Abstract
Since the first transgastric natural orifice transluminal endoscopic surgery was described, various applications and modified procedures have been investigated. Transgastric natural orifice transluminal endoscopic surgery for periotoneoscopy, cholecystectomy, and appendectomy all seem viable in humans, but additional studies are required to demonstrate their benefits and roles in clinical practice. The submucosal tunneling method enhances the safety of peritoneal access and gastric closure and minimizes the risk of intraperitoneal leakage of gastric air and juice. Submucosal tunneling involves submucosal tumor resection and peroral endoscopic myotomy. Peroral endoscopic myotomy is a safe and effective treatment option for achalasia, and the most promising natural orifice transluminal endoscopic surgery procedure. Endoscopic full-thickness resection is a rapidly developing natural orifice transluminal endoscopic surgery procedure for the upper gastrointestinal tract and can be performed with a hybrid natural orifice transluminal endoscopic surgery technique (combining a laparoscopic approach) to overcome some limitations of pure natural orifice transluminal endoscopic surgery. Studies to identify the most appropriate role of endoscopic full-thickness resection are anticipated. In this article, I review the procedures of natural orifice transluminal endoscopic surgery associated with the upper gastrointestinal tract.
Keywords: Natural orifice transluminal endoscopic surgery, Peroral endoscopic myotomy, Endoscopic full-thickness resection
Introduction
Natural orifice transluminal endoscopic surgery (NOTES) is a new minimally invasive surgery that accesses the peritoneal or thoracic spaces through a transvisceral incision instead of a skin incision. To overcome the technical limitations of NOTES, a hybrid NOTES technique, which combines a transcutaneous rigid laparoscopic approach with pure NOTES, can be used. Possible transvisceral routes for hybrid NOTES include transesophageal, transgastric, transcolonic, and transvaginal routes. In theory, NOTES could reduce postoperative pain, wound complications, and the need for anesthesia, improve cosmetic results, and accelerate patient recovery and return to normal function, although these benefits have not been fully proven.1
The current upper gastrointestinal tract-related NOTES procedures have been performed in humans for transgastric organ resection (i.e., cholecystectomy, appendectomy), transgastric peritoneoscopy, transesophageal procedures (peroral endoscopic myotomy, POEM), and endoscopic full-thickness resection (EFTR). This paper reviews the NOTES procedures associated with the upper gastrointestinal tract in humans.
Transgastric Intraperitoneal Natural Orifice Transluminal Endoscopic Surgery Using Direct Incision
NOTES was first performed for transgastric peritoneoscopy in pigs.2 The peritoneal cavity was entered by direct incision of the anterior gastric wall with a needle knife, followed by dilation of the tract with a balloon dilator. After this first report, various NOTES procedures were tested in animal models, and the transgastric route was preferred in the beginning of NOTES because gastroscopy was familiar with gastroenterologist procedures.3 Current transgastric intraperitoneal NOTES procedures using direct incision have been used in humans for peritoneoscopy, cholecystectomy, and appendectomy.
The first NOTES peritoneoscopy performed in humans was reported in 2008.4 Ten patients underwent diagnostic laparoscopy followed by transgastric access and endoscopic peritoneoscopy. Transgastric NOTES peritoneoscopy was reported to be safe in all patients, and the mean duration of the procedure was 24.8 minutes. The largest study of transgastric cholecystectomy in humans was reported in 2010.5 A total of 27 transgastric cholecystectomies were performed by hybrid NOTES, and the rate of complications such as gastric hematoma, abdominal sepsis, and esophageal perforations was 18%. A recent study including 14 consecutive transgastric appendectomies6 showed that two patients with purulent peritonitis required laparoscopic lavage several days after the procedure, although no leaks were detected at the appendiceal stump or stomach.
All of these transgastric intraperitoneal NOTES procedures were successful in humans, but are not widely applied in clinic practice. In a recent randomized study in a porcine model, transgastric peritoneoscopy showed worse outcomes than laparoscopic peritoneoscopy. Standard laparoscopy provided significantly better lesion detection (78.5% vs. 38.9%), organ visualization (7.15 vs. 4.35), and biopsy capability (87% vs. 65%) than transgastric NOTES.7 Additional studies on transgastric cholecystectomy and appendectomy are required to demonstrate their role in clinical practice.
