Abstract
Acute abdominal pain is a common complaint in childhood, and it can be caused by a wide range of underlying surgical and non-surgical conditions. The most common non-surgical condition is gastroenteritis, while the most common surgical condition is appendicitis. Abdominal pain in children varies with age, associated symptoms, and pain location. Although acute abdominal pain is usually benign and self-limiting, there are uncommon but life-threatening conditions that require urgent care. Meticulous history taking and physical examinations are essential to determine the cause of acute abdominal pain and to identify children with surgical conditions such as appendicitis.
Keywords: Abdominal pain, Acute abdominal, Appendicitis, Child
INTRODUCTION
Acute abdominal pain is one of the most common complaints in children, and it poses a diagnostic challenge owing to the variety of underlying causes. Acute abdominal pain is usually a self-limiting, benign condition, such as in gastroenteritis, constipation, or viral illness [1]. However, the challenge for the physician is to identify children who have uncommon and potentially life-threatening conditions that require urgent evaluation and treatment, such as appendicitis, intussusception, volvulus, or adhesion [1,2]. The frequency of surgical intervention in patients presenting with acute abdominal pain is around 1% [3], but the possibility of overlooking a serious organic etiology is a major concern for physicians. Unfortunately, a small number of patients with acute abdominal pain may not receive a definitive diagnosis on first evaluation because of the early stage of the disease or subtle and atypical signs [3]. It is important to understand that accurate and timely diagnosis is the key to preventing significant morbidity and mortality. This article provides a review of the pathogenesis, etiology, clinical evaluation, and management of children with acute abdominal pain.
PATHOGENESIS
Abdominal pain may be classified as visceral, somatoparietal, and referred pain according to the nature of the pain receptors involved. Interestingly, most abdominal pain is associated with visceral pain receptors [4].
Visceral pain receptors are located on the serosal surface, in the mesentery, within the intestinal muscle, and the mucosa of hollow organs. These pain receptors respond to mechanical and chemical stimuli, such as stretching, tension, and ischemia. Because visceral pain fibers are unmyelinated C-fibers, and enter the spinal cord bilaterally at several levels, visceral pain is usually dull, poorly localized, and perceived in the midline. In addition, there are three broad pain areas with anatomic associations. Pain emanating from foregut structures (e.g., lower esophagus, stomach) is felt in the epigastric area, pain from midgut structures (e.g., small intestine) is felt in the periumbilical area, and pain from hindgut structures (e.g., colon) is felt in the lower abdomen.
Somatoparietal pain receptors are located in the parietal peritoneum, the muscle, and the skin. Pain resulting from inflammation, stretching, or tearing of the parietal peritoneum is transmitted through myelinated A-δ fibers to specific dorsal root ganglia. Somatoparietal pain is characterized by sharp, more intense, and more localized sensation. Movement may aggravate the pain; thus, the child will stay still.
Referred pain is well localized but felt in distant areas of the same cutaneous dermatome as the affected organ. It results from shared spinal cord level for afferent neurons from different sites. For example, inflammatory conditions that affect the diaphragm can be perceived as pain in the shoulder or lower neck area [4,5].
ETIOLOGY
The causes of acute abdominal pain in children are listed in Table 1. A wide range of surgical and non-surgical conditions can cause acute abdominal pain in children. A brief discussion of some life-threatening and common causes of acute abdominal pain follows.
Table 1.
