Abstract
Background
The technique and results of shoulder arthroplasty are influenced by glenohumeral pathoanatomy. Although some authors advocate a routine preoperative CT scan to define this anatomy, ordering a CT scan substantially increases the cost and the radiation exposure for the patient.
Questions/purposes
We asked whether measurements of arthritic shoulders on a standardized axillary view are reliable; if postoperative radiographs can reliably show the changes in glenoid anatomy and glenohumeral relationships after shoulder arthroplasty, and if the axillary view can show differences in glenohumeral pathoanatomy in the different sexes and disease types.
Methods
These questions were addressed using cross-sectional studies of 344 shoulders with different types of arthritis and of 128 osteoarthritic shoulders having a ream and run arthroplasty (a glenohumeral arthroplasty that combines a noncemented humeral hemiarthroplasty with concentric reaming of the glenoid bone without implantation of a prosthetic glenoid component). Measurements of glenoid type, glenoid version, and glenohumeral contact were made on standardized axillary radiographs. Interobserver reliability was calculated, preoperative and postoperative measurements were compared, and morphologic differences were compared as stratified by sex and disease type.
Results
The measurements on axillary views showed a high degree of interobserver reliability and sensitivity to the changes effected by arthroplasty. The ream and run substantially corrected the glenoid type and point of glenohumeral contact. Male shoulders and shoulders with osteoarthritis had more type B glenoids (ie, those with posterior erosion and biconcavity of the glenoid), more retroversion, and a greater degree of posterior displacement of the point of glenohumeral contact.
Conclusions
The axillary view provides a practical method of characterizing glenohumeral anatomy before and after surgery that is less costly and exposes the patient to less radiation than a CT scan.
Level of Evidence
Level IV, diagnostic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Glenohumeral arthritis is a commonly encountered condition of the shoulder; its treatment by shoulder arthroplasty is increasing annually [28]. Although many consider total shoulder arthroplasty with a glenoid prosthesis to be the gold standard treatment for glenohumeral arthritis, glenoid component failure remains a major complication, occurring in as much as 1/3 of cases at 10 years [4, 5, 8, 11, 14, 26, 31, 39, 49, 50, 54–56]. The preoperative assessment of glenohumeral anatomy is important; the risk of glenoid component failure is greater for shoulders in which preoperative assessment indicates that the glenoid surface is retroverted, the glenoid surface is biconcave, and/or the humeral head is posteriorly subluxated on the glenoid, features that are seen in almost ½ of arthritic shoulders requiring arthroplasty [5, 8, 12, 13, 16, 17, 21, 23, 24, 30, 35, 41, 45, 51–55].
Although some authors have reported the use of standardized plain radiographs to evaluate glenohumeral relationships before and after surgery [30, 31, 33, 39, 58], many have advocated the use of CT for assessment of preoperative and postoperative glenohumeral pathoanatomy [6, 7, 16, 17, 24, 32, 35–37, 41–44, 48, 52, 53]. CT scans add more than USD $1000 in cost [34] and expose the patient to 2.06 mSv, approximately 26 times the radiation of conventional radiographs [3], each time the shoulder is imaged before and after surgery. The clinical value to the patient of the increased radiation and increased cost of a routine CT scan has yet to be seen; specifically, it remains to be shown whether patients having preoperative CT scans have better clinical results than those whose preoperative imaging is limited to plain films.
The purpose of this investigation is to show the utility of a standardized plain axillary radiograph in determining glenoid shape, glenoid version, and position of glenohumeral contact before and after reconstructive arthroplasty. Specifically, the study addresses three questions: (1) what is the interobserver reliability of these measurements on standardized axillary views; (2) can postoperative axillary radiographs reproducibly show the change in glenoid anatomy and glenohumeral relationships after shoulder arthroplasty; and (3) can the standardized axillary view document the differences in glenoid type, glenoid version, and point of glenohumeral contact for shoulders of patients of different sexes and with different types of arthritis?
Patients and Methods
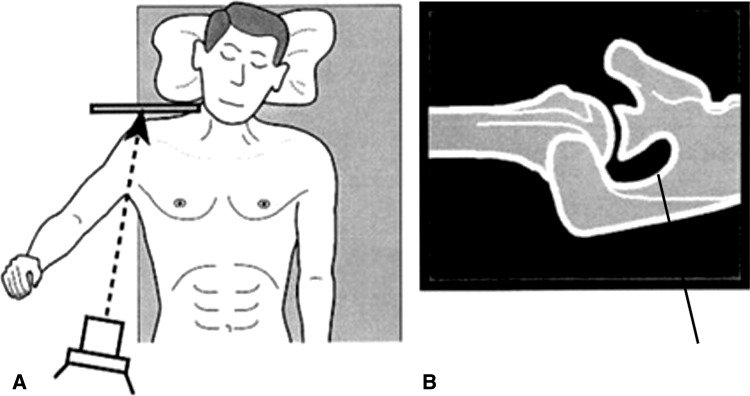
Standardized axillary radiographs were obtained by radiology technologists experienced in the desired method. The patients lay supine with the arm in neutral rotation and elevated 60° in the plane of the scapula. The radiographic beam was directed parallel to the plane of the scapula from the axilla toward the glenohumeral joint while the cassette was held on the superior aspect of the shoulder (Fig. 1) [36, 57, 58]. Axillary radiographs were deemed adequate if the spinoglenoid notch was clearly visible [57, 58]. The processing time to determine the glenoid type, version, and contact position was less than 2 minutes from the time the radiograph became available; no reformatting, reconstruction, or special software was necessary.
Fig. 1A–B.
