Abstract
Background and Aims: Scars are common and cause functional problems and psychological morbidity. Recent advances in optical technologies have produced various laser systems capable of revising the appearance of scars from various etiologies to optimize their appearance.
Methods: Laser treatment can commence as early as the time of the initial injury and as late as several years after the injury. Several optical technologies are currently available and combined laser/light treatments are required for treatment of scars. Since 2006, we have set up a scar management department in our clinic and more than 2000 patients have been treated by our combined laser irradiation techniques. Herein, we review several available light technologies for treatment of surgical, traumatic, and inflammatory scars, and discuss our combined laser treatment of scars, based upon our clinical experience.
Results and Conclusions: Because scars have a variety of potential aetiologies and take a number of forms, no single approach can consistenty provide good scar treatment and management. The combination of laser and devices is essential, the choice of wavelength and approach being dictated by each patient as an individual.
Keywords: Scar, Laser Treatment, Combination
Introduction
Although scars may in some cases fade to some degree, the majority of scars never disappear. If a patient has some symptoms or unsightly lesions due to their scar, they usually try to conceal or manage their scar in one way or another. Recently, the mechanisms underlying the wound healing process have been gradually elucidated and medical or cosmetic procedures for scars have been developed. The treatment of scars has become more effective and good scar management has developed well, On the other hand, the treatment and management of scars cannot be accomplished with only one laser device, and many kinds of laser or non-laser devices are needed to achieve the total management of scars. We review the history of scar treatment by lasers and then our treatment procedure of scars will be introduced.
History of laser treatment for scars and keloids
In the 1980s, the argon laser and CO2 lasers were used for the treatment of scars. 1-3) These lasers could flatten the scar surface by vaporizing the scar tissue. Around the same time, laser diode-based systems were also applied for scars and keloids. 4-5) Irradiation of scars with low incident levels of laser energy, such as diode laser low level light therapy as advocated by Ohshiro (LLLT) 6-7) could induce the decrease of symptoms, such as pain and itchiness, and achieve the improvement of appearance of scars through photobiomodulatory activities. In the 1990s, the tunable pulsed dye laser (PDL) was applied, and many good clinical results and basic studies were reported by researchers such as Alster et al. 8-11) In PDL treatment, it is considered that the target of the PDL is the microvasculature in scars and keloids, and selective destruction of blood vessels in scars induces the improvement of the appearance of scars through several photochemical and other cascades. 12-15)
In the 2000s, the long pulsed dye laser (LPDL) was developed. Irradiation of tissues with different LPDL pulse widths induced a number of different clinical results. 16) Non-ablative fractional lasers (wavelength 1550 nm, 1540 nm and so on) and ablative fractional lasers (wavelength 2790 nm and 10600 nm) were introduced, and so many clinical results were reported in the field of treatment of scars. 17-20)
Now many kinds of laser technology are available for scar treatments, but no medical guidelines currently exist concerning the laser scar treatment and management. Through our 40 years' clinical experience of laser treatment, we have established our original treatment guidelines for scar treatment.
Laser scar management techniques
Scars never disappear histologically. It is necessary for scar treatment to make the scars unnoticeable and to manage the different symptoms associated with scars in one way or another. We therefore named our laser scar treatment strategy ‘laser scar management techniques’.
In laser scar management techniques, the following two steps are important. The first step is to diagnose the characteristics of each scar as an individual case, and the second step is to decide the prompt therapeutic planning.
