Abstract
Background:
Low birth weight (LBW) is considered as an important outcome of birth and pregnancy, which is associated with long-term consequences and health-care problems. Maternal lifestyle and health care during pregnancy are powerful predictors of BW of infants. The purpose of this study was to assess the effect of a self-care educational program based on the Health Belief Model (HBM) on reducing LBW among a sample of pregnant Iranian women.
Methods:
In this randomized controlled trial, we recruited 270 pregnant women referred to prenatal clinics in the south of Tehran, Iran. The participants were randomly allocated to two intervention and control groups. Women in the intervention group received an educational program to promote self-care behaviors during pregnancy. The control group received routine care. BW was compared between the two groups. Baseline demographic characteristics and knowledge and attitude scores before the intervention in both groups were compared using the Chi-square test for categorical variables. Logistic regression analysis was conducted to control the effect of demographic variables on BW.
Results:
The results showed that LBW was reduced significantly in the intervention group at the follow-up measurement (5.6 vs. 13.2%, P = 0.03). After controlling for demographic characteristics, we found a significant decrease in the risk of LBW in the intervention group [odds ratio (OR): 0.333; 95% confidence interval (CI): 0.12-0.88, P = 0.02].
Conclusions:
Implementation of a self-care educational program designed on the basis of an HBM on pregnant women was effective in reducing the rate of LBW.
Keywords: Health belief model, health-care education, low birth weight, outcome of pregnancy, self-care
INTRODUCTION
Low birth weight (LBW), defined as weighing less than 2,500 g at birth,[1] has known adverse effects including higher incidences of mortalities and chronic diseases with long-term consequences, increased hospital costs, and impaired growth,[2,3] and is considered as an important outcome of birth and pregnancy.[4] A total of 15.5% of infants are born with LBW worldwide, of whom 95.6% occur in the developing countries.[1]
Although LBW has multiple causes, maternal lifestyle and health during pregnancy are powerful predictors of BWs of infants.[2,5] Physical activity, food intake and weight gain, oral health, substance and drug abuse, smoking, and hard work are some behaviors related to health care that can affect the outcomes of pregnancy.[5,6,7] Women need a continuum of care throughout pregnancy which starts with self-care activities,[8] aimed at maintaining and improving health.[9,10]
Presenting theory- and evidence-based educational programs for pregnant women during prenatal care helps to solve health-care problems related to pregnancy, decreases risky behaviors, and improves outcomes of pregnancy.[11]
In the field of health-care education, theories and models help us to explain and predict behaviors to conduct effective health-care educational programs for changing behaviors.[12] The HBM, one of the most widely used conceptual frameworks in research on health behavior, has been used by health-care educators to predict, describe, and explain behavior related to health care based on the perceptions and belief patterns of individuals. The HBM contains several primary concepts by which individuals evaluate themselves to take action to change their behaviors. According to this model, if a person believes that he or she is susceptible to a condition or disease (perceived susceptibility), believes that the condition would have potentially serious consequences (perceived severity), believes that the benefits of taking action outweigh the barriers (perceived benefits and barriers), believes that he or she can engage in a behavior (self-efficacy), is ready to take action, and could be potentiated by cues to action (cue to action), he or she is more likely to take action to change. The HBM constructs generally have been found to predict most behaviors related to health care such as screening for breast cancer, mammography, screening for colorectal cancer, and AIDS-related behaviors.[13]
According to the Demographic and Health Survey (DHS) 2000, a great number of pregnant women in Tehran had not attended health-care centers for prenatal care.[14] It seems that providing the necessary information for women might increase the rate of attendance.
Moreover, it is recommended that health-care educational programs should be designed according to the cultural context of the audiences. In this study, we used the HBM as a conceptual model for understanding and predicting adherence to self-care behavior. It was hypothesized that an intervention based on HBM that included self-care education would result in a greater increase in self-care activities among pregnant women. So we developed a self-care educational program based on the HBM for pregnant Iranian women and assessed its effect on the knowledge and beliefs related to health care of women, and incidence of LBW.
