Abstract
Morbidity and mortality from sepsis remains unacceptably high. Large variability in clinical practice, plus the increasing awareness that certain processes of care associated with improved critical care outcomes, has led to the development of clinical practice guidelines in a variety of areas related to infection and sepsis. The Surviving Sepsis Guidelines for Management of Severe Sepsis and Septic Shock were first published in 2004, revised in 2008, and recently revised again and published in 2013. The first part of this manuscript is a summary of the 2013 guidelines with some editorial comment. The second part of the manuscript characterizes hospital based sepsis performance improvement programs and highlights the sepsis bundles from the Surviving Sepsis Campaign as a key component of such a program.
Keywords: guidelines, severe sepsis, sepsis bundles, resuscitation, performance improvement
Introduction
Morbidity and mortality from sepsis remains unacceptably high.1,2 Large variability in clinical practice, plus the increasing awareness that certain processes of care associated with improved critical care outcomes, has led to the development of clinical practice guidelines in a variety of areas related to infection and sepsis.3 The Surviving Sepsis Guidelines for Management of Severe Sepsis and Septic Shock were first published in 2004, revised in 2008, and recently revised again and published in 2013.4-6 The first part of this manuscript is a summary of the 2013 guidelines with some editorial comment. The second part of the manuscript characterizes hospital based sepsis performance improvement programs and highlights the sepsis bundles from the Surviving Sepsis Campaign as a key component of such a program.
Diagnostic Terminology
Sepsis is defined as infection plus systemic manifestations of infection7 (Table 1). Severe sepsis is defined as infection plus infection induced organ dysfunction or tissue hypoperfusion7 (Table 2). Sepsis induced hypotension is defined as infection induced decrease in blood pressure (systolic pressure <90 mmHg or mean arterial pressure <70 mmHg). Septic shock is defined as the requirement for vasopressors after initial fluid resuscitation fails to correct sepsis induced hypotension.7
Table 1. Diagnostic criteria for sepsis.
| Infection, documented, or suspected, and some of the following: |
|---|
| General variables |
| Fever, >38.3 °C |
| Hypothermia (core temperature <36 °C) |
| Heart rate >90/min−1 or more than two SD above the normal value for age |
| Tachypnea |
| Altered mental status |
| Significant edema or positive fluid balance (>20 mL/kg over 24 h) |
| Hyperglycemia (plasma glucose >140 mg/dL or 7.7 mmol/L) in the absence of diabetes |
| Inflammatory variables |
| Leukocytosis (WBC >12 000 μL−1) |
| Leukopenia (WBC count <4000 μL−1) |
| Normal WBC count with greater than 10% immature forms |
| Plasma C-reactive protein more than two SD above the normal value |
| Plasma procalcitonin more than 2 SD above the normal value |
| Hemodynamic variables |
| Arterial hypotension (SBP <90 mmHg, MAP <70 mmHG, or an SBP decrease >40 mmHg in adults or less than 2 SD below normal for age) |
| Organ dysfunction variables |
| Arterial hypoxemia (PaO2/FiO2 <300) |
| Acute oliguria (urine output <0.5 mL/kg/h for at least 2 h despite adequate fluid resuscitation) |
| Creatinine increase >0.5 mg/dL or 44.2 μmol/L |
| Coagulation abnormalities (INR >1.5 or aPTT >60 s) |
| Ileus (absent bowel sound) |
| Thrombocytopenia (platelet count <100 000 μL−1) |
| Hyperbilirubinemia (plasma total bilirubin >4 mg/dL or 70 μmol/L) |
| Tissue perfusion variables |
| Hyperlactatemia (>1 mmol/L) |
| Decreased capillary refill or mottling |
WBC, white blood cell; SBP, systolic blood pressure; MAP, mean arterial pressure; INR, international normalized ratio; aPTT, activated partial thromboplastin time. Diagnostic criteria for sepsis in the pediatric population are signs and symptoms of inflammation plus infection with hyper- or hypothermia (rectal temperature 38.5 °C or <35 °C), tachycardia (may be absent in hypothermic patients), and at least one of the following indications of altered organ function: altered mental status, hypoxemia, increased serum lactate level, or bounding pulses. Used with permission from reference 6 as adapted from reference 125.
Table 2. Severe sepsis.
| Severe sepsis definition = sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to the infection) |
|---|
| Sepsis-induced hypotension |
| Lactate above upper limits laboratory normal |
| Urine output <0.5 mL/kg/h for more than 2 h despite adequate fluid resuscitation |
| Acute lung injury with PaO2/FiO2 <250 in the absence of pneumonia as infection source |
| Acute lung injury with PaO2/FiO2 <200 in the presence of pneumonia as infection source |
| Creatinine >2.0 mg/dL (176.8 μmol/L) |
| Bilirubin >2 mg/dL (34.2 μmol/L) |
| Platelet count <100 000 μL |
| Coagulopathy (international normalized ratio >1.5) |
Management
Initial resuscitation
Protocolized, quantitative resuscitation of patients with sepsis-induced tissue hypoperfusion (defined as hypotension persisting after initial fluid challenge or a blood lactate concentration ≥4 mmol/L) is recommended.8-15 For the initial resuscitation of these patients the goals during the first 6 h of resuscitation include a central venous pressure 8–12 mmHg,16,17 a mean arterial pressure (MAP) ≥65 mmHg,18,19 a urine output ≥0.5 mL/kg/h, and a superior vena cava venous oxygen saturation of ≥70%.20
In patients who are found to initially have elevated lactate levels, targeting resuscitation to normalize lactate is suggested. Normalization of lactate seems a more appropriate goal than a percent reduction in baseline elevated lactate, although the latter has been demonstrated to be an effective resuscitation target variable.21,22 Where capability to measure central venous oxygen saturation does not exist, lactate clearance can be used as an alternative. Where both technologies are available, both targets are recommended.
Diagnosis of infection
Early diagnosis of sepsis, source of sepsis, and ideally causative organism is important.23-25 Two sets of blood cultures (both aerobic and anaerobic bottles) should be obtained before initiation of antimicrobial therapy unless it induces a significant delay (greater than 45 min) in the administration of antimicrobials.26,27 At least one of these blood cultures should be drawn percutaneously and one drawn through each vascular access device, unless the device was recently (less than 48 h) inserted. Imaging studies should be obtained promptly to confirm a potential infection source.
Prevention of selective oral decontamination and selective digestive decontamination should be considered as an ICU wide process to prevent the occurrence of sepsis and severe sepsis.28-30 Oral chlorhexidine gluconate is suggested as a form of oropharyngeal decontamination to reduce the risk of ventilator-associated pneumonia in ICU patients with severe sepsis.
Treatment of infection
Antimicrobials administered within the first hour of recognition of severe sepsis and septic shock should be the “goal” of therapy.31-36 Although an admirable goal, this time window is not the current standard of clinical practice. Initial empiric anti-infective therapy should be broad and target all likely pathogens and include antimicrobials that penetrate in adequate concentrations into the tissues presumed to be the source of sepsis. The antimicrobial regimen should be reassessed daily with the potential for de-escalation. Combination empirical therapy for a particular known or suspected infecting organism may be considered in certain patient groups such as neutropenic patients; patients with difficult-to-treat, multidrug-resistant bacterial pathogens; patients with severe infections associated with respiratory failure and septic shock and for septic shock from bacteremic pneumococcal infections.37-39 Empiric combination therapy should not be administered for more than 3–5 d. De-escalation to the most appropriate single drug therapy should be performed as soon as the susceptibility profile is known.