(A) The standardized axillary view is obtained with the arm elevated 60° in the plane of the scapula. The beam is aimed at the axilla parallel to the blade of the scapula toward the cassette held over the superior aspect of the shoulder. (B) The standardized axillary view shows the spinoglenoid notch (arrow). (Both illustrations published with permission of Elsevier from Matsen FA 3rd, Lippitt SB, Sidles JA, Harryman DT 2nd. Practical Evaluation and Management of the Shoulder. Philadelphia, PA: WB Saunders; 1994:44.)
The glenohumeral anatomy was classified according to the commonly used Walch classification system [52, 53]. In this classification, Type A1 is a glenoid without erosion and with the humeral head centered; Type A2 is a glenoid with medial erosion and a centered head (Fig. 2A); Type B1 is a posteriorly eroded glenoid with posterior displacement of the head on the glenoid; and Type B2 is a posteriorly eroded glenoid with a biconcavity and posterior displacement of the head on the glenoid (Fig. 2B). The glenoid angle is the angle between a line drawn from the anterior lip to the posterior lip of the glenoid and a line drawn along the plane of the body of the scapula (Fig. 3A). Glenoid retroversion is 90° minus the glenoid angle [36]. The AP position of the head in relation to the glenoid was characterized as the ratio of the distance from the anterior glenoid lip to the center of glenohumeral contact divided by the AP dimension of the glenoid (Fig. 3B). This metric was selected rather than measuring the relationship of the center of the head to a line perpendicular to the glenoid face [17, 52, 53], because it is easy to standardize and because it reflects the degree of eccentricity of glenoid loading, a factor that can contribute to “rocking horse” loosening of the glenoid component [9, 15, 17, 19, 26, 31, 46, 47, 51, 53].
Fig. 2A–B.
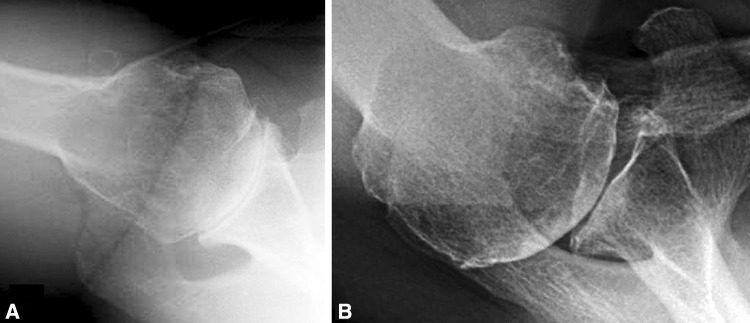
Standardized axillary radiographs of (A) Type A2 and (B) Type B2 glenoids typical of those used in this investigation are shown.
Fig. 3A–B.
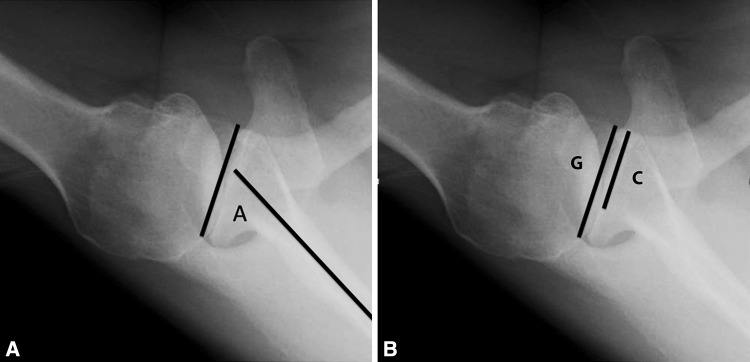
(A) The glenoid angle (A) is measured as the angle between a line drawn along the scapular body (longer line) and a line connecting the anterior and posterior rims of the glenoid (shorter line). The retroversion is the difference between 90° and this angle. (B) The contact position is the ratio of the length of a line segment drawn from the anterior rim of the glenoid to the center of glenohumeral contact, C, to the length of the line segment connecting the anterior and posterior rims of the glenoid, G.
Question 1. What is the interobserver reliability of these measurements on standardized axillary views?
We conducted a retrospective cross-sectional study of 128 patients (135 shoulders) who had a ream and run procedure (a glenohumeral arthroplasty that combines a noncemented humeral hemiarthroplasty with concentric reaming of the glenoid bone without implantation of a prosthetic glenoid component) by the senior author (FAM) between December 2009 and January 2013. All shoulders having a ream and run during this time initially were included, but eight subsequently were excluded. Seven patients had bilateral ream and run procedures during this period but only the first was included in the study reducing the number of shoulders to 128. Standardized axillary views were obtained within 1 month before surgery. The radiographs for one patient were of unacceptable quality, leaving 127 shoulders for the study. Glenoid type, glenoid version, and position of glenohumeral contact were determined independently on each axillary view by Observer 1 (AG, an orthopaedic resident without special training in shoulder surgery) and by Observer 2 (FAM, an attending surgeon experienced in shoulder reconstruction). The results of the two observers were compared using correlation coefficients for continuous variables (glenoid angle and the position of the contact point) and with kappa statistics for categorical variables (glenoid type).
Question 2. Can postoperative axillary radiographs consistently show the change in glenoid anatomy and glenohumeral relationships after shoulder arthroplasty?
Using the same shoulders as for Question 1, the preoperative and postoperative glenoid angles and the preoperative and postoperative contact positions were compared using a paired t-test. The relative preoperative and postoperative prevalences of the different glenoid types were compared using Fisher’s exact test. The results of the two observers were compared using correlation coefficients for continuous variables (glenoid angle and position of the contact point) and with kappa statistics for categorical variables (glenoid type).
Question 3. Can the standardized axillary view document differences in glenoid type, glenoid version, and point of glenohumeral contact point for shoulders of patients of different sexes and with different types of arthritis?
