Abstract
Background:
Training medical students in tobacco prevention and cessation skills is critical to have competent physicians who are prepared to address the grave levels of morbidity and mortality associated with tobacco use. However, in India, enough attention has not been given to elicit the active participation of physicians in tobacco control. Keeping this in view, a program was undertaken to develop the skills and competence of medical students with the objective of improving medical student inquiry into smoking and the delivery of advice accordingly for patients in their clinical year's routine consultations.
Methods:
The targeted learners were 149 1st-year medical and dental students of SCB Medical College, Cuttack, Orissa, India, who had appeared the second semester examination; 84 of the participants were male. Students were allowed to appear a test before the training session on knowledge of tobacco cessation and post test was done after 1.5 months of training. The knowledge score was evaluated to evaluate the learning outcome.
Results:
We observed that a curriculum on tobacco intervention could improve relevant knowledge, attitudes and self-confidence and be applied in students early clinical experiences.
Conclusions:
There is need of joint action by practicing clinicians, the medical faculty and the curriculum planners of the country to incorporate tobacco cessation into the curriculum.
Keywords: Medical curriculum, physician education, student learning, tobacco prevention
INTRODUCTION
The negative health effects of tobacco constitute the single largest preventable cause of death and disease in economically developed countries, with increasing implications in the developing world.[1] Although tobacco-related deaths rarely come into highlight, tobacco consumption is responsible for one-third to one-half of all people who use it,[2] on an average 15 years before the actual life expectancy.[3,4] Tobacco smoking is the leading cause of morbidity and premature mortality in India.[5,6] Considering the scale of this health impact, there should be little debate about the importance of providing medical personnel with the knowledge and skills to reduce the impact of tobacco. Health care professionals bear significant responsibility to address smoking, given that opportunistic advice from a doctor has been shown to promote smoking cessation in patients. The importance of identification of smoking has led to calls for smoking status to be recorded as a vital sign.[7] However, smoking continues to be identified by medical practitioners in India with variable frequency, despite a knowledge of its effects. This suggests that doctors are not considerably effective at incorporating anti-smoking health promotion into clinical practice. Past studies based on the tobacco cessation practice among general practitioners (GP) in India had revealed that most of the physicians are not providing tobacco cessation counseling to their patients and that they feel ill prepared to advice their patients on tobacco cessation. They attribute this low intervention rate primarily to lack of appropriate training in the undergraduate medical years.[8] Analyses of the tobacco control content of the extant medical curriculum in India reveal that although the negative effects of tobacco are incorporated in some way in the curricula, it is neither systematically nor vertically integrated and makes no mention of the issues of the skills and competence surrounding anti-tobacco counseling. This has resulted in insufficient knowledge of smoking cessation strategies and perceived lack of effectiveness among the physicians to intervene.[9] It is the general belief among health care professionals in India that anti-smoking advice is not under the domain of a physician; majority of the GPs view smoking in clinical practice with a casual attitude and, often, it is left for the patients to deal with this behavioral problem on their own.[10,11]
To have a sustainable critical mass of competent and skilled physicians in tobacco cessation and treatment, it is imperative that they should acquire the basic knowledge and skills as a component of medical education. Medical students, the doctors of the future, should be familiar with the negative health effects of smoking – they should possess adequate knowledge base and inculcate specific patient-centered smoking cessation counseling skills during the formative years. There is no area of medical education and preventive medicine that will yield greater returns in better health, saved lives and reduce medical costs than an emphasis on cessation of smoking.[12,13] However, medical faculty and curriculum designers in India have remained oblivious to this vital need till date. The large mass of medical students have remained an unexplored potential and missed opportunity in the battle against the tobacco epidemic.[14,15]
Keeping this in view, the present work was undertaken to develop the skills and competence of medical students, with the objective of improving medical student inquiry into smoking and the delivery of advice accordingly for the needy patients in their clinical years and future practice. The project specifically attempted to determine whether a curriculum on tobacco intervention integrated with a skill-building program could garner medical students’ acceptance; improve relevant knowledge, attitudes and self-confidence; and be applied in students’ early clinical experience. The primary outcome measure was a change in the anti-smoking health promotion practice of the students demonstrated within an objective structured clinical examination (OSCE).[16] This study is, to the best of our knowledge, the first of its kind in the state Orissa (India).
METHODS
The intervention was carried out during the summer of 2006 at SCB Medical College, Cuttack, Orissa, India. SCB Medical College is the most premier medical institute of the state of Orissa, imparting MBBS, Dental, Nursing and allied health programs. Universal sampling was done to include study participants. Students who had appeared in the second semester examination were allowed to participate voluntarily. A total of 149 students were eligible and were included in the study. This was a quasi-experimental study.
