Abstract
Background:
The aim of the present study was to determine the prevalence and prognosis of cerebrovascular accident (CVA) and its subtypes among Iranian patients with systemic lupus erythematosus (SLE).
Methods:
In a cross-sectional study, medical records of 575 SLE patients were reviewed. The patients developing CVA in their course of disease were extracted. In these patients, data about demographic features, lupus anti bodies, duration of the disease until CVA, CVA manifestation(s) and follow-up duration were gathered. In the next step, patients with any kinds of CVA were summoned to Neurology clinic to identify the grade of disability in each patient with CVA.
Results:
We identified 38 patients with CVA of which 6 (15.8%) were men and 32 (84.2%) were women. The most common subtype of CVA was small vessels thrombosis (21.05%) among the study patients and hemi paresis was the most prevalent initial presentation (39.47%). In 11 (28.9%) patients, SLE was initiated with CVA and in 3 (7.9%) patients CVA had happened in the 1st year of SLE. Anti-phospholipid antibodies (APLA) were positive in 29 (76.3%) patients. Mean modified Rankin Scale in patient with positive and negative serology for APLA was 0.93 ± 1.11 and 0.22 ± 0.66 respectively (P = 0.006).
Conclusions:
Our study shows that 6.6% of Iranian SLE patients have CVA during their course of the disease. Small vessels thrombosis is the most common CVA subtype and hemi paresis is the most prevalent initial presentation. Moreover, we showed that the prognosis of CVA in Iranian SLE patients is not unfavorable.
Keywords: Cerebrovascular accident, stroke, systemic lupus erythamatosus
INTRODUCTION
Systemic lupus erythematosus (SLE) is a chronic autoimmune disease of unknown cause which can affect several parts of the body even central nervous system (CNS).[1,2,3]. Among CNS manifestations, cerebrovascular accident (CVA) is one of the severe complications. Previous cohort studies revealed that 3-20% of SLE patients may experience an episode of CVA during their course of the disease.[4,5,6] Data about differential features and various subtypes of CVA in Iranian SLE patients are lacking. In this study, we aimed to determine the prevalence and prognosis of CVA and its subtypes among Iranian SLE patients.
METHODS
Patients and settings
This study was a cross-sectional hospital clinic-based study that performed in Isfahan, Iran. During the period of 1 year, since February 2010-2011, SLE patients attending the Rheumatology Clinic of Alzahra Hospital (a tertiary referral center in Isfahan, Iran) enrolled in the study. Their medical documents have been reviewed and patients who had developed acute CVA include of ischemic attack, hemorrhagic attack, cerebral vasculitis and cerebral vein thrombosis in their course of disease were extracted. Drug-induced vasculitis, generalized vasculopathy, transverse myelitis and loss of consciousness due to metabolic disorders were causes of exclusion.
In patients who enrolled the study demographic data, SLE related clinical and laboratory findings and neurological symptoms in the disease duration were recorded.
Diagnosis and assessment
SLE was diagnosed according to the revised criteria which suggested by American College of Rheumatology at 1997.[7] Stroke was diagnosed according to the World Health Organization definition.[8]
“Trial of Org 10172 in Acute Stroke Treatment” (TOAST) classification system was used to denote different subtypes of CVA.[9] Diagnosis was based on the clinical features and on data collected by brain imaging.
In patients with CVA, demographic features, history of hypertension, dyslipidemia and diabetes mellitus, anti-phospholipid antibodies (APLA), duration of the disease until CVA, CVA manifestation(s) and follow-up duration were extracted.
In the next step, patients with any kinds of CVA were summoned to neurology clinic to identify the grade of disability. The grade of disability of CVA determined for each patient through a precise neurological exam by a single expert neurologist using modified Rankin scale (MRS).[10]
Imaging study of each patient (which was done at the time of hospitalization) was studied again and the subtype of CVA was confirmed by a single neurologist.
We used SPSS 20.0 software (IBM SPSS Statistics) for analysis of the data. The t-test was used as appropriate. Statistical significance was assumed at P ≤ 0.05.
RESULTS
Of the total number 575 patients (64 men and 511 women) enrolled in the study, 38 were identified to have CVA. 6 (15.8%) were men and 32 (84.2%) were women. Their ages at the time of CVA ranged from 19 to 69 years, with the mean of 35.1 ± 1.2 years.
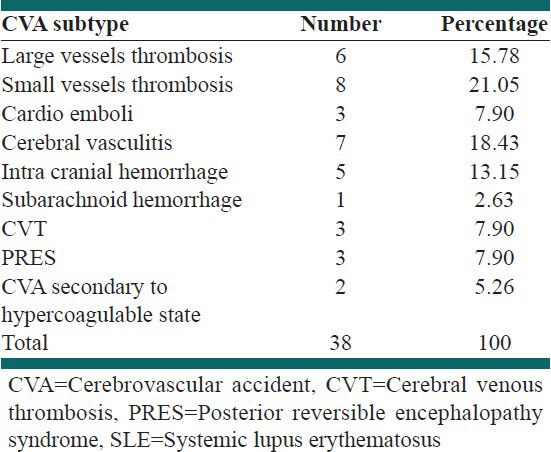
Small vessels thrombosis was the most common subtype, which includes eight patients (21.05%).