METHODS
Study design and population
This randomized controlled trial was conducted on 270 pregnant women referred to the prenatal clinics of a health service network in the south of Tehran during 2009-2011. This health-care service network covers five districts of Tehran municipality. These districts have the characteristics of densely populated communities and low to moderate socioeconomic status. The main objective of the study was to estimate the proportion of LBW and its odds ratio (OR). Considering the proportion of LBW in similar studies,[2] the sample size was calculated with a 95% confidence interval (CI) and 80% power of test. Two health-care centers were randomly selected from each district and half of the cases from each center were separated randomly for the intervention group and the other half for the control group. Thus, each pregnant woman was randomly assigned to either the intervention or control group (135 participants in each group). Eligibility criteria included maximum 12-week gestational age at baseline and no prior diagnosis of chronic disease. Unhealthy women such as women with chronic diseases were excluded.
At first, knowledge and attitudes of women, which can provide the rationale for behavior related to health care, were assessed as predisposing factors using an instrument designed on the basis of the HBM constructs. The instrument included sections on demographic characteristics, knowledge (seven items), and attitude (23 items based on the Likert scale). Scores of the variables were classified as weak (<60%) and good (≥60%). Ten health-care education and health-care promotion professionals confirmed the validity of the face and content of the questionnaires. The reliability of the attitude questionnaire was confirmed with a Cronbach's alpha reliability coefficient of 0.80 obtained in a pilot study on 30 pregnant women other than the two main study groups. A test-retest method was used for determining the reliability of the knowledge questionnaire in the pilot sample, and a correlation coefficient of 0.75 was achieved.
All the pregnant women provided informed consent before collection of the data. The study protocol conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The research project received the confirmation of the Institution Ethics Committee of Tehran University of Medical Sciences.
Intervention
Based on the findings of the baseline data, an intervention was developed and implemented in the intervention group. Educational objectives, content of the educational program, messages, concepts, and materials were developed using the results of formative research, views of experts, and scientific resources. The educational content toward self-care in pregnancy included several items on physical activity, nutrition, and oral health, side effects of substance and illegal drug abuse and smoking during pregnancy, the risk signs of pregnancy complications, ways to prevent toxoplasmosis, sexually transmitted infection, and exposure to X-rays, and prevention of traffic accidents. We also presented guidelines in performing recommended actions. Women in the intervention group received the educational package in addition to the usual antenatal care and education during each visit throughout their pregnancies by the health-care staff, including family health staff.
Educational intervention was conducted through holding training sessions for self-care education, colloquy sessions about issues related to pregnancy, distributing educational pamphlets related to self-care activities during pregnancy for pregnant women in the intervention group and holding discussion sessions with the participants developed on the basis of the HBM about issues related to pregnancy, information on the consequences of adverse outcomes of pregnancy, especially LBW for the newborn, the importance of self-care activities and a healthy lifestyle during pregnancy, and benefits and barriers of self-care activities during pregnancy. We tried to reach appropriate attitudes toward the issues related to self-care in pregnancy among the women. Participants in the control group received only the usual care from health-care professionals. Women in both groups were followed throughout the pregnancy and postpartum period and their newborns were followed during the first six months of life. This study compared the incidence of LBW between newborns of the women in both study groups.
Statistical analysis
The data was analyzed using the statistical software SPSS (version 18). Baseline demographic characteristics and knowledge and attitude scores before the intervention in both groups were compared using the Chi-square test for categorical variables. Following this, logistic regression analysis was conducted to control the effect of demographic variables including education, age, family size, housing, occupation, and history of participation in self-care education classes on BW. These factors were entered in the logistic regression and LBW (Yes/No) was entered as a dependent variable. OR and CI were calculated for these tests of association. A P < 0.05 was considered significant.
RESULTS
A total of 270 women participated in the study. There were 23 pregnant women (nine women from the intervention group and 14 women from the control group) who were excluded from the study because of unwillingness to continue the study (n = 2), migration to other cities (n = 10), and abortion (n = 11).
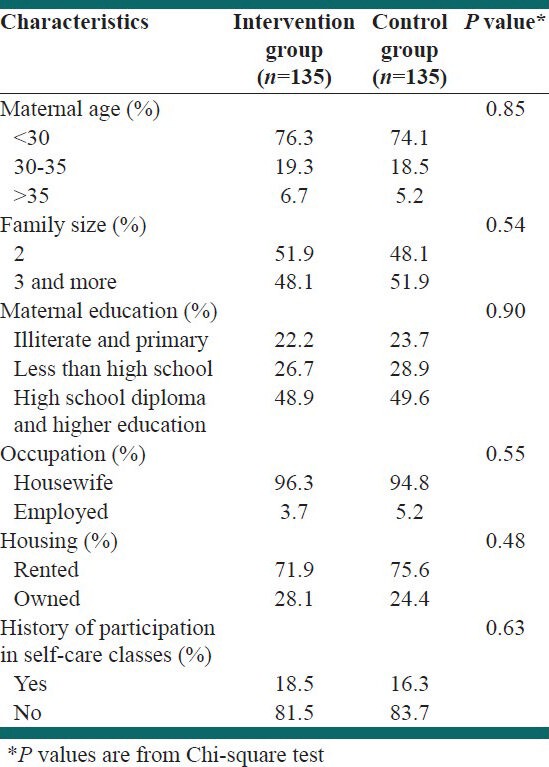
As shown in Table 1, there were no significant differences in any of the demographic characteristics between the two study groups (i.e., the intervention and the control groups) (P > 0.05).
