Abstract
Background
Hispanics with diabetes often have deficits in health literacy (HL). We examined the association among HL, psychosocial factors, and diabetes-related self-care activities.
Methods
Cross-sectional analysis of 149 patients. Data included patient demographics and validated measures of HL, physician trust, self-efficacy, acculturation, self-care behaviors, and A1c.
Results
Participants (N=60) with limited HL were older and less educated, and had more years with diabetes compared with adequate HL participants (N=89). Limited HL participants reported greater trust in their physician, greater self-efficacy, and better diet, foot care, and medication adherence. Health literacy status was not associated with acculturation or A1c. In adjusted analyses, HL status remained associated with physician trust, and we observed a notable but nonsignificant trend between HL status and medication adherence.
Discussion
Lower HL was associated with greater physician trust and better medication adherence. Further research is warranted to clarify the role of HL and physician trust in optimizing self-care for Hispanics.
Keywords: Health literacy, Hispanics, diabetes, self-care, trust
Health literacy is defined as the degree to which individuals have the capacity to obtain, process, and understand basic health information to make appropriate health decisions.1 Deficits in health literacy have been documented among Hispanic patients with diabetes.2–4 According to the most recent National Assessment of Adult Literacy, approximately 66% of Hispanics have basic or below basic health literacy skills.2 Hispanics with diabetes often experience both suboptimal processes of care (e.g., timing and receipt of appropriate testing)5,6 and diabetes-related health outcomes compared with their non-Hispanic White counterparts.6–9 As both the U.S. Hispanic population and its disproportionate burden of diabetes continue to rise,7,9–11 so too does the need for improved diabetes care in this population. Paramount in effective management of diabetes is an individual’s ability to engage in several daily self-care activities. These include, but are not limited to, blood glucose monitoring, managing insulin and oral medication regimens, performing foot care, monitoring dietary intake, and engaging in physical activity. Each of these activities requires varying levels of time and disease-specific knowledge, motivation, and skill, posing significant challenges for patients, particularly those with limited health literacy and psychosocial barriers.12–14
Psychosocial factors such as trust in one’s physician, self-efficacy for diabetes care, and level of acculturation can influence diabetes-related outcomes. In several previous studies, focused predominantly on White, English-speaking adults with diabetes, increased trust in one’s physician has been associated with better glycemic control,15,16 yet to date it remains unclear whether level of physician trust differs by literacy status.17 Diabetes self-efficacy, which represents one’s confidence in performing the tasks of self-care18 has been shown among English-speaking patients to explain the relationship between patient’s HL status, numeracy status (i.e., math skills), and glycemic control.19 Higher self-efficacy has also been associated with improved diet, exercise, and self-monitoring behaviors across race/ethnicity and HL levels.4 Acculturation is best understood as a non-linear process in which an individual adopts varying degrees of values, norms, and behaviors from a predominant culture into their own way of life.20 The impact of acculturation on diabetes for Hispanics has been mixed with some studies reporting an association between higher acculturation and an increased prevalence of type 2 diabetes,21 obesity, and poorer dietary quality,22 while others report no relationship between level of acculturation and glycemic control.23,24
Theoretical/conceptual framework
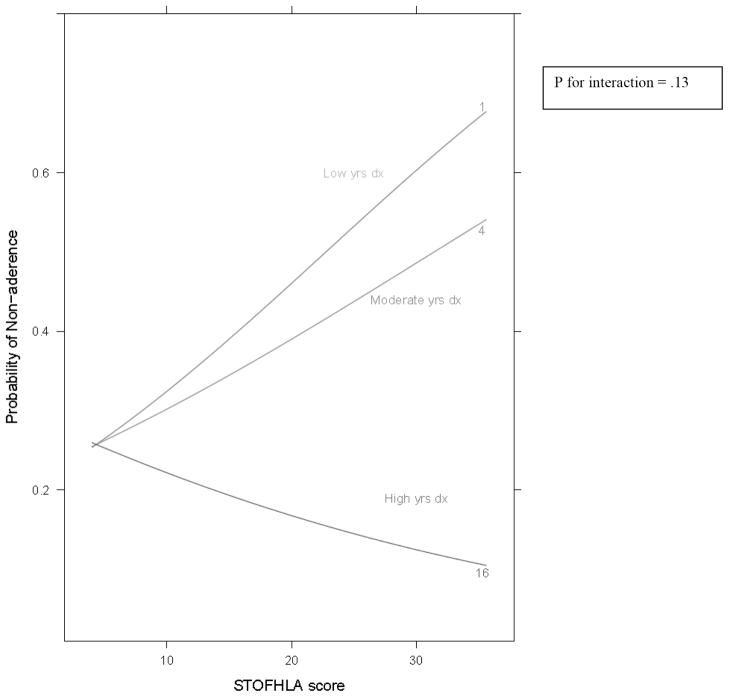
Paasche-Orlow and Wolf 25 conceptualized the relationship between health literacy and health outcomes along a continuum of health care. Therein it is believed that both patient factors (i.e., health literacy, age, race/ethnicity) and health system factors (i.e., complexity of the health care environment, available resources, and provider communication skills) influence patient access and utilization of health care, the patient-provider interaction, and self-care behaviors. In turn, these factors are believed to affect health outcomes. Additionally, we propose that for Hispanics with diabetes, other individual factors such as trust, acculturation, and years living with disease may also provide additional influence on an individual’s healthcare experience and in turn affect the attitudes and behaviors related specifically to diabetes control (Figure 1). Latham and Calvillo,26 in their Hispanic Health Protection Model, showed that greater acculturation was associated with greater knowledge of diabetes and improved diabetes-related quality of life, but they were unable to include self-care indices in their final analysis. Taken in concert, these models raise additional questions regarding the factors that promote self-care among low income Hispanic adults with diabetes. Of particular interest to us was the relationship between HL, trust in one’s physician, self-efficacy, acculturation, and self-care behaviors. Based on the aforementioned models, we hypothesized that among Hispanic adults with diabetes, greater HL would be associated with higher levels of trust in one’s physician, greater self-efficacy for diabetes care, higher levels of acculturation, improved self-care behaviors, and better glycemic control compared with those with lower HL status.