Duration of antimicrobial therapy is typically 7–10 d; however, longer courses may be appropriate in patients who have a slow clinical response, an undrainable focus of infection, bacteremia with Staphylococcus aureus, Pseudomonas ventilator-acquired pneumonia, as well as some fungal and viral infections or immunologic deficiencies, including neutropenia. Antiviral therapy should be initiated as early as possible in patients with severe sepsis or septic shock of viral origin including targeting influenza during flu outbreaks, such as H1N1.40
Source control is paramount.41,42 A specific anatomical diagnosis of infection requiring consideration for emergent source control should be sought and diagnosed or excluded as rapidly as possible, and intervention be undertaken for source control within the first 12 h after the diagnosis is made, if feasible. When source control is needed the “effective” intervention associated with the least physiologic insult should be considered (e.g., percutaneous rather than surgical drainage of an abscess). If intravascular access devices are a possible source of severe sepsis or septic shock, they should be removed promptly after another vascular access has been established. When infected peripancreatic necrosis is identified as a potential source of infection, definitive intervention is best delayed until adequate demarcation of viable and nonviable tissues has occurred.
Hemodynamic support
Crystalloids are the initial fluid of choice in the resuscitation of severe sepsis and septic shock.43 Hydroxyethyl starches are not recommended.44-46 Albumin is suggested to be added to crystalloid fluid resuscitation when patients require substantial amounts of crystalloids.47 Initial fluid challenge in patients with sepsis-induced tissue hypoperfusion with suspicion of hypovolemia should include a minimum of 30 mL/kg of crystalloids (a portion of this may be albumin equivalent). More rapid administration and greater amounts of fluid may be needed in some patients. Fluid challenge techniques should continue as long as there is hemodynamic improvement based either on dynamic (e.g., change in pulse pressure, stroke volume variation) or static (e.g., arterial pressure, heart rate) variables. Methods to assess intravascular volume such as echocardiography for assessment of left ventricular size or ultrasound assessment of inferior vena cava may also be used. Direct measurement of flow with assessment of effect of fluid boluses on stroke volume may be potentially useful, where that technology is available, and may include pulmonary artery catheters for thermodilution cardiac output measurement, esophageal Doppler for assessment of aortic flow and estimation of stroke volume based on arterial pressure waveform assessment using minimally invasive cardiac output measurement technologies such as LiDCO™, PiCCO®, and Flo Trac™. All of these devices have risks and some limitations.
Vasopressor therapy should initially target a mean arterial pressure (MAP) of ≥65 mmHg. Norepinephrine is the first choice vasopressor.48-50 When norepinephrine fails to achieve the MAP target, epinephrine added to and potentially substituted for norepinephrine may be needed to maintain adequate blood pressure.51,52 Alternatively, vasopressin up to 0.03 units/minute can be added to norepinephrine with the intent of either raising MAP or decreasing norepinephrine dosage.53 Low dose vasopressin is not recommended as the single initial vasopressor therapy and is not recommended to be used at doses higher than 0.03–0.04 units/minute unless used for salvage therapy (failure of other vasopressors to achieve adequate MAP). Dopamine as an alternative vasopressor agent to norepinephrine is in general discouraged but may be used in highly selected patients groups (e.g., patients with low risk of tachyarrhythmias and absolute or relative bradycardia).49 Phenylephrine is not recommended in the treatment of septic shock except in circumstances where (a) norepinephrine is associated with serious arrhythmias, (b) cardiac output is known to be high and blood pressure persistently low and difficult to maintain with vasopressor, or (c) as salvage therapy when combined inotrope/vasopressor drugs and low-dose vasopressin have failed to achieve MAP target. Low-dose dopamine should not be used for renal protection.54 All patients requiring vasopressor therapy should have an arterial catheter placed as soon as practical if resources are available.
During initial resuscitation dobutamine may be used to increase oxygen delivery in the presence of ongoing signs of hypoperfusion (such as lactic acidosis), despite achieving adequate intravascular volume and adequate MAP in patients with ScvO2 <70%. Following initial resuscitation of patients with sepsis induced hypoperfusion, where tissue hypoperfusion persists, a trail of dobutamine infusion up to 20 µg/kg/min may be administered singularly or added to vasopressor (if in use) in the presence of (a) myocardial dysfunction as suggested by elevated cardiac filling pressures and low cardiac output, or (b) ongoing signs of hypoperfusion, despite achieving adequate intravascular volume and adequate MAP.
Steroid therapy
Intravenous corticosteroids are not recommended in the treatment of adult septic shock if adequate fluid resuscitation and vasopressor therapy is able to restore hemodynamic stability.55-59 In case this goal is not achieved, intravenous hydrocortisone alone at a dose of 200 mg per day (50 mg q6h IV or 50 mg IV followed by 24 h continuous infusion to minimize swings in glucose) for up to 7 d is suggested.60,61 It is not necessary to use the ACTH stimulation test to identify adults with septic shock who should receive hydrocortisone. Instead, bedside clinical assessment as described above should be used. In patients treated with hydrocortisone for septic shock tapering should be performed when vasopressors are no longer required and steroids may be delivered for up to 7 d.62 Steroids should not be administered for the treatment of sepsis in the absence of shock.
Other supportive therapy of severe sepsis
Once tissue hypoperfusion has resolved and in the absence of extenuating circumstances, such as myocardial ischemia, severe hypoxemia, acute hemorrhage, or ischemic heart disease, red blood cell transfusion should occur only when hemoglobin concentration decreases to <7.0 g/dL.63 The anemia of severe sepsis should not be treated with erythropoietin unless another indication exists.64,65 Fresh frozen plasma should not be used to correct laboratory clotting abnormalities in the absence of bleeding or planned invasive procedures.66,67 Antithrombin is not indicated to treat severe sepsis.68,69 In patients with severe sepsis, and without significant risk of bleeding or with planned invasive procedures or active bleeding, transfusion threshold for platelets is <10 000/mm3.70 Platelets should be transfused when <20 000/mm3 if the patient has a significant risk of bleeding and platelet counts ≥50 000/mm3 should be maintained in the presence of active bleeding or if surgery or invasive procedures are needed. Immunoglobulins are not recommended in adult patients with severe sepsis or septic shock.71 Possibly exceptions include toxic shock syndrome or severe life threatening H1N1 ARDS. There is no current data that would support the use of intravenous selenium for the treatment of severe sepsis.
In the patient with sepsis induced acute respiratory distress syndrome (ARDS), ARDSnet lung protective strategy is recommended to include targeting 6 mL/kg predicted body weight (PBW) tidal volume and a plateau pressure ≤30 cm H2O.72 When a tidal volume of 6 mL/kg/PBW results in plateau pressure >30 cm H2O then tidal volume is decreased to as low as 4 mL/kg in 0.5 ml/kg/PBW increments in order to achieve a <30 cm H2O plateau pressure target. Plateau pressures higher than 30 cm H2O may be allowed in patients with increased chest wall or abdominal elastance (morbid obesity or anasarca). A level of positive end-expiratory pressure (PEEP) should be applied to avoid alveolar collapse at end expiration (atelectotrauma).73 Strategy based on higher rather than lower levels of PEEP is suggested for patients with sepsis-induced moderate or severe ARDS.74-77 Recruitment maneuvers are suggested in sepsis patients with ARDS induced severe refractory hypoxemia.78,79 Prone positioning is suggested to be used in sepsis-induced ARDS patients with a PaO2/FiO2 ratio ≤100 mmHg in facilities that have experience with such practices.80,81
A conservative rather than a liberal fluid strategy is recommended for patients with established sepsis-induced ARDS who do not have evidence of tissue hypoperfusion.82 Utilizing a CVP target of <4 mmHg is equally effective as using a pulmonary artery catheter to target a pulmonary artery occlusive pressure of <8 mmHg. In the absence of bronchospasm, β 2-agonists should not be used in patients with sepsis- induced ARDS.83 Neuromuscular blocking agents (NMBAs) should be avoided in the septic patient without ARDS;84,85 however, a short course of NMBA is suggested (for not greater than 48 h) in the patient with early sepsis induced ARDS and a PaO2/FiO2 <150 mmHg.86
When two consecutive glucose levels >180 mg/dL are encountered a continuous infusion of insulin should be instituted, targeting an upper blood glucose ≤180 mg/dL.87 Hypoglycemia should be avoided.88 Blood glucose values should be monitored every 1–2 h until glucose values and insulin infusion rates are stable and then every 4 h thereafter.88 Glucose levels obtained with point-of-care testing of capillary blood should be interpreted with caution, as such measurements may not accurately estimate arterial blood or plasma glucose values.89-91
Continuous renal replacement therapies and intermittent hemodialysis are equivalent in patients with severe sepsis and acute renal failure.92-96 The use of continuous renal replacement therapies to facilitate management of fluid balance in hemodynamically unstable septic patients is an acceptable approach. Sodium bicarbonate given to septic patients with tissue hypoperfusion and a pH ≥7.15 should not be expected to improve hemodynamics or decrease vasopressor requirement when compared with equimolar quantities of crystalloid.97,98
Deep vein thrombosis and stress ulcer prophylaxis are both recommended in the patient with severe sepsis.99-105 Deep vein thrombosis prophylaxis should be given with either daily low-molecular weight heparin (LMWH) or unfractionated heparin (UFH) thrice daily. If creatinine clearance is <30 mL/min and LMWH is given, either dalteparin or another form of LMWH with a low degree of renal metabolism or unfractionated heparin should be used. Severely septic patients with a contraindication to heparin use (e.g., clinically significant thrombocytopenia, severe coagulopathy, active bleeding, recent intracerebral hemorrhage), should receive mechanical prophylactic treatment such as graduated compression stockings or intermittent compression devices, unless contraindicated. It is suggested that patients with severe sepsis receive both pharmacologic therapy and intermittent pneumatic compression devices when there are no contraindications to the use of either therapies in patients with severe sepsis. Stress ulcer prophylaxis is strongly recommended with either an H2 blocker or a proton pump inhibitor. Proton pump inhibitors have a weak preference over H2 blockers.106,107 In the absence of risk factors, no stress ulcer prophylaxis should be given.
