Abstract
A long-term indwelling urinary catheter intervention was tested in a randomized trial that is described in this article. The perceived value of the intervention to the catheter users, one of the study’s specific aims, was assessed at the end of their 12-month participation and is reported here. Study participants’ responses, our findings, and implications for home healthcare are discussed.
Introduction and Purpose of the Study
There is limited evidence to guide long-term urinary catheter users for self-management. They ordinarily are not in support groups of any sort and might not know others using such a device, yet many use an indwelling urinary catheter (suprapubic or urethral) for years (Wilde et al., 2013) or indefinitely. Those with intractable urinary retention who are unable to perform intermittent catheterization or have no one to do it are sometimes without other options. This type of urinary retention is most often caused by a neurologically based injury or disease, such as a spinal cord injury, multiple sclerosis, diabetes, or by obstructive prostate disease (Cottenden et al., 2013). In our experience, individuals with long-term catheters often learn about self-managing through piecemeal instruction from healthcare providers and by trial and error.
This report describes a new intervention to teach self-management to community-living long-term indwelling urinary catheter users and their perceived value of the intervention. Understanding how the study participants responded provides information that could be useful in dissemination and/or changes in the research.
Background and Literature Review
Although policies and procedures are well developed for patients with indwelling urinary catheters in home care and in clinics, an emphasis on self-management is not the norm. Self-management is a form of collaborative care with a healthcare provider (nurse or physician) in which the patient learns to pay attention to bodily symptoms, makes observations and recordings (e.g., diaries), and determines how behavioral changes they are making affect the condition. Self-management research is often conducted with people having chronic conditions, such as arthritis (Ackerman et al., 2013), diabetes (Rothman et al., 2008), or asthma (Kaptein et al., 2010), but self-management research has not been done in indwelling urinary catheter users.
The National Home and Hospice Care Study conducted in 2000 by U.S. National Center for Health Statistics estimated that there are 148,400 urinary catheter users in the United States, for a prevalence of 0.05% in the adult population in community settings (CDC, 2013a). A more recent National Home and Hospice Care Survey in 2007 reported catheter prevalence in home care (excluding hospice) at 9% (n = 4683) (CDC, 2013b) or 135,000 people with catheters of the 1.5 million home care patients in 2007 (http://www.cdc.gov/nchs/fastats/homehealthcare.htm). However, it is not known how many of them have long-term catheters nor whether they use indwelling or nonindwelling catheters (Lisa Dwyer, National Center for Health Statistics, personal communication, June 20, 2013).
Persistent catheter-related problems are common in long-term catheter users. In one recent study of 43 people over an 8-month period, 74% experienced blockage of the catheter from encrustations, 70% had catheter-associated urinary tract infection (CAUTI), 79% had leakage of urine (bypassing), and 33% had accidental dislodgement (Wilde et al., 2010). In a larger study with 202 long-term indwelling urinary catheter users, catheter problems were recorded by recall for the previous 2-month period, and in this short period of time, 31% had experienced CAUTI, 24% had blockage, 12% had accidental dislodgment, 43% had leakage of urine, and 23% had catheter-associated pain (Wilde et al., 2013).
Most research in the past has focused on improving the catheter itself through: coatings, such as silver or antibiotic (Johnson et al., 2006), catheter materials like silicone (Schumm & Lam, 2008), instillations into the drainage bag (Washington, 2001), and special care to the urinary meatus (Burke et al., 1983), but none have proven effective in preventing blockage or CAUTI (Parker et al., 2009). Other interventions, commonly believed to be of value, such as smaller catheter size, cranberry juice consumption (Jepson & Craig, 2008), and acidic instillations or irrigations, have not been tested in randomized controlled trials in people with catheters (Moore et al., 2009). Closed drainage, which has been shown to significantly reduce the rate of CAUTI, is the only critical innovation in the last 40 years to prove beneficial (Stickler & Feneley, 2010). However, many persons with catheters open them daily to switch from leg to night bags or to clean the bags between uses. In the aforementioned larger study of 202 long-term catheter users, 58% used both leg and overnight bags, and a majority cleaned their bags, using water, soap and water, or a solution of water with bleach or vinegar (Wilde et al., 2013). Cleaning with a diluted bleach solution was shown in a seminal study to increase bag life to 1 month; however, rates of CAUTI remained unchanged (Dille et al., 1993). Consumption of a citrated drink (water with lemon juice) or additional fluids was tested in one study, and results are promising that either can decrease catheter blockage (Khan et al., 2010), but trials have not been done. Thus, evidence-based self-management strategies for persons using indwelling urinary catheters remain in a preliminary stage.