Figure 1.
Conceptual model of the relationship between patient/health system factors and self-care for low-income Hispanics with diabetes; Adapted from Paasche-Orlow and Wolf, 2007.
Methods
Identification of participants and data collection
From March 2008 through August 2009, patients were approached during regular clinic hours at an adult community-based academic Internal Medicine clinic and two federally qualified health centers (FQHC) in Nashville, Tennessee. All three centers serve a Hispanic population that has experienced significant growth and contains many new immigrants.10,11 Eligible patients were ages 18–85, self-identified as Hispanic, had spoken Spanish fluency, corrected visual acuity ≤ 20/50, and did not have a history of psychosis or dementia. The Meharry Medical College Institutional Review Board approved the study protocol, and both safety-net clinics provided written agreements for participation. Informed consent and HIPAA authorization to access medical records were obtained from each participant in Spanish prior to enrollment.
Trained bilingual research assistants27 conducted a semi-structured interview with each participant that lasted approximately 60 minutes. For patients categorized as having inadequate HL according to the Short Test of Functional Health Literacy in Adults (S-TOFHLA), RAs verbally administered the remaining measures. Glycated hemoglobin (A1c) and lipid blood tests were collected using point-of-care measurements for participants who did not have results of these tests in the medical record within six weeks prior to recruitment. All participants were compensated $20.
All measures were administered in Spanish due to the high prevalence of limited English proficiency among our sample. Data collection included age, gender, Hispanic subgroup, years of formal education, insurance status, income level, years since diagnosis, previous receipt of diabetes education, diabetes type, and insulin use. Body Mass Index (BMI) (kg/m2) was calculated using weight and height data extracted from the medical record. Additionally, reliable and validated Spanish versions of the following instruments were administered to each participant: the Short Test of Functional Health Literacy in Adults (S-TOFHLA),28 Short Acculturation Scale for Hispanics (SASH),29 and Summary of Diabetes Self-Care Activities (SDSCA)30,31 questionnaire. As validated Spanish versions of the Trust in Physician Scale (TPS),32 and Perceived Diabetes Self-Management Scale (PDSMS),33 did not exist, we implemented a rigorous translation, back-translation process with iterative feedback from bilingual staff and potential participants to ensure each instrument’s readability and face validity prior to use.34
The S-TOFHLA is a 36-item questionnaire that assesses health literacy status using two prose passages. Scores of 0–16, 17–22, and >23 distinguish inadequate, marginal, and adequate HL, respectively.28 The Short Acculturation Scale for Hispanics (SASH) consists of 12 items that measure acculturation in the domains of language, media use, and social interactions.29 This scale has been used with a variety of Hispanic subgroups including Mexicans, Cubans, Puerto Ricans, Dominicans, and Central and South Americans. Average SASH scores greater than or equal to three identify individuals with greater levels of acculturation.29 The SDSCA is a 14-item measure that assesses self-reported adherence during the prior week to different self-care activities including medication use, general and specific diet (i.e., following a “healthful eating plan” or consuming fruits/vegetables and foods low in fat, respectively), foot care, exercise, and blood-glucose testing. All responses to self-care activities ranged from 0–7 days.30 The Trust in Physician Scale measures interpersonal level of trust in one’s physician across 11 items. Scores range from 11–55 with higher scores indicating greater levels of trust.32 Finally, the PDSMS is an eight-item measure of one’s confidence in diabetes self-management. Higher scores indicate greater confidence in self-care with scores ranging from 8–40.33
Statistical analysis
Demographic and diabetes related factors were compared by HL status dichotomized as adequate vs. marginal + inadequate (subsequently referred to as “limited HL”). Median and interquartile range [IQR] was used for continuous variables and compared by HL status using the Wilcoxon rank-sum test. Categorical variables were described as frequencies with percent and compared by HL status using chi-square tests. All self-care activities were assessed using integer scale except for medication adherence which was dichotomized to non-perfect (referent group) vs. perfect for consistency with previously described methodologies.35,36