Between March 2010 and October 2012 standardized axillary radiographs were obtained on 344 shoulders within 1 month before a shoulder arthroplasty of any type (total shoulder, ream and run, cuff tear arthropathy prosthesis, or reverse total shoulder). One observer (FAM) blinded to patient sex and clinical diagnosis determined glenoid type, glenoid version, and point of glenohumeral contact. After the measurements were recorded, the results were analyzed by sex, diagnosis, and glenoid type. To determine the relation of gender to glenoid angle and humeral contact position on the glenoid, we used the unpaired t-test. To determine if the pathoanatomy of less common diagnoses (avascular necrosis, cuff tear arthropathy, and other) was different from that of the most common diagnosis, osteoarthritis, we compared the glenoid angles and humeral contact positions for each of the other diagnoses with those of osteoarthritis using the unpaired t-test. To determine the proportions of Type A and Type B glenoids by gender, we used Fisher’s exact test. To compare the proportions of Type A and Type B glenoids for the common diagnosis of osteoarthritis with those for less common diagnoses (avascular necrosis, cuff tear arthropathy, and other), we used the Fisher’s exact test. To determine the relationship between glenoid type, glenoid version, and point of humeral contact on the glenoid in shoulders with osteoarthritis, the glenoid angle and point of contact were compared between Type A and Type B glenoids using the unpaired t test. Correlation coefficients were used to examine the relationships between glenoid version and contact center position. These results were compared with those previously published for similar patients using different imaging methods.
Results
Interobserver Reproducibility of Measurements Made on Preoperative Axillary Radiographs
The agreement between the two independent observers was high for all three preoperative measurements. The correlation coefficient for the two observers was r = 0.81 for glenoid angle and 0.92 for the position of glenohumeral contact. The weighed kappa statistic for glenoid type was 0.859 (Table 1).
Table 1.
Preoperative and postoperative measurements of glenoid angle, contact point, and glenoid type for each observer*
| Attribute | Observer 1 Preoperative | Observer 2 Preoperative | Observer 1 Postoperative | Observer 2 Postoperative | Preoperative/postoperative p value |
|---|---|---|---|---|---|
| Glenoid angle | 73 ± 10 | 71 ± 10 (r = 0.81) |
74 ± 10 | 73 ± 9 (r = 0.77) |
Not significant for Observer 1, p = 0.016 for Observer 2† |
| Contact point | 64% ± 12% | 65% ± 13% (r = 0.92) |
54% ± 7% | 54% ± 7% (r = 0.69) |
< 0.001† |
| Type A1 | 11 | 10 | 119 | 116 | |
| Type A2 | 22 | 29 | 1 | 1 | |
| Type B1 | 31 | 27 | 5 | 7 | |
| Type B2 | 63 | 61 | 2 | 3 | |
| Weighted kappa 0.859 | Weighted kappa 0.832 | < 0.001‡ |
* Agreement between observers is characterized by correlation coefficients (r) and weighted kappa statistics. The significance of the change with surgery is shown in the far right column; †paired t-test; ‡Fisher’s exact test for Type A versus Type B.
Postoperative Changes to Anatomy and Glenohumeral Relationships on Axillary Radiographs
The agreement between the two independent observers was good for all three postoperative measurements. The correlation coefficient for the two observers was r = 0.77 for glenoid angle and 0.69 for the position of glenohumeral contact. The weighed kappa statistic for glenoid type was 0.832 (Table 1; Fig. 4). The ream and run procedure significantly improved the centering of the glenohumeral contact point from an average of 65% ± 13% posterior to 54% ± 7% posterior (50% represents the centered position) (p < 0.001). On the preoperative radiographs, there was a wide range of contact positions, ranging from 25% to 94% of the distance from the anterior to the posterior lip of the glenoid. Postoperatively this range was narrower, from 40% to 80%. The ream and run procedure resulted in a significant change in the glenohumeral type: Observer 1 found the percentage of Type A glenoids increased from 26% before surgery to 94% after surgery (p < 0.001); Observer 2 found the change to be from 31% to 92% (p < 0.001) (Table 1). The change in glenoid angle was small (from 73° ± 10° to 74° ± 10°, p not significant for Observer 1 and from 71° ± 10° to 73° ± 9°, p = .016 for Observer 2) (Table 1).
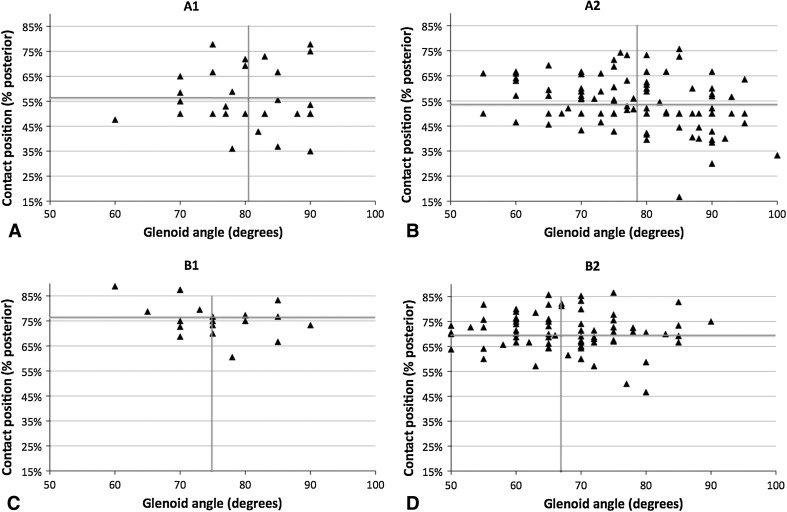
Fig. 4A–B.
