Abstract
Background and Objective: The objective of this study was to compare the efficacy and safety of Endovenous Laser Photocoagulation (EVLP) at wavelengths of 1064 nm versus 810 nm for chronic venous insufficiency (varicose veins) in a large series of patients.
Study Design/Materials and Methods: A retrospective review was conducted of 108 patients with chronic venous insufficiency treated over a 8-year period. Subjects' ages ranged between 16 to 79 years; there were 83 females and 25 males, all of whom were Asian. Patients (n=54) received EVLP at wavelengths of 1064 nm (EVLP-1064 nm), Nd:YAG laser. Subsequent patients (n=54) received 810 nm (EVLP-810 nm), Diode laser. The primary efficacy measurement was the quantitative assessment of final outcome for 1064 nm versus 810 nm. Patients were monitored for adverse effects as well.
Results: Complications were observed at 3 weeks (early), 6 weeks (late) and 6 months after EVLP. In both groups, the commonest complication in early convalescence was swelling. This was followed by Local paraesthesia, pigmentation, superficial burns, superficial phlebitis, and localized hematomas. At 6 weeks postoperatively, local paraesthesia, persistent hyperpigmentation, and minimal scarring were presented. These problems all disappeared completely after the 6 months study period. Based on chi-squared analysis, there were clinical, and statistically significant differences in the severity score of final results favoring the EVLP-810 nm group.
Conclusion: All patients achieved good or excellent improvement after EVLP-1064nm and EVLP-810nm. However, the difference of final outcome was significant, and indicates that improvement was greater in the Diode group. Further studies of different wavelengths and optimization of cryogen spray cooling (CSC) may lead to improved results in the eradication of varicose veins.
Introduction
Chronic venous insufficiency of the lower extremities is one of the common conditions affecting mankind 1). Visible tortuous varicose veins can be found in 20 – 25% of women and 10 – 15% of men above the age of 15 2). Minor degrees of varicosis (e.g., reticular veins) affect 50% of women and 45% of men 3). The risk factors include age, female gender, pregnancy, geographical sites, and race 2).
Primary varicose veins are caused mostly by the failure of a single valve in a critical location, while secondary varicose veins occur when thrombophlebitis causes deep system and perforator valve damage. Other secondary causes of varicose veins can be pregnancy, obesity, trauma, tumor compression and gravity. Patients with varicose veins display a variety of non-specific symptoms, that may include pain, swelling, soreness, burning, aching, itching, throbbing, cramping, muscle fatigue, and a restless leg. The squeal include chronic pain and edema, recurrent cellulites and dermatitis, pigmentation, lipodermatosclerosis, non-healing leg ulcers (ulcer crura), cutaneous infarction (atrophy blanche), hemorrhage from varices, superficial thrombophlebitis, deep vein thrombosis, pulmonary embolism, and even malignant transformation 4).
Treatment aims to eliminate symptoms, improve appearance, and to prevent further deterioration. Multiple options available include compression stockings, sclerotherapy, ambulatory phlebectomy, surgical stripping, surgical ligation, and radio-frequency ablation—either isolated or in combination. 5-11) Surgical treatment has evolved from large, open surgeries to minimally invasive approaches. Safe and effective use of lasers in angioplasty 12) and for the treatment of vascular lesions and emangiomas 13-16) has been variously reported. Endovascular laser photocoagulation (EVLP) is becoming the preferred treatment for varicose veins of the lower extremities due to the simplification of the procedure and good outcome. 17)
The purpose of this study was to compare the efficacy and safety of EVLP at wavelengths of 1064 nm (EVLP-1064 nm) versus 810 nm (EVLP-810 nm) for chronic venous insufficiency in a large series of patients. The primary efficacy measure was the quantitative assessment of the response scores based on Hach's classification system of EVLP-1064 nm as compared, on a blinded basis, to EVLP-810nm . Safety was also evaluated for each treatment group.
Materials and Methods
A retrospective review was conducted of 108 patients with 180 varicose veins treated with the EVLP over an 8-year period (January 2003–January 2011). Subject age ranged between 16 and 79 years (average age, 42 years 11 months). There were 83 females and 25 males, all of whom were Asian. During January 2003 to January 2007, 54 patients received EVLP at wavelengths of 1064 nm, a neodymium: yttrium-aluminum-garnet (Nd: YAG) laser system (Sharplan, Inc., NJ, USA). The Nd:YAG laser system was calibrated to deliver laser pulses with 10–15W of energy and pulse duration of 10 seconds upon each trigger by a foot pedal. The total energy delivery ranged from 9200-191257
J. For the subsequent period of January 2007 to January 2011, 54 patients received 810 nm Diode laser (Diomed, Inc., Andover, MA, USA). The Diode laser system was calibrated to deliver laser pulses with 7–10W of energy and pulse duration of 10 seconds upon each trigger by a foot pedal as well. The total energy delivery ranged from 7234- 16682.75J.
