How did a country physician in 19th century Europe emerge as an icon in the world of medicine for all times to come? What inspires and motivates a discoverer to achieve what many observed and debated before him but were unable to achieve? What sweat and toil culminate in irrefutable evidence that peers accept and generations follow, expand and investigate? Is a landmark discovery, invention or innovation merely an idea whose time has come? The succeeding paragraphs illustrate how one man’s life and times provide an answer to these complex questions and forever relegate the pre-Koch era of tuberculosis (TB) to antiquity.3
Born Heinrich Hermann Robert Koch, in 1843, this Prussian physician’s abbreviated name ‘Robert Koch’ became a byword in infectious diseases practice, for having identified the bacillary aetiology of TB, the 19th century scourge.4 The enormous public health impact of this discovery on a disease that, at the time, claimed the lives of humans in epidemic proportions, overshadowed his first contribution to the field of bacteriology: the identification of the Bacillus anthracis. The juggernaut of bacterial discoveries continued with the identification of the Staphylococcus species (wound infections) and the Vibrio cholerae bacterium (cholera).5
The Pied Piper of Bacteriology
The date of Friday 24th March 1882 became a milestone in medical microbiology when Koch’s brilliant exposition of his findings on TB was witnessed, in the reading room of the library of the Institute of Physiology at 7pm, by the dazzled fraternity of the Berlin Physiological Society.4 He explained and illustrated all the scientific evidence, which his laboratory and animal experiments had yielded for the identification and isolation of the tubercle bacillus and demonstrated its transmissible nature and how it caused TB in man. Four seminal papers followed that stamped his mark on his discovery.6 This new concept of an exogenous agent initiating disease challenged and decimated the prevailing concept (spearheaded by luminaries like Virchow) that all diseases were endogenous in origin.7 Koch’s labour of love, that unveiled the anthrax and tubercle bacilli, was to spawn a generation of ‘microbe hunters’ who rapidly identified and linked specific bacteria to the diseases they caused.
In 1884, Koch’s assistant, Loeffler, and his pupil, Kaffky, identified the diphtheria and typhoid bacillus, respectively.8 In a span of thirty years, beginning from 1876, at least 20 bacterial pathogens were identified for a host of diseases including gonorrhoea, tetanus, pneumonia and the plague—all killers of those times.5 Ehrlich modified Koch’s staining techniques and Gram, Ziehl and Neelsen found their names embedded in laboratory manuals through the stains they developed which we still use today. It deserves mention that Koch, a prolific explorer and intrepid traveller, dabbled in the investigation of a variety of tropical illnesses, like the plague, dysentery, trachoma, typhus and a host of veterinary infections. The Pied Piper’s tune (translated here as Koch’s ‘style’ of research) was thus not a call to doom but heralded the light of knowledge and life for humankind. The blueprint for identifying infectious pathogens had been developed and treatment was just a few steps away.
To See what Everyone has Seen; to Think what No One has Thought
The foundation of Koch’s principles lay in the scientific legacy Koch inherited from his teachers Henle, Meissner, Wohler and Krause at the University of Göttingen.9,10 Pasteur’s contribution to wound sepsis and Lister’s disinfection techniques had already made inroads in the warfare against germs. Villemin, Cohnheim and others had encouraged acceptance of the communicability of infection.11 Early in his pursuit for recognition of the anthrax germ, Koch sought the technical patronage of Cohn, a botanist. Cohn’s encouragement enabled publication of their joint drawings of the anthrax bacillus when Koch was only 32 years old.12 Koch however, built upon their achievements and stole a march on his mentors and collaborators by his elegant animal experiments and ingenious culture techniques that were verifiable and reproducible. They resulted in the eponymous Henle-Koch’s postulates that stipulated that an organism could be considered the cause of an infectious disease if: (1) it occurred in every case of the disease; (2) it did not occur in other diseases or non-pathogenic conditions, and (3) after isolation and growth in culture, it could produce the same disease when inoculated into a healthy animal.13
