Abstract
The purpose of this study was to examine utilization and growth in echocardiography among the general population of Ontario between 2001 and 2009. The age- and sex-adjusted rates of echocardiography grew from 39.1 per 1,000 persons in 2001 to 59.9 per 1,000 persons in 2009, for an annual rate of increase of 5.5%. Repeat echocardiograms increased at a rate of 10.6% per year and accounted for 25.3% of all procedures in 2009 as compared to 18.5% in 2002. While significant increases in echocardiography utilization were observed, opportunities may exist to improve the clinical utility of the echocardiograms performed in Ontario.
Keywords: echocardiography, resource utilization, cardiovascular imaging
Introduction
The rapid increase in utilization of imaging procedures has received substantial attention from both researchers and policymakers.(1) In particular, the utilization of echocardiography has grown at an extremely high rate in both the United States and Canada. (2-6) Recent studies of utilization using claims from the United States Veteran's Administration and Medicare plans have attributed the majority of the growth in echocardiography to increased enrollment in their health plans and variations in disease prevalence. Nonetheless, there has been ongoing concern that increases in utilization may also be influenced by a number of non-clinical or system-related factors, such as fee for service incentives,(7,8) increased availability,(3,8) duplicate imaging, (1) and increased physician reliance on technology. (9) In response to such concerns of overuse, the American College of Cardiology Foundation (ACCF), in conjunction with the American Society of Echocardiography and other societies, published Appropriate Use Criteria (AUC) for echocardiography, which are currently being evaluated for usability. (10-13)
The province of Ontario provides universal coverage for healthcare to its residents, so is less subject to the enrollment shifts of large United States insurers. Furthermore, the prevalence of cardiovascular disease has remained relatively stable over the past decade in Canada. (14) The purpose of this study was to examine the utilization of echocardiography and frequency of repeat studies among the general population of Ontario. We hypothesized that there would be significant growth in echocardiography utilization between 2001 and 2009 despite a relatively stable rate of cardiovascular disease during this period. (14,15) We explored factors that might influence utilization including indication, geography, and physician supply.
Methods
Study Design and Data Sources
We conducted a population-based, repeated cross sectional study of all outpatient echocardiograms performed in Ontario between 2001 and 2009. Our primary data source was the Ontario Health Insurance Plan (OHIP) administrative database. The OHIP database contains claims submitted for all outpatient services, including echocardiography, covered by the Ontario Ministry of Health and Long-Term Care. (2) The Registered Persons Database (RPDB) was used to obtain demographic information including age, gender, and geographic location. Patients' postal codes of residence from the RPDB were linked to the Census Area Profile using the Postal Code Conversion File to obtain median neighborhood income and urban density. Hospitalizations were determined using the Canadian Institutes Health Information (CIHI) database. Physician specialty was assessed using the Ontario Physician Human Resource Data Centre (OPHRDC) database.
Echocardiography Utilization Assessment
We included transthoracic echocardiograms billed to OHIP between January 2001 and December 2009. Echocardiography utilization was assessed by the technical component of the billing codes for one- and two- dimensional transthoracic echocardiograms (G560, G566, G570, G574). (2,16) Prior to 2006, echocardiography was covered under the global hospital budget for inpatients and was not available in the OHIP database. (6) For this reason, we only included outpatient echocardiography in this study. Other exclusion criteria included echocardiography billed after the beneficiary was deceased; echocardiography with an associated claim to OHIP that was not reimbursed; and echocardiography performed on individuals less than 18 years of age. We did not include transesophageal echocardiography as these are invasive tests. To avoid duplicate claims, only one echocardiogram was counted per individual in a given day.
An echocardiogram was considered to be a repeat test if another test had been performed in the 365 days before the index test. Because we considered studies starting on January 1, 2001, we examined the frequency of repeat studies beginning in 2002.
Demographic information
Individual demographic information was obtained at the time of echocardiogram. Average neighborhood income was based on census tract and categorized into quintiles. Urban density was categorized as rural if the population was less than 10,000. (17) Regional variation was assessed using fourteen geographically-defined Local Health Integration Networks (LHINs) in Ontario. (18) LHINs were developed by the government to allow for local planning and funding of health care services to a population residing in a specific geographic region. These networks cover the entire province and vary in population size from 180,000 to 1.3 million.
For each individual, we assessed if a hospitalization occurred in the 30 days prior to the time of echocardiography. In addition, we determined if a cardiology consultation took place either 30 days before or 30 days after the procedure, based on an OHIP claim from a physician encounter.
Physician specialty in the OPHRDC database was based on the type of care that is primarily delivered by the physician. (19) The specialty of the billing physician was dichotomized as cardiac specialist and other specialties. Non-cardiac specialists were then categorized as internal medicine, family physician or general practitioner, radiology, and other.
We determined the top ten most common indications for echocardiography during the study period. Diagnosis codes for procedure claims submitted to OHIP are three digits and based on the International Classification of Diseases, Eight Revision (ICD-8) coding system. (20)
Statistical Analysis
The number of echocardiograms performed in each calendar year was determined and characteristics compared across years using χ2 test for categorical variables and analysis of variance (ANOVA) for continuous variables. Rates of echocardiography were calculated by dividing the number of studies by the population of Ontario in a specific year and estimated per 1,000 individuals. Rates were standardized with age and gender adjustment to the 2006 Ontario population using the direct standardization method. Average changes in echocardiography rates and repeat echocardiography rates in the population were calculated using a negative binomial regression model.