Submucosal Tunneling Method
Submucosal tunneling was developed to guarantee safe peritoneal access, secure gastric closure, and accelerate healing of the incision site. The submucosal tunnel was created using endoscopic submucosal dissection techniques and tools. After submucosal injection of 5 to 15 ml of normal saline, a 2-cm incision was made in the mucosa using ESD knives. Submucosal dissection was then performed to create a submucosal tunnel. The length of the tunnel depended on the type of procedure. A 4 to 5 cm tunnel was adequate for subepithelial tumor dissection, but a 10-cm tunnel was used for POEM. After the NOTES procedure, closure of the mucosal incision was performed using several endoscopic clips.8,9
Submucosal tunneling has the advantage8,9 of the seromuscular incision site being situated far from the mucosal incision site, which allows minimization of any intraperitoneal leakage of gastric content and air by the narrow, long submucosal tract during the procedure. Maintaining gastric distension even after seromuscular incision allows better endoscopic view and working space, thus allowing easy placement of the clips for closure of the incision. Approximated surfaces of the narrow and longitudinal tunnel healed rapidly. Submucosal tunneling can be used for transgastric intraperitoneal procedures, dissection of subepithelial tumors, and POEM.
The initial submucosal tunneling procedure was access peritoneum via stomach.8 Diagnostic transgastric peritoneoscopy using submucosal tunneling was successful with the patient under conscious sedation.10 However, in a recent randomized trial in an animal model, submucosal tunneling was found to permit lower visualization than direct incision.11
Laparoscopic resection is not easy for subepithelial tumors that are located in the esophagus or gastric cardia. For these locations, dissection of subepithelial tumors using the submucosal tunneling technique is a possible alternative intervention. Several recent retrospective studies have shown a 78% to 100% rate of successful subepithelial tumor resection using submucosal tunneling (Table 1).12-17 Frequent complications seen were pneumothorax and subcutaneous emphysema, which improved in most cases with conservative management, although a few patients required chest tube insertion or subcutaneous puncture.16,17 Further studies are required to demonstrate the efficiency of this technique for subepithelial tumors (particularly gastrointestinal stromal tumors) with regard to its safety and ability to achieve complete resection with an intact capsule. The long-term follow-up data after resection is also required.
Table 1.
Published studies on submucosal tunneling method for subepithelial tumors
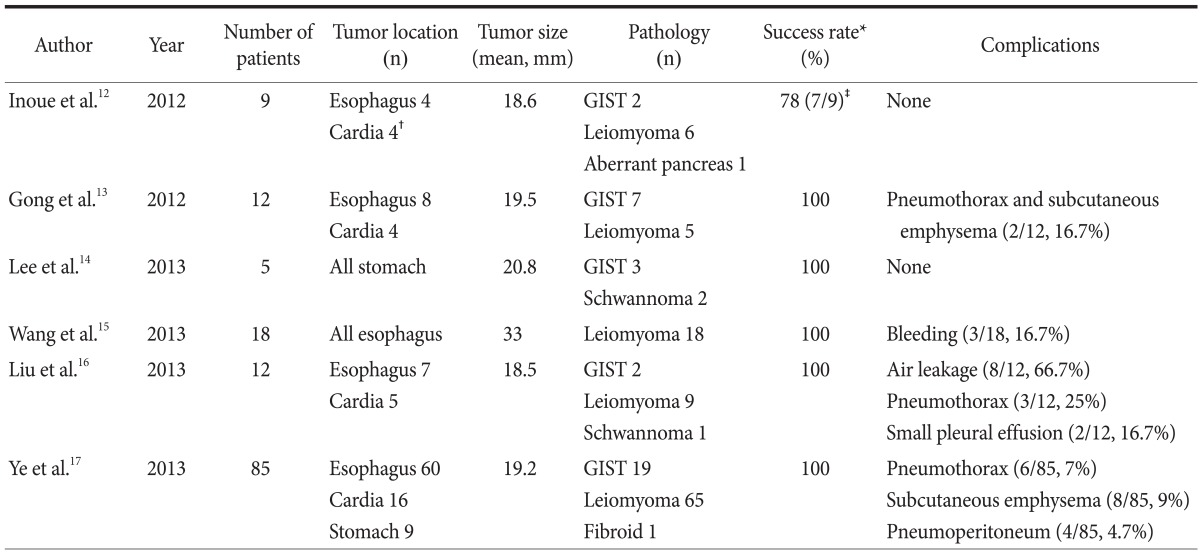
GIST = gastrointestinal stromal tumor. *Success of complete and en bloc resection by submucosal tunneling method. †Unknown location of one case. ‡Failed for large subepithelial tumors (60 mm and 75 mm).
