Summary:
Enterolith is a rare cause of afferent loop obstruction following Billroth II gastrectomy. We report a case of acute afferent loop syndrome (ALS) due to a huge enterolith, necessitating prompt surgery. The clinical pattern may mimic acute cholangitis and/or pancreatitis. Delayed diagnosis may result in severe complications such as bowel ischemia or perforation. Only 14 reported cases of enterolith causing afferent loop obstruction were found in the English literature.
Keywords: Acute afferent loop syndrome, Enterolith, Billroth II
Introduction
Afferent loop syndrome (ALS) is a rare complication of Billroth-II gastrojejunostomy, Roux-en-Y gastroenterotomy, and Whipple’s operation. ALS are classically distinguished in chronic and acute. Several causes, such as adhesions, intussusception, strictures, malignancy, and internal hernias, have been attributed to the mechanical obstruction of the afferent loop (1). Rarely this syndrome occurs in relation to an enterolith impacted in the afferent loop (2). We describe a case of acute ALS caused by an enterolith developed in the afferent loop of Billroth II anastomosis.
Case report
A 80-yr-old man was admitted to a hospital for severe upper abdominal pain associated with nausea and fever. Physical examination revealed a distended abdomen with right upper quadrant tenderness and jaundice. The patient had undergone a Billroth II partial gastrectomy for benign ulcer 27 years before. Laboratory tests showed an elevated white blood cell count of 15,000/mm3, biliary stasis and pancreatitis (bilirubin 4.8 mg/dL - direct 3,5 mg/dL; GGT 213 mU/mL; alkaline phosphatase 521 mU/mL; amylase 1,512 U/L). The preliminary diagnosis was pancreatitis and acute cholangitis. An appropriate therapy was started. In the following few hours, no symptom relief was observed and the patient’s condition made worse.
Abdominal computed tomography (CT) showed dilatation of both the main pancreatic duct and the biliary duct (Fig. 1), and a huge stone in the dilated duodenal afferent loop (Fig. 2). The pancreas was normal and no gallstones were found in the gallbladder. The diagnosis of acute afferent loop obstruction by enterolith was made. Urgent laparotomy was planned.
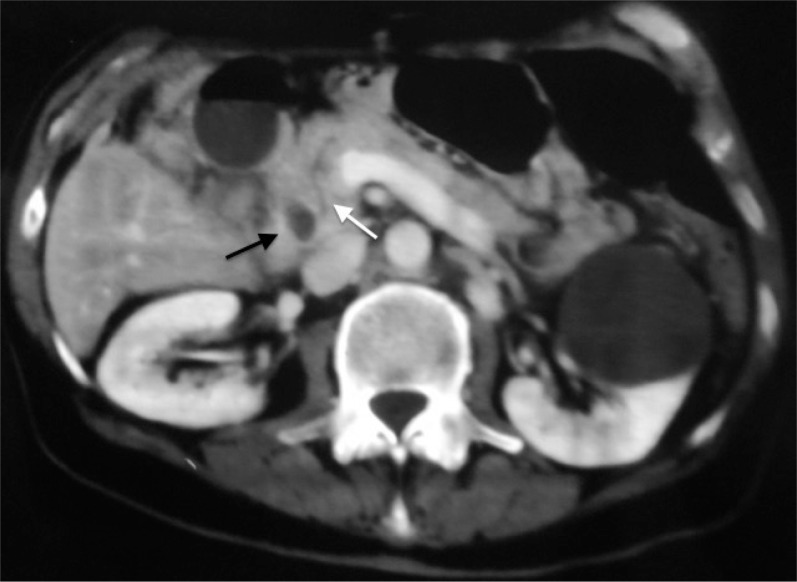
Fig. 1.
Abdominal CT - Dilated common bile duct (black arrow) and main pancreatic duct (white arrow).
Fig. 2.
Abdominal CT - A large incarcerated enterolith in the dilated afferent loop.