Table 1.
Demographic characteristics of the study population (n=270)
Knowledge and the HBM constructs were compared in both groups [Table 2]. Before the intervention, the majority of women in the intervention and control groups (91.9 and 92.6%, respectively) had a good level of knowledge regarding self-care activities during pregnancy, and there were no significant differences in the mean score of knowledge between the two study groups (P > 0.05).
Table 2.
Comparison of the scores of knowledge and the constructs of HBM between the intervention and control groups
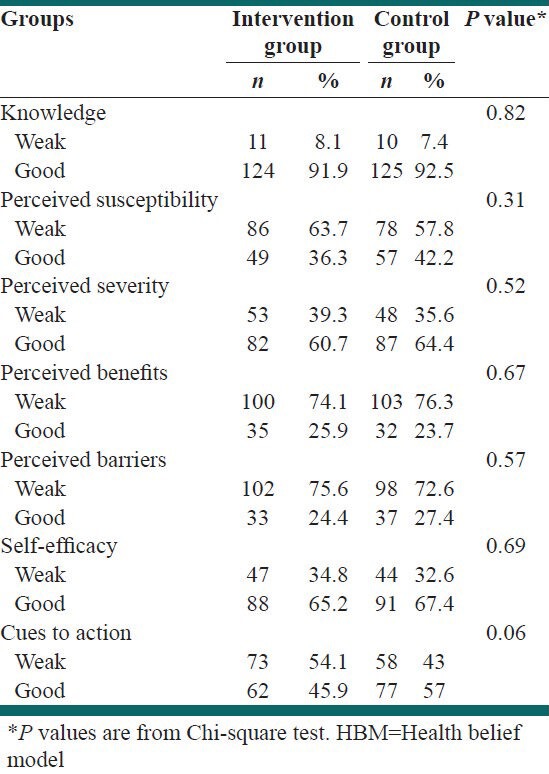
At the baseline, the scores of some constructs of HBM including perceived susceptibility, perceived benefits, and perceived barriers were at low levels in the women of both groups; however, perceived severity and self-efficacy were high in both groups. There were no significant differences in the scores of the HBM constructs between the two groups (P > 0.05).
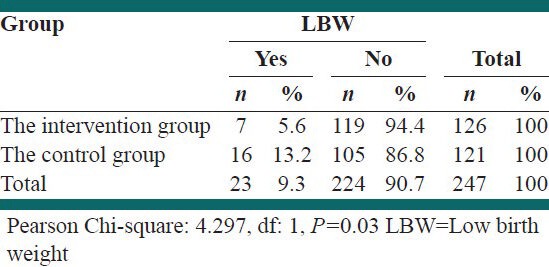
The rate of LBW in the intervention group was significantly lower than the control group (5.6 vs. 13.2%.) in the follow-up measurement. The Chi-square test showed significant difference between the two groups in terms of BW (P = 0.03) [Table 3].
Table 3.