Peroral Esophageal Myotomy
Achalasia is the primary esophageal motility dysfunction disorder. The loss of inhibitory neurons of the myenteric plexus results in failure of the lower esophageal sphincter to relax in response to swallowing. Traditional treatments include pharmacological management, endoscopic intervention (botulinum toxin injection, pneumatic dilation), and surgical treatment (laparoscopic Heller myotomy, LHM). LHM has shown the most satisfactory long-term results. The overall success rate of LHM was 77.0% to 97.2%.18
POEM is a new endoscopic treatment modality for achalasia. Endoscopic myotomy was first used in achalasia patients 30 years ago with the needle knife used for direct incision of muscle at the esophagogastric junction (EGJ).19 Pasricha et al.20 first described the current method using submucosal tunneling and an insulated-tip knife in a pig model, which was then performed by Inoue et al.21 in humans. POEM consists of several steps. 1) After submucosal injection, a 2-cm long mucosal incision is made at approximately 10 to 13 cm proximal to the EGJ. 2) A long submucosal tunnel is created 2 to 3 cm distal to the EGJ. 3) Endoscopic myotomy is performed 3 to 5 cm distal from the mucosal incision site in a proximal to distal direction. Long endoscopic myotomy of the inner circular muscle bundles is performed using an insulated-tip knife, leaving the outer longitudinal muscle layer intact. The expected end point of myotomy is 2 cm distal to the EGJ. 4) The mucosal incision is closed using hemostatic clips. The learning curve for POEM plateaus at approximately 20 cases for experienced endoscopists.22
Over 10 reports of POEM use for achalasia have been published, and these indicate good short-term results without serious complications. In a recent international prospective multicenter study on POEM of 70 patients at five centers in the Europe and North America, the endoscopist had to perform at least two procedures under the direct guidance of an endoscopist with good experience in performing POEM, prior to performing POEM independently.23 All procedures were successful, and no conversions to laparoscopic or open surgery were required. The percentage of patients in symptom remission at 3, 6, and 12 months was 97%, 89%, and 82%, respectively.
POEM has several theoretical advantages over LHM because it is less invasive and can allow myotomy to be performed in the proximal esophagus. Extending the distance to allow LHM to be performed in the thoracic esophagus is difficult in patients with advanced disease, and the risk of injury to the vagus nerve is lower with POEM because myotomy is performed from inside the esophageal lumen. Because the target area for POEM is the lateral side of the esophagus and that for LHM is the anterior side, a subsequent LHM is a feasible second-line treatment if POEM fails.23
Acid reflux is a major complication after successful LHM and POEM. Addition of an anti-reflux procedure to LHM can substantially reduce the incidence and severity of acid reflux.24,25 The incidence of reflux after LHM, with or without an anti-reflux procedure is 3% to 34% according to the literature.18 In a multicenter study, the rate of acidic reflux was 42% at 3 months after POEM.23 Although the rate of reflux after POEM appears to be higher than that after LHM, the severity of esophagitis was minor (grade A or B) and only 12% of patients required daily proton pump inhibitor therapy.23 Currently, no randomized trial has compared LHM with POEM. Outcomes of POEM were comparable with those of LHM in short-term retrospective studies and long-term prospective randomized trials are required.26-28
Endoscopic Full-Thickness Resection
Conventional endoscopic submucosal dissection techniques are not used for subepithelial tumors originating from, or infiltrating into, the muscularis propria layer because of the increased risk of incomplete resection and perforation. Laparoscopic wedge resection is a minimally invasive treatment that is effective for most subepithelial tumors, and is usually performed from outside the stomach using a linear stapler. The exogastric approach with a linear stapler can lead to excessive resection of healthy tissue of the gastric wall resulting in deformity or stenosis. Attaining a positive surgical margin is also possible. EFTR can be used for tumor resection by direct visualization of the tumor from inside the stomach lumen leading to a free surgical margin with little resection of healthy tissue.
EFTR can be performed using pure NOTES that involves only endoscopy without laparoscopy (Table 2).29-31 In a simple method of EFTR, gastric tumors can be grasped and lifted by the tissue anchor and then resected with a snare.29 In other procedures, the tumors are separated from the muscularis layer using an insulated-tip knife under direct vision until less than one-fifth of the lesion remains, and then a snare used.30 In the most detailed procedure, a circumferential incision is made as deep as the muscularis propria around the lesion, and incision of the serosal layer is performed with a Hook knife or insulated-tip knife. Finally, the tumor is removed with a snare.31 En bloc resection rates were 100% and no patient had severe complications, although 2 of the 20 patients needed ultrasound-guided percutaneous puncture for drainage of the abdominal cavity effusion in a retrospective study.30
Table 2.