Within 48 h after a diagnosis of severe sepsis/septic shock administer oral or enteral feedings, as tolerated, rather than either complete fasting or provision of only intravenous glucose.108-111 Low dose feeding beginning with 500 calories per day (intravenous glucose plus enteral feeding) advanced as tolerated, is recommended over initial mandatory full caloric feeding (addition of TPN to achieve) in the first week. There is no indication for specific immunomodulating supplementation in patients with severe sepsis.112-114
In patients with severe sepsis and septic shock, it is important to discuss goals of care and prognosis with patients and families.115-117 As appropriate, the goals of care, including any end of life care planning or the use of palliative care principles should be accomplished. Although goals of care should be addressed as early as feasible, this should occur no later than 72 h following ICU admission.
See Tables S1–3 for concise summations of SSC guidelines recommendations.
Sepsis performance improvement programs118-120
Guidelines have little immediate impact on bedside behavior in the management of disease processes. Guidelines, however, serve as a resource document for creation of treatment protocols that when coupled with audit and feedback as part of a formal hospital based performance improvement initiative can change bedside practice. Bundles represent a number of treatment goals to be achieved in a disease process over a set time period and function as measurable quality indicators. When chart audit scores performance on bundle goals, and is followed by feedback to the treating clinicians (audit and feedback) bedside behavior is likely to change in line with guideline recommendations.
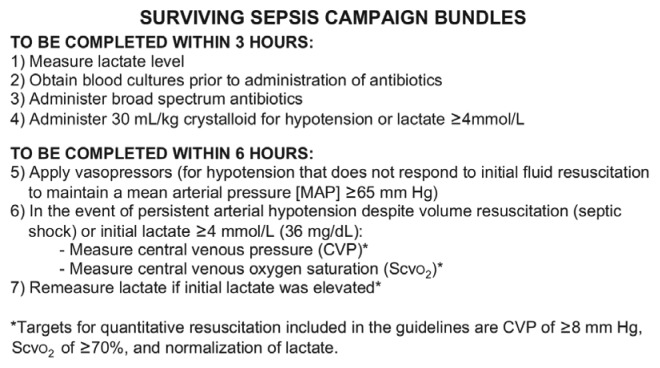
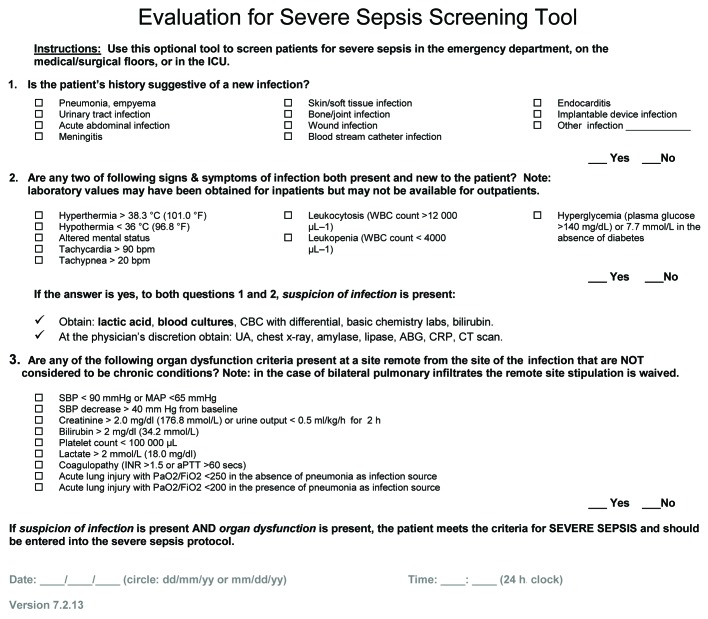
Sepsis bundles are created to act as a cohesive unit to ensure all steps of care are consistently delivered.121-124 The Surviving Sepsis Campaign and the Institute for Healthcare Improvement collaborated to apply the sepsis guidelines of 2004 to assemble two sepsis bundles, the 6-h resuscitation and 24-h management bundles. Following the creation of the 2012 guidelines, the bundles were revised, creating a 3-h and a 6-h bundle (Fig. 1). A free standardized database, provided by the Surviving Sepsis Campaign, allows hospitals to enter de-identified patient data and track sepsis bundle performance and outcomes. Participating hospitals are urged to transmit their Health Insurance Portability and Accountability Act (HIPAA) compliant data to a central repository at the Society of Critical Care Medicine for aggregate analysis. Queries of data and graphical display of bundle indicator performance can be retrieved locally using the electronic database. Patients are identified for entry into the database based on a standardized screening tool (Fig. 2). Steps to implement a sepsis protocol are shown in Table 3.
Figure 1. Surviving sepsis campaign bundles. Used with permission from reference 6.
Figure 2. Evaluation for severe sepsis screening tool. Online at http://www.survivingsepsis.org/SiteCollectionDocuments/ScreeningTool.pdf.
Table 3. Steps to implementing a sepsis protocol.
| • Obtain administrative support |
| • Evaluate inter-departmental interactions |
| • Develop and relay a firm understanding of the goals |
| • Establish a formal interactive relationship with the emergency department and the critical care unit |
| • Collaborate with the general/internal medicine team |
| • Identify champions/unit protocol leaders |
| • Provide a unit/hospital system wide education campaign |
Used with permission from reference 126.
Achieving performance improvement goals requires ongoing data collection and feedback. Protocols can be successful in changing bedside behavior only with the application of education and commitment of physician, nursing, and other health care professional champions from key areas of the hospital (ICU, ED, and hospital floors). Success of severe sepsis performance improvement programs require, not only champions but also multidisciplinary commitment from physicians, nurses, pharmacy, respiratory, and administration. Programs must be multispecialty as well, and include medicine, surgery, emergency medicine, and others. Establishing support from key ICU, ED, and floor leaders is crucial. Interdepartmental communication and collaboration facilitate seamless steps in the continuum of care, and give the best chance of success. And ultimately behavior is changed with audit and feedback.