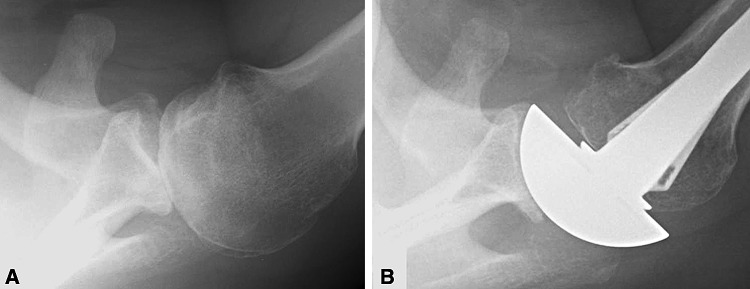
(A) This preoperative axillary view radiograph shows a B2 glenoid and posterior contact position. (B) The postoperative axillary view shows the corrected glenoid shape and contact position. An anteriorly eccentric humeral component was used.
Analyses of Glenohumeral Anatomy by Sex, Arthritis Type, and Glenoid Type on Axillary Radiographs
The axillary view effectively showed the differences in glenohumeral anatomy for the two sexes, different types of arthritis, and different glenoid types.
Type B glenoids, and glenoids having more retroversion and posterior displacement, were more closely associated with male patients and shoulders with osteoarthritis and certain other diagnoses (glenoid dysplasia, rheumatoid arthritis, postseptic arthritis, capsulorrhaphy arthropathy, chondrolysis, posttraumatic arthritis, and other causes of secondary arthritis of the glenohumeral joint), but not with avascular necrosis and rotator cuff tear arthropathy (Tables 2 and 3; Fig. 5).
Table 2.
Relationship of sex, diagnosis, glenoid angle, and contact position (rows) to glenoid type (columns)
| Category | Glenoid type | A1 | A2 | B1 | B2 | C |
|---|---|---|---|---|---|---|
| All diagnoses* | ||||||
| Female | 127 | 34 (27%) | 68 (53%) | 5 (4%) | 20 (16%) | 0 (0%) |
| Male | 213 | 32 (15%) | 80 (38%) | 21 (10%) | 78 (37%) | 2 (1%) |
| By diagnosis | ||||||
| Osteoarthritis | 231 | 30 (13%) | 104 (45%) | 19 (8%) | 78 (34%) | 0 |
| Avascular necrosis† | 18 | 13 (72%) | 4 (22%) | 1 (6%) | 0 (0%) | 0 |
| Cuff tear arthropathy‡ | 40 | 14 (35%) | 22 (55%) | 0 (0%) | 3 (8%) | 0 |
| Other§ | 51 | 9 (18%) | 18 (35%) | 6 (12%) | 16 (31%) | 2 (4%) |
| Osteoarthritis|| | ||||||
| Female | 70 | 12 (17%) | 40 (57%) | 3 (4%) | 15 (21%) | 0 (0%) |
| Male | 161 | 18 (11%) | 64 (40%) | 16 (10%) | 63 (39%) | 0 (0%) |
| Osteoarthritis only | ||||||
| Glenoid angle (degrees)¶ | 80.6 ± 7.8 | 78.3 ± 10.0 | 75.32 ± 7.6 | 67.7 ± 9.0 | ||
| Contact position (percent posterior)¶ | 56 ± 12 | 54 ± 10 | 76 ± 7 | 71 ± 8 | ||
* Fisher’s exact p < 0.001 for rate of Types A and B by sex; †Fisher’s exact p = 0.0018 for rate of Types A and B in comparison to osteoarthritis; ‡Fisher’s exact p < 0.001 for rate of Types A and B in comparison to osteoarthritis; §Fisher’s exact not signficant for rate of Types A and B in comparison to osteoarthritis; ||Fisher’s exact p = 0.0013 for rate of Types A and B by sex; ¶t-test comparing values for Types A and B < 0.001.
Table 3.
Relationship of sex and diagnosis (rows) to glenoid angle and contact position (columns)
| Category | Number | Glenoid angle (degrees) | Contact position (percent posterior) |
|---|---|---|---|
| All diagnoses | |||
| Female | 127 | 82.6 ± 9.4* | 57 ± 13* |
| Male | 213 | 72.3 ± 10.8 | 63 ± 13 |
| By diagnosis | |||
| Osteoarthritis | 231 | 75 ± 11 | 62 ± 13 |
| Avascular necrosis | 18 | 83 ± 8§ | 56 ± 10† |
| Cuff tear arthropathy | 40 | 81 ± 12‡ | 55 ± 13‡ |
| Other | 51 | 76 ± 14 | 63 ± 16 |
* t-test p < 0.001 for sex; †t-test in comparison to osteoarthritis p = .05; ‡t-test in comparison to osteoarthritis p = .0019; §t-test in comparison to osteoarthritis p = .0028.
Fig. 5A–D.
The relationships between the glenoid angle (horizontal axis) and contact position (vertical axis) for patients with osteoarthritis and (A) Type A1, (B) A2, (C) B1, or (D) B2 glenoid type are shown. The vertical and horizontal lines indicate the mean values for each group. Glenoid angles less than 90° indicate retroversion and contact positions greater than 50% indicate that the center of glenohumeral contact is posterior to the midglenoid. The spread of the data and lack of correlation between the glenoid angle and posterior displacement of the humeral head on the glenoid can be seen.
The correlation between glenoid version and AP contact center position was weak (R2 was 0.10 for all patients and 0.19 for patients with osteoarthritis) (Fig. 5).