INTERVENTION
Selected model for behavioral change
We selected motivational interviewing as a framework for promoting behavior change.[17] Research demonstrates that motivational interviewers help patients who are not committed to change reflect on the advantages and disadvantages of change in light of their personal life goals and values. Simultaneously, they help committed patients to change design their own change plans in consonance with their own goals and values, assess their progress and refine their plans as needed. Evidences suggest that stage-based interventions and motivational interviewing are effective in promoting change in a variety of unhealthy and risky behaviors. Moreover, motivational interviewing possesses inherent cultural sensitivity, and it puts special emphasis on empathy, respect and partnership with current teaching on communication.[18,19]
Curriculum design and program development
The curriculum was designed based on various key principles. Several factors were taken into account for the preparation of this text material [Table 1].
Table 1.
Key principles taken into consideration while designing the curriculum
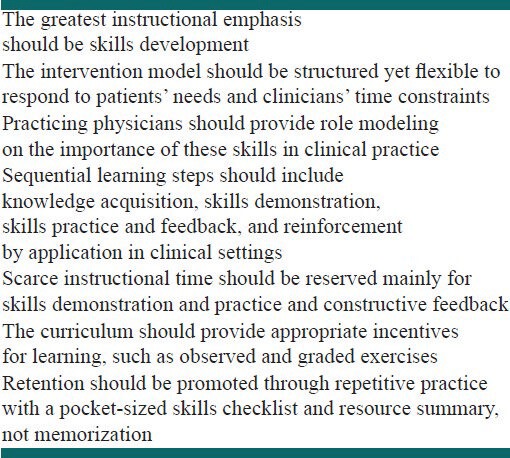
The contents of the curriculum and the components of the program were developed from the materials on motivational interviewing, established standardized guidelines on smoking cessation and different international tobacco intervention curricula of proven efficacy.[20,21] A computer-generated manual served as the text along with a small pocket guide that summarized the intervention model, key resources and information on referral options and pharmacotherapy. The teaching, along with skill building, was imparted during the 2-month inter-semester summer break.
Implementation and learning activities
The implementation involved following components and learning activities. The sequence of learning process is shown in Chart 1 [Table 2].
Table 2.
The key components of the skill-building program
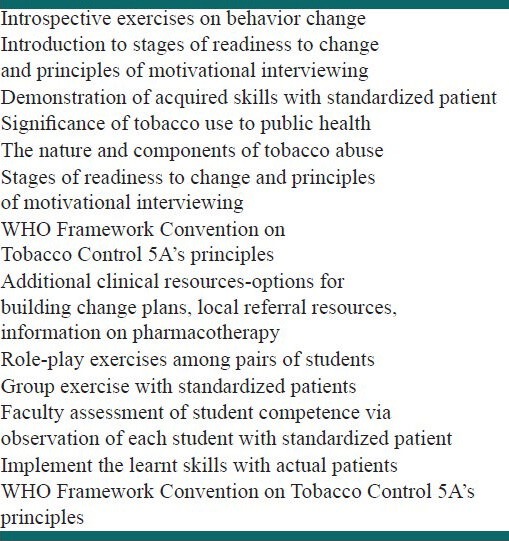
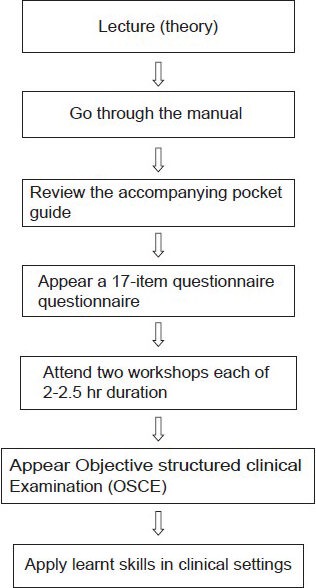
A self-administered 17-item Objective Knowledge Questionnaire was developed related to smoking morbidity and mortality, and was intended to ensure adequate knowledge before the workshop.[22,23] It was distributed in the lecture the day before the workshop. Students were asked to complete and return the questionnaire immediately. Students were assured that their responses were voluntary and confidential and would have no bearing on the academic assessment.
Two skill-building workshops (each spanning 2-2.5 h) were held with approximately 15 participants in each workshop and four staff facilitating each workshop. Both the workshops employed a mixture of didactic presentation, small-group discussion, large-group question-and-answer sessions and case studies. This covered all the key components enumerated above. Case studies involved the students taking on the perspectives of the patient. Written literature on intervention strategies was provided. The staffs were recruited from specialists in general medicine, community medicine and pulmonary medicine. They were assisted by senior residents of various medical and surgical disciplines.