To assess the adjusted association between HL and psychosocial factors (i.e., trust in one’s physician, self-efficacy, acculturation), and HL and self-care activities (e.g., general and specific diet, blood glucose testing, exercise, and foot care), we conducted separate multivariable linear regression models controlling for patient age, gender, income, and insurance status. To assess the independent association of HL status with self-reported medication adherence, a multivariable logistic regression model was used adjusting for the covariates described above. In multivariable regression models, HL was included as a continuous measure (s-TOFHLA raw score). Additionally, several data driven decisions were made, including assessment of the direct association between years since diabetes diagnosis and both level of physician trust and self-efficacy for diabetes care using Spearman correlations (rho). We subsequently included these covariates (i.e., years since diagnosis and self-efficacy) in the adjusted models that assessed the association between HL/trust and HL/medication adherence. Finally, we assessed the potential mediating effect of trust in one’s physician on the association of HL and medication adherence using three sequential sets of multivariable regression models. These first assessed the association between trust and medication adherence, and HL and trust, and then assessed whether the relationship between HL and medication adherence was attenuated by the inclusion of trust in the model. Statistical analyses were performed using R version 2.12.1 (http://www.r-project.org).37
Results
During the recruitment period, 163 adult Hispanics with diabetes were approached. Thirteen declined participation due to time constraints, inability to sign consent, or lack of interest, and one participant was screened ineligible due to a history of dementia. Of the 149 who were eligible and agreed to participate, complete data are available on 140 (94%). Scores on the S-TOFHLA indicated that 40% of the sample had limited HL. Table 1 presents differences in demographic and diabetes-related factors by HL status. On average, participants with limited HL were older, less likely to be of Mexican heritage, had less educational attainment, more years living with diabetes, and were more likely to be unsure of their diabetes type. There were no significant differences by HL status in gender, income, insulin use, previous receipt of diabetes education, BMI, lipids, or A1c. In both groups, nearly all of the participants had low levels of acculturation, were monolingual in Spanish and uninsured.
Table 1.
PATIENT DEMOGRAPHICS AND DIABETES-RELATED FACTORS BY HEALTH LITERACY STATUS
| Patient Demographics | Median (IQR) or n (%)
|
p-value | |
|---|---|---|---|
| Limited HL N=60 |
Adequate HL N=89 |
||
| Age | 50 (40–60) | 46 (38–54) | .01 |
| Gender | |||
| Female | 34 (57) | 58 (65) | .27 |
| Hispanic subgroup | .011 | ||
| Mexican | 40 (66) | 76 (85) | |
| Other | 20 (33) | 14 (15) | |
| Education level | |||
| ≤ High School | 47 (78) | 36 (40) | <.001 |
| Insurance Status | |||
| Uninsured | 51 (85) | 70 (79) | .33 |
| Income | .18 | ||
| {less or equal} 10,000 | 21 (37) | 44 (52) | |
| 10,000–19,999 | 27 (47) | 29 (35) | |
| 20,000–39,999 | 9 (16) | 11 (13) | |
| Acculturation level (SASH) | .75 | ||
| Low | 55 (96) | 83 (95) | |
| High | 2 (4) | 4 (5) | |
| Household monolingual in Spanish? | |||
| Yes | 52 (88) | 69 (78) | .20 |
| Diabetes related factors | |||
| Years since diagnosis | 6 (2–12) | 4 (2–8) | .01 |
| Previous diabetes education? | |||
| Yes | 28 (47) | 45 (50) | .61 |
| Diabetes type | .002 | ||
| Type 2 | 45 (75) | 83 (93) | |
| Unsure | 12 (20) | 3 (3) | |
| Do you use insulin? | .35 | ||
| Yes | 19 (32) | 22 (25) | |
| Current HgbA1c | .16 | ||
| >7% | 37 (63) | 45 (51) | |
| <7% | 22 (37) | 43 (49) | |
| LDL, mg/dl | 106 (94–129) | 101 (79–124) | .18 |
| BMI, kg/m2 | 28 (25–35) | 30 (26–36) | .48 |
HL = health literacy
SASH = Short Acculturation Scale for Hispanics
Table 2 presents the unadjusted and adjusted associations between HL status and the psychosocial factors of interest (i.e., self-efficacy, acculturation, trust in one’s physician), and between HL status and various diabetes self-care activities. In unadjusted analyses, participants with limited HL reported greater self-efficacy for diabetes care and greater trust in their physician compared with participants with adequate HL. HL status was not associated with acculturation scores. Participants with limited HL also reported greater adherence to a general diet (i.e., “healthful eating plan”), better foot care, and better medication adherence compared with participants with adequate HL. HL status was not associated with following a specific diet (i.e., fruit/vegetable, low fat), blood glucose testing, or physical activity.