Discussion
The conduct and results of shoulder arthroplasty are influenced by the preoperative glenohumeral pathoanatomy. Although many authors advocate regular use of a CT scan for assessment of the arthritic joint [6, 7, 16, 17, 24, 36, 37, 41, 43, 48, 52, 53], a CT scan is expensive, is associated with a greater radiation dose than plain films, and has not, to our knowledge, been associated with improved clinical results than those achieved with plain films.
These observations led us to attempt to answer three questions regarding use of the standardized axillary radiograph to the assessment of important pathoanatomic features of the arthritic glenohumeral joint: (1) What is the interobserver reliability of these measurements on standardized axillary views? (2) Can postoperative radiographs reproducibly show the change in glenoid anatomy and glenohumeral relationships after shoulder arthroplasty? (3) Can the standardized axillary view document the differences in glenoid type, glenoid version, and point of glenohumeral contact for shoulders of patients of different sexes and with different types of arthritis? We found that measurements based on the axillary view were reliable between observers, showed the change in glenohumeral anatomy after a shoulder arthroplasty, and documented the differences in pathoanatomy of arthritic shoulders for the different sexes and different types of arthritis.
The results of this study must be viewed in light of certain limitations. This was a radiographic study; clinical correlations were not part of this analysis. The axillary images were obtained by radiology technologists experienced in standardization of the view and patient position, conditions that may not exist elsewhere; however, the axillary radiographic view is part of the usual imaging repertoire—the only unique aspect of these images is that the technologists knew we wanted a view that showed the spinoglenoid notch (Fig. 1). The consistency of the results of the two independent observers may be attributable in large part to standardization of the axillary radiographs. Part of the standardization of the imaging technique is that the arm of the supine patient is held elevated in the plane of the scapula, a position of function not possible with CT imaging and a position not consistent in prior reports using the axillary view [22]. The high degree of interobserver consistency in our values for the point of glenohumeral contact may be related to the fact that the arm position was standardized and that this measurement is simpler than trying to relate an estimated humeral head center to scapular landmarks [27]. Although from a scientific standpoint it would have been preferable to obtain CT scans of these patients to enable direct comparison of the results, we could not clinically justify the incremental cost and radiation dosage for a test that would not have improved management of these patients. Furthermore, as is well documented in the literature, there is no gold standard measurement of glenohumeral pathoanatomy against which the accuracy of a method can be compared. As is the case for all imaging modalities, CT scan results are affected by the details of positioning, technique, and measurement technique [6, 7, 23, 32, 36, 42, 43]. The surgical procedures were performed by one high-volume shoulder arthroplasty surgeon (FAM) and, therefore, may not relate to other practice settings. Finally, the senior author (FAM) prefers the axillary view in assessing glenohumeral anatomy because it is less costly and exposes the patient to less radiation, and the ream and run procedure because it is a method of glenohumeral arthroplasty that does not carry the risks of glenoid component failure.
Our study showed (1) that reproducible measurements of preoperative glenoid version, glenoid type, and point of glenohumeral contact can be made from standardized axillary radiographs; (2) that the standardized postoperative axillary view shows the significant changes in glenoid type and centering of the point of glenohumeral contact after a ream and run procedure; and (3) the axillary view documents the differences in glenoid pathoanatomy of the different sexes and the different types of glenohumeral arthritis.
The results from our large cohort of 344 arthritic shoulders are highly congruent with published findings from CT studies on similar groups of patients with arthritis of the glenohumeral joint [2, 10, 16, 23, 25, 29, 38, 40, 42, 52]. For example, the distribution of Types A and B glenoids in the subset of 231 shoulders with osteoarthritis (58% and 42%, respectively) is similar to the pooled results of seven smaller series of patients with osteoarthritis having CT scans (52% A, 43% B, 5% C) [5, 8, 18, 42, 48, 52, 59]. As a second example, the average glenoid retroversion of 15° ± 11° (90° minus the glenoid angle) in our patients with osteoarthritis is well within the 8° to 27° averages in 10 smaller series that used CT scans [2, 10, 16, 23, 25, 29, 38, 40, 42, 52]. As a third example, we found an average posterior displacement of the glenoid humeral contact of 76% ± 7% in 19 B1 glenoids and 71% ± 8% in 78 B2 glenoids, while Gerber et al., in their study of shoulders with static posterior subluxation, presented a series of CT scans on nine B1 glenoids, five B2 glenoids, and nine C glenoids with an average posterior subluxation index of 71% [17]. Similar CT findings have been reported by others s [1, 20, 24, 51, 52]. Interestingly, the observations of these CT studies were consistent with our finding that glenoid version was correlated only weakly with posterior positioning of the humeral head on the glenoid [5, 17, 24, 51]. The concordance of the findings of prior CT studies with those of our investigation using the plain axillary view is particularly remarkable because somewhat different landmarks are referenced in the two methods [36].
This is, to our knowledge, the first study to document the interobserver reliability in the use of a standardized axillary view to document the glenoid shape, angle, and point of glenohumeral contact before and after shoulder arthroplasty. It is also the largest analysis of preoperative glenohumeral pathoanatomy by sex and diagnosis. We found that standardized axillary views enable the reproducible determination of glenoid version, type, and point of contact including the changes in glenohumeral centering and congruence after shoulder arthroplasty, even in shoulders having Type B glenoids and those with substantial posterior subluxation before surgery. Forty-seven thousand shoulder arthroplasties were performed in the United States in 2008; the rate of shoulder arthroplasty is increasing dramatically [28]. Routine use of CT scans before shoulder arthroplasty would add millions of dollars in healthcare expense. In our experience, the information from the preoperative axillary view is sufficient for planning a primary shoulder arthroplasty for arthritis without the increased cost and radiation of routine CT scans.