Published studies on endoscopic full-thickness resection with pure NOTES in humans
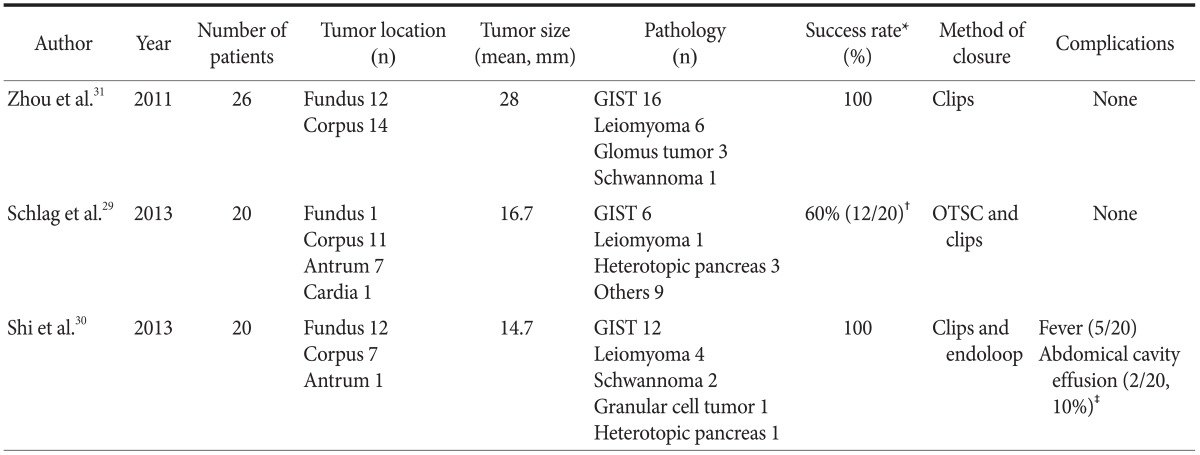
NOTES = natural orifice transluminal endoscopic surgery; GIST = gastrointestinal stromal tumor; OTSC = over-the-scope clip. *Success of complete and en bloc resection followed by clipping using pure NOTES. †In 6 of 20 cases, pure NOTES was impossible and conversion to laparoscopic wedge resection was necessary due to extraluminal growth and the large size of the tumors. Incomplete resection with positive deep margins occurred in 2 cases of 14 patients in the pure NOTES group. ‡Needed ulltrosound-guided percutaneous puncture drainage.
The most important step of EFTR with pure NOTES is the successful closure of the gastric wall opening after resection. Multiple metallic clips and endoloop and over-the-scope clips have been used for successful closure.29-31 These studies showed the possibility of performing endoscopic resection without the need for laparoscopy. However, appropriate indication (i.e., location and size of the subepithelial tumor), details of procedures (i.e., resection and closure methods), and other management requirements for patients (i.e., pre- and post-management) should be studied before widely using pure NOTES for subepithelial tumors.
Hybrid NOTES (combining NOTES with laparoscopic approach) is more acceptable than pure NOTES. Hybrid NOTES has been applied for gastric subepithelial tumors and early gastric cancer (EGC). Hiki et al.32 developed a hybrid NOTES procedure called laparoscopic and endoscopic cooperative surgery.33 The gastric wall was perforated using a needle knife from inside the stomach lumen after circumferential submucosal dissection. Seromuscular dissection and closure of the opening were performed using a laparoscopic procedure at the peritoneum. Two recent studies showed that laparoscopic and endoscopic cooperative surgeries for gastric subepithelial tumors (n=7 and n=20) were successful without complications.32,33
Endoscopic seromuscular incision (EFTR) was performed by Abe et al.34,35 After circumferential submucosal dissection, endoscopic full-thickness (from the muscle layer to the serosal layer) cut around three-fourths of the circumference of the above-mentioned submucosal incision was made under laparoscopic supervision. Complete resection and closure of the wall defect were performed by the laparoscopic approach from the peritoneal cavity. Abe et al.35 presented four cases of sub-endothelial tumors that were successfully resected using EFTR with laparoscopic assistance with no complications and minimal resection of healthy tissue. The mean size of the resected specimens and tumors was 37 mm and 30 mm, respectively. In this study, the advantage of EFTR over conventional laparoscopic wedge resection was the minimal resection of healthy tissue. Theoretically, EFTR with laparoscopic assistance can be used for lesions located near the EGJ or the pyloric ring because conventional laparoscopic wedge resection for these lesions is technically complex. Further investigations to evaluate the advantages of EFTR are needed.
EFTR can also be used to treat EGCs. Abe et al.34 first reported EFTR with laparoscopic assistance for EGC, followed by a prospective pilot study by Cho et al.36 Lymph node dissection including sentinel lymph node navigation was performed before EFTR. EFTR needed to be converted to subtotal gastrectomy in 5 of 14 EGCs because of issues with reconstruction, insufficient vascular flow after gastric wall closure, and leakage at the suture site. Although this study showed that EFTR was technically successful, two important barriers hinder its wide application for EGCs. First, the safety and effectiveness of sentinel lymph node biopsy should be confirmed. A recent multicenter, single-arm phase II study showed promising outcomes for sentinel lymph node biopsy in gastric cancer.37 Confirmation using randomized phase III studies is needed. Another barrier is the current EFTR technique because the gastric mucosa is exposed to the peritoneum, which could cause flow of gastric juice into the peritoneal cavity. The mucosal cancer is exposed and manipulated in the peritoneum from the open gastric wall incision. Therefore, it is difficult to completely prevent viable cancer cell seeding into the peritoneal cavity.