A Technologist Par Excellence
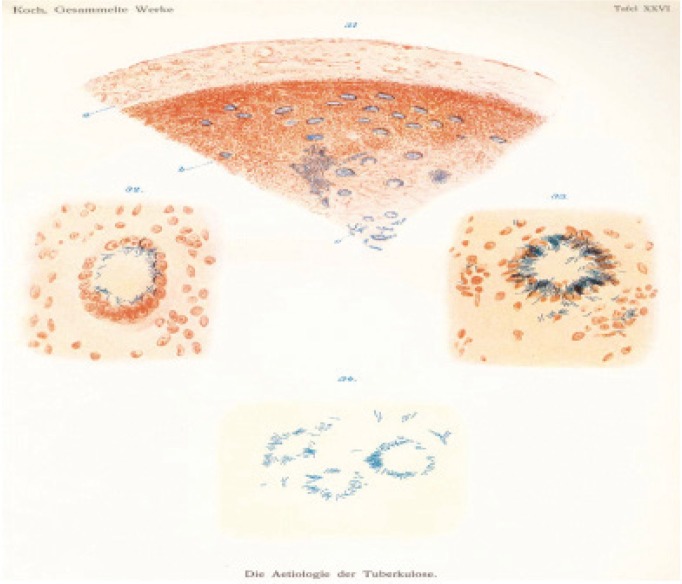
In vivo and in vitro innoculations in the cornea and aqueous humour; establishing superiority of solid- over liquid-based media for obtaining pure cultures; microscopy and illumination methods; the fixation of bacterial smears on slides, and a host of stains that made it easy to identify bacteria (the alkaline methylene blue solution stained tubercular bacteria that contrasted with the background tissue stained with the Vesuvin brown dye) are some of the significant ‘bench’ methods which Koch toiled to produce [Figure 1].7 These became the bedrock methods of modern bacteriological laboratories. It is noteworthy that his co-workers, Hesse and Petri, were responsible for the establishment of agar as a vital base for solid media and the shallow ‘petri’ dish, respectively.5 Koch’s comprehensive approach to the scientific method is illustrated by his integration of these exacting techniques with animal innoculations and, in the case of cholera, with autopsies.14 Koch is also credited with replacing pencil drawings by microphotography as an established tool for scientific documentation and the representation of bacteria.4
Figure 1:
Original drawing by Koch of tubercle bacilli within infected tissue which accompanied his groundbreaking report on the aetiology of tuberculosis.7
Figure reproduced with permission.
Personal Attributes: Passion, patience, persistence
A child prodigy, Koch had astonished his parents when, at the age of five, they learnt that he had taught himself to read through newspapers; it was no surprise that he went on to graduate maxima cum laude in his M.D. in 1866.15 The motto nunquam otiosus (Latin: never idle) was the driving force behind the prodigious contributions of this man who was passionate in equal measure about biological sciences, nature and travel. This drove him from the temples of learning in France, Berlin, London and Hannover to exotic locations like Alexandria and Calcutta. The hallmarks of his life’s mission were technological excellence and indisputable scientific logic. These stood him in good stead in convincing—where others had failed—his hard-nosed scientific peers of the veracity of the hotly-debated ‘germ theory’.
The economics of animal husbandry has often spearheaded ground-breaking research in human disease. Others before Koch had recognised the anthrax bacilli in the blood of infected animals, but failed to establish its transmissibility. Koch persisted and was able to establish growth of the bacilli in culture and observe the formation of spores: “After anthrax bacilli develop for a short time, shiny egg-shaped bodies form in the filaments. Shortly thereafter, the filaments decompose… If they are placed in a nourishing medium, they germinate and grow into rods and then into long filaments”.16 This sound scientific observation succeeded in explaining the time-lag in the transmission of the disease between animals. It predated the deluge of attention showered on him after the identification of the tubercle bacillus.
Accolades and Patronage
Koch’s success earned him the Order of the Crown, 100,000 marks and appointments such as Privy Imperial Councillor by Emperor Wilhelm I, Professor of Hygiene at the University of Berlin and Director of the Hygiene Institute.4,15 He then went on to head the newly established Institute of Infectious Diseases which, after his death, was renamed the Robert Koch Institute in his honour. The million marks provided by the banker Bleichroeder to transform the erstwhile government house into this institute is a telling comment on the relevance of financial patronage for science and research.4 The Nobel Prize for Medicine and Physiology, bestowed on him in 1905, recognised both his discovery of the tubercular bacillus and its monumental impact on public hygiene measures, as well as the pioneering impact of his postulates on the broader understanding of infectious diseases as a whole.2 At the same time, the Nobel Prize presentation speech, with equal clarity, offered a critique on the controversy surrounding his ongoing experimentation with tuberculin as a form of therapy. Since 1982, 24th February has been designated ‘World Tuberculosis Day’ by the World Health Organization (WHO) to honour the day Koch first presented his findings on the aetiology of TB.