A first step for catheter users to prevent or minimize catheter-related problems (e.g., CAUTI, blockage, or accidental dislodgement) is to become aware of what to notice and how to self-monitor urine flow. Strategies can then be selected for self-managing the catheter based on this knowledge to address problems early to prevent more serious complications, such as an insidious CAUTI requiring intravenous antibiotics and hospitalization.
Study Description
A research study was conducted, building on the prior investigations. A new catheter self-management educational intervention was piloted (Wilde & Brasch, 2008a, 2008b) and tested for effectiveness in a randomized clinical trial in long-term indwelling urinary catheter users. The 4-year study was conducted in one northeastern U.S. state, including a large city and a mix of urban/suburban and rural areas. Two hundred and two adult persons with long-term indwelling catheters (56% urethral and 44% suprapubic) who were expecting to use catheters indefinitely, or at least for a year, were enrolled in the study for 12 months. Equal numbers of 101 were assigned to the intervention group or the control group. One hundred seventy-five study participants (87%) were recruited through home care agencies (one large city agency enrolled 152 persons); the rest were referred through a combination of clinics or private urological offices. Approximately equal numbers of men and women were enrolled, aged 19 to 96 years (mean 61, SD 17.4), with racial and ethnic diversity (White 57%, Black 30%, other races 13%).
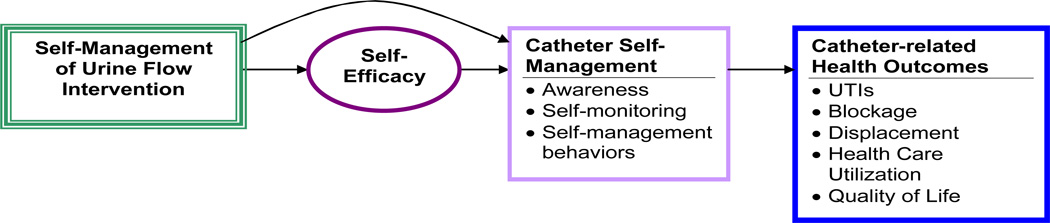
The self-management intervention was theoretically based on Bandura’s self-efficacy theory (Bandura, 1997). Self-efficacy is the confidence to perform a specific behavior and, in this study, optimal and consistent levels of fluid intake and preventing accidental dislodgment were the key behaviors targeted. Study participants were taught to pay attention to urine flow, self-monitor bodily changes, and choose appropriate self-management behaviors. The theoretical concepts of awareness, self-monitoring, and self-management (Wilde & Garvin, 2007) were central to the intervention, and Stanford’s Chronic Disease Self-management program (Lorig et al., 2001) provided the overall model (Figure 1). The intervention was designed to enhance self-management of urine flow in the intervention group. The control group received only their usual care.
Figure 1.
Theoretical Model of the Study. UTI = urinary tract infection.
Study outcomes were: (a) catheter-related complications (CAUTI, catheter blockage, and accidental dislodgement), (b) complications’ associated costs, and (c) quality of life. To measure study outcomes, data were collected from both groups about catheter-related problems for a year, once face to face in their homes when enrolled and then in six follow-up bimonthly telephone interviews with trained interviewers.
The intervention group was visited by a study nurse in their home three times, for a total of three home visits. Two of them occurred in the first month. The first home visit was to teach about self-monitoring using a urinary diary, and the second home visit was to use this information to plan for improved self-management and to introduce an educational booklet. This was followed by one phone call 2 weeks later to identify any additional issues and to reinforce the teaching. The third home visit was a “booster” of the intervention at 4 months to further refine teaching.