Developing a nonexposure technique is a possible solution. Recently, two nonexposure techniques have been developed. After laparoscopic circumferential seromuscular dissection from the peritoneal cavity, the tumor was resected endoscopically or using a stapler. The opening was sutured using a linear stapler or was hand-sewn.38,39 However, laparoscopic seromuscular hand-sewn suture and laparoscopic circumferential seromuscular dissection without perforation may not be easy. Intraoperative perforations occurred in 2 of 6 cases, and the mean operation time was 349 minutes in the first 3 cases and 198 minutes in the remaining 3 cases.39 Easier, safer, and more effective techniques may be needed.
Risks of Infection
Contamination of the peritoneal cavity is a big concern during NOTES procedures because an endoscope is passed through the unsterile upper gastrointestinal tract into the usually sterile peritoneal cavity. NOTES peritoneoscopy and intraperitoneal procedures (i.e., biopsy or organ extraction) need intraperitoneal navigation of the endoscope, and sterile methods may be needed for these procedures. In a randomized controlled study in a live porcine model, all non-sterile pigs (n=8) showed gross infection in the peritoneal cavity, including fibrinopurulent exudates, pus, and abscesses.40 The pigs in the non-sterile group underwent the procedure with non-sterile endoscopes and accessories, no antiseptic lavage of the gastric and oral cavities, and no antibiotics. On the other hand, all pigs in the sterile group demonstrated no gross evidence of intraperitoneal infection and negative cultures when samples were obtained from the peritoneal cavity.40 In another randomized study in a porcine model, the use of intravenous antibiotics with topical antimicrobial lavage of the mouth and stomach decreased the peritoneal bacterial load to almost zero, and this was associated with a significantly lower peritoneal infection rate than that with saline lavage.41
However, the extent of sterile methods needed is unclear. Aggressive maximal sterile techniques include disinfection of the stomach and oral cavity, and use of intravenous antibiotics, sterile endoscopes with sterile overtubes, and sterile gowns, gloves, and face masks.40 In a randomized study in pigs, excluding disinfection of the stomach and oral cavity, these techniques were not associated with postoperative clinically relevant infections, although bacterial contamination could occur.42 Moreover, excluding the sterilization of the oroesophageal overtube and decontamination of the stomach, these techniques were not associated with infectious complications in human trials, although these studies had a small number of participants (n=8 or n=10).43,44
Whether proton pump inhibitors (PPIs), which raise the gastric pH resulting in increased bacterial colonization of the stomach, increase the risk of peritoneal infection was not determined. In a rat model, pretreatment with a PPI resulted in a higher rate of peritoneal bacterial contamination (PPI vs. control; 60% vs. 20%) and abscess formation (33% vs. 13%).45 On the other hand, leakage of gastric juice into the peritoneum leads to chemical peritonitis. In a pig model, an aggressive sterile technique using PPI demonstrated no gross or bacteriological evidence of infection.40
The infection risk with POEM and EFTR seems to be lower than that with NOTES peritoneoscopy because the endoscope does not navigate the sterile peritoneum or mediastinum in POEM and EFTR. No penetration of endoscope occurs during procedure, with only the insulated-tip knife penetrating the gastric and esophageal walls. In addition, the insulated tip knife does not make contact with the peritoneal or mediastinal organs. In fact, the clinical outcomes of recent POEM and EFTR studies have shown no significant infection, although antibiotics may be needed in the pre- or post-procedures.12-17,29-31
Therefore, I assume that infection is not an obstacle to the use of NOTES in the upper gastrointestinal tract if appropriate disinfection is performed for each procedure.
Conclusions
Various transgastric NOTES procedures such as periotoneoscopy, cholecystectomy, and appendectomy have been investigated in humans. However, transgastric NOTES procedures have not been used widely because of its obscure benefits and roles. On the other hand, POEM has several advantages, and recent studies on POEM show good outcomes without serious complications. EFTR is a developing technology, and previous data on its use with pure or hybrid NOTES techniques indicate that it may be a feasible treatment method for subepithelial tumors. Favorable outcomes for EFTR are anticipated in the future.
Acknowledgments
This work was supported by grant 1210270 from the National Cancer Center, Korea.
