholar]
- 11.Hiyama S, Kuribayashi G, Ono T, Ishiwata Y, Kuroda T. Nocturnal masseter and suprahyoid muscle activity induced by wearing a bionator. Angle Orthod. 2002;72:48–54. doi: 10.1043/0003-3219(2002)072<0048:NMASMA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Ozbek MM, Memikoglu TU, Gögen H, Lowe AA, Baspinar E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal Class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 13.Hänggi MP, Teuscher UM, Roos M, Peltomäki TA. Long-term changes in pharyngeal airway dimensions following activator-headgear and fixed appliance treatment. Eur J Orthod. 2008;30:598–605. doi: 10.1093/ejo/cjn055. [DOI] [PubMed] [Google Scholar]
- 14.Fishman LS. Radiographic evaluation of skeletal maturation. A clinically oriented method based on hand-wrist films. Angle Orthod. 1982;52:88–112. doi: 10.1043/0003-3219(1982)052<0088:REOSM>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 15.Baccetti T, Franchi L, McNamara JA, Jr, Tollaro I. Early dentofacial features of Class II malocclusion: a longitudinal study from the deciduous through the mixed dentition. Am J Orthod Dentofacial Orthop. 1997;111:502–509. doi: 10.1016/s0889-5406(97)70287-7. [DOI] [PubMed] [Google Scholar]
- 16.Goncalves JR, Buschang PH, Goncalves DG, Wolford LM. Postsurgical stability of oropharyngeal airway changes following counter-clockwise maxillo-mandibular advancement surgery. J Oral Maxillofac Surg. 2006;64:755–762. doi: 10.1016/j.joms.2005.11.046. [DOI] [PubMed] [Google Scholar]
- 17.Restrepo C, Santamaría A, Peláez S, Tapias A. Oropharyngeal airway dimensions after treatment with functional appliances in class II retrognathic children. J Oral Rehabil. 2011;38:588–594. doi: 10.1111/j.1365-2842.2011.02199.x. [DOI] [PubMed] [Google Scholar]
- 18.Hwang CJ, Ryu YK. A longitudinal study of nasopharynx and adenoid growth of Korean children. Korean J Orthod. 1985;15:93–103. [Google Scholar]
- 19.Harris JA, Jacksn CM, Paterson DG, Scammon RE. The measurement of man. Minneapolis: University of Minnesota Press; 1930. [Google Scholar]
- 20.Subtelny JD, Baker HK. The significance of adenoid tissue in velopharyngeal function. Plast Reconstr Surg (1946) 1956;17:235–250. doi: 10.1097/00006534-195603000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Avrahami E, Englender M. Relation between CT axial cross-sectional area of the oropharynx and obstructive sleep apnea syndrome in adults. AJNR Am J Neuroradiol. 1995;16:135–140. [PMC free article] [PubMed] [Google Scholar]
- 22.Abu Allhaija ES, Al-Khateeb SN. Uvulo-glosso-pharyngeal dimensions in different anteroposterior skeletal patterns. Angle Orthod. 2005;75:1012–1018. doi: 10.1043/0003-3219(2005)75[1012:UDIDAS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 23.Ceylan I, Oktay H. A study on the pharyngeal size in different skeletal patterns. Am J Orthod Dentofacial Orthop. 1995;108:69–75. doi: 10.1016/s0889-5406(95)70068-4. [DOI] [PubMed] [Google Scholar]
- 24.Rose EC, Germann M, Sorichter S, Jonas IE. Case control study in the treatment of obstructive sleep-disordered breathing with an intraoral protrusive appliance. J Orofac Orthop. 2004;65:489–500. doi: 10.1007/s00056-004-0423-y. [DOI] [PubMed] [Google Scholar]
- 25.McNamara JA., Jr A method of cephalometric evaluation. Am J Orthod. 1984;86:449–469. doi: 10.1016/s0002-9416(84)90352-x. [DOI] [PubMed] [Google Scholar]