Diagnosis
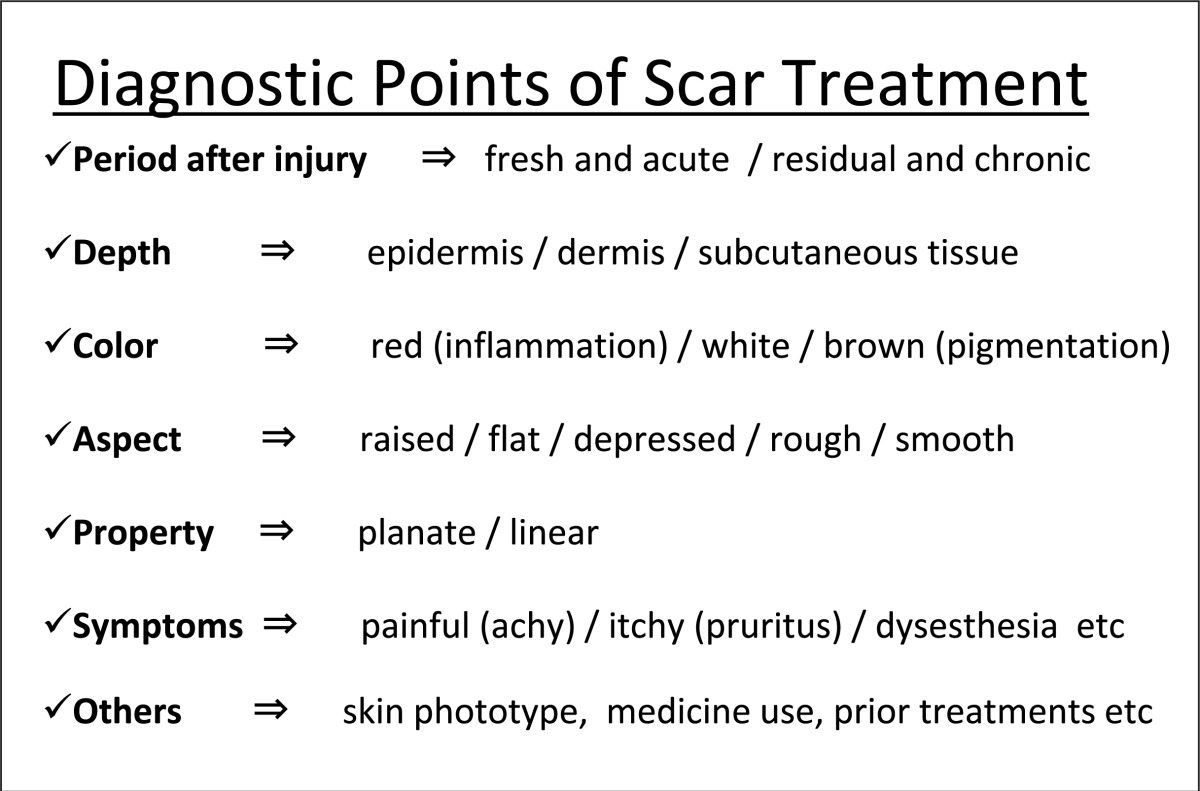
Scars differ from one site to another, so we have to diagnose them precisely. Table 1 shows the points related to the therapeutic planning.
Table 1: Diagnostic points of scar treatment.
 |
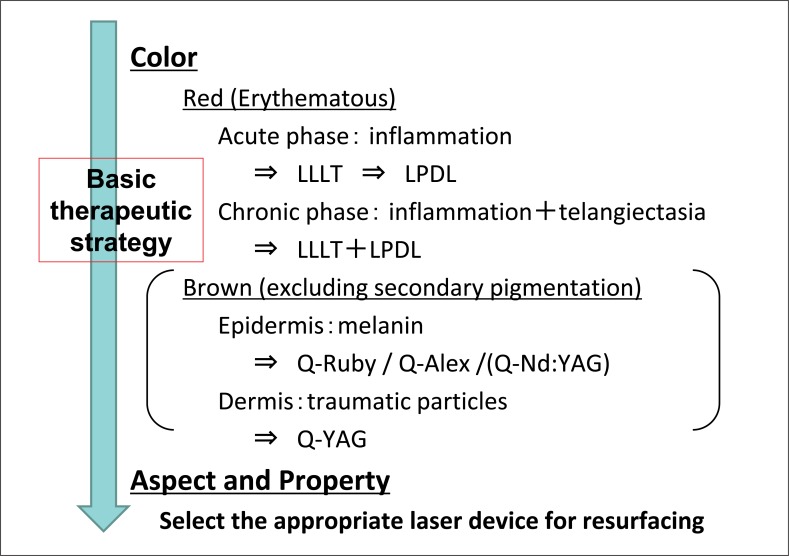
Therapeutic planning and procedures (Figure 1)
Figure 1:
Therapeutic planning and procedures
Scars have several characteristics and we have to resolve the individual points sequentially. Figure 1 shows our basic therapeutic protocols for scars.