References
- 1.Santos BF, Hungness ES. Natural orifice translumenal endoscopic surgery: progress in humans since white paper. World J Gastroenterol. 2011;17:1655–1665. doi: 10.3748/wjg.v17.i13.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalloo AN, Singh VK, Jagannath SB, Niiyama H, Hill SL, Vaughn CA, et al. Flexible transgastric peritoneoscopy: a novel approach to diagnostic and therapeutic interventions in the peritoneal cavity. Gastrointest Endosc. 2004;60:114–117. doi: 10.1016/s0016-5107(04)01309-4. [DOI] [PubMed] [Google Scholar]
- 3.Rattner DW, Hawes R, Schwaitzberg S, Kochman M, Swanstrom L. The Second SAGES/ASGE White Paper on natural orifice transluminal endoscopic surgery: 5 years of progress. Surg Endosc. 2011;25:2441–2448. doi: 10.1007/s00464-011-1605-5. [DOI] [PubMed] [Google Scholar]
- 4.Hazey JW, Narula VK, Renton DB, Reavis KM, Paul CM, Hinshaw KE, et al. Natural-orifice transgastric endoscopic peritoneoscopy in humans: initial clinical trial. Surg Endosc. 2008;22:16–20. doi: 10.1007/s00464-007-9548-6. [DOI] [PubMed] [Google Scholar]
- 5.Salinas G, Saavedra L, Agurto H, Quispe R, Ramírez E, Grande J, et al. Early experience in human hybrid transgastric and transvaginal endoscopic cholecystectomy. Surg Endosc. 2010;24:1092–1098. doi: 10.1007/s00464-009-0733-7. [DOI] [PubMed] [Google Scholar]
- 6.Kaehler G, Schoenberg MB, Kienle P, Post S, Magdeburg R. Transgastric appendicectomy. Br J Surg. 2013;100:911–915. doi: 10.1002/bjs.9115. [DOI] [PubMed] [Google Scholar]
- 7.von Renteln D, Gutmann TE, Schmidt A, Vassiliou MC, Rudolph HU, Caca K. Standard diagnostic laparoscopy is superior to NOTES approaches: results of a blinded, randomized controlled porcine study. Endoscopy. 2012;44:596–604. doi: 10.1055/s-0031-1291790. [DOI] [PubMed] [Google Scholar]
- 8.Sumiyama K, Gostout CJ, Rajan E, Bakken TA, Knipschield MA. Transesophageal mediastinoscopy by submucosal endoscopy with mucosal flap safety valve technique. Gastrointest Endosc. 2007;65:679–683. doi: 10.1016/j.gie.2006.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Yoshizumi F, Yasuda K, Kawaguchi K, Suzuki K, Shiraishi N, Kitano S. Submucosal tunneling using endoscopic submucosal dissection for peritoneal access and closure in natural orifice transluminal endoscopic surgery: a porcine survival study. Endoscopy. 2009;41:707–711. doi: 10.1055/s-0029-1214959. [DOI] [PubMed] [Google Scholar]
- 10.Lee CK, Lee SH, Chung IK, Lee TH, Lee SH, Kim HS, et al. Human diagnostic transgastric peritoneoscopy with the submucosal tunnel technique performed with the patient under conscious sedation (with video) Gastrointest Endosc. 2010;72:889–891. doi: 10.1016/j.gie.2010.01.035. [DOI] [PubMed] [Google Scholar]
- 11.Teoh AY, Chiu PW, Chan SM, Wong TC, Lau JY, Ng EK. Direct incision versus submucosal tunneling as a method of creating transgastric accesses for natural orifice transluminal endoscopic surgery (NOTES) peritoneoscopy: randomized controlled trial. Dig Endosc. 2013;25:281–287. doi: 10.1111/j.1443-1661.2012.01390.x. [DOI] [PubMed] [Google Scholar]
- 12.Inoue H, Ikeda H, Hosoya T, Onimaru M, Yoshida A, Eleftheriadis N, et al. Submucosal endoscopic tumor resection for subepithelial tumors in the esophagus and cardia. Endoscopy. 2012;44:225–230. doi: 10.1055/s-0031-1291659. [DOI] [PubMed] [Google Scholar]
- 13.Gong W, Xiong Y, Zhi F, Liu S, Wang A, Jiang B. Preliminary experience of endoscopic submucosal tunnel dissection for upper gastrointestinal submucosal tumors. Endoscopy. 2012;44:231–235. doi: 10.1055/s-0031-1291720. [DOI] [PubMed] [Google Scholar]
- 14.Lee SH, Kim SJ, Lee TH, Chung IK, Park SH, Kim EO, et al. Human applications of submucosal endoscopy under conscious sedation for pure natural orifice transluminal endoscopic surgery. Surg Endosc. 2013;27:3016–3020. doi: 10.1007/s00464-013-2844-4. [DOI] [PubMed] [Google Scholar]
- 15.Wang L, Ren W, Zhang Z, Yu J, Li Y, Song Y. Retrospective study of endoscopic submucosal tunnel dissection (ESTD) for surgical resection of esophageal leiomyoma. Surg Endosc. 2013;27:4259–4266. doi: 10.1007/s00464-013-3035-z. [DOI] [PubMed] [Google Scholar]