Table 2.
UNADJUSTED VS. ADJUSTED ASSOCIATIONS BETWEEN HEALTH LITERACY, PSYCHOSOCIAL FACTORS, AND SELECT DIABETES SELF-CARE ACTIVITIES
| Median (IQR) or n (%)
|
unadjusted p-value | Beta 95%CI: | adjusted p-value | ||
|---|---|---|---|---|---|
| Limited HL | Adequate HL | ||||
| Psychosocial factors | |||||
| Self-efficacy (PDSMS), n=141 | 23 (19–27) | 20 (18–23) | .002a* | −0.83 (−2.4, .76) | .31c |
| Acculturation (SASH), n=137 | 1.25 (1.0–1.5) | 1.3 (1.2–1.9) | .10a | 0.03 (−0.1, 0.2) | .65c |
| Physician Trust (TPS), n=134 | 46 (40–51) | 41 (37–47) | .003a* | −1.8 (−3.6, 0.02) | .05c* |
| Self-care activities | |||||
| General Diet, n=139 | 4 (2–6) | 3 (1–4) | .03a* | −0.1 (−0.7, 0.43) | .64c |
| Specific Diet, n=139 | 4 (3–5) | 4 (2–4) | .20a | −0.04 (−0.4, 0.4) | .84c |
| Blood Glucose Testing, n=139 | 3 (0–6) | 1 (0–5) | .40a | 0.03 (−0.7, 0.7) | .94c |
| Exercise, n=139 | 2 (0.5–3.5) | 1.8 (0.5–3.5) | .90a | 0.35 (−0.2, 0.9) | .21c |
| Foot care, n=138 | 4.75 (3.5–7.0) | 3.5 (1.0–7.0) | .02a* | −0.3 (−0.9, 0.4) | .42c |
| OR (95% CI) | |||||
| Medication non-adherence, n=139 | 14 (24) | 35 (40) | .04b* | 1.63e (0.9, 3.0) | .11e |
p<0.05
Wilcoxon rank-sum test to compare continuous variables between groups.
Pearson’s chi-square test to compare proportions of perfect vs. non-perfect adherence
Multivariable linear
Logistic regression adjusted for age, gender, income, and insurance status.
Odds ratio for an interquartile difference of health literacy score.
PDSMS = Perceived Diabetes Self-Management Scale; SASH = Short Acculturation Scale for Hispanics; TPS = trust in physician scale; IQR = interquartile range; HL = health literacy; OR = odds ratio; CI = confidence interval.