More detailed data are shown in Table 1.
Table 1.
CVA subtypes among Iranian SLE patients who enrolled in the study
12 (31.6%) patients had a history of hypertension; positive history of diabetes mellitus was present in two (5.7%) patients and seven (18.4%) had hyperlipidemia.
Duration of SLE before CVA in the study patients ranged from 0 to 16 years, with the mean of 4.25 ± 4.59 years. In 11 (28.9%) patients SLE was initiated with CVA and in three (7.9%) patients CVA was happened in the 1st year of SLE. APLAs were positive in 29 (76.3%) patients. In fact, in 88.2% of all ischemic attacks (include of large vessels thrombosis, small vessels thrombosis and cardio emboli) APLAs were positive.
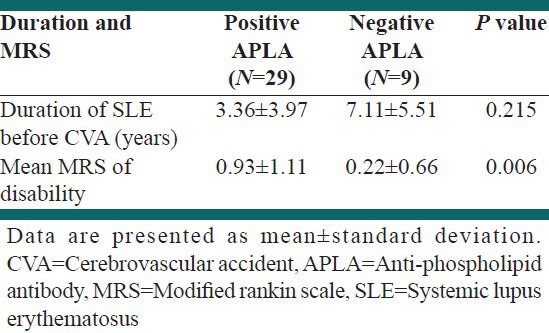
With the mean follow-up of 4.4 ± 3.4 years, mean MRS was 0.76 ± 1.12. In 24 patients, MRS at the last visit was zero. More detailed are shown in Table 2. In two patients, the CVA had recurred and in two patients transient ischemic attacks was recorded prior to CVA.
Table 2.
The comparison of MRS and SLE duration before CVA among CVA patients with positive and negative APLA
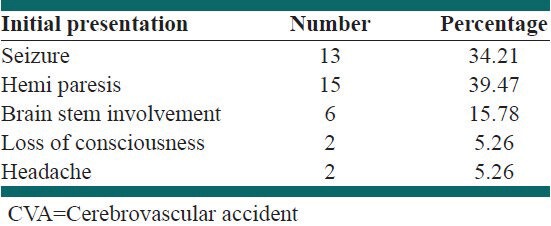
The most common CVA manifestation in our study was hemi paresis, which occurred in 15 (39.47%) patients. Detailed data about CVA initial presentations are shown in Table 3.
Table 3.
Initial presentation of CVA among the study patients
DISCUSSION
Previously, it has been demonstrated that age of SLE onset and sex ratio in Iranian patients are similar to those from other racial groups.[11] Present study showed that the prevalence of CVA in Iranian SLE patients is 6.6%. This prevalence is also within the range that reported from other parts of the world.[4,5,6]
Of the 38 CVA patients, in 11 cases CVA was the initial symptom of SLE. Futrell et al. implied that most SLE patients who develop CVA have their first CVA during the first 5 years of their disease and the highest rate is found during the 1st year.[3] In fact, it seems that in some patients SLE has special tendency to involve cerebral vessels, which is not related to the duration of SLE, but the nature of SLE.
The current study implies that a large proportion of all acute CVAs in Iranian SLE patients are constituted by ischemic attacks. This fact may reflect the influence of APLA and other autoantibodies, premature atherosclerosis, small vessel vasculopathy, arterial and venous thrombosis, embolism and vessel spasm in SLE.[5,12]
Although CVT, posterior reversible encephalopathy syndrome (PRES) and CVA secondary to hypercoagulable state are not in TOAST classification, but in that classification there is a category for “stroke of other determined etiology.”[9] We expanded the classification for more exact recognition of stroke subtypes in SLE patients.
Among our patients, we identified three cases of CVT. Two were positive for APLA. Our data showed that CVT is constituted 7.9% of CVAs in Iranian SLE patients, which is higher than the prevalence of CVT in the normal population.[13]
We also identified three cases with PRES. There is no study about the rate of PRES in SLE patients. Although PRES is not one of the classic CVA subtypes, but as the mechanism of PRES is cerebral vasospasm and because of endothelium dysfunction in SLE patients,[14] we report PRES as the cause of 7.9% of CVAs in Iranian SLE patients.
As following the average follow-up of 4.4 years, mean MRS of patients were less than 1, we may construe that if a patient with SLE survives CVA and his or her 5 year rehabilitation would not be unfavorable. This finding in Iranian SLE patients is differed from previous studies in this field.[15] Significant relationship between APLA and MRS (P = 0.006) shows that in patients with negative serology for APLA, morbidity rate of CVA is even less.