For summative assessment, the students appeared a designed OSCE, with feedback on each student offered by the instructor and other students. The faculty found that all students demonstrated basic competence. Students were encouraged to apply the newly acquired skills during their ward duty, in which each student spends two half-days per month with patients under the supervision of a senior resident.[21,22]
Evaluation
Student endorsement of the curriculum and its components was assessed by a confidential evaluation questionnaire. Students provided ratings using 7-point Likert-type scales with anchors at the midpoints and the extremes. Gains in students’ attitudes, knowledge and self-confidence were gauged by comparing responses to pre-test and post-test versions of the Learning Outcomes Questionnaire (LOQ). The pre-test version was administered immediately before the lecture while the post-test version was administered 1.5 months after the skill-building program. In the LOQ, the items assessed attitudes regarding physicians’ roles, beliefs regarding the reasons patients maintain unhealthy behaviors despite physician advice and the self-confidence to apply knowledge and implement motivational interviewing skills. Subsequently, as a knowledge test, items asked students in an open-ended manner to provide suggestions for promoting behavior change for case studies. Finally, the LOQ elicited self-reports on use of stage-based motivational techniques for promoting changes in several listed health-related behaviors in the students’ clinical settings.[23]
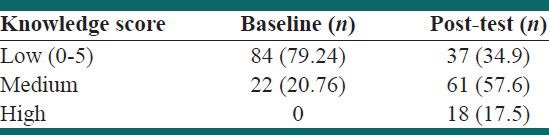
To assess knowledge, a score was calculated by summing correct answers to each of 17 knowledge questions. A change score was then calculated by subtracting the baseline score from the post-test score for each participant. To estimate attitudes, ordinal responses to attitudinal statements were compared. For skills, responses of “always” and “frequently” for use of specific smoking cessation techniques were combined and proportions compared between baseline and post-test. Change in self-rated competence was calculated as the difference between baseline and post-test ratings for each participant.
RESULTS
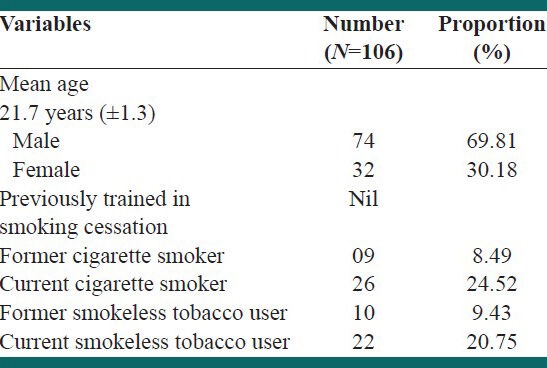
The targeted learners were 149 1st-year medical and dental students of the college who had appeared the second semester examination; 84 of the participants were male. One hundred thirty-eight (92%) of the students completed the evaluation questionnaire at the conclusion of the program. One hundred twenty-one (81%) of the students attended the initial lecture and completed the LOQ pre-test, 128 (86%) completed the LOQ post-test and 106 (71%) students completed both. One hundred and fifteen (77%) of the students completed the questions on applying the tobacco intervention skills (TIS) in clinical practice.
Of 106 students, most of them were male and the mean age of the study participants was 21.7 years. Twenty-six of the students have current habit of smoking, whereas 22 of the 106 students were current smokeless tobacco users [Table 3].
Table 3.
Socio-demographic information
In response to open-ended questions, many students suggested reducing workshop time for practice and feedback and conducting the final skills assessment without student observers. Nearly two-thirds of the students gave the entire curriculum one of the top two ratings. Additional unsolicited feedback included several requests from 2nd- and 3rd-year students for this training.
Students manifested more favorable attitudes regarding physician roles in promoting behavior change, less judgment toward non-adherent patients and more self-confidence in applying TIS knowledge and skills after the TIS program exposure; responses to case scenarios improved after TIS. For all items, categorical results regarding statistical significance for the pre-test and post-test comparisons (P < 0.05) were identical for the paired t tests and the non-paired, 2-sample t tests. Many students (>75%) reported using TIS in clinical settings after exposure to the curriculum.