Frustrations, Dissent and Disappointment
The history of discoveries is replete with human emotions of exultation and despair. Convinced of his proposed ‘germ theory’ Koch went to great lengths to see, and show his sceptical colleagues, the germs that circulated in the blood in septicaemia. This, as we can well imagine, was no easy task but he developed the simple potato medium that would make the organisms multiply. Complemented with staining techniques, the organisms were revealed in all their glory. The Koch-Pasteur squabbles based on the physician versus chemist approach to disease created political boundaries that prevented the use of Koch’s culture techniques and Pasteur’s immunisation schedules in France and Germany, respectively.16 Elated by his triumphal march on TB he attempted to prove that tuberculin (a glycerine extract of the tubercle bacilli) would provide a cure for the disease. While tuberculin proved useful in diagnosis, it met with disappointment and failure in therapy.7 After the revolutionary highpoints of his early career, this setback was particularly difficult to accept. At the Fourth World Congress on TB, he vehemently opposed the notion that bovine TB could spread to humans, declaring, “I therefore consider it unnecessary to take any measures against this form of TB. The fight against TB clearly has to concentrate on the human bacillus”.17 Fortunately, his opponents won the day and milk pasteurisation became the norm.18
And the Story Continued...
The indefatigable war against TB continued in the wake of Koch’s discoveries and extended to other medical domains. Roentgen’s discovery of X-rays in 1896 was a giant leap forward in medical diagnostic tools.19 In addition to public health measures, the French bacteriologists Calmette and Guérin’s bovine tubercular strain created the Bacillus Calmette–Guérin (BCG) vaccine that turned the tide from a therapy-only approach to TB to one of active prevention.20 In 1944, for the first time, streptomycin showed a light at the end of the tunnel—although monotherapy left many with hearing loss for the rest of their lives. Soon, other drugs (rifampicin, pyrazinamide, para-amino salicylic acid, ethambutol, etc.) joined the fray and the philosophy of treatment rested on combinations in adequate doses for long periods of time. Since 1993, the adoption of the Directly Observed Treatment, Short-Course (DOTS) strategy by the WHO, as part of its Stop TB strategy, is credited with having made a significant impact on the global TB burden.21
Like many bacteria, the tubercular bacterium adopted wily ways of acquiring multi-drug resistance and the battle between it and newer drugs continues. Since the turn of the last century, the HIV-AIDS epidemic has rendered a mortal blow to attempts to control TB, especially in Sub-Saharan Africa. Industrialisation, urban slums and poverty are no longer the only determinants of disease prevalence. It is certain that as newer epidemics emerge, ‘old’ infections like the ‘white plague’ will seize the advantage and challenge generations of scientists to fight back through gruelling research efforts and newer weaponry.
Lessons From Koch’s Life and Times
Henle’s influence and Cohn’s support in Koch’s early experiments show us that pupils often surpass their gurus and surprise their peers by trailblazing their way into eternity. In today’s world of subspecialisation, it is pertinent to recall that a well-rounded knowledge of pathology and bacteriology integrated with a physician’s knowledge of human disease, combined with technology, microscopy, animal experiments and autopsies have been the mantra for the deluge of successful discoveries in the last two centuries. The discovery of the spore stage of bacterial dormancy in anthrax demonstrates that a hands-on approach to the laboratory bench can yield unexpected and astonishing results. Koch’s investigative forays as a district medical officer into anthrax were inspired by the affliction of country cattle in his rural backyard and his experiments were first performed in a makeshift laboratory in his own house on mice caught in his barn! His wife’s resilience and support needs no better endorsement. Research rests first and foremost on the ‘spirit’ of enquiry. Funding, state-of-art laboratories and fame are not necessary pre-requisites.
Koch’s insistence on use of tuberculin for therapy, despite the incontrovertible evidence to the contrary, illustrates the fact that spectacular discoveries may be followed by offbeat theories that are anticlimactic. Fame and acclaim can impose an unreasonable burden of expectations for a single man’s lifetime.
Biography
Seldom has an investigator been able to comprehend in advance with such clear-sightedness a new, unbroken field of investigation, and seldom has someone succeeded in working on it with the brilliance and success with which Robert Koch has done. Seldom have so many discoveries of such decisive significance to humanity stemmed from the activity of a single man, as is the case with him.1
Nobel Prize for Medicine or Physiology, Presentation Speech, Professor the Count K.A.H. Mörner, Rector of the Royal Caroline Institute (Karolinska Institute), Stockholm, Sweden, 10th December 1905.2

Robert Koch (1843–1910)1
References
- 1.Koch R. Zur Aetiologie des Milzbrandes. Mitteilungen aus dem Kaiserliche Gesundheitsamte. 1881;1:174–206. [Google Scholar]
- 2.Nobel Prize Laureates 1905. From: http://www.nobelprize.org/nobel_prizes/medicine/laureates/1905/press.html Accessed Oct 2013.