Change in number of echocardiograms by physician specialty during the period was calculated by dividing the number of studies performed in 2009 by the number of studies performed in 2001. We divided the change in number of echocardiograms for each specialty by the total provincial change in studies during this period to determine the amount of growth that was attributable to each physician specialty. Rates of echocardiography and repeat echocardiography by physician specialty were calculated by dividing the number of procedures performed by the number of physicians who had billed at least one claim. Annual change in number of physicians and number and rate of echocardiography by physician specialty were calculated using a negative binomial regression model.
We determined the age- and gender-adjusted rates for total and repeat echocardiography studies for each of the fourteen LHINs. The difference across LHINs in a given year was determined by dividing the rate of echocardiography in the region with the highest rate in that year by the region with the lowest in that year to calculate an extremal quotient. (21) We evaluated the average change in extremal quotient using linear regression with year as the independent variable.
P <.05 was considered statistically significant and all tests were 2-sided. Statistical analyses were performed using SAS 9.2 (Cary, NC) and Stata 10 (StataCorp, College Station, TX).
Results
Between 2001 and 2009, there were 4,844,483 outpatient OHIP claims for echocardiograms. After exclusion of claims with no reimbursement, children, repeat procedures on the same day, billing date after death date or missing gender or postal code information, 4,234,166 echocardiograms were included in our study.
The mean age of Ontario patients at the time of an echocardiogram was 59.5 years with a slight increase during the 9 year study period (Table 1). There was also an increase in the percent of echocardiograms performed on individuals who were male and from urban regions. In most years, procedures were evenly distributed across strata of income, our measure of socioeconomic status. The percentage of echocardiograms performed within 30 days of a hospitalization steadily declined from 4.6% in 2001 to 2.8% in 2009.
Table 1.
Characteristics of patients receiving and physicians performing echocardiograms performed in Ontario, 2001-2009.
| 2001 N=345,767 | 2002 N=371,356 | 2003 N=382,187 | 2004 N=431,716 | 2005 N=459,692 | 2006 N=504,581 | 2007 N=536,655 | 2008 N=571,520 | 2009 N=630,692 | Overall N=4,234,166 | p-trend | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||||
| Mean (SD) | 59.0 (16.4) | 59.1 (16.5) | 59.2 (16.4) | 59.4 (16.3) | 59.5 (16.4) | 59.5 (16.4) | 59.7 (16.3) | 59.9 (16.3) | 59.8 (16.3) | 59.5 (16.4) | <0.001 |