The primary efficacy measurement was the quantitative assessment based on Hach's Classification for 1064 nm versus 810 nm. Meanwhile, patients were monitored for adverse effects. Each patient was evaluated by chart review. Information regarding the following variables was extracted: age, gender, anatomic locations (bilateral or unilateral), severity of varicose veins, complications noted at time of consultation, type of laser treatment, outcome after laser therapy. All preand posttreatment photographs were taken under standardized conditions for film, light source, and exposure.
Clinical outcomes were assessed by three plastic surgeons knowledgeable of and experienced in laser treatment, but not involved previously in the study. On a blinded basis, each evaluator was given pre- and posttreatment photographs of eachpatient's lesion. The primary efficacy measure was the quantitative assessment of improvements the severity of varicose veins. Complications were observed at 3 weeks (early), at 6 weeks (late), and 6 months after their last treatment. Results for both groups were compared. Differences between the severity scores for both groups were determined, and a chi-squared analysis was performed.
Results
Information regarding the variables of age, gender, anatomic location, and comps at first consultation was obtained for statistical comparison. The mean ages for the EVLP-1064nm and EVLP-810nm groups were 58.43 years and 56.49 years respectively. The male-to-female ratios for the corresponding groups were 11:43 and 14:40 respectively. Meanwhile, the bilateral-to-unilateral ratios for the corresponding groups were 36:18 and 35:20 respectively. Preoperative findings of EVLP-1064nm group (Table 1) involved pain/tension in 50 patients (92.59%). Eczema was seen in 25 patients (46.30%), and 8 patients (14.81%) gave a family history. pigmentation occurred in 13 patient (24.07%) and was secondary to previous ulceration. Nine patients (16.67%) had ulceration. There were 3 patients had phlebitis (5.55%), and 2 patients (3.70%) had deep vein thrombosis (DVT). In EVLP-810 nm group, pain/tension in 46 patients (84.61%). Eczema was seen in 19 patients (35.89%), and 7 patients (12.82%) gave a family history. Pigmentation occurred in 7 patient (12.82%) and was secondary to previous ulceration. Six patients (16.25%) had ulceration. Visible varicose veins were found along the truncal GSV systems. Based on the Hach's score of severity, 10 legs (11.2%) were scored 4, 30 legs (33.3%) were scored 3, 47 legs (52.2%) were scored 2, and 4 legs (4.5%) were scored 1 in EVLP- 1064 nm group. 13 legs (14.9%) were scored 4, 34 legs (37.3%) were scored 3, 39 legs (43.3 %) were scored 2, and 3 legs (3.3%) were scored 1 in EVLP-810 nm group. The mean number of preoperatively severity scores for the corresponding groups were 2.52 and 2.62 respectively.
Table 1: Preoperative Findings.
| Number of Patient | Diode | Nd:YAG |
|---|---|---|
| n=54 | n=54 | |
| Pain/tension | 46 (84.61%) | 50 (92.59%) |
| Eczema | 19 (35.89%) | 25 (46.30%) |
| Pigmentation | 7 (12.82%) | 13 (24.07%) |
| Family history | 7 (12.82%) | 8 (14.81%) |
| Ulceration | 6 (10.25%) | 9 (16.67%) |
| Phlebitis | 0 (0%) | 3 (5.55%) |
| DVT | 0 (0%) | 2 (3.70%) |
The mean follow-up period was 39 months with a range of 12– 66 months. There were no phlebitis and deep vein thrombosis (DVT). The two treatment groups exhibited nonsignificant differences with regard to patient age (p = 0.3342), gender (p = 0.851), anatomic locations (p = 0.244), and preoperative findings (x2 = 5.807, p = 0.213). The operating time for EVLP-1064nm group was from 51 to 201 minutes (mean 121 minutes) and for EVLP-810nm group of 30–184 minutes (mean 81.07 minutes).