Comparison of LBW between the intervention and the control group (n=247)
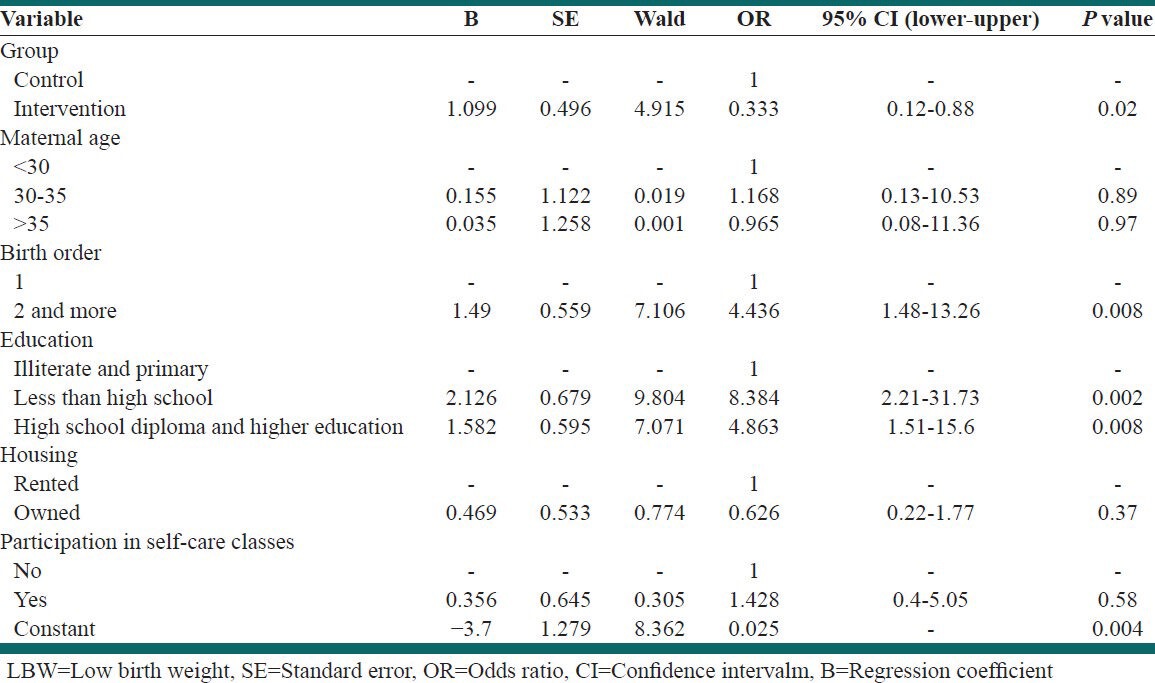
Considering the OR for each demographic variable, a lower birth order increased the risk of LBW, such that nulliparous women (no history of abortion) had a significantly higher odds of having an LBW infant than other women (OR: 4.436; 95% CI: 1.48-13.26; P = 0.008). Women with primary school education had a significantly higher odds of having an LBW infant than women with high school diploma and higher education (OR: 8.384; 95% CI: 2.21-31.73; P: 0.002). Also, women with less than high school education had a significantly higher odds of having an LBW infant than women with a high school diploma and higher education (OR: 4.863; 95% CI: 1.51-15.6; P = 0.008). After controlling for demographic characteristics, implementation of a self-care educational program was significantly associated with a reduced risk of LBW (OR: 0.333; 95% CI: 0.12-0.88, P = 0.02). The results of the binary logistic regression are shown in Table 4.
Table 4.
Logistic regression analysis for LBW and its risk factors
DISCUSSION
In this study, we developed a self-care educational program based on the HBM for pregnant Iranian women and assessed its effect on the incidence of LBW.
During the last few decades, various health-care education models have been applied to achieve large-scale changes in behavior.[15,16] The HBM has been largely applied as a guiding framework for interventions in health-care behavior to change unhealthy behaviors and maintain healthy behaviors.[13] The access of pregnant women to proper information on issues related to pregnancy and delivery and empowering them to make positive changes in health-care behaviors are among the main challenges for health-care providers.[5] Some studies have indicated that maternal education is the most important social factor that can affect outcomes of pregnancy and birth.[17]
According to our findings, educational intervention should focus primarily on changing attitudes related to self-care during pregnancy, especially via focusing on some constructs of the HBM such as perceived susceptibility, perceived benefits, and perceived barriers. We considered these constructs in developing our educational objectives and content. If pregnant women regarded themselves as susceptible to adverse outcomes of pregnancy, believed that self-care activities during pregnancy would be beneficial in reducing adverse outcomes of pregnancy and birth, and if they were convinced that the anticipated benefits of taking action outweighed the barriers or costs of action, they were likely to take action that they believed would reduce their risks. It is generally accepted that cultural perceptions and attitudes can influence the performance of women during pregnancy.[11] One possible explanation for the success of the intervention in promoting self-care behaviors during pregnancy is that highly perceived susceptibility and severity, lowly perceived barriers, and highly perceived benefits to take action can increase the likelihood of engaging in self-care behaviors during pregnancy.
In our study, significant improvement in BW was seen in the newborns of women who received self-care education based on the HBM during pregnancy. Thus, results of this study suggest that self-care education based on HBM during pregnancy reduces the risk of LBW.