- 16.Liu BR, Song JT, Kong LJ, Pei FH, Wang XH, Du YJ. Tunneling endoscopic muscularis dissection for subepithelial tumors originating from the muscularis propria of the esophagus and gastric cardia. Surg Endosc. 2013;27:4354–4359. doi: 10.1007/s00464-013-3023-3. [DOI] [PubMed] [Google Scholar]
- 17.Ye LP, Zhang Y, Mao XL, Zhu LH, Zhou X, Chen JY. Submucosal tunneling endoscopic resection for small upper gastrointestinal subepithelial tumors originating from the muscularis propria layer. Surg Endosc. 2013 doi: 10.1007/s00464-013-3197-8. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 18.Chuah SK, Chiu CH, Tai WC, Lee JH, Lu HI, Changchien CS, et al. Current status in the treatment options for esophageal achalasia. World J Gastroenterol. 2013;19:5421–5429. doi: 10.3748/wjg.v19.i33.5421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ortega JA, Madureri V, Perez L. Endoscopic myotomy in the treatment of achalasia. Gastrointest Endosc. 1980;26:8–10. doi: 10.1016/s0016-5107(80)73249-2. [DOI] [PubMed] [Google Scholar]
- 20.Pasricha PJ, Hawari R, Ahmed I, Chen J, Cotton PB, Hawes RH, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy. 2007;39:761–764. doi: 10.1055/s-2007-966764. [DOI] [PubMed] [Google Scholar]
- 21.Inoue H, Minami H, Kobayashi Y, Sato Y, Kaga M, Suzuki M, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 22.Kurian AA, Dunst CM, Sharata A, Bhayani NH, Reavis KM, Swanström LL. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc. 2013;77:719–725. doi: 10.1016/j.gie.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 23.Von Renteln D, Fuchs KH, Fockens P, Bauerfeind P, Vassiliou MC, Werner YB, et al. Peroral endoscopic myotomy for the treatment of achalasia: an international prospective multicenter study. Gastroenterology. 2013;145:309–311.e1-3. doi: 10.1053/j.gastro.2013.04.057. [DOI] [PubMed] [Google Scholar]
- 24.Richards WO, Torquati A, Holzman MD, Khaitan L, Byrne D, Lutfi R, et al. Heller myotomy versus Heller myotomy with Dor fundoplication for achalasia: a prospective randomized double-blind clinical trial. Ann Surg. 2004;240:405–412. doi: 10.1097/01.sla.0000136940.32255.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Falkenback D, Johansson J, Oberg S, Kjellin A, Wenner J, Zilling T, et al. Heller's esophagomyotomy with or without a 360 degrees floppy Nissen fundoplication for achalasia. Long-term results from a prospective randomized study. Dis Esophagus. 2003;16:284–290. doi: 10.1111/j.1442-2050.2003.00348.x. [DOI] [PubMed] [Google Scholar]
- 26.Ujiki MB, Yetasook AK, Zapf M, Linn JG, Carbray JM, Denham W. Peroral endoscopic myotomy: a short-term comparison with the standard laparoscopic approach. Surgery. 2013;154:893–897. doi: 10.1016/j.surg.2013.04.042. [DOI] [PubMed] [Google Scholar]
- 27.Bhayani NH, Kurian AA, Dunst CM, Sharata AM, Rieder E, Swanstrom LL. A comparative study on comprehensive, objective outcomes of laparoscopic heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg. 2013 doi: 10.1097/SLA.0000000000000268. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Hungness ES, Teitelbaum EN, Santos BF, Arafat FO, Pandolfino JE, Kahrilas PJ, et al. Comparison of perioperative outcomes between peroral esophageal myotomy (POEM) and laparoscopic Heller myotomy. J Gastrointest Surg. 2013;17:228–235. doi: 10.1007/s11605-012-2030-3. [DOI] [PubMed] [Google Scholar]
- 29.Schlag C, Wilhelm D, von Delius S, Feussner H, Meining A. EndoResect study: endoscopic full-thickness resection of gastric subepithelial tumors. Endoscopy. 2013;45:4–11. doi: 10.1055/s-0032-1325760. [DOI] [PubMed] [Google Scholar]
- 30.Shi Q, Chen T, Zhong YS, Zhou PH, Ren Z, Xu MD, et al. Complete closure of large gastric defects after endoscopic full-thickness resection, using endoloop and metallic clip interrupted suture. Endoscopy. 2013;45:329–334. doi: 10.1055/s-0032-1326214. [DOI] [PubMed] [Google Scholar]
- 31.Zhou PH, Yao LQ, Qin XY, Cai MY, Xu MD, Zhong YS, et al. Endoscopic full-thickness resection without laparoscopic assistance for gastric submucosal tumors originated from the muscularis propria. Surg Endosc. 2011;25:2926–2931. doi: 10.1007/s00464-011-1644-y. [DOI] [PubMed] [Google Scholar]