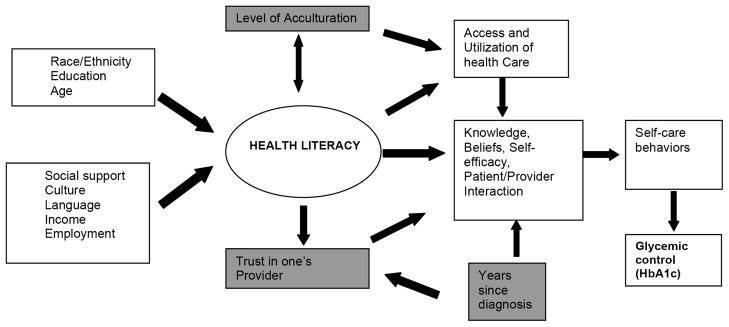
In multivariable analyses, after adjusting for age, gender, income, and insurance status, Higher HL remained significantly associated with less trust in one’s physician (β = −1.80; 95% CI:−3.6, 0.02, p=.05), and there was a non-significant yet notable trend between higher HL scores (IQR difference of 14 points) and greater probability of non-adherence to one’s medication regimen (AOR = 1.6; 95% CI:0.9,3.0, p=.11). Interestingly, in our sample greater years living with diabetes significantly correlated with greater self-efficacy for diabetes care for the limited HL participants (rho=0.27, p=.04) but not for those with adequate HL (rho=0.20, p=.06). Similarly, years with diabetes correlated significantly with higher levels of physician trust in the sample as a whole (rho=0.17, p=.04) but not when stratified by HL status. The post-hoc addition of years with diabetes and self-efficacy as covariates in the models assessing the association between HL and trust in physician and HL and medication adherence did attenuate the previously observed relationships to non-significant; however, analysis of the modifying effects of these covariates on those relationships did not demonstrate significant evidence for effect modification (Figure 2; shown for medication non-adherence only). Similarly, sequential regression modeling to assess the mediating effect of trust in one’s physician on the relationship between HL and medication adherence did not demonstrate statistically significant association to support this role.
Figure 2.
Predicted probability of medication non-adherence by health literacy level at 1, 4, and 16 years since diabetes diagnosis.
Discussion
In this sample of low-income adult Hispanics with diabetes, those with limited HL reported greater trust in their physician, greater self-efficacy for diabetes care, and greater adherence to several self-care activities including following a general diet, performing foot care, and adhering to their medication regimen. Even after controlling for important covariates, higher HL remained marginally associated with lower physician trust and there was a notable trend towards poorer medication adherence. These findings were unexpected yet provide some important and useful insight into the potential relationship between HL and several important psychosocial and behavioral factors among Hispanics with diabetes.
Trust in one’s physician is known to influence several health-related factors including the quality of the patient-provider interaction,38–40 patient utilization of health care services,41–43 and patient satisfaction with care.44,45 Ciechanowski et al. reported that patients who had a “dismissing” attachment style characterized by high self-reliance and less trust of others were more likely to have lower adherence to diet, foot care, physical activity, and diabetes medication adherence, and that these associations were mediated by the patient-provider relationship.46 Larkey et al. have identified confianza (trust) and personalismo (i.e., an expectation of being dealt with in a caring and personal manner) as important constructs that influence Hispanic health-seeking behavior in general,47 but our study is the first to specifically demonstrate an association between HL status and trust in one’s physician and HL status and diabetes-related behaviors in this population.
The question remains as to why higher HL did not associate with greater trust in one’s physician, greater self-efficacy for diabetes care, and improved medication adherence as we stated a priori. The fact that lower HL status in our sample was associated with significantly greater years living with diabetes may reflect greater opportunity for these participants to have developed a trusting relationship with a provider and gain the confidence needed for self-care. This is supported by our observed significant correlation between years with diabetes and self-efficacy among the low literate subgroup in our sample and the significant association between years with diabetes and physician trust among the sample as a whole. Furthermore, patients with higher educational attainment (often a proxy for HL) have been shown to conceptualize their involvement in medical decision making as a shared process between themselves and their provider. This includes verifying the credibility of information and exploring options beyond what is given during the encounter.48 It is plausible then that lower health literate patients may be more inclined to “trust” without questioning the recommendations of their physician compared with higher health literate patients. These higher levels of trust and self-efficacy may in some circumstances translate into better self-care irrespective of literacy status. Finally, Schillinger et. al showed that patients with higher and lower functional health literacy skills experience similar quality of communication with their provider in the “listening” domains of communication49 (eg., eliciting concerns) which arguably could influence trust more so than the “explanatory” domains in which lower functionally health literate patients consistently experience poorer communication. Similarly, Sudore et al. provided evidence that higher health literacy is not always an adequate buffer for poor communication particularly in language discordant settings.50 Overall, our findings may suggest that particularly for lower literacy patients, time with disease may be an important factor for the development of certain interpersonal processes (e.g., trust, self-efficacy, disease management skills) that can potentially affect diabetes-related outcomes.