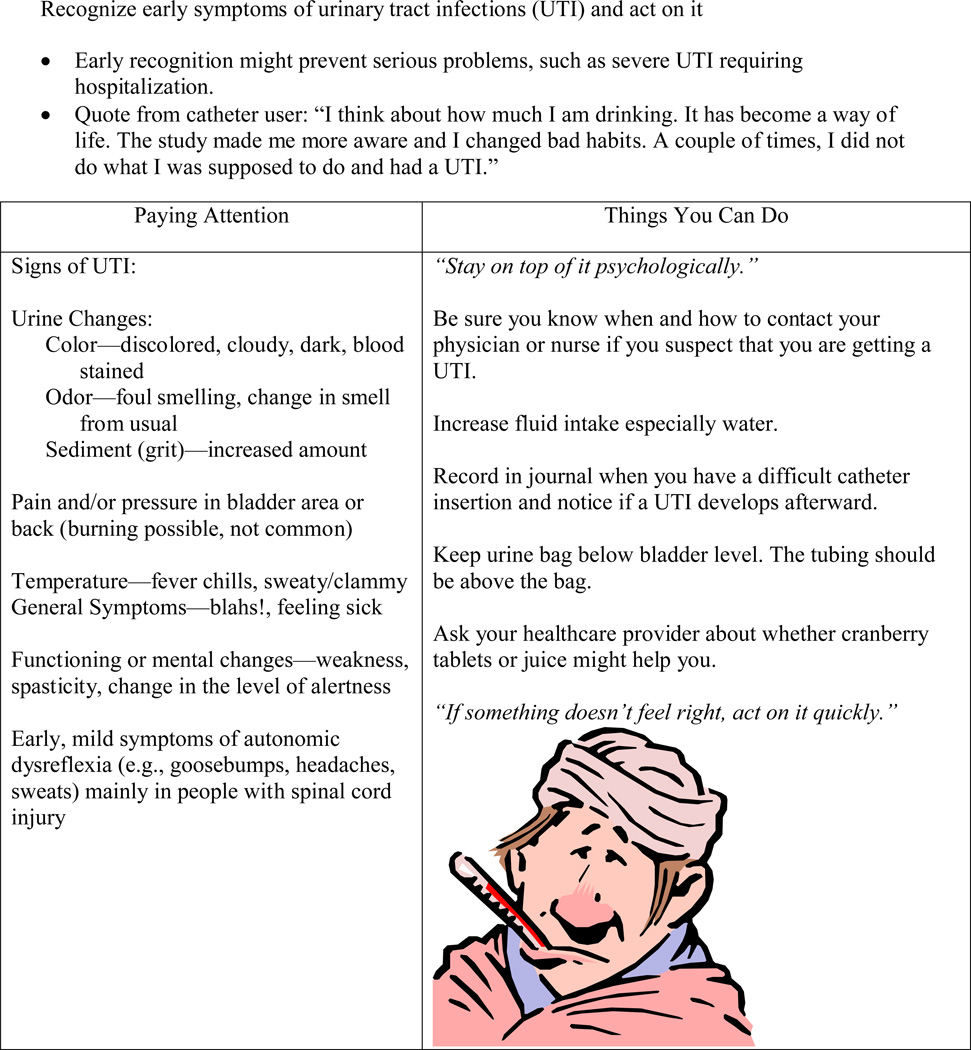
Specifically, study participants were taught to increase their awareness of sensations of urine flow and to learn how these change with daily activities or catheter-related problems. Problem areas were identified in conjunction with information from the 3-day urinary diary (intake and output and open-ended journal). After learning about basic catheter self-management (Table 1 from the Paying Attention Educational Booklet), all were taught to pay attention to fluid intake and catheter position to prevent dislodgement. Then the study nurse reviewed all sections of the educational booklet, focusing on areas of individual interest (Table 2 and Figure 2). The study nurse filled out forms after each encounter, which were similar to a care plan, to remind her of the participant’s catheter problems and interests or goals. Whenever possible, measurable goals were set and written into the educational booklet.
Table 1.
Basic Catheter Self-Management
|
|
Table 2.