- 32.Hiki N, Yamamoto Y, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, et al. Laparoscopic and endoscopic cooperative surgery for gastrointestinal stromal tumor dissection. Surg Endosc. 2008;22:1729–1735. doi: 10.1007/s00464-007-9696-8. [DOI] [PubMed] [Google Scholar]
- 33.Tsujimoto H, Yaguchi Y, Kumano I, Takahata R, Ono S, Hase K. Successful gastric submucosal tumor resection using laparoscopic and endoscopic cooperative surgery. World J Surg. 2012;36:327–330. doi: 10.1007/s00268-011-1387-x. [DOI] [PubMed] [Google Scholar]
- 34.Abe N, Mori T, Takeuchi H, Ueki H, Yanagida O, Masaki T, et al. Successful treatment of early stage gastric cancer by laparoscopy-assisted endoscopic full-thickness resection with lymphadenectomy. Gastrointest Endosc. 2008;68:1220–1224. doi: 10.1016/j.gie.2008.02.077. [DOI] [PubMed] [Google Scholar]
- 35.Abe N, Takeuchi H, Yanagida O, Masaki T, Mori T, Sugiyama M, et al. Endoscopic full-thickness resection with laparoscopic assistance as hybrid NOTES for gastric submucosal tumor. Surg Endosc. 2009;23:1908–1913. doi: 10.1007/s00464-008-0317-y. [DOI] [PubMed] [Google Scholar]
- 36.Cho WY, Kim YJ, Cho JY, Bok GH, Jin SY, Lee TH, et al. Hybrid natural orifice transluminal endoscopic surgery: endoscopic full-thickness resection of early gastric cancer and laparoscopic regional lymph node dissection--14 human cases. Endoscopy. 2011;43:134–139. doi: 10.1055/s-0030-1255955. [DOI] [PubMed] [Google Scholar]
- 37.Kitagawa Y, Takeuchi H, Takagi Y, Natsugoe S, Terashima M, Murakami N, et al. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol. 2013;31:3704–3710. doi: 10.1200/JCO.2013.50.3789. [DOI] [PubMed] [Google Scholar]
- 38.Inoue H, Ikeda H, Hosoya T, Yoshida A, Onimaru M, Suzuki M, et al. Endoscopic mucosal resection, endoscopic submucosal dissection, and beyond: full-layer resection for gastric cancer with nonexposure technique (CLEAN-NET) Surg Oncol Clin N Am. 2012;21:129–140. doi: 10.1016/j.soc.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 39.Mitsui T, Niimi K, Yamashita H, Goto O, Aikou S, Hatao F, et al. Non-exposed endoscopic wall-inversion surgery as a novel partial gastrectomy technique. Gastric Cancer. 2013 doi: 10.1007/s10120-013-0291-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Giday SA, Dray X, Magno P, Buscaglia JM, Shin EJ, Surti VC, et al. Infection during natural orifice transluminal endoscopic surgery: a randomized, controlled study in a live porcine model. Gastrointest Endosc. 2010;71:812–816. doi: 10.1016/j.gie.2009.11.037. [DOI] [PubMed] [Google Scholar]
- 41.Eickhoff A, Vetter S, von Renteln D, Caca K, Kähler G, Eickhoff JC, et al. Effectivity of current sterility methods for transgastric NOTES procedures: results of a randomized porcine study. Endoscopy. 2010;42:748–752. doi: 10.1055/s-0030-1255597. [DOI] [PubMed] [Google Scholar]
- 42.Azadani A, Jonsson H, Park PO, Bergström M. A randomized trial comparing rates of abdominal contamination and postoperative infection among natural orifice transluminal endoscopic surgery, laparoscopic surgery, and open surgery in pigs. Gastrointest Endosc. 2012;75:849–855. doi: 10.1016/j.gie.2011.11.039. [DOI] [PubMed] [Google Scholar]
- 43.Narula VK, Happel LC, Volt K, Bergman S, Roland JC, Dettorre R, et al. Transgastric endoscopic peritoneoscopy does not require decontamination of the stomach in humans. Surg Endosc. 2009;23:1331–1336. doi: 10.1007/s00464-008-0161-0. [DOI] [PubMed] [Google Scholar]
- 44.Nikfarjam M, McGee MF, Trunzo JA, Onders RP, Pearl JP, Poulose BK, et al. Transgastric natural-orifice transluminal endoscopic surgery peritoneoscopy in humans: a pilot study in efficacy and gastrotomy site selection by using a hybrid technique. Gastrointest Endosc. 2010;72:279–283. doi: 10.1016/j.gie.2010.03.1070. [DOI] [PubMed] [Google Scholar]
- 45.Ramamoorthy SL, Lee JK, Mintz Y, Cullen J, Savu MK, Easter DW, et al. The impact of proton-pump inhibitors on intraperitoneal sepsis: a word of caution for transgastric NOTES procedures. Surg Endosc. 2010;24:16–20. doi: 10.1007/s00464-009-0559-3. [DOI] [PubMed] [Google Scholar]