The final outcomes and comparison of the EVLP-1064nm and EVLP-810nm groups are summarized in Table 3 and Figures 1 and 2. Complications were observed at 3 weeks (early), 6 weeks (late) and 6 months after EVLP. As expected in EVLP-1064nm group, all patients developed post-operative swelling of the lower limbs. The commonest complication in early convalescence was local paraesthesia of treated areas in 39 legs (43.5%). This was followed by ecchymosis and dyschromia in 25 legs (27.7.%), superficial burns in 4 legs (4.8%), superficial phlebitis in one leg (1.1%), and localized hematomas in one leg (1.1%). Most of these complications resolved spontaneously or with conservative measures. At 6 weeks postoperatively, local paraesthesia was found in only 3 legs (3.3%). Only 1 leg (1.1%) presented persistent hyperpigmentation and 2 legs (2.6%) with burn injuries showed minimal scarring. These problems all disappeared completely after the 6 months study period. In EVLP-810nm group, all patients also developed post-operative swelling of the lower limbs. Local paraesthesia of treated areas in 30 legs (33.3%). This was followed by ecchymosis and dyschromia in 23 legs (25.3.%), superficial burns in 2 legs (2.6%), and no phlebitis one hematomas (1.1%) were found. At 6 weeks postoperatively, local paraesthesia was found in only 3 legs (3.3%). Only 7 legs (7.9 %) presented persistent hyperpigmentation and 1 leg (1.1%) with burn injuries showed minimal scarring. These problems all disappeared completely after the 6 months study period (Table 2). All patients achieved good or excellent improvement.
Table 3: Score of Severity Before and After Nd:YAG -(1064nm)V.S. Diode (810nm).
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Number of lower extremity | 1064 nm | 810 nm | 1064 nm | 810 nm | 1064 nm | 810 nm | 1064 nm | 810 nm | 1064 nm | 810 nm |
| n=90 | n=90 | n=90 | n=90 | n=90 | n=90 | n=90 | n=90 | n=90 | n=90 | |
| Pre-OP | 0 | 0 | 4 | 3 | 39 | 47 | 34 | 30 | 13 | 10 |
| Post-OP* | 87 | 90 | 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
P < 0.05
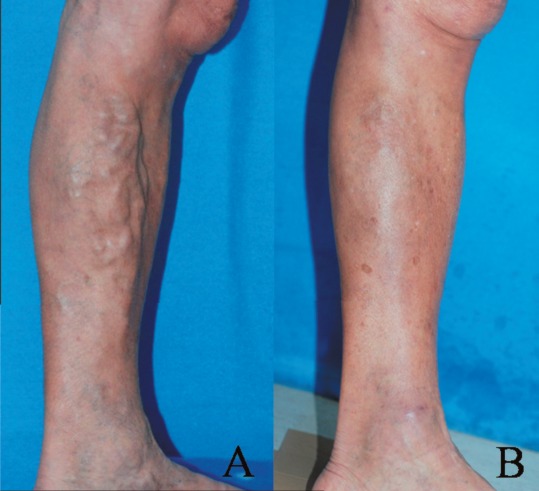
Figure 1:

A 71-years-old male with severe varicose veins (Grade 3) at bilateral medial thigh, and leg (Figure 1A) complete resolution of his symptoms 12 months after Diode laser (810nm) EVLP for one treatment (Figure 1B).
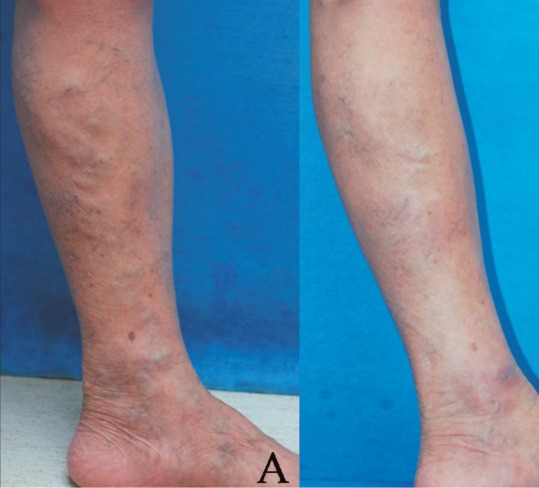
Figure 2:
A 72-years-old female with varicose veins (Grade 2) at left knee, and leg (Figure 2A) complete resolution of her symptoms 15 months after Diode laser (810nm) EVLP for one treatment (Figure 2B).