| 18-49 | 27.8 | 27.9 | 27.5 | 27.2 | 27.0 | 26.9 | 26.5 | 25.9 | 26.0 | 26.8 | |
| 50-64 | 29.7 | 29.6 | 30.1 | 30.3 | 30.6 | 30.8 | 31.2 | 31.4 | 31.8 | 30.8 | |
| 65-74 | 23.4 | 23.1 | 22.6 | 22.4 | 22.2 | 21.7 | 21.6 | 21.6 | 21.4 | 22.1 | |
| ≥75 | 19.1 | 19.4 | 19.8 | 20.1 | 20.2 | 20.5 | 20.7 | 21.0 | 20.7 | 20.3 | |
| Female Gender | 51.6 | 51.5 | 50.8 | 50.4 | 49.9 | 49.9 | 49.7 | 49.3 | 49.5 | 50.1 | <0.001 |
| Rural | 11.4 | 11.4 | 11.2 | 10.4 | 10.3 | 9.9 | 9.9 | 9.8 | 9.7 | 10.3 | <0.001 |
| Income quintile | <0.001 | ||||||||||
| 1 | 19.6 | 19.3 | 19.1 | 20.3 | 20.1 | 20.1 | 19.9 | 19.7 | 19.6 | 19.8 | |
| 2 | 20.8 | 20.6 | 20.3 | 20.5 | 20.3 | 20.3 | 20.2 | 20.2 | 20.2 | 20.3 | |
| 3 | 19.9 | 20.0 | 20.0 | 19.4 | 19.8 | 19.6 | 19.7 | 19.7 | 19.8 | 19.8 | |
| 4 | 19.4 | 19.7 | 20.0 | 19.5 | 19.7 | 19.7 | 20.0 | 20.1 | 20.2 | 19.8 | |
| 5 | 20.3 | 20.5 | 20.6 | 20.2 | 20.1 | 20.2 | 20.3 | 20.3 | 20.1 | 20.3 | |
| Hospitalization within prior 30 days | 4.6 | 4.4 | 4.1 | 3.8 | 3.7 | 3.3 | 3.1 | 2.9 | 2.8 | 3.5 | <0.001 |
| Physician Specialty | <0.001 | ||||||||||
| Cardiology | 76.0 | 75.8 | 76.0 | 75.6 | 75.5 | 77.1 | 78.5 | 77.9 | 78.1 | 76.9 | |
| Non-cardiology | 24.0 | 24.2 | 24.0 | 24.4 | 24.5 | 22.9 | 21.5 | 22.1 | 21.9 | 23.1 | |
| Family physician | 1.7 | 2.0 | 2.2 | 2.6 | 1.9 | 2.0 | 1.9 | 2.1 | 1.7 | 2.0 | |
| Internal medicine | 10.9 | 11.2 | 10.2 | 10.4 | 11.8 | 9.8 | 9.0 | 9.6 | 10.0 | 10.2 | |
| Radiology | 8.5 | 7.8 | 8.1 | 7.1 | 6.2 | 6.1 | 5.7 | 5.4 | 5.2 | 6.5 | |
| Other | 2.9 | 3.2 | 3.5 | 4.3 | 5.2 | 5.0 | 4.9 | 5.0 | 4.9 | 4.5 | |
| Cardiology consultation within 30 Days | 41.2 | 40.4 | 40.8 | 39.6 | 39.3 | 39.5 | 40.9 | 40.8 | 41.5 | 40.5 | <0.001 |
Values are in percentages unless otherwise specified. SD=Standard Deviation
The number of echocardiograms increased in each consecutive year, rising from 345,767 in 2001 to 630,692 in 2009 (Table 1). This represented a growth of 82% in absolute number of studies performed during the period. The age and gender adjusted rates of echocardiography grew from 39.1 per 1,000 individuals in 2001 to 59.9 per 1,000 individuals in 2009 (Figure 1). Overall growth in adjusted rate of tests was 53% during this period, with an annual rate of increase of 5.5% (Figure 2). The age and gender adjusted percentage of the population who had an echocardiogram performed increased from 3.6% in 2001 to 5.2% in 2009. On average, 4.3% of individuals in Ontario (approximately 1 in every 25 adults) had an echocardiogram performed in a given year.
Figure 1.
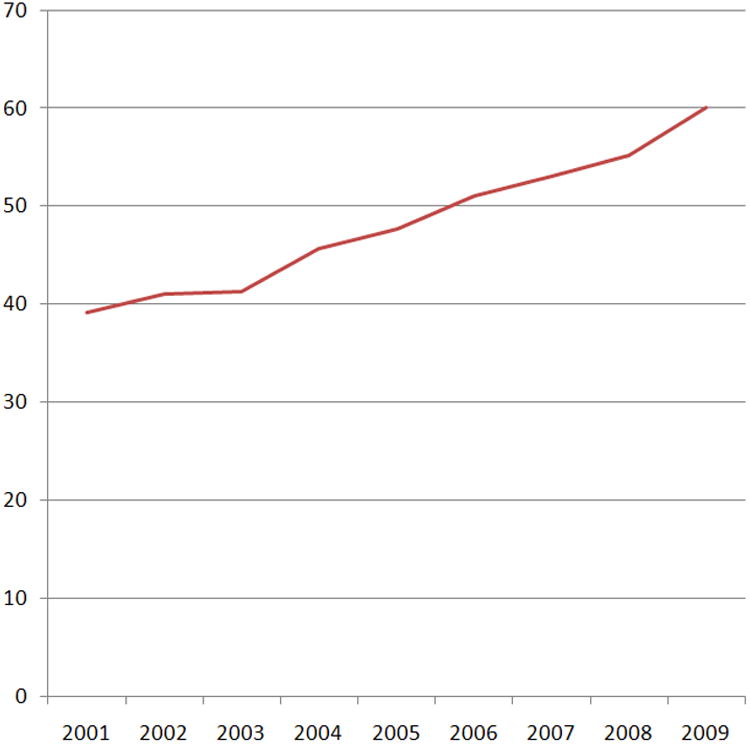
Age and gender adjusted rate of echocardiograms per 1,000 persons.
Figure 2.
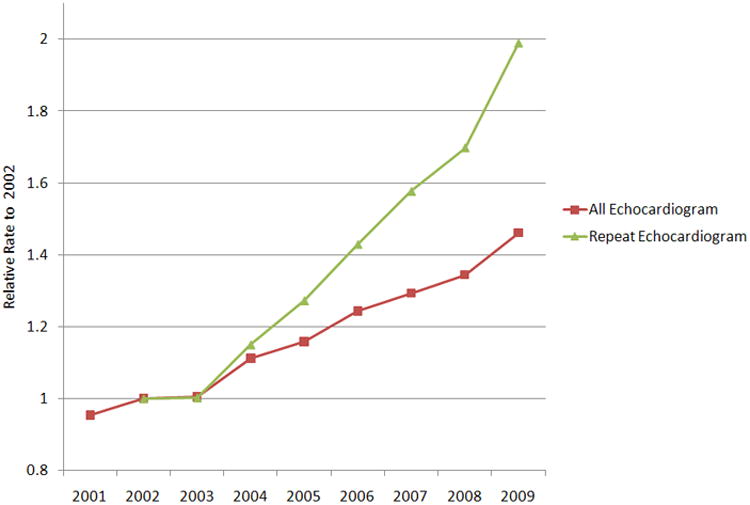
Annual change in relative rate of echocardiogram and repeat echocardiogram as compared to 2002, adjusted for age and gender.