Programs typically start with a hospital-wide education initiative, centered around early identification and familiarity with the treatment protocol that will be applied once the patient is identified. Educational sessions are conducted by members of the sepsis performance improvement leadership team. Education may be provided through departmental conferences, staff meetings, and unit-based in-services. Baseline data may or may not be collected prior to initiation of the formal performance improvement initiative. Data collection typically occurs Monday through Friday morning with a review of patients admitted to the ICU service over the last 24 h, applying the screening tool to ascertain if the patient qualifies for entry into the severe sepsis database. Performance is assessed periodically, typically quarterly through query of the database. The SSC software allows performance to be plotted and displayed over time with tables and linear or bar graphs. This display functions as the feedback tool. Evaluation of process change requires consistent data collection, measurement of indicators and feedback in order to facilitate performance improvement. Ongoing educational sessions to reinforce early identification and treatment steps continue in line with the protocol are needed. When roadblocks are encountered in process improvement a plan, do, study, act process (PDSA cycle) is employed to study the reasons for failure and to implement changes to improve process performance. This process includes initiation of a plan of action, studying results and when problems are identified, altering the plan to solve the problem. Since performance is being judged based on the time to accomplish the indicator, it is necessary to have a time zero (T0) representing when the clock starts ticking for scoring indicator compliance in treatment of severe sepsis. For ED admissions T0 is triage time. For patients presenting with severe sepsis in units other than the ED, T0 is the time that the chart reveals variables allowing the identification of the patient as having severe sepsis.
Conclusion
Only with early diagnosis and expedited treatment based on evidence based medicine can sepsis morbidity and mortality be decreased. Sepsis guidelines create a base to allow change in healthcare practitioner behavior, but lead to only modest slow change in bedside behavior. Change comes when institutions initiate a formal performance improvement program with a formal treatment protocol, education on early identification of severe sepsis patients, followed by audit of performance and periodic feedback to the healthcare professionals taking care of these patients.
Supplementary Material
Disclosure of Potential Conflicts of Interest
No potential conflicts of interest were disclosed.
References
- 1.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–10. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–54. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 3.Cinel I, Dellinger RP. Current treatment of severe sepsis. Curr Infect Dis Rep. 2006;8:358–65. doi: 10.1007/s11908-006-0046-0. [DOI] [PubMed] [Google Scholar]
- 4.Dellinger RP, Carlet JM, Masur H, Gerlach H, Calandra T, Cohen J, Gea-Banacloche J, Keh D, Marshall JC, Parker MM, et al. Surviving Sepsis Campaign Management Guidelines Committee Surviving Sepsis Campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32:858–73. doi: 10.1097/01.CCM.0000117317.18092.E4. [DOI] [PubMed] [Google Scholar]
- 5.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, Reinhart K, Angus DC, Brun-Buisson C, Beale R, et al. International Surviving Sepsis Campaign Guidelines Committee. American Association of Critical-Care Nurses. American College of Chest Physicians. American College of Emergency Physicians. Canadian Critical Care Society. European Society of Clinical Microbiology and Infectious Diseases. European Society of Intensive Care Medicine. European Respiratory Society. International Sepsis Forum. Japanese Association for Acute Medicine. Japanese Society of Intensive Care Medicine. Society of Critical Care Medicine. Society of Hospital Medicine. Surgical Infection Society. World Federation of Societies of Intensive and Critical Care Medicine Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 6.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R, et al. Surviving Sepsis Campaign Guidelines Committee including the Pediatric Subgroup Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637. doi: 10.1097/CCM.0b013e31827e83af. [DOI] [PubMed] [Google Scholar]
- 7.Dombrovskiy VY, Martin AA, Sunderram J, Paz HL. Rapid increase in hospitalization and mortality rates for severe sepsis in the United States: a trend analysis from 1993 to 2003. Crit Care Med. 2007;35:1244–50. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 8.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 9.Early Goal-Directed Therapy Collaborative Group of Zhejiang Province [The effect of early goal-directed therapy on treatment of critical patients with severe sepsis/septic shock: a multi-center, prospective, randomized, controlled study] Zhongguo Wei Zhong Bing Ji Jiu Yi Xue. 2010;22:331–4. [in Chinese] [PubMed] [Google Scholar]
- 10.Kortgen A, Niederprüm P, Bauer M. Implementation of an evidence-based “standard operating procedure” and outcome in septic shock. Crit Care Med. 2006;34:943–9. doi: 10.1097/01.CCM.0000206112.32673.D4. [DOI] [PubMed] [Google Scholar]
- 11.Sebat F, Johnson D, Musthafa AA, Watnik M, Moore S, Henry K, Saari M. A multidisciplinary community hospital program for early and rapid resuscitation of shock in nontrauma patients. Chest. 2005;127:1729–43. doi: 10.1378/chest.127.5.1729. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro NI, Howell MD, Talmor D, Lahey D, Ngo L, Buras J, Wolfe RE, Weiss JW, Lisbon A. implementation and outcomes of the multiple urgent sepsis therapies (MUST) protocol. Crit Care Med. 2006;34:1025–32. doi: 10.1097/01.CCM.0000206104.18647.A8. [DOI] [PubMed] [Google Scholar]
- 13.Micek ST, Roubinian N, Heuring T, Bode M, Williams J, Harrison C, Murphy T, Prentice D, Ruoff BE, Kollef MH. Before-after study of a standardized hospital order set for the management of septic shock. Crit Care Med. 2006;34:2707–13. doi: 10.1097/01.CCM.0000241151.25426.D7. [DOI] [PubMed] [Google Scholar]
- 14.Nguyen HB, Corbett SW, Steele R, Banta J, Clark RT, Hayes SR, Edwards J, Cho TW, Wittlake WA. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med. 2007;35:1105–12. doi: 10.1097/01.CCM.0000259463.33848.3D. [DOI] [PubMed] [Google Scholar]
- 15.Trzeciak S, Dellinger RP, Abate NL, Cowan RM, Stauss M, Kilgannon JH, Zanotti S, Parrillo JE. Translating research to clinical practice: a 1-year experience with implementing early goal-directed therapy for septic shock in the emergency department. Chest. 2006;129:225–32. doi: 10.1378/chest.129.2.225. [DOI] [PubMed] [Google Scholar]
- 16.Magder S. Central venous pressure: A useful but not so simple measurement. Crit Care Med. 2006;34:2224–7. doi: 10.1097/01.CCM.0000227646.98423.98. [DOI] [PubMed] [Google Scholar]
- 17.Vincent JL, Weil MH. Fluid challenge revisited. Crit Care Med. 2006;34:1333–7. doi: 10.1097/01.CCM.0000214677.76535.A5. [DOI] [PubMed] [Google Scholar]
- 18.Varpula M, Tallgren M, Saukkonen K, Voipio-Pulkki LM, Pettilä V. Hemodynamic variables related to outcome in septic shock. Intensive Care Med. 2005;31:1066–71. doi: 10.1007/s00134-005-2688-z. [DOI] [PubMed] [Google Scholar]