Table 2: Post-operative Complication in Patients Using Nd:YAG (1064nm) V.S. Diode Laser (810nm).
| Complication | Early (3 weeks)(%) | Late (6 weeks) | (%) Final (> 6 months) | |||
|---|---|---|---|---|---|---|
| Number of lower extremity | 1064 nm | 810 nm | 1064 nm | 810 nm | 1064 nm | 810 nm |
| N=90 | N=90 | N=90 | N=90 | N=90 | N=90 | |
| Swelling | 90 (100%) | 90 (100%) | 0 | 0 | 0 | 0 |
| Paraesthesia | 39 (43.5%) | 30 (33.3%) | 3 (3.3%) | 3 (3.3%) | 0 | 0 |
| Pigmentation | 25 (27.7%) | 23 (25.3%) | 1 (1.1%) | 7 (7.9%) | 0 | 0 |
| Superficial burn/scar | 4 (4.8%) | 2 (2.6%) | 2 (2.6%) | 1 (1.1%) | 0 | 0 |
| Superficial phlebitis | 1 (1.1%) | 2 (2.6%) | 0 | 0 | 0 | 0 |
| Hematoma | 1 (1.1%) | 1 (1.1%) | 0 | 0 | 0 | 0 |
| Recanalization | 0 | 0 | 0 | 0 | 0 | 0 |
Figure 3:
A 49-years-old female with varicose veins (Grade 2) at left knee, and leg (Figure 3A) complete resolution of her symptoms after Nd: YAG laser (1064nm) EVLP for one treatment (Figure 3B).
In the severity score of the final outcome, 3 legs (3.3%) were scored 1, 87 legs were scored 0 in EVLP-1064 nm group. 90 legs (100%) were scored 0 in EVLP-810 nm group. This difference was significant (x2 = 37.154, p = 0.001), and indicates that improvement was greater in the EVLP-810 nm group (Table 3).
Discussion
In 1999, the radiofrequency endovenous ablation system has been applied by its effect of thermal destruction of venous tissues using electrical energy passing through tissue in the form of a high-frequency alternating current by the VNUS® RF (radiofrequency) ablation system (AngioDynamics, NY, USA). This current was converted into heat, which causes irreversible localized tissue damage. Radiofrequency energy is delivered through a special catheter with deployable electrodes at the tip, the electrodes touch the vein walls and deliver energy directly into the tissues without coagulating blood 18).
One of the most prominent evolutions of EVLP systems has been the introduction of numerous wavelengths, each of which have different absorption characteristics: the 810nm wavelength is specific for hemoglobin absorption; the 940nm wavelength provides a balanced ratio between the light irradiated into the tissue and the absorption by hemoglobin and water; the 980nm wavelength is such that it is specific for hemoglobin and water; the 1319nm/1320nm wavelength is specific for water absorption, targeting collagen in the vein wall; and the 1470nm wavelength features an absorption coefficient in water that is 40 times greater than that at the 810nm and 980nm wavelengths. From the basic theories, thermal ablation leaders have divided endovenous lasers into two categories based on hypothetical mechanisms of action: hemoglobin-specific laser wavelengths (HSLWs) and water-specific laser wavelengths (WSLWs). (Table 4) Hemoglobin-specific lasers are thought to produce thermal damage by using intravascular blood as a chromophore to absorb laser energy and create steam bubbles. Lasers that target hemoglobin absorption include 810nm, 940nm, and 980nm, with the lowest wavelength having the highest specificity for hemoglobin. The HSLWs lasers create bubbles from boiling blood as a result of absorption of laser energy by hemoglobin. These bubbles can disburse throughout the vein and cause heat damage to the inner vein wall up to the remote site from the fiber tip. Perforation also occurs from direct contact of the fiber tip with the vein wall when there is no blood in the vein. Carbonization of the vein wall is also caused at the perforation site by uncontrolled high temperature.
Table 4: Application for Endovascular Lasers.
| Wave Length(nm) | 810 | 940 | 980 | 1064 | 1320 | 1470 |
|---|---|---|---|---|---|---|
| Type | Diode | Diode | Diode | Nd:YAG | Nd:YAG | Diode |
| Optical Fiber(µm) | 600 | 600 | 600 | 600 | 600 | 600 |
| Power Watt(W) | 14 | 15 | 11 | 10 or 15 | 8 | 15 |
| Mean Unit Energy(J/cm) | 49.3 | 23.4 | 45.9 | Not Provided | 63 | 90 |
The WSLWs lasers are conjectured to inflict vein wall damage by targeting the interstitial fluid in the vein wall. The 1064nm, 1320nm and 1470nm lasers believed to produce thermal damage with this mechanismwith higher wavelengths demonstrating a greater affinity for water absorption.