Abdominal exploration revealed dilatation of the duodenum without signs of ischemia and an entrapment of the afferent loop by extensive adhesions, causing kinks, particulary at the anastomosis site. Adhesiolysis was carried out and a greenish stone measuring 5 × 6 cm was removed through a longitudinal cut in the second portion of duodenum. The enterolith was ovoid in shape and composed mainly of cholesterol and bile salts.
The postoperative course was uneventful and the patient was discharged home 9 days after surgery.
Discussion
Afferent loop syndrome is a relatively uncommon complication encountered after gastrectomy and Billroth II reconstruction (3). The incidence reported in literature ranges between 0,2% and 20% (4); with modern surgical techniques it has been reduced to 0,3% (5,6). The afferent loop syndrome has been attributed to the stasis of biliary, pancreatic and intestinal secretions in the afferent loop. When the pressure within the afferent loop exceeds the resistant threshold of the obstruction, its content is then propelled into the stomach to cause sudden bilious vomiting and so pain is relieved. It is usually caused by adhesions, internal hernias, volvulus, intussusception, intestinal kinks/strictures, a long afferent loop and malignancy (2).
ALS may present as an acute syndrome, caused by complete obstruction of the afferent loop. Clinically, the acute form is characterized by abrupt onset of upper abdominal pain and rapid clinical deterioration. It usually develops within the first week after surgery, mainly due to retrograde intussusception, technical error in constructing the gastrojejunostomy, or kinking or edema at the anastomotic site (7). Rarely, as in our case, this syndrome occurs many years after surgery and also in relation to an enterolith (3,4). Most of the enteroliths have been reported in association with diverticula of the small intestine, Crohn’s disease or tuberculosis of the small bowel (3). The formation of enteroliths requires intestinal stasis. The chronically obstructed blind afferent loop promote bacterial overgrowth, resulting in bile salt deconjugation. Precipitation of insoluble bile acids within the bowel lumen leads to the development of stones and sludge (8). Complications of enteroliths include inflammation, perforation, and obstruction. If impaction at the stenotic site occurs, the obstruction becomes total; no vomiting occurs and epigastric pain is persistent (7). In our patient, stasis within the afferent loop from adhesions was responsible for the formation of the enterolith. However, duodenal motility disorder due to altered food passage and changes in cholecystokinin secretion may account for formation of the enterolith (9).
Only 14 cases of an enterolith causing afferent loop obstruction have been reported in the English literature (1,2). All patients presented with symptoms of abdominal pain. Jaundice and cholangitis are often present (2). The increased pressure within the duodenum may provoke biliary and pancreatic duct dilatation. The reflux of intestinal content in pancreatic ducts consequently activating pancreatic enzymes can cause acute pancreatitis. In addition, serum amylase level may increase in situations of strangulated or necrotic bowel (10). Early diagnosis is mandatory to prevent life-threatening complications such as afferent loop perforation (11). The mortality rate reported before the development of CT or ultrasound (US) was high (30–60%) (12).
The clinical diagnosis can be difficult. Symptoms are non-specific and can address towards acute pancreatitis (11) and cholangitis (1,13). These circumstances may result in non operative management or delayed intervention with lethal results. Plain abdominal X-rays offer little for the diagnosis because the afferent loop is fluid - filled and gasless owing total obstruction (14). Enteroliths forming in an afferent limb are more likely to be radiolucent and less likely identifiable on plain radiographs (2). An upper gastrointestinal series can be helpful to the diagnosis because of poor filling or non filling of the afferent jejunal limb (12); but 20% of normal afferent loops are not opacified (15). Ultrasound (US), used as initial diagnostic procedure in patients with acute abdominal symptoms, may demonstrate a enterolith in a large and dilated bowel loop (2,13). However, its differentiation from a pancreatic pseudocyst (14) or cholecystolithiasis (2,16)can be difficult. CT appearance of afferent loop syndrome is usually characteristic, if not pathognomonic (17). In our case, CT allowed the diagnosis. CT shows U-shaped, liquid filled, tubular structure, which does not opacify with oral contrast and usually surrounds the head of pancreas (5). The valvulae conniventes projecting into the lumen are a common feature. Additional findings include complications of afferent loop syndrome such as biliary dilatation, pancreatitis and enteroliths (15). Multidetector-row computed tomography (MDCT) with coronal plane similar to the human anatomy is believed better than conventional CT in diagnosing site, level, and cause of ALS (18).