Our study also has some limitations; this study was not hospital-based so we were unwitting about the mortality rate of CVA in SLE patients. Thus, the prevalence of CVA in Iranian SLE patients that we have identified is likely to be an underestimation of the true frequency. Second, due to positive history of some factors such as hypertension, hyperlipidemia and diabetes mellitus in some stroke patients, it was favorable to operate proper statistical tests for eliminating their effects on the occurrence of stroke. However, as our recorded data about the presence of these factors in other non-stroke patients was not sufficient this step was not possible. Disease activity of SLE and the type of APLA (anti-cardiolipin antibody or lupus anticoagulant) at the time of stroke were absent in our medical records which might have a correlation with the stroke subtypes. However, the study showed positive APLA in SLE patients with stroke had more prevalence and was associated with a worse prognosis.
CONCLUSIONS
According to the significant prevalence of CVA among SLE patients, CVA prevention should start at the early phase of disease and be considered as an essential component of therapeutic strategies. Iranian SLE patients are susceptible for different CVA subtypes include ischemic and hemorrhagic events. Moreover, we showed that the prognosis of CVA in Iranian SLE patients is not unfavorable.
ACKNOWLEDGMENTS
This study was supported by a grant from Isfahan University of Medical Sciences (Grant No. 289305).
Footnotes
Source of Support: Isfahan University of Medical Sciences (Grant No. 289305)
Conflict of Interest: None declared.
REFERENCES
- 1.Brey RL. Neuropsychiatric lupus: Clinical and imaging aspects. Bull NYU Hosp Jt Dis. 2007;65:194–9. [PubMed] [Google Scholar]
- 2.Schur PH, Gladman DD. Overview of the clinical manifestations of systemic lupus erythematosus in adults. In: Basow DS, editor. Up To Date. Waltham, MA: Up to Date; 2009. [Google Scholar]
- 3.Sayed Bonakdara Z, Mohtasham N, Karimifara M. Evaluation of damage index and its association with risk factors in patients with systemic lupus erythematosus. Journal of Research in Medical Science. 2011;16(special issue):427–32. [PMC free article] [PubMed] [Google Scholar]
- 4.Futrell N, Millikan C. Frequency, etiology, and prevention of stroke in patients with systemic lupus erythematosus. Stroke. 1989;20:583–91. doi: 10.1161/01.str.20.5.583. [DOI] [PubMed] [Google Scholar]
- 5.Krishnan E. Stroke subtypes among young patients with systemic lupus erythematosus. Am J Med. 2005;118:1415. doi: 10.1016/j.amjmed.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 6.Ward MM. Premature morbidity from cardiovascular and cerebrovascular diseases in women with systemic lupus erythematosus. Arthritis Rheum. 1999;42:338–46. doi: 10.1002/1529-0131(199902)42:2<338::AID-ANR17>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 7.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 8.Hatano S. Experience from a multicentre stroke register: A preliminary report. Bull World Health Organ. 1976;54:541–53. [PMC free article] [PubMed] [Google Scholar]
- 9.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]
- 10.Huybrechts KF, Caro JJ, Xenakis JJ, Vemmos KN. The prognostic value of the modified Rankin Scale score for long-term survival after first-ever stroke. Results from the Athens Stroke Registry. Cerebrovasc Dis. 2008;26:381–7. doi: 10.1159/000151678. [DOI] [PubMed] [Google Scholar]
- 11.Nazarinia MA, Ghaffarpasand F, Shamsdin A, Karimi AA, Abbasi N, Amiri A. Systemic lupus erythematosus in the Fars Province of Iran. Lupus. 2008;17:221–7. doi: 10.1177/0961203307086509. [DOI] [PubMed] [Google Scholar]
- 12.Mashhadi MA, Bari Z. Thrombotic thrombocytopenic purpura and deep vein thrombosis as the presenting manifestations of systemic lupus erythematosus: A case report and review of literature. Journal of Research in Medical Science. 2011;16:1082–8. [PMC free article] [PubMed] [Google Scholar]
- 13.Ferro JM, Correia M, Pontes C, Baptista MV, Pita F Cerebral Venous Thrombosis Portuguese Collaborative Study Group (Venoport) Cerebral vein and dural sinus thrombosis in Portugal: 1980-1998. Cerebrovasc Dis. 2001;11:177–82. doi: 10.1159/000047635. [DOI] [PubMed] [Google Scholar]
- 14.Ahmadi B, Bonakdar ZS, Hashemi SM, Sadrkabir SM, Karimifar M. Endothelial dysfunction in Iranian lupus patients. Rheumatol Int. 2011;31:27–31. doi: 10.1007/s00296-009-1212-0. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen-Oghalai TU, Wu H, McNearney TA, Granger CV, Ottenbacher KJ. Functional outcome after stroke in patients with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum. 2008;59:984–8. doi: 10.1002/art.23816. [DOI] [PMC free article] [PubMed] [Google Scholar]