Acknowledgments
We thank Susan DeBartolo for her great assistance with preparation of this manuscript.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Badet R, Boileau P, Noel E, Walch G. Arthrography and computed arthrotomography study of seventy patients with primary glenohumeral osteoarthritis. Rev Rhum Engl Ed. 1995;62:555–562. [PubMed] [Google Scholar]
- 2.Badet R, Walch G, Boulahia A. Computed tomography in primary glenohumeral osteoarthritis without humeral head elevation. Rev Rhum Engl Ed. 1998;65:187–194. [PubMed] [Google Scholar]
- 3.Biswas D, Bible JE, Bohan M, Simpson AK, Whang PG, Grauer JN. Radiation exposure from musculoskeletal computerized tomographic scans. J Bone Joint Surg Am. 2009;91:1882–1889. doi: 10.2106/JBJS.H.01199. [DOI] [PubMed] [Google Scholar]
- 4.Bohsali KI, Wirth MA, Rockwood CA., Jr Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. doi: 10.2106/JBJS.F.00125. [DOI] [PubMed] [Google Scholar]
- 5.Boileau P, Avidor C, Krishnan SG, Walch G, Kempf JF, Mole D. Cemented polyethylene versus uncemented metal-backed glenoid components in total shoulder arthroplasty: a prospective, double-blind, randomized study. J Shoulder Elbow Surg. 2002;11:351–359. doi: 10.1067/mse.2002.125807. [DOI] [PubMed] [Google Scholar]
- 6.Bokor DJ, O’Sullivan MD, Hazan GJ. Variability of measurement of glenoid version on computed tomography scan. J Shoulder Elbow Surg. 1999;8:595–598. doi: 10.1016/S1058-2746(99)90096-4. [DOI] [PubMed] [Google Scholar]
- 7.Budge MD, Lewis GS, Schaefer E, Coquia S, Flemming DJ, Armstrong AD. Comparison of standard two-dimensional and three-dimensional corrected glenoid version measurements. J Shoulder Elbow Surg. 2011;20:577–583. doi: 10.1016/j.jse.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 8.Collin P, Tay AK, Melis B, Boileau P, Walch G. A ten-year radiologic comparison of two-all polyethylene glenoid component designs: a prospective trial. J Shoulder Elbow Surg. 2011;20:1217–1223. doi: 10.1016/j.jse.2011.06.012. [DOI] [PubMed] [Google Scholar]
- 9.Collins D, Tencer A, Sidles J, Matsen F., 3rd Edge displacement and deformation of glenoid components in response to eccentric loading: the effect of preparation of the glenoid bone. J Bone Joint Surg Am. 1992;74:501–507. [PubMed] [Google Scholar]
- 10.Couteau B, Mansat P, Darmana R, Mansat M, Egan J. Morphological and mechanical analysis of the glenoid by 3D geometric reconstruction using computed tomography. Clin Biomech (Bristol, Avon). 2000;15(s uppl 1):S8–12. [DOI] [PubMed]
- 11.Denard PJ, Raiss P, Sowa B, Walch G. Mid- to long-term follow-up of total shoulder arthroplasty using a keeled glenoid in young adults with primary glenohumeral arthritis. J Shoulder Elbow Surg. 2013;22:894–900. doi: 10.1016/j.jse.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 12.Edwards TB, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. Shoulder arthroplasty in patients with osteoarthritis and dysplastic glenoid morphology. J Shoulder Elbow Surg. 2004;13:1–4. doi: 10.1016/j.jse.2003.09.011. [DOI] [PubMed] [Google Scholar]
- 13.Farron A, Terrier A, Buchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg. 2006;15:521–526. doi: 10.1016/j.jse.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 14.Fox TJ, Cil A, Sperling JW, Sanchez-Sotelo J, Schleck CD, Cofield RH. Survival of the glenoid component in shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:859–863. doi: 10.1016/j.jse.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 15.Franklin JL, Barrett WP, Jackins SE, Matsen FA., 3rd Glenoid loosening in total shoulder arthroplasty: association with rotator cuff deficiency. J Arthroplasty. 1988;3:39–46. doi: 10.1016/S0883-5403(88)80051-2. [DOI] [PubMed] [Google Scholar]
- 16.Friedman RJ, Hawthorne KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992;74:1032–1037. [PubMed] [Google Scholar]
- 17.Gerber C, Costouros JG, Sukthankar A, Fucentese SF. Static posterior humeral head subluxation and total shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18:505–510. doi: 10.1016/j.jse.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 18.Godeneche A, Boileau P, Favard L, Le Huec JC, Levigne C, Nove-Josserand L, Walch G, Edwards TB. Prosthetic replacement in the treatment of osteoarthritis of the shoulder: early results of 268 cases. J Shoulder Elbow Surg. 2002;11:11–18. doi: 10.1067/mse.2002.120140. [DOI] [PubMed] [Google Scholar]
- 19.Gunther SB, Lynch TL, O’Farrell D, Calyore C, Rodenhouse A. Finite element analysis and physiologic testing of a novel, inset glenoid fixation technique. J Shoulder Elbow Surg. 2012;21:795–803. doi: 10.1016/j.jse.2011.08.073. [DOI] [PubMed] [Google Scholar]
- 20.Habermeyer P, Magosch P, Lichtenberg S. Recentering the humeral head for glenoid deficiency in total shoulder arthroplasty. Clin Orthop Relat Res. 2007;457:124–132. doi: 10.1097/BLO.0b013e31802ff03c. [DOI] [PubMed] [Google Scholar]
- 21.Habermeyer P, Magosch P, Luz V, Lichtenberg S. Three-dimensional glenoid deformity in patients with osteoarthritis: a radiographic analysis. J Bone Joint Surg Am. 2006;88:1301–1307. doi: 10.2106/JBJS.E.00622. [DOI] [PubMed] [Google Scholar]