Quick Guide to Catheter Problems (from the Paying Attention Educational Booklet)
| Problem | Action Strategies |
|---|---|
| Decreased/inconsistent fluid intake | Increase fluid intake |
| Urinary tract infection | Increase fluid intake Recognize early symptoms of urinary tract infection and act on it |
| Catheter blocks | Increase fluid intake Promote catheter changes at best intervals |
| Adjustment to living with a catheter | Approaches for living with a catheter |
| Not sure of the best schedule for catheter changes | Promote catheter changes at best intervals |
| Kinks, twists, or tugs on catheter | Prevent kinks, twists, or tugs on catheter |
| Too much caffeine | Decrease caffeine |
| Catheter leaks | Decrease catheter leakage Empty urine bag |
| Urine bag odor | Clean urine drainage bag |
| Changes with sex | Make adjustments for sexual activity |
Figure 2.
Sample of educational module (Note: the quotes are from previous study participants (Wilde & Brasch, 2008a, 2008b).1 UTI = urinary tract infection.
Below is a report of one of the specific aims of this study, to describe the perceived value of the self-management intervention received by the intervention group. A full report of the main outcomes for this research will be published elsewhere.
Perceived Value of the Catheter Self-Management Program
Methods
Study participants who received the catheter self-management intervention were contacted by phone by one of the two study coordinators within a month of their year-long study participation to assess their perceived value of the intervention. Not everyone was able to be reached or was not able to be interviewed; therefore, out of the 74 persons who completed the intervention arm of the study, 60 brief telephone interviews were conducted. Study participants were asked several quantitative questions about helpfulness of each component of the intervention, using a modification of items previously piloted (Wilde & Brasch, 2008a, 2008b), on a scale of 1 to 10, with 1 being not helpful at all and 10 being very helpful. Study participants were also asked five open-ended questions, allowing for comments to be shared, related: (a) goals, (b) changes to behavior, (c) impact on self-management, (d) helpfulness of the program, and (e) suggestions for improving the program. The interviewers took brief notes to obtain the comments data, which were entered into a spreadsheet and SPSS.
Data Analysis
Quantitative items were analyzed descriptively for means and standard deviations. For the comments data, a descriptive analysis was conducted using simple coding by two researchers, the principal investigator and a doctoral student. Coded comments were then organized into tables before writing a descriptive summary of responses for each item. Both coders agreed on the final codes, the organization of data, and the summary.
Results
Based on the scores, the study nurse visits and the intake and output part of the urinary diary were the most favored elements of the intervention (Table 3). A large majority of the persons rated each component of the intervention (i.e., intake and output, journal, educational booklet, study nurse encounters, and learning self-management) between 8 and 10 on the 10-point scale. The means (SD) for each component ranged from 7.25 (2.40) to 8.33 (3.15). The open-ended journal, which was identified in the study nurses’ process recordings (not reported in this article) as being used by only 2% of the intervention sample, was valued less with the lowest mean score 7.25 (3.15).
Table 3.
Helpfulness of the Self-Management Program Components
| On a scale of 1–10, With 1 Being Almost No Help, and 10 Meaning It Was a Very Big Help |
n | M | SDs | 1–4 | 5–7 | 8–10 |
|---|---|---|---|---|---|---|
| 1. Intake and output | 56 | 8.04 | 2.40 | 11% | 12% | 77% |
| 2. Catheter journal | 56 | 7.25 | 3.15 | 20% | 14% | 66% |
| 3. Educational booklet | 57 | 7.72 | 2.79 | 12% | 19% | 68% |
| 4. Study nurse’s home visits and TC | 58 | 8.33 | 2.53 | 10% | 12% | 78% |
| 5. How helpful was learning self-management | 60 | 8.18 | 2.65 | 10% | 18% | 63% |
Out of the 60 persons interviewed, goals were recalled by 21 persons (35%), not set by 36 (60%), and 3 (5%) did not remember. Responses to whether they were doing anything differently with the catheter because of the study were: 25 (42%) said no, 18 (30%) said yes somewhat, and 17 (28%) said yes greatly. 43 (71%) had suggestions for improving the program and 17 (29%) did not.