The color and appearance, including the aspect and the properties of each scar, are the most important points. At the beginning, we start by treating the color of the scar, followed by treatment of the configuration.
For color treatment, the red color of the scar is very important. Erythematous scars have at the very least a mild degree of inflammation. So at first, to reduce the acute or chronic inflammation, LLLT devices and/or LPDL are applied. Along with the gradual improvement of the inflammation, scars become soften and flatten, concomitantly with a decrease in the major symptoms such as itchiness and pain. If the scars exhibit a brownish color/pigmentation, this is somewhat difficult to treat, because the aetiology which has induced the color is different in each case. For the temporary and secondary pigmented lesion, waiting for 6 months is the best approach. Using topical bleaching agents (hydroquinone, retinoic acid and so on) and moisturizing agents, the brown color can gradually be bleached. If on the other hand, the brown color which is not bleached by topical ointments within 6 months, Q-switched lasers (Q-switched Ruby laser, Q-switched Alexandrite laser and Q-switched Nd:YAG laser) are applied.
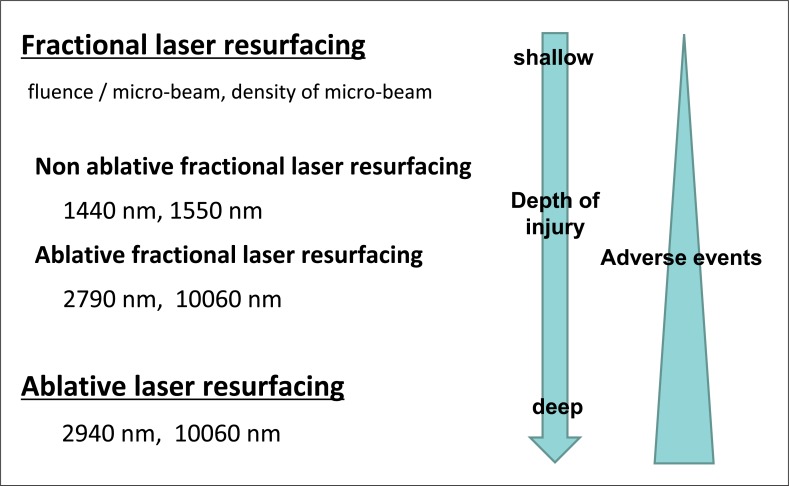
Finally, the scar aspect and properties are treated with the appropriate resurfacing laser device to make the scars less noticeable, There are two resurfacing procedures, one is fractional laser resurfacing, the other is conventional ablative laser resurfacing (Figure 2). Since 2000, various types of fractional laser devices have been introduced. According to the treatment purpose, non-ablative fractional laser resurfacing or ablative fractional laser resurfacing can be selected. As the scar aspect and properties are different in each case, we must therefore select the appropriate resurfacing laser device, or use different resurfacing lasers in turn. This final step makes the scar surface flat, and obscures the shape and appearance, resulting in a less noticeable scar.
Figure 2:
Resurfacing procedures and therapeutic features
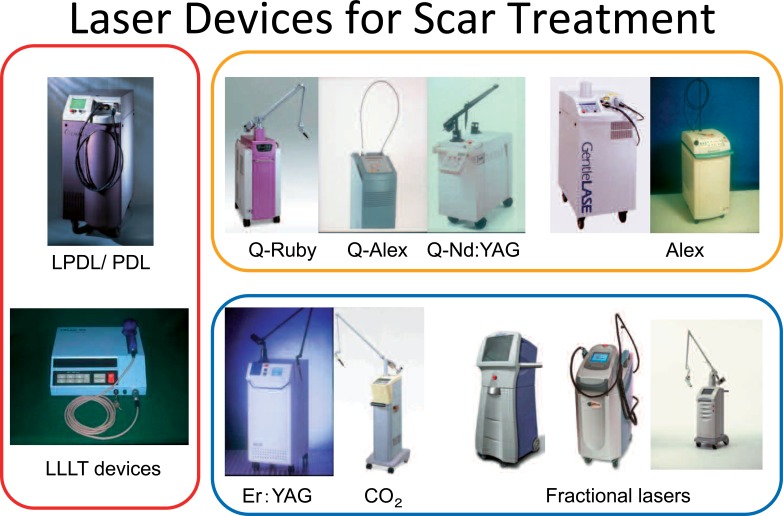
Laser Devices
Figure 3 shows the laser devices for scar management.