First-year medical and dental students favorably received the initial implementation of the curriculum. Most students found the educational content important and appropriate for their level of training. Although the major purpose of this project was skill building, the program elicited significant attitudinal shifts. After TIS, students’ extant sense of responsibility for promoting behavior change was enhanced. Students demonstrated improvement in perceived and actual knowledge and in perceived skills to promote behavior change. Students demonstrated improvement in perceived and actual knowledge and in perceived skills to promote behavior change [Table 4]. The high number of students who used the TIS model with actual patients in their clinical years shows a favorable sign for long-term retention of the skills. A similar result was described in the study done in the USA.[24]
Table 4.
Percentage of students with correct responses on smoking cessation knowledge from baseline to post test
This piloting study of the TIS curriculum has some important limitations. The study demonstrated only short-term changes in attitudes and knowledge. The study did not document in a blinded, objective manner whether students’ skills were enhanced for standardized or actual patients. Background information about their training status was not asked. Similar previous studies in western countries have observed that medical students improved their attitudes, knowledge and self-confidence in skills for promoting behavior change after elective course on motivational interviewing. The current study echoes their findings.[25,26]
CONCLUSIONS
The current study is first of its kind in employment of tobacco intervention training as an initial experience for training medical students in promoting a change in smoking behavior in an Indian context. If 1st-year students can gain from training on promoting behavior change, should such training start in the 1st year? A study comparing individuals trained under different curricula could provide a definitive answer. However, current physician inattention to risky and unhealthy behaviors, the high mortality and morbidity associated with them, the lack of data to support the traditional curricular sequence and, now, the potential for 1st-year students to begin gaining from training on promoting behavior change argue for including such training in the 1st year.[27] The present work bodes well to advocate for the integration of a longitudinal curriculum on promoting behavior change in smoking cessation among medical and dental students. Early initiation of training on promoting behavior change might be advantageous for the medical and dental students. Earlier acquisition and application of skills in promoting behavior change might enhance 1st- and 2nd-year medical students’ sense of belonging and usefulness in clinical environments. Training on such skills might reinforce the importance of basic communication skills, such as building rapport, attending to affective issues, and cross-cultural communication. These advantages could only be realized if teaching these skills earlier were feasible and acceptable to medical students. This study reveals that the development of a specific intervention can lead to an improvement in addressing smoking within a complex clinical scenario as measured by performance in an OSCE. Presumably, performance could be improved further if the importance and practice of these skills was reinforced by regular observation of practitioners during their clinical years.[28,29] Furthermore, such reinforcement would be helpful in the maintenance of these new skills in the early years of postgraduate medical practice. This calls for a joint action by practicing clinicians, the medical faculty and the curriculum planners of the country.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.WHO; 1996. World Health Organization. The tobacco epidemic: A global public health emergency. Tobacco Alert (Special Issue) p. 126. [Google Scholar]
- 2.Peto R, Lopez AD, Boreham J, Thun M, Heath C, Jr, Doll R. Mortality from smoking worldwide. Br Med Bull. 1996;52:12–21. doi: 10.1093/oxfordjournals.bmb.a011519. [DOI] [PubMed] [Google Scholar]
- 3.Atlanta, US: Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2004. [Last accessed 2012 18 April]. US Department of Health and Human Services. The health consequences of smoking: A report of the Surgeon General. Available from: http://www.cdc.gov/tobacco/data_statistics/sgr/sgr_2004/chapters.htm . [Google Scholar]
- 4.Peto R, Lopez AD, Boreham J, Thun M, Heath C., Jr Mortality from tobacco in developed countries: Indirect estimation from national vital statistics. Lancet. 1992;339:1268–78. doi: 10.1016/0140-6736(92)91600-d. [DOI] [PubMed] [Google Scholar]
- 5.Reddy KS, Gupta PC. New Delhi: Ministry of Health and Family Welfare, Government of India; 2004. Report on tobacco control in India. [Google Scholar]