It is concordant with other studies which have shown that educational interventions during pregnancy can be effective in improving the outcomes of pregnancy and birth. These studies have been carried out in different societies with different methods and techniques of health-care education. Most studies found that using adequate antenatal care was significantly associated with a reduced risk of LBW.[18,19] In some of these studies, similar to the results of the present study, it is shown that local and national programs that provide education on nutrition, nutrient supplementation, and social and medical service referrals to pregnant women, and peer-centered prenatal education are effective in empowering women to make pregnancy safer and improving outcomes of pregnancy including decrease in the incidence of LBW.[20,21,22,23]
Most likely, the success of such programs is associated with improving self-care behaviors among pregnant women. Some studies suggested that participation in moderate-to-vigorous physical activity during pregnancy can enhance BW.[2] Moreover, studies have shown that oral health and treatment of periodontitis can lead to a reduction in preterm LBW.[24] Results of an educational intervention aimed at improving dietary intake and weight gain during pregnancy showed also that the rate of LBW was significantly lower among women in the intervention group.[6] According to studies, similar to the results of the present study, pregnant women who participate early (within the first three months of their pregnancy) in prenatal education programs give birth to newborns with higher BW.[18,20]
Strengths and limitations of the study
This is the first study that has applied the HBM to promote self-care behaviors during pregnancy among pregnant Iranian women. We believe that the effectiveness of this educational intervention can be attributed to the use of the HBM as a conceptual framework which can play an important role in enhancing the quality of programs planning for self-care education during pregnancy. This model can identify the factors associated with the beliefs of individuals which influence their behaviors.
This educational program was provided for pregnant women by health-care providers during regular prenatal visits. As the costs of this health-care education program were small, implementation of such programs can be economic and valuable.
Although this study demonstrated that positive effects of self-care education based on the HBM during pregnancy, the effect of the other social and environmental factors on outcomes of birth especially BW remains unknown.
CONCLUSIONS
Self-care education program in early pregnancy could be positively associated with the decreased risk of LBW. Pregnant women should be trained and empowered to contribute positively in making pregnancy safer. Implementation of such programs among pregnant women that do not need major techniques and materials may help to reduce adverse outcomes of pregnancy in developing countries.
ACKNOWLEDGMENT
This study has been funded and supported by the Tehran University of Medical Sciences (TUMS) (grant no: 9397-27-03-88).
Footnotes
Source of Support: This study has been funded and supported by the Tehran University of Medical Sciences; (Grant no: 9397-27-03-88)
Conflict of Interest: The authors report no declarations of interest.
REFERENCES
- 1.New York: UNICEF and WHO; 2004. The United Nations Children's Fund and World Health Organization. Low Birth weight: Country, Regional and Global Estimates; p. 1. [Google Scholar]
- 2.Muthayya S. Maternal nutrition and low birth weight-what is really important? Indian J Med Res. 2009;130:600–8. [PubMed] [Google Scholar]
- 3.Russell RB, Green NS, Steiner CA, Meikle S, Howse JL, Poschman K, et al. Cost of hospitalization for preterm and low birth weight infants in the United States. Pediatrics. 2007;120:e1–9. doi: 10.1542/peds.2006-2386. [DOI] [PubMed] [Google Scholar]
- 4.Muula AS, Siziya S, Rudatsikira E. Parity and maternal education are associated with low birth weight in Malawi. Afr Health Sci. 2011;11:65–71. [PMC free article] [PubMed] [Google Scholar]
- 5.Wallace DA, Dodd MM, McNeil DA, Jocelyn Churchill A, Oelke ND, Arnold SL, et al. A pregnancy wellness guide to enhance care through self-assessment, personal reflection, and self-referral. J Obstet Gynecol Neonatal Nurs. 2009;38:134–47. doi: 10.1111/j.1552-6909.2009.01008.x. [DOI] [PubMed] [Google Scholar]