Early explorative laparoscopy is optimal option, when the diagnosis remains unclear (19). Acute afferent loop syndrome is a true surgical emergency (5). Preoperative direct percutaneous decompression of the afferent limb using ultrasound guidance can stabilize patients with sepsis and decrease surgical morbidity and mortality. In these cases, through the drainage catheter, it is possible a radiological study of the afferent loop and the percutaneus removal of the enterolith (2). The endoscopic extraction is difficult (1,3,20) and may lead to perforation (20). Using electrohydraulic lithotripsy endoscopic removal of the enterolith is feasible (6). Surgery consists in decompression of the obstructed loop and in removal of the stone through an enterotomy. In case of hemodynamic instability an external drainage of the duodenal stump using Foley catheter can be a temporary treatment (5). Surgical revision of any anatomical pathology predisposing the stasis of the afferent loop must be done to avoid recurrence. This may require adhesiolysis, stricturoplasty of the anastomosis, resection of stenotic segment, resection of the redundant portion of the afferent loop, conversion of a Billroth II to a Billroth I anastomosis, Braun entero-entero anastomosis between afferent and efferent loops or duodenum bypassed with a Roux- en-Y technique (2,4).
Conclusion
Acute obstruction of the afferent loop should be strongly suspected in patients with a history of Billroth II gastrectomy and symptoms suggestive of acute cholangitis or pancreatitis, especially when there is no clinical improvement after initial treatment. Although rarely, an enterolith can be the cause of obstruction. Early diagnosis and prompt surgery can improve the prognosis.
References
- 1.Su PY, Yen HH, Chen YY. An Unusual Cause of Abdominal Pain in a 86-Year-Old Woman. Gastroenterology. 2012;142(1):e24–5. doi: 10.1053/j.gastro.2011.01.070. [DOI] [PubMed] [Google Scholar]
- 2.Lee Michael C, Bui James T, Knuttinen M-Grace, Gaba Ron C, Scott Helton W, Owens Charles A. Enterolith Causing Afferent Loop Obstruction: A Case Report and Literature Review. Cardiovasc Intervent Radiol. 2009;32(5):1091–6. doi: 10.1007/s00270-009-9561-3. [DOI] [PubMed] [Google Scholar]
- 3.Carbognin G, Biasutti C, El-Khaldi M, Ceratti S, Procacci C. Afferent loop syndrome presenting as enterolith after Billroth II subtotal gastrectomy: a case report. Abdom Imaging. 2000;25(2):129–31. doi: 10.1007/s002619910030. [DOI] [PubMed] [Google Scholar]
- 4.Mitty WF, Jr, Grossi C, Nealon TF., Jr Chronic afferent loop syndrome. Ann Surg. 1970;172(6):996–1001. doi: 10.1097/00000658-197012000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ballas KD, Rafailidis SE, Konstantinidis HD, Pavlidis TE, Marakis GN, Anagnostara E, Sakadamis AK. Acute afferent loop syndrome: a true emergency A case report. Acta chirurgica Belgica. 2009;1:101–103. doi: 10.1080/00015458.2009.11680382. 109. [DOI] [PubMed] [Google Scholar]
- 6.Kim HJ, Moon JH, Choi HJ, Koo HC, Park SJ, Cheon YK, Cho YD, Lee MS, Shim CS. Endoscopic removal of an enterolith causing afferent loop syndrome using electrohydraulic lithotripsy. Dig Endosc. 2010;22(3):220–2. doi: 10.1111/j.1443-1661.2010.00981.x. [DOI] [PubMed] [Google Scholar]