The rate of repeat echocardiography per 1,000 individuals increased from 7.6 in 2002 to 15.1 in 2009, representing an annual increase of 10.6% per year. The percentage of all echocardiograms that represented repeat studies increased from 18.5 to 25.3% (p<0.001) between 2002 and 2009 (Table 2). Additionally, the percentage of individuals receiving at least one repeat test grew from 16.6% to 22.5% (p<0.001) during the study period, with the increase observed among both individuals who had one repeat test and those who had multiple repeat tests. About half of repeat tests were performed by the same physician (Table 2).
Table 2. Characteristics of repeat echocardiograms in Ontario.
| 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | |
|---|---|---|---|---|---|---|---|---|
| Number of echocardiogram | 371,356 | 382,187 | 431,716 | 459,692 | 504,581 | 536,655 | 571,520 | 630,692 |
| Percent repeats | 18.5 | 18.4 | 19.1 | 20.3 | 21.3 | 22.6 | 23.5 | 25.3 |
| Adjusted rate of repeat (per 1000 people) | 7.6 | 7.6 | 8.7 | 9.7 | 10.9 | 12.0 | 12.9 | 15.1 |
| Percent of repeats performed by same physician | 43.4 | 45.3 | 46.3 | 45.6 | 48.0 | 47.6 | 46.5 | 46.5 |
| Number of individuals with echocardiogram | 338,055 | 348,181 | 390,220 | 413,157 | 449,277 | 474,264 | 500,432 | 543,772 |
| Percent of individuals with repeat echocardiogram | ||||||||
| 0 repeat | 83.4 | 83.5 | 82.8 | 81.7 | 80.9 | 79.5 | 79.0 | 77.5 |
| 1 repeat | 13.7 | 13.5 | 13.9 | 14.8 | 15.3 | 16.4 | 16.5 | 17.3 |
| 2 repeat | 2.5 | 2.5 | 2.7 | 2.9 | 3.1 | 3.3 | 3.6 | 4.0 |
| 3 repeat | 0.4 | 0.4 | 0.5 | 0.5 | 0.6 | 0.6 | 0.7 | 0.9 |
| ≥4 repeat | 0.1 | 0.1 | 0.1 | 0.1 | 0.2 | 0.2 | 0.2 | 0.3 |
The majority of echocardiograms were performed by cardiac specialists throughout the study period, with significant growth taking place: cardiologists performed 87% more echocardiograms in 2009 in comparison to 2001, and this increase accounted for 81% of the overall growth in echocardiograms in the province. The average annual rate of change in number of cardiac specialists performing echocardiograms in Ontario was 3.1%, while the volume of tests per cardiac specialist increased by 5.1% per year (Table 3). Among cardiologists, 34% of the growth in the rate of echocardiograms between 2002 and 2009 could be attributed to an increase in repeat echocardiography.
Table 3. Characteristics of specialty of physicians performing echocardiograms in Ontario, by year.
| Specialty | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | Annual Rate of Change (95% CI) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cardiology | |||||||||||
| Number of physicians billing echo | 304 | 305 | 328 | 330 | 335 | 361 | 361 | 363 | 395 | 3% | (3%-4%)* |
| Number of echo | 262634 | 281499 | 290325 | 326215 | 347082 | 388870 | 421152 | 445271 | 492406 | 8% | (8%-9%)* |
| Average echo per physician | 864 | 923 | 885 | 989 | 1036 | 1077 | 1167 | 1227 | 1247 | 5% | (4%-6%)* |
| Number of repeat echo | 56679 | 58693 | 68745 | 76630 | 89799 | 101782 | 109964 | 128829 | 13% | (12%-14%)* | |
| Average repeat echo per physician | 186 | 179 | 208 | 229 | 249 | 282 | 303 | 326 | 9% | (7%-12%)* | |
| Non-Cardiology | |||||||||||
| Number of physicians billing echo | 399 | 411 | 395 | 374 | 406 | 385 | 352 | 395 | 395 | -1% | (-2%-1%) |
| Number of echo | 83133 | 89857 | 91862 | 105501 | 112610 | 115711 | 115503 | 126249 | 138286 | 6% | (5%-7%)* |
| Average echo per physician | 208 | 219 | 233 | 282 | 277 | 301 | 328 | 320 | 350 | 7% | (5%-8%)* |
| Number of repeat echo | 11852 | 11605 | 13859 | 16806 | 17638 | 19713 | 24148 | 30619 | 15% | (12%-17%)* | |
| Average repeat echo per physician | 29 | 29 | 37 | 41 | 46 | 56 | 61 | 78 | 16% | (11%-21%)* | |
| Internal Medicine | |||||||||||
| Number of physicians billing echo | 95 | 89 | 107 | 95 | 108 | 104 | 94 | 118 | 119 | 3% | (0%-5%)‡ |
| Number of echo | 37711 | 41435 | 38980 | 45025 | 51307 | 49330 | 48441 | 55034 | 63249 | 6% | (4%-7%)* |
| Average echo per physician | 397 | 466 | 364 | 474 | 475 | 474 | 515 | 466 | 532 | 3% | (1%-5%)† |
| Number of repeat echo | 6215 | 5108 | 5826 | 7701 | 7280 | 8297 | 10593 | 11065 | 11% | (8%-14%)* | |
| Average repeat echo per physician | 70 | 48 | 61 | 71 | 70 | 88 | 90 | 93 | 8% | (4%-11%)* | |
| Family Practice/General Practitioner | |||||||||||
| Number of physicians billing echo | 62 | 74 | 74 | 70 | 79 | 59 | 66 | 64 | 60 | -2% | (-5%-1%) |
| Number of echo | 5785 | 7591 | 8574 | 11339 | 8920 | 10314 | 10441 | 11737 | 10911 | 7% | (4%-10%)* |
| Average echo per physician | 93 | 103 | 116 | 162 | 113 | 175 | 158 | 183 | 182 | 9% | (5%-12%)* |