- 6.Dam A. Tobacco related cancers: An emerging public health problem in India. Indian J Community Med. 2005:30–05. [Google Scholar]
- 7.WHO; 2004. [last accessed on 2012 29 April]. World Health Organization. Code of practice on tobacco control for health professional organizations. Available at: http://www.who.int/tobacco/research/cessation/code_practice_en.pdf . [Google Scholar]
- 8.Pati S. A study on Tobacco Cessation Practice among General Practitioners in Orissa (India) Lung Cancer. 2005;49:S195. [Google Scholar]
- 9.Pati S. Attitudes to Tobacco Control among Medical Interns in Orissa, India: Book of Abstracts. In: Bos EM, editor. The Netherlands: ISCOMS, June; 2005. p. 249. ISBN: 90-367-2296-9. [Google Scholar]
- 10.Bhatia RS, Vijayan VK. Tobacco and health: What can the medical profession do? Lung India. 1994;12:178–85. [Google Scholar]
- 11.Sarkar D, Dhand R, Malhotra A, Malhotra S, Sharma BK. Perceptions and attitude towards tobacco smoking among doctors in Chandigarh. Indian J Chest Dis Allied Sci. 1990;32:1–9. [PubMed] [Google Scholar]
- 12.New Delhi, India: Medical Council of India; 1997. [Last accessed on 15-May -2012]. Medical Council of India (MCI). Regulations on graduate medical education. Available at http://www.mciindia.org/RulesandRegulations/GraduateMedicalEducationRegulations1997.aspx . [Google Scholar]
- 13.Warren CW. Tobacco use and cessation counselling: Global Health Professionals Survey Pilot Study, 10 countries, 2005. Tob Control. 2006;15:ii31–4. doi: 10.1136/tc.2006.015701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zwar NA, Richmond RL. Role of the general practitioner in smoking cessation. Drug Alcohol Rev. 2006;25:21–6. doi: 10.1080/09595230500459487. [DOI] [PubMed] [Google Scholar]
- 15.Silagy C, Stead LF. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2001;2:3. doi: 10.1002/14651858.CD000165. [DOI] [PubMed] [Google Scholar]
- 16.Roseby R, Marks MK, Conn J, Sawyer SM. Improving medical student performance in adolescent anti-smoking health promotion. Med Educ. 2003;37:704–8. doi: 10.1046/j.1365-2923.2003.01560.x. [DOI] [PubMed] [Google Scholar]
- 17.Miller WR, Rollnick S. Chapter 15. New York: Guilford Press; 2002. Motivational Interviewing. Preparing people for change; pp. 201–216. [Google Scholar]
- 18.Miller WR. Treatment Improvement Protocol (TIP) Substance Abuse and Mental Health Services Administration; 1999. Enhancing motivation for change in substance abuse treatment. Series 35, DHHS Publication No. (SMA) 99-3354. [PubMed] [Google Scholar]
- 19.Brown RL. Providence New England: Addiction Technology Transfer Center; 2002. [last accessed on 2012 17 January]. Motivational Interviewing: A Web-based Course. Available at: http://www.motivationalinterview.org/quick_links/mitraining.html . [Google Scholar]
- 20.Boehlecke B, Sperber AD, Kowlowitz V, Becker M, Contreras A, McGaghie WC. Smoking history-taking skills: A simple guide to teach medical students. Med Educ. 1996;30:2839. doi: 10.1111/j.1365-2923.1996.tb00830.x. [DOI] [PubMed] [Google Scholar]
- 21.Richmond R, editor. Paris: International Union against Tuberculosis and Lung Disease; 1996. Educating Medical Students about Tobacco: Planning and Implementation. [Google Scholar]
- 22.Arizona Department of Health Services Tobacco Education and Prevention Program (AzTEPP) [Last accessed on April 2012]. Available at http://www.tepp.org .
- 23.Cohen J. 2nd ed. Chapter 1. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences; pp. 14–15. [Google Scholar]
- 24.Leong SL, Lewis PR, Curry WJ, Gingrich DL. Tobacco world: Evaluation of a tobacco cessation training program for third-year medical students. Acad Med. 2008;83:S25–8. doi: 10.1097/ACM.0b013e318183e271. [DOI] [PubMed] [Google Scholar]
- 25.Skochelak S, Thaler S, Gjerde C. The Interdisciplinary Generalist Curriculum Project at the University of Wisconsin Medical School: The Generalist Partners Program. Acad Med. 2001;76:S131–3. doi: 10.1097/00001888-200104001-00026. [DOI] [PubMed] [Google Scholar]
- 26.Papadakis MA, Croughan-Minihane M, Fromm LJ, Wilkie HA, Ernster VL. A comparison of two methods to teach smoking-cessation techniques to medical students. Acad Med. 1997;72:725–7. doi: 10.1097/00001888-199708000-00021. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Chapter 10. New Jersey: Prentice Hall, Englewood Cliffs; 1986. Social foundations of thought and action: A social cognitive theory; pp. 520–2. [Google Scholar]
- 28.Ajzen I, Fishbein M. Upper Saddle River, NJ: Pearson Education; 1980. Building intention and prediction of: Understanding Attitudes and Predicting Social Behavior; pp. 167–71. [Google Scholar]
- 29.Washington, DC: Center for Advancement of Health; 2001. [Last accessed on 2012 14 April]. Center for Advancement of Health. Integration of Health Behavior Counseling in Routine MedicalCare. Available at http://www.prescriptionforhealth.org/downloads/integration2001.pdf . [Google Scholar]