Causes of Acute Abdominal Pain in Children
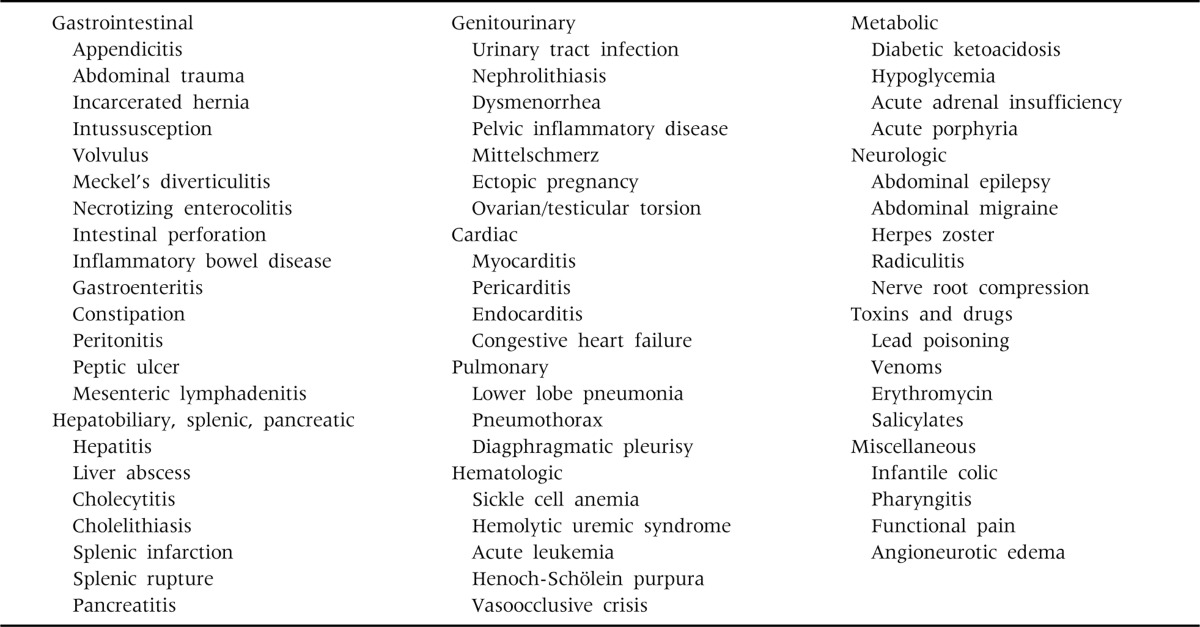
Life-threatening causes of abdominal pain often result from hemorrhage, obstruction, or perforation of the gastrointestinal tract or intra-abdominal organs, and may be associated with specific clinical features [2,4]. Extra-abdominal causes of abdominal pain (e.g., diabetic ketoacidosis, hemolytic uremic syndrome, and myocarditis) also have other distinguishing clinical features. Common causes of abdominal pain include gastroenteritis, constipation, systemic viral illness, infections outside of the gastrointestinal tract (e.g., streptococcal pharyngitis, lower lobe pneumonia, and urinary tract infection), mesenteric lymphadenitis, and infantile colic [1, 5-7].
Acute appendicitis
Acute appendicitis is the most common surgical cause of acute abdominal pain in children [4,7]. Typically, children with appendicitis present with visceral, vague, poorly localized, periumbilical pain. Within 6 to 48 hours, the pain becomes parietal as the overlying peritoneum becomes inflamed. The pain manifests itself as a well-localized pain in the right lower quadrant. However, some of these characteristic manifestations are frequently absent, particularly in younger children [8]. Therefore, physicians should consider the diagnosis of appendicitis in all cases of previously healthy children who have a history of abdominal pain and vomiting, with or without fever or focal abdominal tenderness [8,9].
Abdominal trauma
Abdominal trauma may cause hemorrhage or laceration of solid organs, bowel perforation, organ ischemia from vascular injury, and intramural hematoma. Blunt abdominal trauma is more common than penetrating injury. Typical mechanisms of trauma include motor vehicle accidents, falling down, and child abuse.
Intestinal obstruction
Intestinal obstruction may produce a characteristic cramping pain. This clinical feature is usually associated with serious intra-abdominal conditions that require urgent diagnosis and treatment. Causes of intestinal obstruction include intussusception, malrotation with midgut volvulus, necrotizing enterocolitis, incarcerated inguinal hernia, and postoperative adhesions [7].
Gastroenteritis
Gastroenteritis is the most common medical condition of abdominal pain in children [10]. Children with acute gastroenteritis may develop fever, severe cramping abdominal pain, and diffuse abdominal tenderness before diarrhea begins. Viruses including rotavirus, Norwalk virus, adenovirus, and enterovirus are the most frequent causes [10]. Bacteria and parasites can also cause acute abdominal pain in children.
Constipation
Children with constipation often present with fecal impaction and severe lower abdominal pain. Constipation is likely in children with at least two of the following characteristics: fewer than three stools weekly, fecal incontinence, large stools palpable in the rectum or through the abdominal wall, retentive posturing, or painful defecation [11].