| Number of repeat echo | 1544 | 2213 | 2481 | 1938 | 1993 | 2033 | 2619 | 2555 | 4% | (0%-9%)‡ | |
| Average repeat echo per physician | 21 | 30 | 35 | 25 | 34 | 31 | 41 | 43 | 8% | (2%-14%)† | |
| Radiology | |||||||||||
| Number of physicians billing echo | 139 | 147 | 133 | 121 | 119 | 115 | 92 | 89 | 95 | -6% | (-8%--4%)* |
| Number of echo | 29485 | 28938 | 30789 | 30773 | 28421 | 30669 | 30421 | 30831 | 33089 | 1% | (0%-2%)‡ |
| Average echo per physician | 212 | 197 | 231 | 254 | 239 | 267 | 331 | 346 | 348 | 8% | (6%-9%)* |
| Number of repeat echo | 2541 | 2719 | 2819 | 3149 | 3425 | 4108 | 4741 | 8289 | 16% | (11%-21%)* | |
| Average repeat echo per physician | 17 | 20 | 23 | 26 | 30 | 45 | 53 | 87 | 27% | (21%-35%)* | |
p<0.001,
p<0.01,
p<0.05. Echo=echocardiograms; CI=Confidence interval
Non-cardiac specialists performed 23% of echocardiograms between 2001 and 2009. The number of non-cardiologists who were performing echocardiography remained stable during the period; nonetheless, growth in the rate of echocardiograms performed by non-cardiologists was 6% per year due to an increase in the average volume performed per provider. Much of this increase in volume per provider was related to increases in repeat studies, as opposed to increased patient volume. Internal medicine physicians accounted for 44% of the procedures performed by non-cardiac specialists.
Rates of echocardiography varied by LHIN and the extent of regional variation increased over time. In 2001, the age and gender adjusted rates of echocardiography ranged from 24.1 to 53.9 per 1,000 individuals across LHINs; in 2009, rates by LHIN ranged from 34.6 to 87.3 per 1,000 individuals. (Appendix Figures 1 and 2) The rates in the highest utilizing LHIN were more than two times (range 2.23-2.68) that of the lowest LHIN in each year. We found the extremal quotient to increase at 0.05 per year (95% CI 0.03-0.07), implying a widening regional variation during the period. The extremal quotient for repeat studies increased from 3.26 in 2002 to 4.54 in 2009.
Of all echocardiography claims submitted during the study period, 73% were missing an indication diagnosis, although there was a slight improvement in reporting of diagnoses during the study period (Appendix Table 1). The most common non-missing diagnosis was code 785, representing “chest pain, tachycardia, syncope, shock, edema, masses” and found in 7.0% of claims during the period of 2007-2009. The next most common indication for echocardiography was code 429, for “all other forms of heart disease.”
Discussion
On average, about four percent of the adult population of Ontario had at least one outpatient transthoracic echocardiogram in any given year from 2001 to 2009. The total cost of performing these echocardiograms was approximately $130 million in Ontario in 2009. During this period, the total number of echocardiograms performed in the province of Ontario grew by 82%; after adjusting for age and gender, population standardized rates increased by 5.5% per annum. If adjusted rates of echocardiography had remained stable during the period, there would have been 215,000 fewer echocardiograms performed in 2009 as compared to the actual number performed. This differential would have resulted in saving the provincial health care system over $44 million in annual costs, given current reimbursement rates for a complete echocardiogram. (16)
The increase in age and gender adjusted rate in our study was similar to the annual increase observed in an earlier OHIP study, which evaluated diagnostic testing between 1992 and 2001. (2) This implies a continued growth of nearly 6% annually in the rate of echocardiograms performed in Ontario over a 19 year period, after accounting for both population growth and aging, both of which are major contributors to increased health care spending. (22) Trends in our study were slightly below the 7.7% growth in rate of echocardiography in the United States Medicare population from the first part of the decade, although the Medicare numbers were unadjusted and included inpatient procedures. (5) Conversely, a study from the Veterans Administration found a total rate of increase in echocardiography of less than 4% between 2000 and 2007. The authors of that study hypothesized that Veterans Administration policy changes to increase the number of veterans eligible for services without an immediate increase in procedural capacity may have resulted in stabilization of echocardiography rates. (23) There were no such policy changes in Ontario during the study period we examined. In our study, physicians appeared to be increasingly reliant on echocardiography to clinically manage patients.