Figure 3:
Laser devices for scar treatment
Red: treatment for red color and symptoms due to acute inflammation
LPDL/PDL: long pulsed dye laser / pulsed dye laser
LLLT devices: devices for low reactive level laser therapy
Yellow: treatment for brown color (pigmentation)
Q-Ruby: Q-switched ruby laser
Q-Alex: Q-switched alexandrite laser
Q-Nd:YAG: Q-switched Nd:YAG laser
ALEX: long pulsed alexandrite laser
Blue: treatment for appearance (aspect and property)
Case Presentation
We have selected 5 typical 5 cases using our laser scar management techniques.
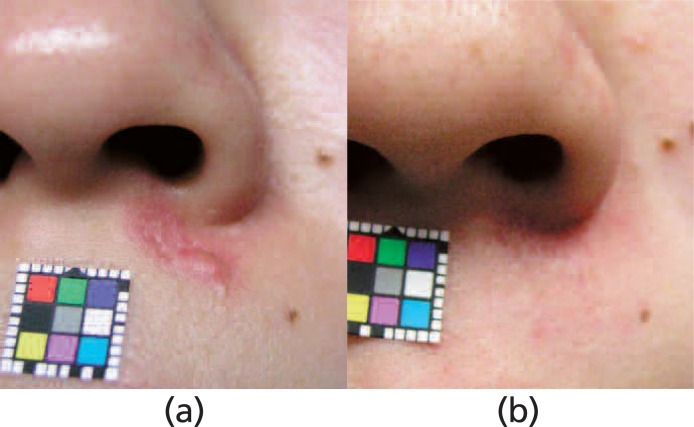
Case 1: Hypertrophic and planate scar (Figure 4)
Figure 4:
Hypertrophic and planate scar 15 months after injury
(a) Pre-treatment (b) Post-treatment
Treatment period: 12 months
Treatment procedures: LLLT 11 sessions
LPDL 8 sessions (8–12 J/cm2 10–20 ms 7 mm Ø)
A 25 y.o. female had suffered an injury to her face in a traffic accident, and was bothered by the hypertrophic and planate scar on her white lip. 15 months after injury, she suffered from persistent pruritus. As there was prolonged inflammation, at first, LLLT was applied once a week. After 5 treatment sessions with 830 nm diode laser LLLT, she became symptom-free. Next, for the residual erythematous scar, the LPDL was utilized once a month. 12 months after the start of treatment, a good appearance was obtained.
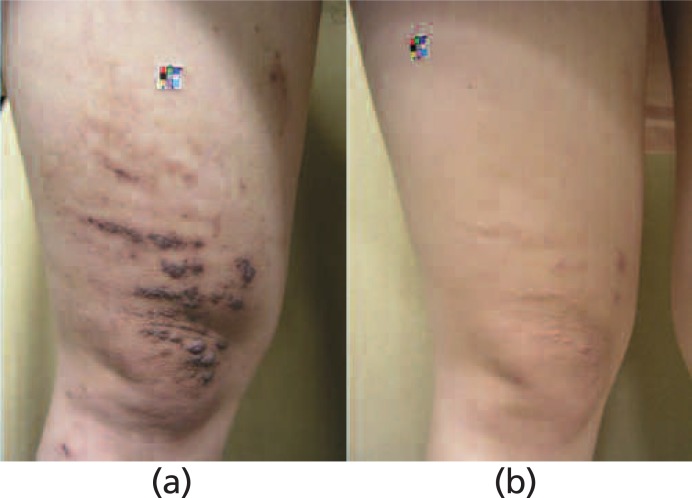
Case 2: Hypertrophic, planate and pigmented scar (Figure 5)
Figure 5:
Hypertrophic, planate and pigmented scar 12 months after injury
(a) Pre-treatment (b) Post-treatment
Treatment period: 12 months
Procedures: LLLT 21 sessions
LPDL 7 sessions (12–14 J/cm2 10–20 ms 7 mm Ø)
A 19 y.o. female had received a chemical burn on her right thigh. Twelve months after the injury, she suffered from both the appearance of the scar and a severe ache. As prolonged inflammation was causing the persistent symptoms, we started 830 nm laser diode LLLT twice a week. Within 1 month after the start of treatment, the inflammation was reduced, and the symptoms were improved. Concurrently the slight pigmentation on the scar gradually disappeared. For the erythematous and hypertrophic appearance of the scar, LPDL was utilized once a month. Finally a good appearance of the scar was obtained, and the patient was free of any scar-related symptoms such as pain and itching.