- 19.LeDoux D, Astiz ME, Carpati CM, Rackow EC. Effects of perfusion pressure on tissue perfusion in septic shock. Crit Care Med. 2000;28:2729–32. doi: 10.1097/00003246-200008000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, Peterson E, Tomlanovich M, Early Goal-Directed Therapy Collaborative Group Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 21.Jones AE, Shapiro NI, Trzeciak S, Arnold RC, Claremont HA, Kline JA, Emergency Medicine Shock Research Network (EMShockNet) Investigators Lactate clearance vs central venous oxygen saturation as goals of early sepsis therapy: a randomized clinical trial. JAMA. 2010;303:739–46. doi: 10.1001/jama.2010.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jansen TC, van Bommel J, Schoonderbeek FJ, Sleeswijk Visser SJ, van der Klooster JM, Lima AP, Willemsen SP, Bakker J, LACTATE study group Early lactate-guided therapy in intensive care unit patients: a multicenter, open-label, randomized controlled trial. Am J Respir Crit Care Med. 2010;182:752–61. doi: 10.1164/rccm.200912-1918OC. [DOI] [PubMed] [Google Scholar]
- 23.Moore LJ, Jones SL, Kreiner LA, McKinley B, Sucher JF, Todd SR, Turner KL, Valdivia A, Moore FA. Validation of a screening tool for the early identification of sepsis. J Trauma. 2009;66:1539–46, discussion 1546-7. doi: 10.1097/TA.0b013e3181a3ac4b. [DOI] [PubMed] [Google Scholar]
- 24.Evaluation for Severe Sepsis Screening Tool, Institute for Healthcare Improvement (IHI) http://www.ihi.org/IHI/Topics/CriticalCare/Sepsis/Tools/EvaluationforSevereSepsisScreeningTool.htm
- 25.Evaluation for severe sepsis screening tool. http://www.survivingsepsis.org/SiteCollectionDocuments/ScreeningTool.pdf
- 26.Weinstein MP, Reller LB, Murphy JR, Lichtenstein KA. The clinical significance of positive blood cultures: a comprehensive analysis of 500 episodes of bacteremia and fungemia in adults. I. Laboratory and epidemiologic observations. Rev Infect Dis. 1983;5:35–53. doi: 10.1093/clinids/5.1.35. [DOI] [PubMed] [Google Scholar]
- 27.Blot F, Schmidt E, Nitenberg G, Tancrède C, Leclercq B, Laplanche A, Andremont A. Earlier positivity of central-venous- versus peripheral-blood cultures is highly predictive of catheter-related sepsis. J Clin Microbiol. 1998;36:105–9. doi: 10.1128/jcm.36.1.105-109.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Jonge E, Schultz MJ, Spanjaard L, Bossuyt PM, Vroom MB, Dankert J, Kesecioglu J. Effects of selective decontamination of digestive tract on mortality and acquisition of resistant bacteria in intensive care: a randomised controlled trial. Lancet. 2003;362:1011–6. doi: 10.1016/S0140-6736(03)14409-1. [DOI] [PubMed] [Google Scholar]
- 29.de Smet AM, Kluytmans JA, Cooper BS, Mascini EM, Benus RF, van der Werf TS, van der Hoeven JG, Pickkers P, Bogaers-Hofman D, van der Meer NJ, et al. Decontamination of the digestive tract and oropharynx in ICU patients. N Engl J Med. 2009;360:20–31. doi: 10.1056/NEJMoa0800394. [DOI] [PubMed] [Google Scholar]
- 30.Cuthbertson BH, Francis J, Campbell MK, MacIntyre L, Seppelt I, Grimshaw J, SuDDICU study groups A study of the perceived risks, benefits and barriers to the use of SDD in adult critical care units (the SuDDICU study) Trials. 2010;11:117. doi: 10.1186/1745-6215-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–96. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 32.Morrell M, Fraser VJ, Kollef MH. Delaying the empiric treatment of candida bloodstream infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrob Agents Chemother. 2005;49:3640–5. doi: 10.1128/AAC.49.9.3640-3645.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barie PS, Hydo LJ, Shou J, Larone DH, Eachempati SR. Influence of antibiotic therapy on mortality of critical surgical illness caused or complicated by infection. Surg Infect (Larchmt) 2005;6:41–54. doi: 10.1089/sur.2005.6.41. [DOI] [PubMed] [Google Scholar]
- 34.Leibovici L, Shraga I, Drucker M, Konigsberger H, Samra Z, Pitlik SD. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med. 1998;244:379–86. doi: 10.1046/j.1365-2796.1998.00379.x. [DOI] [PubMed] [Google Scholar]
- 35.Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118:146–55. doi: 10.1378/chest.118.1.146. [DOI] [PubMed] [Google Scholar]
- 36.Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R, et al. Surviving Sepsis Campaign The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367–74. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 37.Micek ST, Welch EC, Khan J, Pervez M, Doherty JA, Reichley RM, Kollef MH. Empiric combination antibiotic therapy is associated with improved outcome against sepsis due to Gram-negative bacteria: a retrospective analysis. Antimicrob Agents Chemother. 2010;54:1742–8. doi: 10.1128/AAC.01365-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Al-Hasan MN, Wilson JW, Lahr BD, Thomsen KM, Eckel-Passow JE, Vetter EA, Tleyjeh IM, Baddour LM. Beta-lactam and fluoroquinolone combination antibiotic therapy for bacteremia caused by gram-negative bacilli. Antimicrob Agents Chemother. 2009;53:1386–94. doi: 10.1128/AAC.01231-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Martin-Loeches I, Lisboa T, Rodriguez A, Putensen C, Annane D, Garnacho-Montero J, Restrepo MI, Rello J. Combination antibiotic therapy with macrolides improves survival in intubated patients with community-acquired pneumonia. Intensive Care Med. 2010;36:612–20. doi: 10.1007/s00134-009-1730-y. [DOI] [PubMed] [Google Scholar]
- 40.Smith JR, Ariano RE, Toovey S. The use of antiviral agents for the management of severe influenza. Crit Care Med. 2010;38(Suppl):e43–51. doi: 10.1097/CCM.0b013e3181c85229. [DOI] [PubMed] [Google Scholar]
- 41.Jimenez MF, Marshall JC, International Sepsis Forum Source control in the management of sepsis. Intensive Care Med. 2001;27(Suppl 1):S49–62. doi: 10.1007/PL00003797. [DOI] [PubMed] [Google Scholar]
- 42.Boyer A, Vargas F, Coste F, Saubusse E, Castaing Y, Gbikpi-Benissan G, Hilbert G, Gruson D. Influence of surgical treatment timing on mortality from necrotizing soft tissue infections requiring intensive care management. Intensive Care Med. 2009;35:847–53. doi: 10.1007/s00134-008-1373-4. [DOI] [PubMed] [Google Scholar]
- 43.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, SAFE Study Investigators A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 44.Guidet B, Martinet O, Boulain T, Philippart F, Poussel JF, Maizel J, Forceville X, Feissel M, Hasselmann M, Heininger A, et al. Assessment of hemodynamic efficacy and safety of 6% hydroxyethylstarch 130/0.4 vs. 0.9% NaCl fluid replacement in patients with severe sepsis: The CRYSTMAS study. Crit Care. 2012;16:R94. doi: 10.1186/cc11358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Perner A, Haase N, Guttormsen AB, Tenhunen J, Klemenzson G, Åneman A, Madsen KR, Møller MH, Elkjær JM, Poulsen LM, et al. 6S Trial Group. Scandinavian Critical Care Trials Group Hydroxyethyl starch 130/0.42 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34. doi: 10.1056/NEJMoa1204242. [DOI] [PubMed] [Google Scholar]
- 46.Myburgh JA, Finfer S, Bellomo R, Billot L, Cass A, Gattas D, Glass P, Lipman J, Liu B, McArthur C, et al. CHEST Investigators. Australian and New Zealand Intensive Care Society Clinical Trials Group Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11. doi: 10.1056/NEJMoa1209759. [DOI] [PubMed] [Google Scholar]