The rate of repeat testing grew faster than the total rate of echocardiography; repeat testing accounted for 18% of all echocardiograms at the beginning of the study period and 25% of total tests by the end, representing a major driver in the increase in overall utilization of echocardiography. Previous studies have shown minimal growth in the rate of repeat echocardiography but were limited to evaluating only the number of repeat studies within the same calendar year. (5,23) In our study, in which a repeat echocardiogram was defined as having occurred within 365 days of a prior outpatient procedure, repeat testing increased by an average of 10% per year.
The ACCF Appropriate Use Criteria (AUC), first published in 2007(10) and updated in 2011, (11) describe many appropriate indications for repeat echocardiography within one year, including symptoms of an acute cardiopulmonary event; changes in clinical status for an individual with pulmonary hypertension, valvular disease, or aortic disease; and evaluation for advanced therapies in heart failure. (11) Nonetheless, most indications for repeat studies within one year are considered to be inappropriate on stable patients, and studies from single centers have demonstrated that repeat echocardiograms are frequently obtained on stable patients, particularly in the outpatient setting. (24-26) We did not include hospitalized patients and found that the rates of tests performed within 30 days of hospitalization decreased during this period; these findings suggest that growth in echocardiography was not related to a higher prevalence of unstable patients.
Importantly, we observed that over half of all repeat echocardiograms were performed by a different physician. We postulate that many of these repeat tests may be related to inefficiencies in the current health care system and/or medico-legal concerns. An inability to access prior echocardiographic images, or questions regarding the quality of either the acquisition or interpretation of previous studies by different physicians, may have led to many repeat procedures.
Given that multi-laboratory image sharing for outpatient echocardiography has not been implemented in Ontario, (27) improving accessibility of imaging across facilities through a common Picture Archiving and Communications System (PACS) may help to reduce unnecessary repeat procedures. Furthermore, certification of facilities that perform echocardiography and basic competency requirements for physicians who interpret echocardiograms may reduce concerns related to variations in quality and possibly result in less repeat procedures. An organization such as the Intersocietal Commission for the Accreditation of Echocardiography Laboratories (ICAEL) (28) may be able to provide such certification but there are only a few facilities in Ontario that are currently accredited.(29)
We were limited in our ability to determine the indication for procedures as the majority of claims in this study had no associated diagnosis. Of the claims that did have a diagnosis code, the diagnosis was based on the ICD-8 classification system, which was updated decades ago due to lack of specificity. (30) As exemplified in this study, the most common diagnosis listed (other than missing) was “chest pain, tachycardia, syncope, shock, edema, masses,” which represents six different symptoms, each of which may incorporate a number of actual diagnoses. Given such lack of specificity, we are significantly limited in our ability to assess the rationale for the minority of procedures which did have an associated diagnosis codes.
A number of other health care systems and payers require that a referral indication be included with outpatient procedures such as echocardiograms, thus allowing for potential tracking of procedure indications. (23,31) Although procedure diagnoses have limitations in accuracy, they may be helpful for improving appropriate utilization. Firstly, clinician who are required to provide a diagnosis for refer may give additional consideration to the necessity for the procedure. Such consideration may lead to further education about appropriate use, which is one of the goals of the Appropriate Use Criteria. (11,31) Secondly, required documentation of echocardiography indication could be used to track the appropriateness of procedures. To maximize the utility of such a tracking mechanism, the diagnosis coding system should be updated to a more specific system. The referral diagnosis could ideally be paired with expert recommendations on utilization, such as the ACCF Appropriate Use Criteria, to evaluate for best practice. Thirdly, the inclusion of indication on claims should be feasible. The Cardiac Care Network of Ontario recently issued a statement on the standards for performance of echocardiography, which included recommendations that laboratories should have mechanisms to ensure that an indication is included with each referral and to educate physicians on appropriate indications for referral. (32) Therefore, a mechanism should be in development for recording an appropriate referral indication; tracking this information can be implemented with improvement of the system that records the diagnosis.
This study should be interpreted in the context of its limitations. Firstly, echocardiography is an extremely useful diagnostic test in many patients but whether a continuous rapid rise in utilization rates is clinically justified remains uncertain, particularly given the lack of rigor in OHIP diagnostic coding for procedures and our inability to determine trends and variations in the prevalence of such conditions as pulmonary hypertension, valvular heart disease, and outpatient heart failure. Secondly, our definition of physician specialty was based on analysis of the type of clinical care delivered rather than specialty certification and, therefore, may be subject to misclassification.(19) Thirdly, due to the nature of claims data, we were only able to determine the proportion of echocardiograms that were attributable to self-referral as we did not have information on the referring physician. Fourthly, as claims data for inpatient echocardiography were unavailable for the majority of the study period, we were unable to evaluate trends in outpatient procedures. A shift in location of performance of echocardiography from hospital to the outpatient setting might have partially accounted for increases in rates. However, OHIP began to reimburse the professional component for inpatient echocardiography by 2007, increasing the financial incentive to perform tests in the hospital rather than moving the site of location of these studies from the hospital to the outpatient setting. Finally, our findings reflect patterns of echocardiography use in the province of Ontario and may not reflect trends in utilization in other provinces or health care systems.