- 7.Yao NS, Wu CW, Tiu CM, Liu JM, Whang-Peng J, Chen LT. Percutaneous Transhepatic Duodenal Drainage as an AlternativeApproach in Afferent Loop Obstruction with Secondary Obstructive Jaundice in Recurrent Gastric Cancer. Cardiovasc Intervent Radiol. 1998;21(4):350–3. doi: 10.1007/s002709900277. [DOI] [PubMed] [Google Scholar]
- 8.Yavuz N, Ergüney S, Ogüt G, Alver O. Enteroliths developed in a chronically obstructed afferent loop coexisting with gastric remnant carcinoma: Case report and review of the literature. J Gastroenterol Hepatol. 2006;21(3):495–8. doi: 10.1111/j.1440-1746.2006.04284.x. [DOI] [PubMed] [Google Scholar]
- 9.Tien Yu-Wen, Lee Po-Huang, Chang King-Jen. Enterolith: An Unusual Cause of Afferent Loop Obstruction. Am J Gastroenterol. 1999;94(5):1391–2. doi: 10.1111/j.1572-0241.1999.01092.x. [DOI] [PubMed] [Google Scholar]
- 10.McMaster P, Wijetunge DB. Postgastrectomy afferent loop obstruction due to efferent loop herniation simulating acute pancreatitis. Br J Surg. 1976;63:526–527. doi: 10.1002/bjs.1800630708. [DOI] [PubMed] [Google Scholar]
- 11.Kaya E, Senyurek G, Dervisoglu A, Danaci M, Kesim M. Acute pancreatitis caused by afferent loop herniation after Billroth IIgastrectomy: report of a case and review of the literature. Hepato-gastroenterology. 2004;51:606–608. 56; [PubMed] [Google Scholar]
- 12.Aoki M, Saka M, Morita S, Fukagawa T, Katai H. Afferent Loop Obstruction After Distal Gastrectomy with Roux-en-Y Reconstruction. World J Surg. 2010;34(10):2389–92. doi: 10.1007/s00268-010-0602-5. [DOI] [PubMed] [Google Scholar]
- 13.Capaccio E, Zuccarino F, Gauglio C, Pretolesi F, Derchi LE. Acute obstruction of the afferent loop caused by an enterolith. Emerg Radiol. 2007;13(4):201–3. doi: 10.1007/s10140-006-0504-x. [DOI] [PubMed] [Google Scholar]
- 14.Lee DH, Lim JH, Ko YT. Afferent loop syndrome: sonographic finding in seven cases. AJR Am J Roentgenol. 1991;157(1):41–3. doi: 10.2214/ajr.157.1.2048535. [DOI] [PubMed] [Google Scholar]
- 15.Gayer G, Barsuk D, Hertz M, Apter S, Zissin R. CT diagnosis of afferent loop syndrome. Clin. Radiol. 2002;57(9):835–9. [PubMed] [Google Scholar]
- 16.Morse JM, Lakshman S, Thomas E. “Pseudogallbladder” appearance in partial afferent loop obstruction in a patient with cholecystectomy. South Med J. 1986;79(8):1030–3. doi: 10.1097/00007611-198608000-00030. [DOI] [PubMed] [Google Scholar]
- 17.Gale ME, Gerzof SG, Kiser LC, Snider JM, Stavis DM, Larsen CR, Robbins AH. CT Appearance of Afferent Loop Obstruction. AJR Am J Roentgenol. 1982;138(6):1085–8. doi: 10.2214/ajr.138.6.1085. [DOI] [PubMed] [Google Scholar]
- 18.Juan YH, Yu CY, Hsu HH, Huang GS, Chan DC, Liu CH, Tung HJ, Chang WC. Using Multidetector-Row CT for the Diagnosis of Afferent Loop Syndrome Following Gastroenterostomy Reconstruction. Yonsei Med J. 2011;52(4):574–80. doi: 10.3349/ymj.2011.52.4.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vettoretto N, Pettinato G, Romessis M, Bravo AF, Barozzi G, Giovanetti M. Laparoscopy in Afferent Loop Obstruction Presenting as Acute Pancreatitis. JSLS. 2006;10(2):270–4. [PMC free article] [PubMed] [Google Scholar]
- 20.Sartori N, Falconi M, Contro C, Bassi C, Pederzoli P. Symptomatic stone in the duodenum after gastrectomy. Surgery. 2001;129(2):238–9. doi: 10.1067/msy.2001.104534. [DOI] [PubMed] [Google Scholar]