The WSLWs lasers penetrate the blood and are absorbed by collagen in the vein wall. This causes contraction of collagen and thermal shrinkage of the vein wall, similar to radiofrequency closure. The vein diameter decreases and occludes with a small amount of thrombus formation. Controlled heating of the vein wall causes shortening and thickening of collagen fibers, vein lumen diameter shrinkage, and fibrotic sealing of the vessel. 19)
In our laser center, both hemoglobin-specific and water-specific laser wavelengths have been used for the EVLP. As factors should be considered to achieve successful results, one of the more important factors affecting EVLP is the rising temperature in the blood flow induced by energy transfer upon contact with vein wall. Another factor is the anatomic location (Saphenofemoral Junctions, side branches or perforators) for treatment as well as vein diameter. 20-21)
When a laser is delivered to a target tissue, it may be reflected, transmitted, refracted, scattered, or absorbed. The immediate tissue effect is dependent on the thermal properties and absorption spectrum of the tissue, and the wavelength and energy of the laser. Common tissue effects include photocoagulation, photovaporization, and photo-disruption. These effects may be harnessed to achieve desired therapeutic effects. Cutaneous lasers are limited by poor tissue penetration and are ineffective against varicosities located within the superficial fascia. In addition, direct application through the skin may cause non-selective thermal injury.
Our method of intravenous photocoagulation delivers the Nd:YAG laser beam via a bare optic fiber into the varicose veins. The optic fiber overcomes the difficulties of insufficient tissue penetration and skin burns by transmitting the laser beam directly into the varicose veins. Immediately after EVLP, there is coagulation of the vessel and its surrounding tissues. EVLP probably affects intravascular thrombogenesis and photocoagulation of vessels as well as surrounding tissues, leading to thrombus blockade, ischemia, sclerosis, fibrosis, and ultimately the obliteration of the varicose veins and their tributaries.
There was no wound infection or deep venous thrombosis in our observation of the early complications. Within the follow-up period, all patients recovered completely. We believe that all these complications are caused by the direct thermal effects of laser treatment. Heat injury of the sensory nerve led to sensory impairment. Positioning the optic fiber too superficially probably caused burns of the overlying skin. Delivering too much laser energy too slowly might also be responsible. The temperature at the varicose veins can be controlled by cooling with chilled water during the procedure and application of cold packs for the first 72 hours after EVLP. Application of compressive bandages on the operating table is also of paramount importance to prevent hematoma formation. Sustained compression is an important adjunct for successful outcome by reducing intravascular thrombus formation, encouraging fibrosis of the collapsed vessel, and preventing deep venous thrombosis. Keeping the patients ambulant also helps to avert deep venous thrombosis.
Although venous lesions found on legs can be categorized as leg veins or varicose veins, based on the concepts and applications of the laser in the fields of angioplasty and vascular lesions after using the EVLP for the varicose veins instead of ligation and stripping. However, small leg veins, (those with a diameter less than 200µm) still often cause cosmetic concern. Combined therapy of reticular and spider veins with laser and sclerotherapy using foam sclerosing agents, and hypertonic solution can be used. Based on the concept of selective photothermolysis, a long pulsed 1064nm Nd:YAG laser (Gentle YAG, Sharplan, Inc., NJ, USA) and flash lamp-pumped pulsed dye laser (FLP-PDL) (ScleroPLUS, Sharplan, Inc., NJ, USA) with longer wavelengths has been used for the treatment of small leg veins and spider veins.
In summary, WSLW (1060nm), and HSLW (810nm) specifically target water and hemoglobin within the blood respectively. All patients achieved good or excellent improvement after EVLP-1064nm and EVLP-810nm. However, the difference of final outcome was significant, and indicates that improvement was greater in the Diode laser group. Inadvertent contact of baretip fibers with the vein wall is unavoidable, regardless of wavelength. EVLP is undoubtedly of great benefit in the treatment of varicose veins, as it is a less invasive method that can minimize the complications of conventional surgery. While a long-pulse dye laser can be effective in the clearance of leg telangietasias, the combination of EVLP and FPPDL creates the most effective and safest method of treatment for varicose veins of late. With ongoing improvements in EVLP use, there will no doubt be even greater results in this field.