In conclusion, we observed high rates of growth in use of echocardiography and repeat echocardiography in the universal health care system of Ontario. There are clearly opportunities to address this rapid growth through basic measures such as required referral indication codes, particularly with an improved coding system. The effect of the implementation of required coding on quality, efficiency, and patient outcomes should be evaluated.
Supplementary Material
Age and gender adjusted rate of echocardiograms per 1,000 persons, by the fourteen geographically-defined regional Local Health Integration Networks (LHIN).
Age and gender adjusted rate of repeat echocardiograms per 1,000 persons, by the fourteen geographically-defined regional Local Health Integration Networks (LHIN).
Ten most common indications for echocardiography in Ontario, 2001-2009.
Acknowledgments
This project was supported by operating grants from the Ontario Ministry of Health and Long-term Care and the Canadian Institutes of Health Research. Dr. Blecker was supported in part by NHLBI grant 5T32HL007024. Dr. Lee is supported by a Clinician-Scientist Award from the Canadian Institutes of Health Research. Dr. Alter is supported by a Career Investigator Award from the Heart and Stroke Foundation of Ontario. Dr. Tu is supported by a Canada Research Chair in Health Services Research and a Career Investigator Award from the Heart and Stroke Foundation of Ontario. The Institute for Clinical Evaluative Sciences (ICES) is supported by the Ontario Ministry of Health and Long-term Care. The results and conclusions are those of the authors, and should not be attributed to any of the funding agencies.
Abbreviations
- ACCF
American College of Cardiology Foundation
- OHIP
Ontario Health Insurance Plan
- LHIN
Local Health Integration Network
References
- 1.Iglehart JK. Health insurers and medical-imaging policy--a work in progress. N Engl J Med. 2009;360:1030–7. doi: 10.1056/NEJMhpr0808703. [DOI] [PubMed] [Google Scholar]
- 2.Alter DA, Stukel TA, Newman A. Proliferation of cardiac technology in Canada: a challenge to the sustainability of Medicare. Circulation. 2006;113:380–7. doi: 10.1161/CIRCULATIONAHA.105.560466. [DOI] [PubMed] [Google Scholar]
- 3.Chan B, Cox JL, Anderson G. Trends in the utilization of noninvasive cardiac diagnostic tests in Ontario from fiscal year 1989/90 to 1992/93. Can J Cardiol. 1996;12:237–48. [PubMed] [Google Scholar]
- 4.Maitino AJ, Levin DC, Parker L, Rao VM, Sunshine JH. Nationwide trends in rates of utilization of noninvasive diagnostic imaging among the Medicare population between 1993 and 1999. Radiology. 2003;227:113–7. doi: 10.1148/radiol.2272020617. [DOI] [PubMed] [Google Scholar]
- 5.Pearlman AS, Ryan T, Picard MH, Douglas PS. Evolving trends in the use of echocardiography: a study of Medicare beneficiaries. J Am Coll Cardiol. 2007;49:2283–91. doi: 10.1016/j.jacc.2007.02.048. [DOI] [PubMed] [Google Scholar]
- 6.Alter DA, Przybbysz R, Iron K. Non-invasive cardiac testing in Ontario. Toronto: Institute for Clinical Evaluative Sciences; 2004. [Google Scholar]
- 7.Bonow RO. 2009 ASNC keynote lecture: measuring cost, cost-effectiveness, and quality in cardiovascular imaging. J Nucl Cardiol. 2010;17:362–9. doi: 10.1007/s12350-010-9224-4. [DOI] [PubMed] [Google Scholar]
- 8.MedPAC. Report to the Congress: Aligning incentives in Medicare. Washington DC: MedPAC; 2010. Medicare Payment Advisory Commission. [Google Scholar]
- 9.Verghese A, Brady E, Kapur CC, Horwitz RI. The bedside evaluation: ritual and reason. Ann Intern Med. 2011;155:550–3. doi: 10.7326/0003-4819-155-8-201110180-00013. [DOI] [PubMed] [Google Scholar]
- 10.Douglas PS, Khandheria B, Stainback RF, et al. ACCF/ASE/ACEP/ASNC/SCAI/SCCT/SCMR 2007 appropriateness criteria for transthoracic and transesophageal echocardiography: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American Society of Echocardiography, American College of Emergency Physicians, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and the Society for Cardiovascular Magnetic Resonance endorsed by the American College of Chest Physicians and the Society of Critical Care Medicine. J Am Coll Cardiol. 2007;50:187–204. doi: 10.1016/j.jacc.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Douglas PS, Garcia MJ, Haines DE, et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126–66. doi: 10.1016/j.jacc.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Parikh PB, Asheld J, Kort S. Does the Revised Appropriate Use Criteria for Echocardiography Represent an Improvement Over the Initial Criteria? A Comparison between the 2011 and the 2007 Appropriateness Use Criteria for Echocardiography. J Am Soc Echocardiogr. 2011 doi: 10.1016/j.echo.2011.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Willens HJ, Hendel RC, Inhaber FR, et al. Appropriateness use criteria for transthoracic echocardiography: relationship with radiology benefit managers preauthorization determination and comparison of the new (2010) criteria to the original (2007) criteria. Am Heart J. 2011;162:772–9. doi: 10.1016/j.ahj.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 14.Lee DS, Chiu M, Manuel DG, et al. Trends in risk factors for cardiovascular disease in Canada: temporal, socio-demographic and geographic factors. CMAJ. 2009;181:E55–66. doi: 10.1503/cmaj.081629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tu JV, Nardi L, Fang J, Liu J, Khalid L, Johansen H. National trends in rates of death and hospital admissions related to acute myocardial infarction, heart failure and stroke, 1994-2004. CMAJ. 2009;180:E118–25. doi: 10.1503/cmaj.081197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ontario Ministry of Health and Long-Term Care. [Accessed November 15, 2011];Schedule of benefits for physician services under the health insurance act. Available at: http://www.health.gov.on.ca/english/providers/program/ohip/sob/physserv/physserv_mn.html.