- 6.Kafatos AG, Vlachonikolis IG, Codrington CA. Nutrition during pregnancy: The effects of an educational intervention program in Greece. Am J Clin Nutr. 1989;50:970–9. doi: 10.1093/ajcn/50.5.970. [DOI] [PubMed] [Google Scholar]
- 7.Gollenberg A, Pekow P, Markenson G, Tucker KL, Chasan-Taber L. Dietary behaviors, physical activity, and cigarette smoking among pregnant Puerto Rican women. Am J Clin Nutr. 2008;87:1844–51. doi: 10.1093/ajcn/87.6.1844. [DOI] [PubMed] [Google Scholar]
- 8.Geneva: World Health Organization; 2004. World Health Organization. Making pregnancy safer: The critical role of the skilled attendant: A joint statement by WHO, ICM and FIGO; p. 1. [Google Scholar]
- 9.Stearns SC, Bernard SL, Fasick SB, Schwartz R, Konrad TR, Ory MG, et al. The economic implications of self-care: The effect of lifestyle, functional adaptations, and medical self-care among a national sample of Medicare beneficiaries. Am J Public Health. 2000;90:1608–12. doi: 10.2105/ajph.90.10.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhuyan KK. BMC Public Health; 2004. Health promotion through self-care and community participation: Elements of a proposed programme in the developing countries; p. 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anya SE, Hydara A, Jaiteh LE. Antenatal care in The Gambia: Missed opportunity for information, education and communication. BMC Pregnancy Childbirth. 2008;8:9. doi: 10.1186/1471-2393-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Modest NN, Tamayose TS. 2th ed. John Wiley and Sons; 2004. Dictionary of public health promotion and education: Terms and concepts; pp. 85–6. [Google Scholar]
- 13.Champion VL, Skinner CS. The Health Belief Model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4th ed. John Wiley and Sons; 2008. pp. 45–65. [Google Scholar]
- 14.Banaem LM, Majlessi F. A comparative study of low 5-minute Apgar scores (<8) in newborns of wanted versus unwanted pregnancies in southern Tehran, Iran (2006-2007) J Matern Fetal Neonatal Med. 2008;21:898–901. doi: 10.1080/14767050802372390. [DOI] [PubMed] [Google Scholar]
- 15.Wasilewski RM, Mateo P, Sidorovsky P. Preventing work-related musculoskeletal disorders within supermarket cashiers: An ergonomic training program based on the theoretical framework of the PRECEDE-PROCEED model. Work (Reading, Mass) 2007;28:23–31. [PubMed] [Google Scholar]
- 16.Grandes G, Sanchez A, Cortada JM, Balague L, Calderon C, Arrazola A, et al. Is integration of healthy lifestyle promotion into primary care feasible? Discussion and consensus sessions between clinicians and researchers. BMC Health Serv Res. 2008;8:213. doi: 10.1186/1472-6963-8-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grjibovski AM, Bygren LO. From the former Soviet Union: Maternal education seems to determine pregnancy outcomes in Russia. BMJ. 2005;331:236. doi: 10.1136/bmj.331.7510.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Krueger PM, Scholl TO. Adequacy of prenatal care and pregnancy outcome. J Am Osteopath Assoc. 2000;100:485–92. [PubMed] [Google Scholar]
- 19.Ngy MH, Nakamura K, Ohinishi M, Kizuki M, Suyama S, Seino K, et al. Improved perinatal health through qualified antenatal care in urban Phnom Penh, Cambodia. Environ Health Prev Med. 2007;12:193–201. doi: 10.1265/ehpm.12.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lazariu-Bauer V, Stratton H, Pruzek R, Woelfel ML. A comparative analysis of effects of early versus late prenatal WIC participation on birth weight: NYS, 1995. Matern Child Health J. 2004;8:77–86. doi: 10.1023/b:maci.0000025730.02966.62. [DOI] [PubMed] [Google Scholar]
- 21.Sachdeva R, Mann SK. Impact of nutrition education and medical supervision on pregnancy outcome. Indian Pediatr. 1993;30:1309–14. [PubMed] [Google Scholar]
- 22.Kotelchuck M, Schwatrz JB, Anderka M, Finison KS. WIC participation and pregnancy outcomes: Massachusetts state wide evaluation project. Am J Public Health. 1984;74:1086–92. doi: 10.2105/ajph.74.10.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford K, Weglicki L, Kershaw T, Schram C, Hoyer PJ, Jacobson ML. Effects of a prenatal care intervention for adolescent mothers on birth weight, repeat pregnancy, and educational outcomes at one year postpartum. J Perinat Educ. 2002;11:35–8. doi: 10.1624/105812402X88588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Agueda A, Echeverria A, Manau C. Association between periodontitis in pregnancy and preterm or low birth weight: Review of the literature. Med Oral Patol Oral Cir Bucal. 2008;13:E609–15. [PubMed] [Google Scholar]