Mesenteric lymphadenitis
Because mesenteric lymph nodes are usually in the right lower quadrant, this condition sometimes mimics appendicitis, except the pain is more diffuse. Often, signs of peritonitis are absent. In one series of 70 children with clinically suspected acute appendicitis, 16% had a final diagnosis of mesenteric lymphadenitis established by ultrasound, clinical course, or surgery [12]. Etiologies of mesenteric lymphadenitis include viral and bacterial gastroenteritis, inflammatory bowel disease, and lymphoma; viral infection is most common.
Infantile colic
Infants with colic, particularly those with hypertonic characters, may have severe abdominal pain. Typically, infants with colic show paroxysmal crying and draw their knees up against their abdomen. Colic is relieved with the passage of flatus or stool during the first three to four weeks of life.
CLINICAL EVALUATION
In the evaluation of a child with acute abdominal pain, the most important components are careful history taking and repeated physical examinations. Selective use of appropriate laboratory and radiological investigations may be necessary to establish a specific diagnosis. However, the diagnosis may remain uncertain despite a thorough initial evaluation process. Children with acute abdominal pain should be detained in an emergency department with serial physical examinations to clarify any diagnostic uncertainty.
History taking
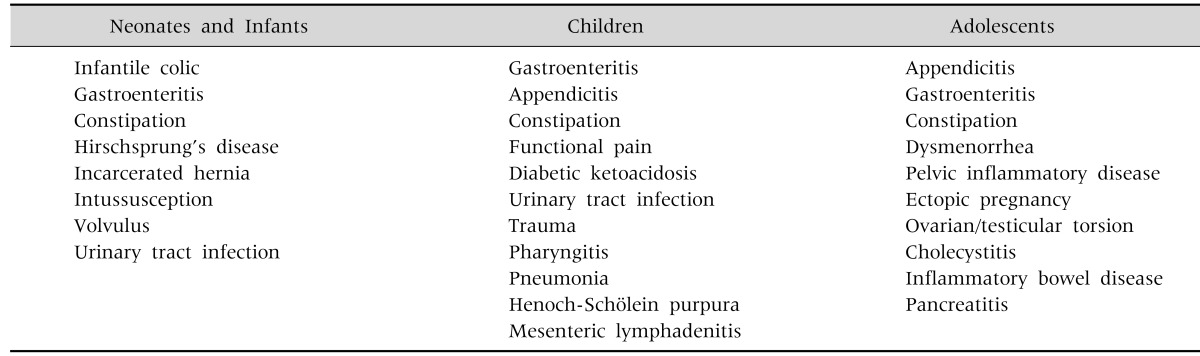
Important details of the history include symptom onset pattern, progression, location, intensity, characters, precipitating and relieving factors of abdominal pain, and associated symptoms. Age of the patient is a key factor in the evaluation of acute abdominal pain as listed in Table 2. Other important historical variables include recent abdominal trauma, previous abdominal surgery, and a thorough review of systems [4-6,10].
Table 2.
Differential Diagnosis of Acute Abdominal Pain by Predominant Age
Pain relief after a bowel movement suggests a colonic condition, and improvement in pain after vomiting may occur with conditions localized to the small bowel. In surgical abdomen, abdominal pain generally precedes vomiting, and vomiting precedes abdominal pain in medical conditions. Any infants and children presenting with bilious vomiting should be presumed to have bowel obstruction.
Physical examinations
Careful physical examination is essential for accurate diagnosis in children with acute abdominal pain. Examination of external genitalia, testes, anus, and rectum should be included as part of the evaluation for abdominal pain. In addition, pelvic examination is important in sexually active female adolescents.
General appearance
Children with peritoneal irritation remain still or resist movement, while patients with visceral pain change position frequently, often writhing with discomfort.
Vital signs
Vital signs are useful in assessing hypovolemia and provide useful clues for diagnosis. Fever indicates an underlying infection or inflammation including acute gastroenteritis, pneumonia, pyelonephritis, or intra-abdominal abscess. Tachypnea may indicate pneumonia. Tachycardia and hypotension suggest hypovolemia or third-space volume loss.