- 17.Tu K, Gong Y, Austin PC, Jaakimanian L, Tu JV. An overview of the types of physicians treating acute cardiac conditions in Canada. Can J Cardiol. 2004;20:282–91. [PubMed] [Google Scholar]
- 18.Coburn N, Przybysz R, Barbera L, et al. CT, MRI and ultrasound scanning rates: evaluation of cancer diagnosis, staging and surveillance in Ontario. J Surg Oncol. 2008;98:490–9. doi: 10.1002/jso.21144. [DOI] [PubMed] [Google Scholar]
- 19.Lee DS, Stukel TA, Austin PC, et al. Improved outcomes with early collaborative care of ambulatory heart failure patients discharged from the emergency department. Circulation. 2010;122:1806–14. doi: 10.1161/CIRCULATIONAHA.110.940262. [DOI] [PubMed] [Google Scholar]
- 20.Ministry of Health and Long-Term Care. [Accessed May 31, 2012];Resource Manual for Physicians. Available at: http://health.gov.on.ca/english/providers/pub/ohip/physmanual/physmanual_mn.html.
- 21.You JJ, Alter DA, Iron K, et al. ICES Investigative Report. Toronto: Institute for Clinical Evaluative Sciences; 2007. Diagnostic Services in Ontario: Descriptive Analysis and Jurisdictional Review. [Google Scholar]
- 22.Alemayehu B, Warner KE. The lifetime distribution of health care costs. Health Serv Res. 2004;39:627–42. doi: 10.1111/j.1475-6773.2004.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Okrah K, Vaughan-Sarrazin M, Cram P. Trends in echocardiography utilization in the Veterans Administration Healthcare System. Am Heart J. 2010;159:477–83. doi: 10.1016/j.ahj.2009.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bhave NM, Mansour IN, Veronesi F, Razi RR, Lang RM, Ward RP. Use of a web-based application of the American College of Cardiology Foundation/American Society of Echocardiography Appropriateness Use Criteria for Transthoracic Echocardiography: a pilot study. J Am Soc Echocardiogr. 2011;24:271–6. doi: 10.1016/j.echo.2010.12.027. [DOI] [PubMed] [Google Scholar]
- 25.Rao G, Sajnani N, Kusnetzky LL, Main ML. Appropriate use of transthoracic echocardiography. Am J Cardiol. 2010;105:1640–2. doi: 10.1016/j.amjcard.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 26.Ward RP, Krauss D, Mansour IN, Lemieux N, Gera N, Lang RM. Comparison of the clinical application of the American College of Cardiology Foundation/American Society of Echocardiography Appropriateness Criteria for outpatient transthoracic echocardiography in academic and community practice settings. J Am Soc Echocardiogr. 2009;22:1375–81. doi: 10.1016/j.echo.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 27.ehealth Ontario. [Accessed June 1, 2012]; http://www.ehealthontario.on.ca/programs/dipacs.asp.
- 28.Heller GV, Katanick SL, Sloper T, Garcia M. Accreditation for cardiovascular imaging: setting quality standards for patient care. JACC Cardiovasc Imaging. 2008;1:390–7. doi: 10.1016/j.jcmg.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 29. [Accessed June 1, 2012];Intersocietal Commission for the Accreditation of Echocardiography Laboratories. Available at: http://www.icael.org/icael/index.htm.
- 30.CDC. [Accessed: June 1, 2012];International Classification Of Diseases-9-CM. Available at: http://wonder.cdc.gov/wonder/sci_data/codes/icd9/type_txt/icd9cm.asp.
- 31.Hendel RC. Utilization management of cardiovascular imaging pre-certification and appropriateness. JACC Cardiovasc Imaging. 2008;1:241–8. doi: 10.1016/j.jcmg.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 32.Sanfilippo A, Chan K, Hughes W, Leong Poi H, Sasson Z, Wald R. Cardiac Care Network of Ontario Echocardiography Working Group Standards for Provision of Echocardiography in Ontario. 2012 doi: 10.1016/j.cjca.2012.11.024. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Age and gender adjusted rate of echocardiograms per 1,000 persons, by the fourteen geographically-defined regional Local Health Integration Networks (LHIN).
Age and gender adjusted rate of repeat echocardiograms per 1,000 persons, by the fourteen geographically-defined regional Local Health Integration Networks (LHIN).
Ten most common indications for echocardiography in Ontario, 2001-2009.