Our study is subject to several limitations. Due to the cross-sectional nature of our design and data collection we must interpret our results with caution and refrain from inferring causation between variables. Our findings are also based on a small sample size that lacked significant variation in terms of socio-demographics and acculturation level. This may affect the generalizability of our findings to other more established Hispanic populations, particularly among those Hispanics who speak English well. Our small sample size additionally precludes a more in-depth analysis of the potential mediation pathways between our variables of interest which could shed additional light on issues of causality. Measurement issues additionally are of concern in that the majority of our measures relied on self-report and particularly for the self-care items were assessed over a short period of time. Furthermore, response bias or simpatia (i.e., a desire to be courteous, respectful, and avoid conflict) has been described as a potential cause of over-reporting among Hispanics,51 although it is unclear whether response bias may differ by HL status. Finally, we did not specifically gauge other factors that may influence trust in one’s physician (e.g., ethnic and linguistic concordance, length of patient-provider relationship, satisfaction with care) nor do we know other details of the participant’s clinical encounter (e.g., length of time, topics discussed, interpreter use, level of patient engagement) that would allow us to assess better the quality of the patient-provider interaction and thus draw further conclusions.
Conclusions
Overall, our study has begun to explore the association of HL with important psychosocial factors and diabetes-related behaviors among Hispanic adults with limited resources. As the Hispanic population continues to grow in the U.S. and face increasing burden of diabetes in the context of socio-political and demographic challenges, more research is needed that focuses on determining the most efficacious methods of improving diabetes care for this vulnerable population. We believe that physician trust and the patient-provider relationship are modifiable factors that will ultimately play an important role in addressing the disparities of diabetes care facing Hispanics patients of all HL levels.
Acknowledgments
ROW led the primary data collection, performed the analysis of the data along with TG, and was the primary author of the manuscript. ROW, CYO, SK, and RLR provided health literacy and numeracy expertise, and provided editorial input into the manuscript. SK and RLR provided mentorship to ROW. All authors have read and approved the final manuscript. This study was funded by a TN Department of Health Project Diabetes Implementation Grant and Pfizer’s Fellowship in Health Literacy and Clear Health Communication. ROW conducted this research with additional support from Meharry Medical College’s CRECD Program (NCRR 1R25RR17577) and is currently supported by an NIDDK Career Award (05DK092470-02). CYO conducted this research with the support of a Diversity Supplement Award (NIDDK 3P60 DK020593-30S2), and is currently supported by an NIDDK Career Award (K01 DK087894). Support for data capture and analysis was provided by REDCap (NCRR/NIH UL1 RR024975). The authors would also like to acknowledge research assistants Mrs. Ana Murto, Miss Patricia Paez, and Dr. Khalil Harbi at Meharry Medical College for their contribution to patient recruitment and data collection and Mary Bufwack, PhD, CEO at United Neighborhood Health Services, for access to their clinics.
Notes
- 1.Nielsen-Bohlman L Institute of Medicine (U.S.), and Committee on Health Literacy. Health literacy: a prescription to end confusion. Washington, D.C: National Academies Press; 2004. What is Health Literacy? [PubMed] [Google Scholar]
- 2.Kutner MA United States. Dept. of Education and National Center for Education Statistics. The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy. Washington, DC: United States Department of Education and National Center for Education Statistics; 2006. [Google Scholar]
- 3.White RO, Osborn CY, Gebretsadik T, et al. Development and Validation of a Spanish Diabetes-Specific Numeracy Measure: DNT-15 Latino. Diabetes Technol Ther. 2011 Sep;13(9):893–8. doi: 10.1089/dia.2011.0070. Epub 2011 Jun 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarkar U, Piette JD, Gonzales R, et al. Preferences for self-management support: findings from a survey of diabetes patients in safety-net health systems. Patient Educ Couns. 2008 Jan;70(1):102–10. doi: 10.1016/j.pec.2007.09.008. Epub 2007 Nov 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng EM, Chen A, Cunningham W. Primary language and receipt of recommended health care among Hispanics in the United States. J Gen Intern Med. 2007 Nov;22( Suppl 2):283–8. doi: 10.1007/s11606-007-0346-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Dept. of Health and Human Services and United States Agency for Healthcare Research and Quality. 2009 national healthcare disparities report. Rockville: U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 7.Centers for Disease Control and Prevention (U.S.) National diabetes fact sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta: Center for Disease Control and Prevention; 2011. Available at http://www.cdc.gov/diabetes/pubs/factsheet11.htm. [Google Scholar]