- 47.Delaney AP, Dan A, McCaffrey J, Finfer S. The role of albumin as a resuscitation fluid for patients with sepsis: a systematic review and meta-analysis. Crit Care Med. 2011;39:386–91. doi: 10.1097/CCM.0b013e3181ffe217. [DOI] [PubMed] [Google Scholar]
- 48.Martin C, Viviand X, Leone M, Thirion X. Effect of norepinephrine on the outcome of septic shock. Crit Care Med. 2000;28:2758–65. doi: 10.1097/00003246-200008000-00012. [DOI] [PubMed] [Google Scholar]
- 49.De Backer D, Biston P, Devriendt J, Madl C, Chochrad D, Aldecoa C, Brasseur A, Defrance P, Gottignies P, Vincent JL, SOAP II Investigators Comparison of dopamine and norepinephrine in the treatment of shock. N Engl J Med. 2010;362:779–89. doi: 10.1056/NEJMoa0907118. [DOI] [PubMed] [Google Scholar]
- 50.De Backer D, Aldecoa C, Njimi H, Vincent JL. Dopamine versus norepinephrine in the treatment of septic shock: a meta-analysis*. Crit Care Med. 2012;40:725–30. doi: 10.1097/CCM.0b013e31823778ee. [DOI] [PubMed] [Google Scholar]
- 51.Annane D, Vignon P, Renault A, Bollaert PE, Charpentier C, Martin C, Troché G, Ricard JD, Nitenberg G, Papazian L, et al. CATS Study Group Norepinephrine plus dobutamine versus epinephrine alone for management of septic shock: a randomised trial. Lancet. 2007;370:676–84. doi: 10.1016/S0140-6736(07)61344-0. [DOI] [PubMed] [Google Scholar]
- 52.Myburgh JA, Higgins A, Jovanovska A, Lipman J, Ramakrishnan N, Santamaria J, CAT Study investigators A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008;34:2226–34. doi: 10.1007/s00134-008-1219-0. [DOI] [PubMed] [Google Scholar]
- 53.Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, et al. VASST Investigators Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358:877–87. doi: 10.1056/NEJMoa067373. [DOI] [PubMed] [Google Scholar]
- 54.Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J, Australian and New Zealand Intensive Care Society (ANZICS) Clinical Trials Group Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Lancet. 2000;356:2139–43. doi: 10.1016/S0140-6736(00)03495-4. [DOI] [PubMed] [Google Scholar]
- 55.Annane D, Sébille V, Charpentier C, Bollaert PE, François B, Korach JM, Capellier G, Cohen Y, Azoulay E, Troché G, et al. Effect of treatment with low doses of hydrocortisone and fludrocortisone on mortality in patients with septic shock. JAMA. 2002;288:862–71. doi: 10.1001/jama.288.7.862. [DOI] [PubMed] [Google Scholar]
- 56.Briegel J, Forst H, Haller M, Schelling G, Kilger E, Kuprat G, Hemmer B, Hummel T, Lenhart A, Heyduck M, et al. Stress doses of hydrocortisone reverse hyperdynamic septic shock: a prospective, randomized, double-blind, single-center study. Crit Care Med. 1999;27:723–32. doi: 10.1097/00003246-199904000-00025. [DOI] [PubMed] [Google Scholar]
- 57.Bollaert PE, Charpentier C, Levy B, Debouverie M, Audibert G, Larcan A. Reversal of late septic shock with supraphysiologic doses of hydrocortisone. Crit Care Med. 1998;26:645–50. doi: 10.1097/00003246-199804000-00010. [DOI] [PubMed] [Google Scholar]
- 58.Sprung CL, Annane D, Keh D, Moreno R, Singer M, Freivogel K, Weiss YG, Benbenishty J, Kalenka A, Forst H, et al. CORTICUS Study Group Hydrocortisone therapy for patients with septic shock. N Engl J Med. 2008;358:111–24. doi: 10.1056/NEJMoa071366. [DOI] [PubMed] [Google Scholar]
- 59.Annane D, Bellissant E, Bollaert PE, Briegel J, Confalonieri M, De Gaudio R, Keh D, Kupfer Y, Oppert M, Meduri GU. Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA. 2009;301:2362–75. doi: 10.1001/jama.2009.815. [DOI] [PubMed] [Google Scholar]
- 60.Huh JW, Choi HS, Lim CM, Koh Y, Oh YM, Shim TS, Lee SD, Kim WS, Kim DS, Hong SB. Low-dose hydrocortisone treatment for patients with septic shock: a pilot study comparing 3days with 7days. Respirology. 2011;16:1088–95. doi: 10.1111/j.1440-1843.2011.02018.x. [DOI] [PubMed] [Google Scholar]
- 61.Weber-Carstens S, Deja M, Bercker S, Dimroth A, Ahlers O, Kaisers U, Keh D. Impact of bolus application of low-dose hydrocortisone on glycemic control in septic shock patients. Intensive Care Med. 2007;33:730–3. doi: 10.1007/s00134-007-0540-3. [DOI] [PubMed] [Google Scholar]
- 62.Keh D, Boehnke T, Weber-Cartens S, Schulz C, Ahlers O, Bercker S, Volk HD, Doecke WD, Falke KJ, Gerlach H. Immunologic and hemodynamic effects of “low-dose” hydrocortisone in septic shock: a double-blind, randomized, placebo-controlled, crossover study. Am J Respir Crit Care Med. 2003;167:512–20. doi: 10.1164/rccm.200205-446OC. [DOI] [PubMed] [Google Scholar]
- 63.Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, Tweeddale M, Schweitzer I, Yetisir E. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 64.Corwin HL, Gettinger A, Rodriguez RM, Pearl RG, Gubler KD, Enny C, Colton T, Corwin MJ. Efficacy of recombinant human erythropoietin in the critically ill patient: a randomized, double-blind, placebo-controlled trial. Crit Care Med. 1999;27:2346–50. doi: 10.1097/00003246-199911000-00004. [DOI] [PubMed] [Google Scholar]
- 65.Corwin HL, Gettinger A, Pearl RG, Fink MP, Levy MM, Shapiro MJ, Corwin MJ, Colton T, EPO Critical Care Trials Group Efficacy of recombinant human erythropoietin in critically ill patients: a randomized controlled trial. JAMA. 2002;288:2827–35. doi: 10.1001/jama.288.22.2827. [DOI] [PubMed] [Google Scholar]
- 66.Liumbruno G, Bennardello F, Lattanzio A, Piccoli P, Rossetti G, Italian Society of Transfusion Medicine and Immunohaematology (SIMTI) Work Group Recommendations for the transfusion of plasma and platelets. Blood Transfus. 2009;7:132–50. doi: 10.2450/2009.0005-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stanworth SJ, Walsh TS, Prescott RJ, Lee RJ, Watson DM, Wyncoll D, Intensive Care Study of Coagulopathy (ISOC) investigators A national study of plasma use in critical care: clinical indications, dose and effect on prothrombin time. Crit Care. 2011;15:R108. doi: 10.1186/cc10129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Warren BL, Eid A, Singer P, Pillay SS, Carl P, Novak I, Chalupa P, Atherstone A, Pénzes I, Kübler A, et al. KyberSept Trial Study Group Caring for the critically ill patient. High-dose antithrombin III in severe sepsis: a randomized controlled trial. JAMA. 2001;286:1869–78. doi: 10.1001/jama.286.15.1869. [DOI] [PubMed] [Google Scholar]
- 69.Wiedermann CJ, Hoffmann JN, Juers M, Ostermann H, Kienast J, Briegel J, Strauss R, Keinecke HO, Warren BL, Opal SM, KyberSept Investigators High-dose antithrombin III in the treatment of severe sepsis in patients with a high risk of death: efficacy and safety. Crit Care Med. 2006;34:285–92. doi: 10.1097/01.CCM.0000194731.08896.99. [DOI] [PubMed] [Google Scholar]
- 70.British Committee for Standards in Haematology, Blood Transfusion Task Force Guidelines for the use of platelet transfusions. Br J Haematol. 2003;122:10–23. doi: 10.1046/j.1365-2141.2003.04468.x. [DOI] [PubMed] [Google Scholar]
- 71.Alejandria MM, Lansang MA, Dans LF, Mantaring JB. Intravenous immunoglobulin for treating sepsis and septic shock. Cochrane Database Syst Rev. 2002;1:CD001090. doi: 10.1002/14651858.CD001090. [DOI] [PubMed] [Google Scholar]
- 72.The Acute Respiratory Distress Syndrome Network Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342:1301–8. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 73.Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, et al. Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med. 1998;338:347–54. doi: 10.1056/NEJM199802053380602. [DOI] [PubMed] [Google Scholar]