Abdominal examination
The evaluating physician should gently palpate the abdomen moving toward the area of maximal tenderness. The physician has to make efforts to determine the degree of abdominal tenderness, location, rebound tenderness, rigidity, distension, masses, or organomegaly. A rectal examination provides useful information about sphincter tone, presence of masses, stool nature, hematochezia, or melena [13].
Investigations
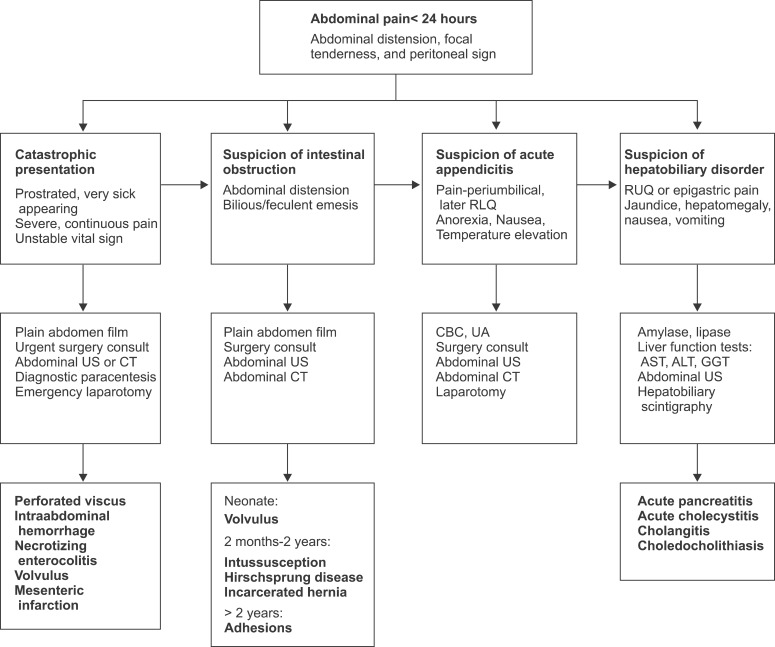
Specific laboratory studies and radiologic evaluation are helpful to assess the patient's physiological status and to make an accurate diagnosis [14]. A complete blood cell count and a urinalysis are generally indicated in all patients with acute abdominal pain. Measurement of serum glucose and electrolytes helps in evaluating the patient's hydration status and acid-base balance. A pregnancy test should be performed in postmenarcheal girls. An algorithmic approach to children with acute abdominal pain requiring urgent intervention is presented in Fig. 1.
Fig. 1.
Algorithmic approach to the children with acute abdominal pain requiring urgent management. RLQ: right lower quadrant, RUQ: right upper quadrant, US: ultrasonography, CT: computed tomography, CBC: complete blood count, UA: urinalysis, AST: aspartate aminotransferase, ALT: alanine aminotransferase, GGT: γ-glutamyltransferase.
Plain abdominal radiographs are helpful if intestinal obstruction or perforation is suspected. Chest radiographs may help rule out pneumonia. In the emergency department, ultrasound and computed tomography are widely used to identify the cause of abdominal pain [12,15-17]. Although computed tomography is more accurate than ultrasound, ultrasound is the preferred imaging modality for an initial evaluation of many potential causes of pediatric abdominal pain because it is noninvasive, radiation-free, and less expensive modality [17].
MANAGEMENT
Treatment should be directed at the underlying cause of abdominal pain. As depicted in Fig. 1, urgent intervention and management is required for children who are prostrated and sick-appearing, have signs of bowel obstruction and evidence of peritoneal irritation. Initial resuscitation measures include correction of hypoxemia, replacement of intravascular volume loss, and correction of metabolic abnormalities. Gastric decompression using nasogastric tube may be necessary if there is bowel obstruction. Empirical intravenous antibiotics are often indicated when there is clinical suspicion of a serious intra-abdominal infection. Moreover, adequate analgesics should be provided to patients with severe pain, preferably prior to surgical evaluation [18].
CONCLUSION
Acute abdominal pain is one of the most common complaints in childhood, and one that frequently requires rapid diagnosis and treatment in the emergency department. Although acute abdominal pain is typically self-limiting and benign, there are potentially life-threatening conditions that require urgent management, such as appendicitis, intussusception, or bowel obstruction. Meticulous history taking and repeated physical examinations are essential to determine the cause of acute abdominal pain and to identify children with surgical conditions.