- 8.Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002 Aug;94(8):666–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. JAMA. 2002 Jul 24–31;288(4):475–82. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- 10.Mendoza M, Petersen MC. New Latino immigration to Tennessee: practicing culturally sensitive health care. Tenn Med. 2000 Oct;93(10):371–6. [PubMed] [Google Scholar]
- 11.Drever AI. Latinos in the new South: transformations of place. Aldershot, England: Ashgate; 2006. New Neighbors in Dixie: The Community Impacts of Latino Migration to Tennessee. [Google Scholar]
- 12.Rodriguez HP, Chen J, Rodriguez MA. A national study of problematic care experiences among Latinos with diabetes. J Health Care Poor Underserved. 2010 Nov;21(4):1152–68. doi: 10.1353/hpu.2010.0923. [DOI] [PubMed] [Google Scholar]
- 13.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011 Feb;26(2):170–6. doi: 10.1007/s11606-010-1507-6. Epub 2010 Sep 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McCloskey J, Flenniken D. Overcoming cultural barriers to diabetes control: a qualitative study of southwestern New Mexico Hispanics. J Cult Divers. 2010 Fall;17(3):110–5. [PubMed] [Google Scholar]
- 15.Alazri MH, Neal RD. The association between satisfaction with services provided in primary care and outcomes in Type 2 diabetes mellitus. Diabet Med. 2003 Jun;20(6):486–90. doi: 10.1046/j.1464-5491.2003.00957.x. [DOI] [PubMed] [Google Scholar]
- 16.Mancuso JM. Impact of health literacy and patient trust on glycemic control in an urban USA population. Nurs Health Sci. 2010 Mar;12(1):94–104. doi: 10.1111/j.1442-2018.2009.00506.x. [DOI] [PubMed] [Google Scholar]
- 17.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007 Sep-Oct;31(Suppl 1):S27–35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 18.Rimer BK. Health behavior and health education: theory, research, and practice. San Francisco: Jossey-Bass; 2002. The Health Belief Model. [Google Scholar]
- 19.Osborn CY, Cavanaugh K, Wallston KA, et al. Self-efficacy links health literacy and numeracy to glycemic control. J Health Commun. 2010;15( Suppl 2):146–58. doi: 10.1080/10810730.2010.499980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lara M, Gamboa C, Kahramanian MI, et al. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health. 2005;26:367–97. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kandula NR, Diez-Roux AV, Chan C, et al. Association of acculturation levels and prevalence of diabetes in the multi-ethnic study of atherosclerosis (MESA) Diabetes Care. 2008 Aug;31(8):1621–8. doi: 10.2337/dc07-2182. Epub 2008 May 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez-Escamilla R. Acculturation, nutrition, and health disparities in Latinos. Am J Clin Nutr. 2011 May;93(5):1163S–7S. doi: 10.3945/ajcn.110.003467. Epub 2011 Mar 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eamranond PP, Wee CC, Legedza AT, et al. Acculturation and cardiovascular risk factor control among Hispanic adults in the United States. Public Health Rep. 2009 Nov-Dec;124(6):818–24. doi: 10.1177/003335490912400609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ross SE, Franks SF, Hall J, et al. Levels of acculturation and effect on glycemic control in Mexicans and Mexican Americans with type 2 diabetes. Postgrad Med. 2011 Jan;123(1):66–72. doi: 10.3810/pgm.2011.01.2246. [DOI] [PubMed] [Google Scholar]
- 25.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007 Sep-Oct;31(Suppl 1):S19–26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 26.Latham CL, Calvillo E. Predictors of successful diabetes management in low-income Hispanic people. West J Nurs Res. 2009 Apr;31(3):364–88. doi: 10.1177/0193945908328263. [DOI] [PubMed] [Google Scholar]
- 27.Zambrana RE, Carter-Pokras O. Role of acculturation research in advancing science and practice in reducing health care disparities among Latinos. Am J Public Health. 2010 Jan;100(1):18–23. doi: 10.2105/AJPH.2008.138826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999 Sep;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 29.Marin G, Sabogal F, Vanoss Marin B, et al. Development of a Short Acculturation Scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9:183–205. [Google Scholar]