- 22.Ho JC, Youderian A, Davidson IU, Bryan J, Iannotti JP. Accuracy and reliability of postoperative radiographic measurements of glenoid anatomy and relationships in patients with total shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22:1068–1077. doi: 10.1016/j.jse.2012.11.015. [DOI] [PubMed] [Google Scholar]
- 23.Hoenecke HR, Jr, Hermida JC, Flores-Hernandez C, D’Lima DD. Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg. 2010;19:166–171. doi: 10.1016/j.jse.2009.08.009. [DOI] [PubMed] [Google Scholar]
- 24.Hoenecke HR, Jr, Tibor LM, D’Lima DD. Glenoid morphology rather than version predicts humeral subluxation: a different perspective on the glenoid in total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:1136–1141. doi: 10.1016/j.jse.2011.08.044. [DOI] [PubMed] [Google Scholar]
- 25.Iannotti JP, Greeson C, Downing D, Sabesan V, Bryan JA. Effect of glenoid deformity on glenoid component placement in primary shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21:48–55. doi: 10.1016/j.jse.2011.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Kasten P, Pape G, Raiss P, Bruckner T, Rickert M, Zeifang F, Loew M. Mid-term survivorship analysis of a shoulder replacement with a keeled glenoid and a modern cementing technique. J Bone Joint Surg Br. 2010;92:387–392. doi: 10.1302/0301-620X.92B3.23073. [DOI] [PubMed] [Google Scholar]
- 27.Kidder JF, Rouleau DM, Pons-Villanueva J, Dynamidis S, DeFranco MJ, Walch G. Humeral head posterior subluxation on CT scan: Validation and comparison of 2 methods of measurement. Tech Shoulder Elbow Surg. 2010;11:72–76. doi: 10.1097/BTE.0b013e3181e5d742. [DOI] [Google Scholar]
- 28.Kim SH, Wise BL, Zhang Y, Szabo RM. Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg. Am. 2011;93:2249–2254. doi: 10.2106/JBJS.J.01994. [DOI] [PubMed] [Google Scholar]
- 29.Kircher J, Wiedemann M, Magosch P, Lichtenberg S, Habermeyer P. Improved accuracy of glenoid positioning in total shoulder arthroplasty with intraoperative navigation: a prospective-randomized clinical study. J Shoulder Elbow Surg. 2009;18:515–520. doi: 10.1016/j.jse.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 30.Lazarus MD, Jensen KL, Southworth C, Matsen FA., 3rd The radiographic evaluation of keeled and pegged glenoid component insertion. J Bone Joint Surg Am. 2002;84:1174–1182. doi: 10.2106/00004623-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Matsen FA, 3rd, Clinton J, Lynch J, Bertelsen A, Richardson ML. Glenoid component failure in total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90:885–896. doi: 10.2106/JBJS.G.01263. [DOI] [PubMed] [Google Scholar]
- 32.Moineau G, Levigne C, Boileau P, Young A, Walch G, French Society for Shoulder & Elbow (SOFEC) Three-dimensional measurement method of arthritic glenoid cavity morphology: feasibility and reproducibility. Orthop Traumatol Surg Res. 2012;98(6 suppl):S139–S145. doi: 10.1016/j.otsr.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 33.Namdari S, Hsu JE, Barron M, Huffman GR, Glaser D. Immediate postoperative radiographs after shoulder arthroplasty are often poor quality and do not alter care. Clin Orthop Relat Res. 2013;471:1257–1262. doi: 10.1007/s11999-012-2551-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.New Choice Health Inc. Shoulder CT scan cost and procedure information. Available at: http://www.newchoicehealth.com/Directory/Procedure/12/ShoulderCTScan. Accessed January 17, 2013.
- 35.Nowak DD, Bahu MJ, Gardner TR, Dyrszka MD, Levine WN, Bigliani LU, Ahmad CS. Simulation of surgical glenoid resurfacing using three-dimensional computed tomography of the arthritic glenohumeral joint: the amount of glenoid retroversion that can be corrected. J Shoulder Elbow Surg. 2009;18:680–688. doi: 10.1016/j.jse.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 36.Nyffeler RW, Jost B, Pfirrmann CW, Gerber C. Measurement of glenoid version: conventional radiographs versus computed tomography scans. J Shoulder Elbow Surg. 2003;12:493–496. doi: 10.1016/S1058-2746(03)00181-2. [DOI] [PubMed] [Google Scholar]
- 37.Nyffeler RW, Sheikh R, Atkinson TS, Jacob HA, Favre P, Gerber C. Effects of glenoid component version on humeral head displacement and joint reaction forces: an experimental study. J Shoulder Elbow Surg. 2006;15:625–629. doi: 10.1016/j.jse.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 38.Poon PC, Ting FS. A 2-dimensional glenoid vault method for measuring glenoid version on computed tomography. J Shoulder Elbow Surg. 2012;21:329–335. doi: 10.1016/j.jse.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 39.Raiss P, Schmitt M, Bruckner T, Kasten P, Pape G, Loew M, Zeifang F. Results of cemented total shoulder replacement with a minimum follow-up of ten years. J Bone Joint Surg Am. 2012;94:e171 1–e171 10. doi: 10.2106/JBJS.K.00580. [DOI] [PubMed] [Google Scholar]
- 40.Rouleau DM, Kidder JF, Pons-Villanueva J, Dynamidis S, Defranco M, Walch G. Glenoid version: how to measure it? Validity of different methods in two-dimensional computed tomography scans. J Shoulder Elbow Surg. 2010;19:1230–1237. doi: 10.1016/j.jse.2010.01.027. [DOI] [PubMed] [Google Scholar]