References
- 1: Callam MJ. (1992): Prevalence of chronic leg ulceration and severe venous disease in western countries. Phlebology 7S:6 - 12 [Google Scholar]
- 2: Callam MJ. (1994): Epidemiology of varicose veins. Br J Surg 81:167 - 173 [DOI] [PubMed] [Google Scholar]
- 3: Hirai M. (1990): Prevalence and risk factors of varicose veins in Japanese women. Angiology 3:228 - 232 [DOI] [PubMed] [Google Scholar]
- 4: Weiss Robert A, Feied Craig F., Weiss Margaret A. (2001): Vein diagnosis and treatment: A comprehensive approach. USA: McGraw-Hill Medical [Google Scholar]
- 5: Fegan G. (1967): Varicose veins: Compression sclerotherapy. London: Heinemann Medical [Google Scholar]
- 6: Lin SD, Tai CC, Lin TM, Lee SS, Chang KP, Lar CS. (2000): Endoscope-assisted correction of primary varicose veins. Ann Plast Surg 44:241 - 249 [DOI] [PubMed] [Google Scholar]
- 7: Goren G, Yellin A E. (1994): Invaginated axial saphenectomy by a semirigid stripper: Perforate-invaginate stripping. J Vasc Surg 20:970 - 977 [DOI] [PubMed] [Google Scholar]
- 8: Goren G, Yellin AE. (1991): Ambulatory stab avulsion phlebectomy for truncal varicose veins. Am J Surg 162:166 - 174 [DOI] [PubMed] [Google Scholar]
- 9: Walsh J, Bergan JJ, Beeman S, Comer TP. (1994): Femoral venous reflux abolished by greater saphenous vein stripping. Ann Vasc Surg 8:566 - 570 [DOI] [PubMed] [Google Scholar]
- 10: Campbell WB, Ridler BMF. (1995): Varicose vein surgery and deep vein thrombosis. Br J Surg 82:1494 - 1497 [DOI] [PubMed] [Google Scholar]
- 11: Harris EJ. (2002): Raidofrequency ablation of the long saphenous vein without high loigstion versus high ligation a stripping for primary varicose veins: Pros and cons. Semi Vasc Surg 15:34 - 38 [PubMed] [Google Scholar]
- 12: Ashley S, Kester RC. (1993): Laser angioplasty. Br J Surg 80: 550 - 551 [DOI] [PubMed] [Google Scholar]
- 13: Alani HM, Warren RM. (1992). Percutaneous photocoagulation of deep vascular lesion using a fiberoptic laser wand. Ann Plast Surg 29:143 - 148 [DOI] [PubMed] [Google Scholar]
- 14: Chang CJ, Fisher DM, Chen YR. (1999): Intralesional photocoagulation of vascular anomalies of the tongue. Br J Plast Surg 52:178 - 181 [DOI] [PubMed] [Google Scholar]
- 15: Fisher DM, Chang CJ, Chau JJ, Chen YR, Achauer BM. (2001): Potential complications of intralesional laser photocoagulation for extensive vascular malformations. Ann Plast Surg 47:252 - 256 [DOI] [PubMed] [Google Scholar]
- 16: Achauer BM, Chang CJ, VanderKam VM, Boyko A. (1999): Intrale- sional photocoagulation (ILP) of periorbital hemangiomas. Plast Reconstr Surg 103(1):11 - 16 [DOI] [PubMed] [Google Scholar]
- 17: Chang CJ, Chua JJ. (2002): Endovenous laser photocoagulation (EVLP) forv aricose veins. Lasers Surg Med 31:257 - 262 [DOI] [PubMed] [Google Scholar]
- 18: Lurie F, Creton D, Eklof B, Kabnick LS, Kistner RL, Pichot O. (2003): Prospective randomized study of endovenous radiofrequency obliteration (closure) versus ligation and stripping in a selected patient population (EVOLVES Study). J Vasc Surg 38:207-14 [DOI] [PubMed] [Google Scholar]
- 19: Almeida JI, Kaufman J, Gockeritz O. (2009): Radiofrequency endovenous closure fast versus laser ablation for the treatment of great saphenous reflux: A multicenter, single-blinded, randomized study (recovery study). J Vasc Interv Radiol 20(6): 752-759 [DOI] [PubMed] [Google Scholar]
- 20: Calcagno D, Rossi JA, Ha C. (2009): Effect of saphenous vein diameter on closure rate with closure fast radiofrequency catheter. vasc endovasc surg. [DOI] [PubMed] [Google Scholar]
- 21: Min RJ, Khilnani NM. (2005): Endovenous laser ablation of varicose veins. J Cardiovasc Surg 40:395-405 [PubMed] [Google Scholar]