- 30.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000 Jul;23(7):943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 31.Vincent D, McEwen MM, Pasvogel A. The validity and reliability of a Spanish version of the summary of diabetes self-care activities questionnaire. Nurs Res. 2008 Mar-Apr;57(2):101–6. doi: 10.1097/01.NNR.0000313484.18670.ab. [DOI] [PubMed] [Google Scholar]
- 32.Anderson LA, Dedrick RF. Development of the Trust in Physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990 Dec;67(3 Pt 2):1091–100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 33.Wallston KA, Rothman RL, Cherrington A. Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS) J Behav Med. 2007 Oct;30(5):395–401. doi: 10.1007/s10865-007-9110-y. Epub 2007 May 24. [DOI] [PubMed] [Google Scholar]
- 34.Hunt SM, Bhopal R. Self report in clinical and epidemiological studies with non-English speakers: the challenge of language and culture. J Epidemiol Community Health. 2004 Jul;58(7):618–22. doi: 10.1136/jech.2003.010074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen HW, Shmukler C, Ullman R, et al. Measurements of medication adherence in diabetic patients with poorly controlled HbA(1c) Diabet Med. 2010 Feb;27(2):210–6. doi: 10.1111/j.1464-5491.2009.02898.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gonzalez JS, Schneider HE. Methodological issues in the assessment of diabetes treatment adherence. Curr Diab Rep. 2011 Dec;11(6):472–9. doi: 10.1007/s11892-011-0229-4. [DOI] [PubMed] [Google Scholar]
- 37.Team RDC. R: A language and environment for statistical computing, reference index version 2.12.1. Vienna, Austria: R Foundation for Statistical Computing; 2006. Available at http://www.r-project.org/ [Google Scholar]
- 38.Bohnert AS, Zivin K, Welsh DE, et al. Ratings of patient-provider communication among veterans: serious mental illnesses, substance use disorders, and the moderating role of trust. Health Commun. 2011 Apr;26(3):267–74. doi: 10.1080/10410236.2010.549813. [DOI] [PubMed] [Google Scholar]
- 39.Moskowitz D, Lyles CR, Karter AJ, et al. Patient reported interpersonal processes of care and perceived social position: The Diabetes Study of Northern California (DISTANCE) Patient Educ Couns. 2013 Mar;90(3):392–8. doi: 10.1016/j.pec.2011.07.019. Epub 2011 Aug 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Epner DE, Ravi V, Baile WF. When patients and families feel abandoned. Support Care Cancer. 2011 Nov;19(11):1713–7. doi: 10.1007/s00520-010-1007-6. [DOI] [PubMed] [Google Scholar]
- 41.Sheppard VB, Zambrana RE, O’Malley AS. Providing health care to low-income women: a matter of trust. Fam Pract. 2004 Oct;21(5):484–91. doi: 10.1093/fampra/cmh503. [DOI] [PubMed] [Google Scholar]
- 42.O’Malley AS, Sheppard VB, Schwartz M, et al. The role of trust in use of preventive services among low-income African-American women. Prev Med. 2004 Jun;38(6):777–85. doi: 10.1016/j.ypmed.2004.01.018. [DOI] [PubMed] [Google Scholar]
- 43.LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009 Dec;44(6):2093–105. doi: 10.1111/j.1475-6773.2009.01017.x. Epub 2009 Sep 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Benkert R, Peters RM, Clark R, et al. Effects of perceived racism, cultural mistrust and trust in providers on satisfaction with care. J Natl Med Assoc. 2006 Sep;98(9):1532–40. [PMC free article] [PubMed] [Google Scholar]
- 45.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Med Care Res Rev. 2000;57( Suppl 1):146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 46.Ciechanowski P, Russo J, Katon W, et al. Influence of patient attachment style on self-care and outcomes in diabetes. Psychosom Med. 2004 Sep-Oct;66(5):720–8. doi: 10.1097/01.psy.0000138125.59122.23. [DOI] [PubMed] [Google Scholar]
- 47.Larkey LK, Hecht ML, Miller K, et al. Hispanic cultural norms for health-seeking behaviors in the face of symptoms. Health Educ Behav. 2001 Feb;28(1):65–80. doi: 10.1177/109019810102800107. [DOI] [PubMed] [Google Scholar]
- 48.Smith SK, Dixon A, Trevena L, et al. Exploring patient involvement in healthcare decision making across different education and functional health literacy groups. Soc Sci Med. 2009 Dec;69(12):1805–12. doi: 10.1016/j.socscimed.2009.09.056. Epub 2009 Oct 19. [DOI] [PubMed] [Google Scholar]
- 49.Schillinger D, Bindman A, Want F, et al. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ Couns. 2004 Mar;52(3):315–23. doi: 10.1016/S0738-3991(03)00107-1. [DOI] [PubMed] [Google Scholar]
- 50.Sudore RL, Landefeld CS, Pérez-Stable EJ, et al. Unraveling the relationship between literacy, language proficiency, and patient-physician communication. Patient Educ Couns. 2009 Jun;75(3):398–402. doi: 10.1016/j.pec.2009.02.019. Epub 2009 May 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Leeman-Castillo BA, Corbett KK, Aagaard EM, et al. Acceptability of a bilingual interactive computerized educational module in a poor, medically underserved patient population. J Health Commun. 2007 Jan-Feb;12(1):77–94. doi: 10.1080/10810730601096630. [DOI] [PubMed] [Google Scholar]