- 3.Lakhtakia R. Of animalcula, phthisis and scrofula – historical insights into tuberculosis in the pre-Koch era. Sultan Qaboos University Med J. 2013;13:486–90. doi: 10.12816/0003306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Munch R. Review. On the shoulders of giants. Robert Koch. Microbes Infect. 2003;5:69–74. doi: 10.1016/s1286-4579(02)00053-9. [DOI] [PubMed] [Google Scholar]
- 5.Blevins SM, Bronze MS. Robert Koch and the ‘golden age’ of bacteriology. Int J Infect Dis. 2010;14:e744–51. doi: 10.1016/j.ijid.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Gradmann C. Robert Koch and the pressures of scientific research: tuberculosis and tuberculin. Med Hist. 2001;45:1–32. doi: 10.1017/s0025727300000028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kaufmann SHE, Schaible UE. 100th anniversary of Robert Koch’s Nobel Prize for the discovery of the tubercle bacillus. Trends in Microbiol. 2005;13:469–75. doi: 10.1016/j.tim.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 8.Sakula A. Robert Koch (1843–1910): Founder of the science of bacteriology and discoverer of the tubercle bacillus. Br J Dis Chest. 1979;73:389–94. [PubMed] [Google Scholar]
- 9.Schwentker FN. Robert Koch (1843–1910) Invest Urol. 1964;2:300–1. [PubMed] [Google Scholar]
- 10.Lakhani SR. Early clinical pathologists: Robert Koch (1843–1910) J Clin Pathol. 1993;46:596–8. doi: 10.1136/jcp.46.7.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carter KC, editor. Essays of Robert Koch. Westport: Greenwood Press; 1987. p. 83. [Google Scholar]
- 12.Koch R. Die Aetiologie der Milzbrand-Krankheit, begründet auf die Entwicklungsgeschichte des Bacillus anthracis. Beiträge zur Biologie der Pflanzen. 1876;1:277–308. [Google Scholar]
- 13.Carter KC, editor. Essays of Robert Koch. Westport: Greenwood Press; 1987. pp. 9–25. [Google Scholar]
- 14.Koch R. Lecture at the first conference for discussion of the cholera question (1884) In: Carter KC, editor. Essays of Robert Koch. Westport: Greenwood Press; 1987. pp. 151–70. [Google Scholar]
- 15.Ligon BL. Robert Koch: Nobel laureate and controversial figure in tuberculin research. Semin Pediatr Infect Dis. 2002;13:289–99. doi: 10.1053/spid.2002.127205. [DOI] [PubMed] [Google Scholar]
- 16.Baxter AG. Louis Pasteur’s beer of revenge. Nature Rev Immunol. 2001;1:229–32. doi: 10.1038/35105083. [DOI] [PubMed] [Google Scholar]
- 17.Kaufmann SHE. A short history of Robert Koch’s fight against tuberculosis: those who do not remember the past are condemned to repeat it. Tuberculosis (Edinb) 2003;83:86–90. doi: 10.1016/s1472-9792(02)00064-1. [DOI] [PubMed] [Google Scholar]
- 18.Smith AE. Report on the International Congress on Tuberculosis. Ill Med J. 1909;15:303–10. [Google Scholar]
- 19.Roentgen WC. Über eine neue Art von Strahlen (Vorläufige Mitteilung) Sitzungsberichte der Physikalisch-Medizinischen Gesellschaft in Würzburg. 1895;137:132–141. [Google Scholar]; Weber AL. History of head and neck radiology: past, present, and future. Radiology. 2001;218:15–24. doi: 10.1148/radiology.218.1.r01ja2715. [DOI] [PubMed] [Google Scholar]
- 20.Luca S, Mihaescu T. History of BCG vaccine. Maedica (Buchar) 2013;8:53–8. [PMC free article] [PubMed] [Google Scholar]
- 21.Bayer R, Wilkinson D. Directly observed therapy for tuberculosis: history of an idea. Lancet. 1995;345:1545–8. doi: 10.1016/s0140-6736(95)91090-5. [DOI] [PubMed] [Google Scholar]