- 74.Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, et al. Expiratory Pressure (Express) Study Group Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:646–55. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 75.Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, Davies AR, Hand LE, Zhou Q, Thabane L, et al. Lung Open Ventilation Study Investigators Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299:637–45. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 76.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 77.Briel M, Meade M, Mercat A, Brower RG, Talmor D, Walter SD, Slutsky AS, Pullenayegum E, Zhou Q, Cook D, et al. Higher vs lower positive end-expiratory pressure in patients with acute lung injury and acute respiratory distress syndrome: systematic review and meta-analysis. JAMA. 2010;303:865–73. doi: 10.1001/jama.2010.218. [DOI] [PubMed] [Google Scholar]
- 78.Gattinoni L, Caironi P, Cressoni M, Chiumello D, Ranieri VM, Quintel M, Russo S, Patroniti N, Cornejo R, Bugedo G. Lung recruitment in patients with the acute respiratory distress syndrome. N Engl J Med. 2006;354:1775–86. doi: 10.1056/NEJMoa052052. [DOI] [PubMed] [Google Scholar]
- 79.Fan E, Wilcox ME, Brower RG, Stewart TE, Mehta S, Lapinsky SE, Meade MO, Ferguson ND. Recruitment maneuvers for acute lung injury: a systematic review. Am J Respir Crit Care Med. 2008;178:1156–63. doi: 10.1164/rccm.200802-335OC. [DOI] [PubMed] [Google Scholar]
- 80.Mancebo J, Fernández R, Blanch L, Rialp G, Gordo F, Ferrer M, Rodríguez F, Garro P, Ricart P, Vallverdú I, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006;173:1233–9. doi: 10.1164/rccm.200503-353OC. [DOI] [PubMed] [Google Scholar]
- 81.Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NK, Latini R, Pesenti A, Guérin C, Mancebo J, Curley MA, et al. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 2010;36:585–99. doi: 10.1007/s00134-009-1748-1. [DOI] [PubMed] [Google Scholar]
- 82.Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF, Jr., Hite RD, Harabin AL, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network Comparison of two fluid-management strategies in acute lung injury. N Engl J Med. 2006;354:2564–75. doi: 10.1056/NEJMoa062200. [DOI] [PubMed] [Google Scholar]
- 83.Gao Smith F, Perkins GD, Gates S, Young D, McAuley DF, Tunnicliffe W, Khan Z, Lamb SE, BALTI-2 study investigators Effect of intravenous β-2 agonist treatment on clinical outcomes in acute respiratory distress syndrome (BALTI-2): a multicentre, randomised controlled trial. Lancet. 2012;379:229–35. doi: 10.1016/S0140-6736(11)61623-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Meyer KC, Prielipp RC, Grossman JE, Coursin DB. Prolonged weakness after infusion of atracurium in two intensive care unit patients. Anesth Analg. 1994;78:772–4. doi: 10.1213/00000539-199404000-00027. [DOI] [PubMed] [Google Scholar]
- 85.Lacomis D, Petrella JT, Giuliani MJ. Causes of neuromuscular weakness in the intensive care unit: a study of ninety-two patients. Muscle Nerve. 1998;21:610–7. doi: 10.1002/(SICI)1097-4598(199805)21:5<610::AID-MUS7>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 86.Papazian L, Forel JM, Gacouin A, Penot-Ragon C, Perrin G, Loundou A, Jaber S, Arnal JM, Perez D, Seghboyan JM, et al. ACURASYS Study Investigators Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med. 2010;363:1107–16. doi: 10.1056/NEJMoa1005372. [DOI] [PubMed] [Google Scholar]
- 87.Finfer S, Chittock DR, Su SY, Blair D, Foster D, Dhingra V, Bellomo R, Cook D, Dodek P, Henderson WR, et al. NICE-SUGAR Study Investigators Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97. doi: 10.1056/NEJMoa0810625. [DOI] [PubMed] [Google Scholar]
- 88.Jacobi J, Bircher N, Krinsley J, Agus M, Braithwaite SS, Deutschman C, Freire AX, Geehan D, Kohl B, Nasraway SA, et al. Guidelines for the use of an insulin infusion for the management of hyperglycemia in critically ill patients. Crit Care Med. 2012;40:3251–76. doi: 10.1097/CCM.0b013e3182653269. [DOI] [PubMed] [Google Scholar]
- 89.Kanji S, Buffie J, Hutton B, Bunting PS, Singh A, McDonald K, Fergusson D, McIntyre LA, Hebert PC. Reliability of point-of-care testing for glucose measurement in critically ill adults. Crit Care Med. 2005;33:2778–85. doi: 10.1097/01.CCM.0000189939.10881.60. [DOI] [PubMed] [Google Scholar]
- 90.Hoedemaekers CW, Klein Gunnewiek JM, Prinsen MA, Willems JL, Van der Hoeven JG. Accuracy of bedside glucose measurement from three glucometers in critically ill patients. Crit Care Med. 2008;36:3062–6. doi: 10.1097/CCM.0b013e318186ffe6. [DOI] [PubMed] [Google Scholar]
- 91.Khan AI, Vasquez Y, Gray J, Wians FH, Jr., Kroll MH. The variability of results between point-of-care testing glucose meters and the central laboratory analyzer. Arch Pathol Lab Med. 2006;130:1527–32. doi: 10.5858/2006-130-1527-TVORBP. [DOI] [PubMed] [Google Scholar]
- 92.Guérin C, Girard R, Selli JM, Ayzac L. Intermittent versus continuous renal replacement therapy for acute renal failure in intensive care units: results from a multicenter prospective epidemiological survey. Intensive Care Med. 2002;28:1411–8. doi: 10.1007/s00134-002-1433-0. [DOI] [PubMed] [Google Scholar]
- 93.Kellum JA, Angus DC, Johnson JP, Leblanc M, Griffin M, Ramakrishnan N, Linde-Zwirble WT. Continuous versus intermittent renal replacement therapy: a meta-analysis. Intensive Care Med. 2002;28:29–37. doi: 10.1007/s00134-001-1159-4. [DOI] [PubMed] [Google Scholar]
- 94.Tonelli M, Manns B, Feller-Kopman D. Acute renal failure in the intensive care unit: a systematic review of the impact of dialytic modality on mortality and renal recovery. Am J Kidney Dis. 2002;40:875–85. doi: 10.1053/ajkd.2002.36318. [DOI] [PubMed] [Google Scholar]
- 95.Mehta RL, McDonald B, Gabbai FB, Pahl M, Pascual MT, Farkas A, Kaplan RM, Collaborative Group for Treatment of ARF in the ICU A randomized clinical trial of continuous versus intermittent dialysis for acute renal failure. Kidney Int. 2001;60:1154–63. doi: 10.1046/j.1523-1755.2001.0600031154.x. [DOI] [PubMed] [Google Scholar]
- 96.Vinsonneau C, Camus C, Combes A, Costa de Beauregard MA, Klouche K, Boulain T, Pallot JL, Chiche JD, Taupin P, Landais P, et al. Hemodiafe Study Group Continuous venovenous haemodiafiltration versus intermittent haemodialysis for acute renal failure in patients with multiple-organ dysfunction syndrome: a multicentre randomised trial. Lancet. 2006;368:379–85. doi: 10.1016/S0140-6736(06)69111-3. [DOI] [PubMed] [Google Scholar]
- 97.Cooper DJ, Walley KR, Wiggs BR, Russell JA. Bicarbonate does not improve hemodynamics in critically ill patients who have lactic acidosis. A prospective, controlled clinical study. Ann Intern Med. 1990;112:492–8. doi: 10.7326/0003-4819-112-7-492. [DOI] [PubMed] [Google Scholar]
- 98.Mathieu D, Neviere R, Billard V, Fleyfel M, Wattel F. Effects of bicarbonate therapy on hemodynamics and tissue oxygenation in patients with lactic acidosis: a prospective, controlled clinical study. Crit Care Med. 1991;19:1352–6. doi: 10.1097/00003246-199111000-00008. [DOI] [PubMed] [Google Scholar]
- 99.Belch JJ, Lowe GD, Ward AG, Forbes CD, Prentice CR. Prevention of deep vein thrombosis in medical patients by low-dose heparin. Scott Med J. 1981;26:115–7. doi: 10.1177/003693308102600205. [DOI] [PubMed] [Google Scholar]