Goals Set During the Study
Fifteen persons had goals related to hygiene or preventing urinary tract infections (UTI), specifically cleaning near the catheter, drinking adequate fluids, and preventing UTI. Self-monitoring goals by 14 persons involved noticing changes in the urine, such as watching for sediment or urine color, or in paying attention to the catheter to maintain an appropriate position, or prevent dislodgment, kinks/twists, or leaks. Two persons also stated they wanted to stay healthy urologically.
Changes to Behavior
Study participants who had said they were doing things differently because of the study were asked to describe in what ways. Some reported changes that were similar to the goals they cited. Self-monitoring of the catheter was identified by nine persons related to repositioning the catheter to prevent leakage and twists, or checking the catheter position in relation to the bag or body; or watching for changes in the urine, sediment, or color. Eight said they paid attention more often to urine output or to avoid letting the bag get too full. Nine said they have increased their fluid intake and two said they keep better track of fluids. Eleven were focused more on the catheter itself, such as knowing the exact amount of water in the balloon, about irrigation or cleaning the bag, changing the catheter more often, and in managing the catheter when traveling by using a larger bag at home and smaller one for travelling, or knowing the locations of available bathrooms. Two stated they knew better when to call the provider for catheter problems. One worked on bowel management more and one stays away from caffeine. One reported fewer UTIs.
Impact on Self-Management
Participants also were asked how the study affected their catheter self-management. Six said they were more aware in relation to: cleaning the catheter, noticing urine color, emptying the bag to prevent urine buildup, and knowing where bathrooms were. Six reported having fewer UTIs, and two had less sediment, blockage, or mucus. One individual had more catheter comfort and was pain-free. Five people spoke of being more knowledgeable about and supported with the catheter, or knew when to call the provider. A few recognized patterns of problems, such as burning sensations and kinks. One noted being hospitalized four times recently (but we are not sure what that meant).
Helpfulness of the Program
The comments related to whether learning self-management was helpful or not were aimed at understanding more about the value of the catheter self-management intervention. Comments from 17 individuals were primarily about catheter-related knowledge gained, skills acquisition (including enhanced awareness of their bodily symptoms related to the catheter), and feeling cared for by the study nurse making home visits. There were just four negative comments: three who did not learn anything new and one who did not think program helped. Also three persons said they do not self-mange, but one said it was helpful to know.
Suggestions for Improving the Self-Management Program
Many suggestions and comments were received also, including more use of Web sites, combining the urinary diary forms (i.e., intake and output forms with the journal), managing pain, and sketches of instructions. Several asked for better designed catheters and equipment.
Discussion
For the quantitative assessment of intervention components, there was a possible small ceiling effect with higher percentages reporting 10 (very helpful) for the study nurse encounters and intake and output, by 41% and 32% of the sample respectively. The open-ended journal was not used by most study participants (2%) and this was the case also during the pilot study (Wilde & Brasch, 2008a, 2008b), and thus it should probably be eliminated from future tests of this intervention.
The information solicited about goals at the end of this 12-month intervention with 60 individuals is in stark contrast to the information collected by the study nurses in their process forms in which 82 persons set initial goals (81% of 101 in the self-management intervention group), and over 70% said they met their goals during the phone call in month 2 or the home visit in month 4. Perhaps goal setting was not a high priority or there was insufficient recall at 12 months, when so much time had passed after the intervention visits. However, those persons who did set goals used language to reflect the key components taught in the intervention, such as goals about fluid intake, preventing UTI, and noticing changes in urine or in the position of the catheter.
Intervention participants showed that they understood key study concepts because they described activities that demonstrated awareness, self-monitoring, and self-management related to fluid intake, preventing CAUTI, and proper positioning of the catheter. Some seemed to have an emotional connection with the study nurse, saying they felt “cared for” by her. A few said that no one else has talked with them like this about the catheter and in such depth, and this made them feel valued as persons. Responses also illustrated individual variation in how much the self-management intervention was liked and for what reasons.