- 41.Scalise JJ, Bryan J, Polster J, Brems JJ, Iannotti JP. Quantitative analysis of glenoid bone loss in osteoarthritis using three-dimensional computed tomography scans. J Shoulder Elbow Surg. 2008;17:328–335. doi: 10.1016/j.jse.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 42.Scalise JJ, Codsi MJ, Brems JJ, Iannotti JP. Inter-rater reliability of an arthritic glenoid morphology classification system. J Shoulder Elbow Surg. 2008;17:575–577. doi: 10.1016/j.jse.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 43.Scalise JJ, Codsi MJ, Bryan J, Brems JJ, Iannotti JP. The influence of three-dimensional computed tomography images of the shoulder in preoperative planning for total shoulder arthroplasty. J Bone Joint Surg Am. 2008;90:2438–2445. doi: 10.2106/JBJS.G.01341. [DOI] [PubMed] [Google Scholar]
- 44.Scalise JJ, Codsi MJ, Bryan J, Iannotti JP. The three-dimensional glenoid vault model can estimate normal glenoid version in osteoarthritis. J Shoulder Elbow Surg. 2008;17:487–491. doi: 10.1016/j.jse.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 45.Sears BW, Johnston PS, Ramsey ML, Williams GR. Glenoid bone loss in primary total shoulder arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2012;20:604–613. doi: 10.5435/JAAOS-20-09-604. [DOI] [PubMed] [Google Scholar]
- 46.Shapiro TA, McGarry MH, Gupta R, Lee YS, Lee TQ. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16(3 suppl):S90–S95. doi: 10.1016/j.jse.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 47.Suarez DR, Nerkens W, Valstar ER, Rozing PM, van Keulen F. Interface micromotions increase with less-conforming cementless glenoid components. J Shoulder Elbow Surg. 2012;21:474–482. doi: 10.1016/j.jse.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 48.Szabo I, Buscayret F, Edwards TB, Nemoz C, Boileau P, Walch G. Radiographic comparison of flat-back and convex-back glenoid components in total shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14:636–642. doi: 10.1016/j.jse.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 49.Tammachote N, Sperling JW, Vathana T, Cofield RH, Harmsen WS, Schleck CD. Long-term results of cemented metal-backed glenoid components for osteoarthritis of the shoulder. J Bone Joint Surg Am. 2009;91:160–166. doi: 10.2106/JBJS.F.01613. [DOI] [PubMed] [Google Scholar]
- 50.Taunton MJ, McIntosh AL, Sperling JW, Cofield RH. Total shoulder arthroplasty with a metal-backed, bone-ingrowth glenoid component: medium to long-term results. J Bone Joint Surg Am. 2008;90:2180–2188. doi: 10.2106/JBJS.G.00966. [DOI] [PubMed] [Google Scholar]
- 51.Walch G, Ascani C, Boulahia A, Nove-Josserand L, Edwards TB. Static posterior subluxation of the humeral head: an unrecognized entity responsible for glenohumeral osteoarthritis in the young adult. J Shoulder Elbow Surg. 2002;11:309–314. doi: 10.1067/mse.2002.124547. [DOI] [PubMed] [Google Scholar]
- 52.Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999;14:756–760. doi: 10.1016/S0883-5403(99)90232-2. [DOI] [PubMed] [Google Scholar]
- 53.Walch G, Boulahia A, Boileau P, Kempf JF. Primary glenohumeral osteoarthritis: clinical and radiographic classification. The Aequalis Group. Acta Orthop Belg. 1998;64(suppl 2):46–52. [PubMed] [Google Scholar]
- 54.Walch G, Moraga C, Young A, Castellanos-Rosas J. Results of anatomic nonconstrained prosthesis in primary osteoarthritis with biconcave glenoid. J Shoulder Elbow Surg. 2012;21:1526–1533. doi: 10.1016/j.jse.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 55.Walch G, Young AA, Boileau P, Loew M, Gazielly D, Mole D. Patterns of loosening of polyethylene keeled glenoid components after shoulder arthroplasty for primary osteoarthritis: results of a multicenter study with more than five years of follow-up. J Bone Joint Surg Am. 2012;94:145–150. doi: 10.2106/JBJS.J.00699. [DOI] [PubMed] [Google Scholar]
- 56.Walch G, Young AA, Melis B, Gazielly D, Loew M, Boileau P. Results of a convex-back cemented keeled glenoid component in primary osteoarthritis: multicenter study with a follow-up greater than 5 years. J Shoulder Elbow Surg. 2011;20:385–394. doi: 10.1016/j.jse.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 57.Wirth MA, Loredo R, Garcia G, Rockwood CA, Jr, Southworth C, Iannotti JP. Total shoulder arthroplasty with an all-polyethylene pegged bone-ingrowth glenoid component: a clinical and radiographic outcome study. J Bone Joint Surg Am. 2012;94:260–267. doi: 10.2106/JBJS.J.01400. [DOI] [PubMed] [Google Scholar]
- 58.Yian EH, Werner CM, Nyffeler RW, Pfirrmann CW, Ramappa A, Sukthankar A, Gerber C. Radiographic and computed tomography analysis of cemented pegged polyethylene glenoid components in total shoulder replacement. J Bone Joint Surg Am. 2005;87:1928–1936. doi: 10.2106/JBJS.D.02675. [DOI] [PubMed] [Google Scholar]
- 59.Young A, Walch G, Boileau P, Favard L, Gohlke F, Loew M, Mole D. A multicentre study of the long-term results of using a flat-back polyethylene glenoid component in shoulder replacement for primary osteoarthritis. J Bone Joint Surg Br. 2011;93:210–216. doi: 10.1302/0301-620X.93B2.25086. [DOI] [PubMed] [Google Scholar]