References
- 1.D'Agostino J. Common abdominal emergencies in children. Emerg Med Clin North Am. 2002;20:139–153. doi: 10.1016/s0733-8627(03)00055-5. [DOI] [PubMed] [Google Scholar]
- 2.Grant HW, Parker MC, Wilson MS, Menzies D, Sunderland G, Thompson JN, et al. Adhesions after abdominal surgery in children. J Pediatr Surg. 2008;43:152–156. doi: 10.1016/j.jpedsurg.2007.09.038. [DOI] [PubMed] [Google Scholar]
- 3.Scholer SJ, Pituch K, Orr DP, Dittus RS. Clinical outcomes of children with acute abdominal pain. Pediatrics. 1996;98:680–685. [PubMed] [Google Scholar]
- 4.Ross A, LeLeiko NS. Acute abdominal pain. Pediatr Rev. 2010;31:135–144. doi: 10.1542/pir.31-4-135. [DOI] [PubMed] [Google Scholar]
- 5.Leung AK, Sigalet DL. Acute abdominal pain in children. Am Fam Physician. 2003;67:2321–2326. [PubMed] [Google Scholar]
- 6.Reynolds SL, Jaffe DM. Diagnosing abdominal pain in a pediatric emergency department. Pediatr Emerg Care. 1992;8:126–128. doi: 10.1097/00006565-199206000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Carty HM. Paediatric emergencies: non-traumatic abdominal emergencies. Eur Radiol. 2002;12:2835–2848. doi: 10.1007/s00330-002-1499-7. [DOI] [PubMed] [Google Scholar]
- 8.Kwok MY, Kim MK, Gorelick MH. Evidence-based approach to the diagnosis of appendicitis in children. Pediatr Emerg Care. 2004;20:690–698. doi: 10.1097/01.pec.0000142957.34501.8d. [DOI] [PubMed] [Google Scholar]
- 9.Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE. Does this child have appendicitis? JAMA. 2007;298:438–451. doi: 10.1001/jama.298.4.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mason JD. The evaluation of acute abdominal pain in children. Emerg Med Clin North Am. 1996;14:629–643. doi: 10.1016/s0733-8627(05)70271-6. [DOI] [PubMed] [Google Scholar]
- 11.Loening-Baucke V, Swidsinski A. Constipation as cause of acute abdominal pain in children. J Pediatr. 2007;151:666–669. doi: 10.1016/j.jpeds.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Vignault F, Filiatrault D, Brandt ML, Garel L, Grignon A, Ouimet A. Acute appendicitis in children: evaluation with US. Radiology. 1990;176:501–504. doi: 10.1148/radiology.176.2.2195594. [DOI] [PubMed] [Google Scholar]
- 13.Kristinsson G, Wall SP, Crain EF. The digital rectal examination in pediatric trauma: a pilot study. J Emerg Med. 2007;32:59–62. doi: 10.1016/j.jemermed.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 14.Kwan KY, Nager AL. Diagnosing pediatric appendicitis: usefulness of laboratory markers. Am J Emerg Med. 2010;28:1009–1015. doi: 10.1016/j.ajem.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 15.Soundappan SV, Holland AJ, Cass DT, Lam A. Diagnostic accuracy of surgeon-performed focused abdominal sonography (FAST) in blunt paediatric trauma. Injury. 2005;36:970–975. doi: 10.1016/j.injury.2005.02.026. [DOI] [PubMed] [Google Scholar]
- 16.Reich JD, Brogdon B, Ray WE, Eckert J, Gorell H. Use of CT scan in the diagnosis of pediatric acute appendicitis. Pediatr Emerg Care. 2000;16:241–243. doi: 10.1097/00006565-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Saito JM. Beyond appendicitis: evaluation and surgical treatment of pediatric acute abdominal pain. Curr Opin Pediatr. 2012;24:357–364. doi: 10.1097/MOP.0b013e328352704e. [DOI] [PubMed] [Google Scholar]
- 18.Nissman SA, Kaplan LJ, Mann BD. Critically reappraising the literature-driven practice of analgesia administration for acute abdominal pain in the emergency room prior to surgical evaluation. Am J Surg. 2003;185:291–296. doi: 10.1016/s0002-9610(02)01412-5. [DOI] [PubMed] [Google Scholar]