Implications for Practice
Long-term indwelling catheter users can be taught to pay attention to urine flow. Specifically they should know how much fluid intake is right for them and what types of fluids should be monitored (e.g., caffeine). By noticing catheter-related changes—such as the color or character of the urine, catheter position, or kinks/twists in the tubing—and by responding quickly, catheter-related problems might be avoided or minimized. In this study, catheter users’ comments indicated how they valued and learned from the self-management intervention. Home care nurses are in an important and unique position to partner with their patients with catheters and their families to improve care and quality of life.
Conclusion
This may be the first self-management intervention in long-term indwelling urinary catheter users. Knowing how the study participants responded to the intervention is critical in determining its dissemination and overall research value. In summary, research participants seemed to like the intervention, were able to identify what they should pay attention to, and told us what they were doing differently related to their catheter. These new behaviors should be beneficial in their catheter-related health. Although this intervention is not ready yet for full dissemination—due to ongoing analysis and writing reports of the main study results—many of the components, such as the urinary diary (I and O), the basic self-management tips in Table 1, and the sample educational page on identifying UTI, could be useful for home care nurses teaching catheter self-management to long-term indwelling urinary catheter users.
Acknowledgments
Funding by National Institute of Nursing Research, National Institutes of Health (U.S.) #R01 NR01553.
Footnotes
Study Nurses: Paula Wilson, RN, BSN, MPH (VNSNY) and Margaret Lash, RN, MS (Rochester); also at Visiting Nurse Service of New York: Penny Feldman, PhD, Seon Lewis-Holman RN, MS-C; Yanick Martelly-Kebreau, RN, MS, CWOCN.
The authors declare no conflicts of interest.
Contributor Information
Mary Wilde, University of Rochester, Rochester, New York..
Feng Zhang, University of Rochester, Rochester, New York..
Eileen Fairbanks, University of Rochester, Rochester, New York..
Shivani Shah, Center for Home Care Policy and Research, New York City, New York..
Margaret V. McDonald, Center for Home Care Policy and Research, New York City, New York.
Judith Brasch, University of Rochester, Rochester, New York..
References
- Ackerman IN, Buchbinder R, Osborne RH. Factors limiting participation in arthritis self-management programmes: An exploration of barriers and patient preferences within a randomized controlled trial. Rheumatology. 2013;52(3):472–479. doi: 10.1093/rheumatology/kes295. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: Freeman; 1997. [Google Scholar]
- Burke JP, Jacobson JA, Garibaldi RA, Conti MT, Alling DW. Evaluation of daily meatal care with poly-antibiotic ointment in prevention of urinary catheter-associated bacteriuria. Journal of Urology. 1983;129(2):331–334. doi: 10.1016/s0022-5347(17)52083-2. [DOI] [PubMed] [Google Scholar]
- CDC. National center for health statistics, NIH. The national home care study. [Accessed on April 24, 2013];2013a at http://www.cdc.gov/nchs/nhhcs.htm.