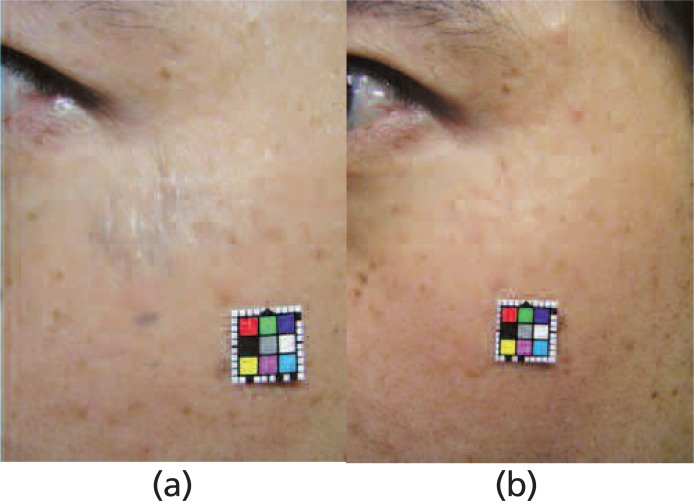
Case 3: Dermal pigmented, planate and rough scar (Figure 6)
Figure 6:
Dermal pigmented, planate and rough scar 7 years after injury
(a) Pre-treatment (b) Post-treatment
Treatment period: 12 months
Procedures: Q-Nd:YAG 3 session (8 J/cm2 .2 mm Ø)
Er:glass fractional laser 4 sessions (Fraxel 10–14 mJ 125 MTZ 8 passes)
A 31 y.o. male had been injured on his cheek in an accident. The inflammation was already reduced. There were remnant particles in the dermis (traumatic tattoo), and the skin surface was irregular. At first, the dermal pigmentation was treated with a Q-switched Nd:YAG laser, and next non-ablative fractional resurfacing was performed on the surface of the scar every 1 month. Within 12 months after starting treatment, the color and texture of the scar surface had remarkably improved.
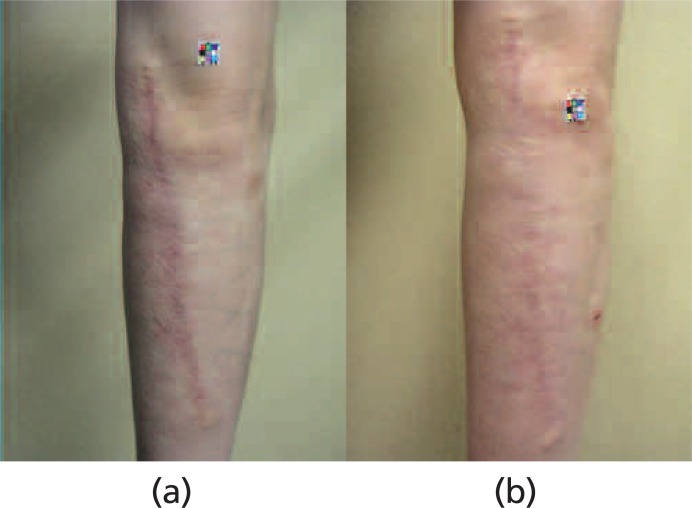
Case 4: Pigmented, planate and post-operative burn scar (Figure 7)
Figure 7:
Pigmented, planate and post-operative burn scar 1 year after scar revision
(a) Pre-treatment (b) Post-treatment
Treatment period: 12 months
Procedures: ALEX 3 sessions (16 J/cm2 20 ms 10 mm Ø)
Er:glass fractional laser 3 sessions (Fraxel 8–10 mJ 125 MTZ 8 passes)
A 53 y.o. male had a slightly pigmented and planate scar on his forearm as a result of a severe burn in his early childhood. One year before visiting our clinic, scar revision was performed in another clinic. Slight pigmentation along the linear scar and planate irregular burn scar were readily apparent, but otherwise the scar was asymptomatic. At first, a long-pulsed alexandrite laser was used for the pigmented lesion, and non-ablative fractional laser resurfacing was performed to flatten the scar surface every 2 months. A good appearance was achieved within 12 months after the start of treatment.