- 100.Samama MM, Cohen AT, Darmon JY, Desjardins L, Eldor A, Janbon C, Leizorovicz A, Nguyen H, Olsson CG, Turpie AG, et al. Prophylaxis in Medical Patients with Enoxaparin Study Group A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. N Engl J Med. 1999;341:793–800. doi: 10.1056/NEJM199909093411103. [DOI] [PubMed] [Google Scholar]
- 101.Cook D, Meade M, Guyatt G, Walter S, Heels-Ansdell D, Warkentin TE, Zytaruk N, Crowther M, Geerts W, Cooper DJ, et al. PROTECT Investigators for the Canadian Critical Care Trials Group and the Australian and New Zealand Intensive Care Society Clinical Trials Group Dalteparin versus unfractionated heparin in critically ill patients. N Engl J Med. 2011;364:1305–14. doi: 10.1056/NEJMoa1014475. [DOI] [PubMed] [Google Scholar]
- 102.King CS, Holley AB, Jackson JL, Shorr AF, Moores LK. Twice vs three times daily heparin dosing for thromboembolism prophylaxis in the general medical population: A metaanalysis. Chest. 2007;131:507–16. doi: 10.1378/chest.06-1861. [DOI] [PubMed] [Google Scholar]
- 103.Vanek VW. Meta-analysis of effectiveness of intermittent pneumatic compression devices with a comparison of thigh-high to knee-high sleeves. Am Surg. 1998;64:1050–8. [PubMed] [Google Scholar]
- 104.Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuünemann HJ; American College of Chest Physicians Antithrombotic Therapy and Prevention of Thrombosis Panel. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141(Suppl 2):7S–47S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Cook DJ, Reeve BK, Guyatt GH, Heyland DK, Griffith LE, Buckingham L, Tryba M. Stress ulcer prophylaxis in critically ill patients. Resolving discordant meta-analyses. JAMA. 1996;275:308–14. doi: 10.1001/jama.1996.03530280060038. [DOI] [PubMed] [Google Scholar]
- 106.Lin PC, Chang CH, Hsu PI, Tseng PL, Huang YB. The efficacy and safety of proton pump inhibitors vs histamine-2 receptor antagonists for stress ulcer bleeding prophylaxis among critical care patients: a meta-analysis. Crit Care Med. 2010;38:1197–205. doi: 10.1097/CCM.0b013e3181d69ccf. [DOI] [PubMed] [Google Scholar]
- 107.Pongprasobchai S, Kridkratoke S, Nopmaneejumruslers C. Proton pump inhibitors for the prevention of stress-related mucosal disease in critically-ill patients: a meta-analysis. J Med Assoc Thai. 2009;92:632–7. [PubMed] [Google Scholar]
- 108.Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK. Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition. 2004;20:843–8. doi: 10.1016/j.nut.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 109.Dhaliwal R, Jurewitsch B, Harrietha D, Heyland DK. Combination enteral and parenteral nutrition in critically ill patients: harmful or beneficial? A systematic review of the evidence. Intensive Care Med. 2004;30:1666–71. doi: 10.1007/s00134-004-2345-y. [DOI] [PubMed] [Google Scholar]
- 110.Simpson F, Doig GS. Parenteral vs. enteral nutrition in the critically ill patient: a meta-analysis of trials using the intention to treat principle. Intensive Care Med. 2005;31:12–23. doi: 10.1007/s00134-004-2511-2. [DOI] [PubMed] [Google Scholar]
- 111.Casaer MP, Mesotten D, Hermans G, Wouters PJ, Schetz M, Meyfroidt G, Van Cromphaut S, Ingels C, Meersseman P, Muller J, et al. Early versus late parenteral nutrition in critically ill adults. N Engl J Med. 2011;365:506–17. doi: 10.1056/NEJMoa1102662. [DOI] [PubMed] [Google Scholar]
- 112.Beale RJ, Bryg DJ, Bihari DJ. Immunonutrition in the critically ill: a systematic review of clinical outcome. Crit Care Med. 1999;27:2799–805. doi: 10.1097/00003246-199912000-00032. [DOI] [PubMed] [Google Scholar]
- 113.Montejo JC, Zarazaga A, López-Martínez J, Urrútia G, Roqué M, Blesa AL, Celaya S, Conejero R, Galbán C, García de Lorenzo A, et al. Spanish Society of Intensive Care Medicine and Coronary Units Immunonutrition in the intensive care unit. A systematic review and consensus statement. Clin Nutr. 2003;22:221–33. doi: 10.1016/S0261-5614(03)00007-4. [DOI] [PubMed] [Google Scholar]
- 114.Marik PE, Zaloga GP. Immunonutrition in critically ill patients: a systematic review and analysis of the literature. Intensive Care Med. 2008;34:1980–90. doi: 10.1007/s00134-008-1213-6. [DOI] [PubMed] [Google Scholar]
- 115.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182:905–9. doi: 10.1164/rccm.201002-0262OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bertolini G, Boffelli S, Malacarne P, Peta M, Marchesi M, Barbisan C, Tomelleri S, Spada S, Satolli R, Gridelli B, et al. End-of-life decision-making and quality of ICU performance: an observational study in 84 Italian units. Intensive Care Med. 2010;36:1495–504. doi: 10.1007/s00134-010-1910-9. [DOI] [PubMed] [Google Scholar]
- 117.Scheunemann LP, McDevitt M, Carson SS, Hanson LC. Randomized, controlled trials of interventions to improve communication in intensive care: a systematic review. Chest. 2011;139:543–54. doi: 10.1378/chest.10-0595. [DOI] [PubMed] [Google Scholar]
- 118.Schorr C, Dellinger RP. Performance improvement in the management of severe sepsis. In: Atualizaçao Em Medicina Intensiva. Valter Nilton Felix (eds). São Paulo, Ed. Do Autor, 2010:23-27. [Google Scholar]
- 119.Schorr C. Performance improvement in the management of sepsis. Crit Care Clin. 2009;25:857–67, x. doi: 10.1016/j.ccc.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 120.Townsend SR, Schorr C, Levy MM, Dellinger RP. Reducing mortality in severe sepsis: the Surviving Sepsis Campaign. Clin Chest Med. 2008;29:721–33, x. doi: 10.1016/j.ccm.2008.06.011. [DOI] [PubMed] [Google Scholar]
- 121.Gao F, Melody T, Daniels DF, Giles S, Fox S. The impact of compliance with 6-hour and 24-hour sepsis bundles on hospital mortality in patients with severe sepsis: a prospective observational study. Crit Care. 2005;9:R764–70. doi: 10.1186/cc3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pestaña D, Espinosa E, Sangüesa-Molina JR, Ramos R, Pérez-Fernández E, Duque M, Martínez-Casanova E, REASEP Sepsis Study Group Compliance with a sepsis bundle and its effect on intensive care unit mortality in surgical septic shock patients. J Trauma. 2010;69:1282–7. doi: 10.1097/TA.0b013e3181c4539f. [DOI] [PubMed] [Google Scholar]
- 123.Levy MM, Pronovost PJ, Dellinger RP, Townsend S, Resar RK, Clemmer TP, Ramsay G. Sepsis change bundles: converting guidelines into meaningful change in behavior and clinical outcome. Crit Care Med. 2004;32(Suppl):S595–7. doi: 10.1097/01.CCM.0000147016.53607.C4. [DOI] [PubMed] [Google Scholar]
- 124.Barochia AV, Cui X, Vitberg D, Suffredini AF, O’Grady NP, Banks SM, Minneci P, Kern SJ, Danner RL, Natanson C, et al. Bundled care for septic shock: an analysis of clinical trials. Crit Care Med. 2010;38:668–78. doi: 10.1097/CCM.0b013e3181cb0ddf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G, SCCM/ESICM/ACCP/ATS/SIS 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003;31:1250–6. doi: 10.1097/01.CCM.0000050454.01978.3B. [DOI] [PubMed] [Google Scholar]
- 126.Schorr C. Value of protocolization and sepsis performance improvement programs in early identification of sepsis handbook: early diagnosis of sepsis. In: Dellinger P, Carlet J, editors. Sepsis Handbook: Early Diagnosis of Sepsis. France: Biomerieux Education; 2007. p. 130-9. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.