- CDC. National center for health statistics, NIH. The 2007 National Home and Hospice care Survey. [Accessed on July 1, 2013];2013b http://www.cdc.gov/nchs/nhhcs.htm, data from: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/NHHCS/2007)
- Cottenden A, Fader M, Wilde MH, Bliss D, Buckley B, Hayer D, et al., editors. Management Using Continence Products, Incontinence: 5th International Consultation on Incontinence. 5th ed. Arnheim, the Netherlands: ICUD-EAU; 2013. [Google Scholar]
- Dille CA, Kirchhoff KT, Sullivan JJ, Larson E. Increasing the wearing time of vinyl urinary drainage bags by decontamination with bleach. Archives of Physical Medicine and Rehabilitation. 1993;74(4):431–437. [PubMed] [Google Scholar]
- Jepson RG, Craig JC. Cranberries for preventing urinary tract infections. Cochrane Database of Systematic Reviews (Online) 2008;(1):CD001321. doi: 10.1002/14651858.CD001321.pub4. [DOI] [PubMed] [Google Scholar]
- Johnson JR, Kuskowski MA, Wilt TJ. Systematic review: Antimicrobial urinary catheters to prevent catheter-associated urinary tract infection in hospitalized patients. Annals of Internal Medicine. 2006;144(2):116–126. doi: 10.7326/0003-4819-144-2-200601170-00009. [DOI] [PubMed] [Google Scholar]
- Kaptein AA, Klok T, Moss-Morris R, Brand PL. Illness perceptions: Impact on self-management and control in asthma. Current Opinion in Allergy and Clinical Immunology. 2010;10(3):194–199. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- Khan A, Housami F, Melotti R, Timoney A, Stickler D. Strategy to control catheter encrustation with citrated drinks: A randomized crossover study. Journal of Urology. 2010;183(4):1390–1394. doi: 10.1016/j.juro.2009.12.024. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, et al. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Moore KN, Hunter KF, McGinnis R, Bacsu C, Fader M, Gray M, et al. Do catheter washouts extend patency time in long-term indwelling urethral catheters? A randomized controlled trial of acidic washout solution, normal saline washout, or standard care. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of the Wound, Ostomy and Continence Nurses Society/WOCN. 2009;36(1):82–90. doi: 10.1097/01.WON.0000345181.37656.de. [DOI] [PubMed] [Google Scholar]
- Parker D, Callan L, Harwood J, Thompson DL, Wilde M, Gray M. Nursing interventions to reduce the risk of catheter-associated urinary tract infection. Part 1: Catheter selection. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of the Wound, Ostomy and Continence Nurses Society/WOCN. 2009;36(1):23–34. doi: 10.1097/01.WON.0000345173.05376.3e. [DOI] [PubMed] [Google Scholar]
- Rothman RL, Mulvaney S, Elasy TA, VanderWoude A, Gebretsadik T, Shintani A, et al. Self-management behaviors, racial disparities, and glycemic control among adolescents with Type 2 diabetes. Pediatrics. 2008;121(4):e912–e919. doi: 10.1542/peds.2007-1484. [DOI] [PubMed] [Google Scholar]
- Schumm K, Lam T. Types of urethral catheters for management of short-term voiding problems in hospitalised adults. Cochrane Database of Systematic Reviews (Online) 2008;(2):CD004013. doi: 10.1002/14651858.CD004013.pub3. [DOI] [PubMed] [Google Scholar]
- Stickler DJ, Feneley RC. The encrustation and blockage of long-term indwelling bladder catheters: A way forward in prevention and control. Spinal Cord. 2010;48(11):784–790. doi: 10.1038/sc.2010.32. [DOI] [PubMed] [Google Scholar]
- Washington EA. Instillation of 3% hydrogen peroxide or distilled vinegar in urethral catheter drainage bag to decrease catheter-associated bacteriuria. Biological Research For Nursing. 2001;3(2):78–87. doi: 10.1177/109980040200300203. [DOI] [PubMed] [Google Scholar]
- Wilde MH, Brasch J. Teaching self-management to long-term urinary catheter users. International Journal of Urological Nursing. 2008a;2(2):62–71. [Google Scholar]
- Wilde MH, Brasch J. A pilot study of self-monitoring urine flow in people with long-term urinary catheters. Research in Nursing & Health. 2008b;31(5):490–500. doi: 10.1002/nur.20281. [DOI] [PubMed] [Google Scholar]
- Wilde MH, Brasch J, Getliffe K, Brown KA, McMahon JM, Smith JA, et al. Study on the use of long-term urinary catheters in community-dwelling individuals. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of the Wound, Ostomy and Continence Nurses Society/WOCN. 2010;37(3):301–310. doi: 10.1097/WON.0b013e3181d73ac4. [DOI] [PubMed] [Google Scholar]
- Wilde MH, Garvin S. A concept analysis of self-monitoring. Journal of Advanced Nursing. 2007;57(3):339–350. doi: 10.1111/j.1365-2648.2006.04089.x. [DOI] [PubMed] [Google Scholar]
- Wilde MH, McDonald MV, Brasch J, McMahon JM, Fairbanks E, Shah S, Scheid E. Long-term urinary catheter users self-care practices and problems. Journal of Clinical Nursing. 2013;22(3–4):356–367. doi: 10.1111/jocn.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]