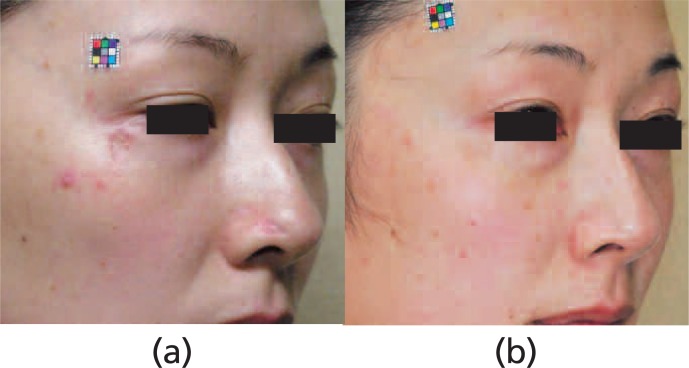
Case 5: Erythematous planate and depressed scars (Figure 8)
Figure 8:
Erythematous planate and depressed scars 1 year after injury
(a) Pre-treatment (b) Post-treatment
Treatment period: 12 months
Procedures: LLLT 22 sessions
LPDL 5 sessions (cheek + nose) (12 J/cm2 10–20 ms 7 mm Ø)
Er:glass fractional laser 4 sessions (cheek) (Fraxel 20 mJ 125 MTZ 5 passes)
CO2 fractional laser 2 sessions (nose) (UCO2 DeepFX 14 mJ 2 passes)
A 35 y.o. female had depressed scars due to varicella-zoster infection on her face. The cheek scar was slight reddish and had a depressed coin-like shape, and the nasal scar was deeply depressed. LLLT and LPDL were started to reduce the residual inflammation, and within 6 months the erythematous color had improved. Fractional laser resurfacing was applied to both depressed lesions to obscure the scar contours. The depressed levels of both scar differed in degree, so a different type of fractional laser was applied to each lesion respectively. Excellent results were obtained within 12 months.
Conclusion
There are several laser systems available that permit successful treatment of various types of scars. Laser scar management technique is optimized when individual patient and scar characteristics are thoroughly evaluated to determine the best course of treatment. As laser technologies evolve and the mechanisms underpinning wound healing continue to be elucidated, new technological indications will be identified, resulting in more improved management of a wide range of wounds and scars.
Reference
- 1: Ohshiro T, Kotaki S, et al. : Argon laser treatment in plastic surgery and dermatology. J JSLSM 1(1),534-538, 1980 [Google Scholar]
- 2: Kotaki S, Ohshiro T, et al. : Laser treatment of hypertrophic scars. J JSLSM (1),482-486,1980 [Google Scholar]
- 3: Henderson DL, Cromwell TA, Mes LG: Argon and carbon dioxide laser treatment of hypertrophic scars and kloid scars. Lasers Surg Med. 3(4): 271-277 1984 [DOI] [PubMed] [Google Scholar]
- 4: Ohshiro T, Maeda T: Application of 830nm diode laser LLLT as successful adjunctive therapy of hypertrophic scars and keloids, Laser Therapy 4(4):155-168, 1992 [Google Scholar]
- 5: Fujii S, Ohshiro T, Ohshiro T, et al. : Low reactive level laser therapy (LLLT) for the treatment of hypertrophic scars and keloids. A re-introduction, Laser Therapy 17: 35-43, 2008 [Google Scholar]
- 6: Ohshiro T, Fujino T: Laser applications in plastic and reconstructive surgery, Keio J Med 42(4):191-195, 1993 [DOI] [PubMed] [Google Scholar]
- 7: Ohshiro T. High reactive-level laser treatment (HLLT) and low reactive-level laser therapy (LLLT) in dermatology. Photomed Photobio 1994; 16: 123-126 [Google Scholar]
- 8: Alster TS, Kurban AK, Grove GL, et al. : Alteration of argon laser-induced scars by the pulsed dye laser, Laser Surg Med 13:368-373, 1993 [DOI] [PubMed] [Google Scholar]
- 9: Alster TS, Williams CM: Treatment of keloidal sternotomy scars with 585nm flashlamp-pumped pulsed-dye laser. Lancet 345:1198-1200, 1995 [DOI] [PubMed] [Google Scholar]
- 10: Manuskiatti W, et al. : Energy density and numbers of treatment affect response of keloidal and hypertrophic sternotomy scars to the 585nm flashlamp pumped pulsed-dye laser, J Am Acad Dermatol 45:p557-565, 2001 [DOI] [PubMed] [Google Scholar]
- 11: Manuskiatti W, Fitzpatrick RE: Treatment response of keloidal and hypertrophic sternotomy scars, Arch Dermatol 138: p1149-1155, 2002 [DOI] [PubMed] [Google Scholar]
- 12: Kuo YR, Jeng SG, Wang FS, et al. : Flashlamp pulsed dye laser (PDL) suppression of keloid proliferation through down regulation of TGF-β1 expression and extracellular matrix expression, Laser Surg Med 34: 104-108, 2004 [DOI] [PubMed] [Google Scholar]
- 13: Kuo YR, Wu WS, Jeng SG, et al. : Activation of ERK and p38 kinase mediated keloid fibroblast apoptosis after flashlanp pulsed-dye laser treatment, Laser Surg Med 36:31-37, 2005 [DOI] [PubMed] [Google Scholar]
- 14: Kuo YR, Wu WS, Wang FS, et al. : Suppressed TGF-β1 expression is correlated with up-regulation of matrix metalloproteinase-13 in keloid regression after flashlamp pulsed-dye laser treatment. Laser Surg Med 36: 38-42, 2005 [DOI] [PubMed] [Google Scholar]
- 15: Kuo YR, Wu WS, Wang FS: Flashlamp pulsed-dye laser suppressed TGF-β1 expression ond proliferation in cultured keloid fibroblast in mediated by MARK pathway. Laser Surg Med 39, 358-364, 2007 [DOI] [PubMed] [Google Scholar]
- 16: Manuskatti W, Wanitphakdeedecha R, Fitzpatrick RE: Effect of pulse width of a 595-nm flashlamp-pumped pulsed dye laser on the treatment response of keloidal and hypertrophic sternotomy scars, Dermatol Surg 33(2), 152-161, 2007 [DOI] [PubMed] [Google Scholar]
- 17: Glaich AS, Pahman Z, Goldberg LH, et al. : Fractional resurfacing for the treatment of hypopigmented scars: a pilot study, Dermatol Surg 33(3): 289-294, 2007 [DOI] [PubMed] [Google Scholar]
- 18: Alster TS, Tanzi EL, Lazarus M: The use of fractional laser photothermolysis for the treatment of atrophic scars, Dermatol Surg 33(3): 295-299, 2007 [DOI] [PubMed] [Google Scholar]
- 19: Tierney E, Mahmoud BH, Srivastava D, et al. : Treatment of surgical scars with nonablative fractional lasers versus pulsed dye laser: a randomized controlled trial, Dermatol Surg 35: 1172-80, 2009 [DOI] [PubMed] [Google Scholar]
- 20: Cervelli V, Gentile P, Spallone D, et al. : Ultrapulsed fractional CO2 laser treatment of post-traumatic and pathological scars, J Drugs Drmatol. 9: 1328-31, 2010 [PubMed] [Google Scholar]