Abstract
Objective. To study patient-level improvements in pain and limitations of key activities of daily living (ADLs) after primary or revision total knee arthroplasty (TKA).
Methods. We analysed prospectively collected data from the Mayo Clinic Total Joint Registry for improvements in index knee pain severity and limitations in three key ADLs (walking, climbing stairs and rising from a chair) from pre-operative to 2 and 5 years post-TKA.
Results. The primary TKA cohort consisted of 7229 responders pre-operatively, 7139 at 2 years and 4234 at 5 years post-operatively. The revision TKA cohort consisted of 1206 responders pre-operatively, 1533 at 2 years and 881 at 5 years post-operatively. In the primary TKA cohort, important pain reduction to mild or no knee pain at 2 years was reported by 92% with moderate pre-operative pain and 93% with severe pre-operative pain; respective proportions were 91% and 91% at 5 years follow-up. For revision TKA, respective proportions were 71% and 66% at 2 years and 68% and 74% at 5 years. Three per cent with no/mild pre-operative overall limitation and 19% with moderate/severe pre-operative overall limitation had moderate/severe overall activity limitation 2 years post-operatively; at 5 years the respective proportions were 4% and 22%. Respective proportions for revision TKA were up to 3% and 32% at 2 years and 4% and 34% at 5 years.
Conclusion. Our study provides comprehensive data for patient-level improvements in pain and key ADLs. These data can be used to inform patients pre-operatively of expected outcomes, based on pre-operative status, which may further help patients set realistic goals for improvements after TKA.
Keywords: pain, activity limitation, activities of daily living, function, functional limitation, total knee replacement, arthroplasty, joint replacement, outcomes, patient-reported outcomes, primary
Introduction
Total knee arthroplasty (TKA) is the most common elective orthopaedic procedure, performed for severe end-stage arthritis and associated with significant improvement of pain, function and daily activities [1]. According to the Healthcare Cost and Utilization Project, 686 000 TKA procedures were performed in 2009 in the USA [2], similar to the estimates from a population-based study [3]. TKA volume is increasing rapidly [4] and is projected to increase 6-fold from 2005 to 2030 [5]. Suboptimal outcomes in pain and function are reported by up to 20% patients after TKA [6]. Most validated scales used for the assessment of TKA outcomes combine pain and function domain assessments with another domain to provide a composite score. A key example is the American Knee Society (AKS) Scale [7], the most common outcome instrument used in TKA, where the knee subscale is a composite of pain, range of motion and stability. Validated composite scales like the Knee Society Scale (KSS) have demonstrated well that significant improvements occur with TKA, but they have certain limitations. First, pain, range of motion and joint stability (and function in some cases), separate domains that are of varying importance to patients undergoing TKA, are often combined into a single score, making the interpretation of patient-level improvements in the pain and function domains separately very difficult [8, 9]. Second, most studies to date provide only average changes at the cohort level rather than patient-level meaningful improvements. Third, these studies have not provided data related to important changes in these scales and the thresholds have been defined for several outcome instruments [10].
The primary reasons a patient undergoes a TKA are to improve knee pain and/or improve the patient’s ability to perform various activities. Patients are most interested in knowing the probability of improvement in their pain and their ability to perform specific activities important to them and in daily living. It is reasonable to start by obtaining such estimates for key activities of daily living (ADLs) related to knee joint function, realizing that ultimately estimates for improvement in both key ADLs (walking, climbing stairs, etc.) and recreational activities (sports, tennis, golf, skiing, etc.) will be needed. It is challenging to extrapolate from group-level mean improvements in the currently published literature to a patient-level meaningful improvement (change in pain from severe pain pre-operatively to mild pain at follow-up). Estimation of the proportion of patients that achieve such improvements can truly provide important information for patients. To our knowledge, these patient-level data are not available at present.
We recently described patient-level improvements for patients undergoing total hip arthroplasty [11]. Using the prospectively collected data from the same institutional US joint registry, our objective was to study patient-level improvements after TKA in an easily interpretable format. Specifically, we aimed to (i) study pain and limitations in three key ADLs, pre- and post-operatively and (ii) describe important changes in pain and three ADLs 2 and 5 years after primary and revision TKA.
Methods
Setting, participants and data sources
We used data collected prospectively in the Mayo Clinic Total Joint Registry. The Mayo Clinic Total Joint Registry collects prospective data on all joint replacements performed at the Mayo Clinic, Rochester, MN, USA Data included patient demographics, surgery and implant details, radiographs, complications/surgeries and pain and function assessments [12, 13]. All patients who undergo TKA at the Mayo Clinic are requested to complete validated Mayo knee questionnaires [14], containing pain and function questions, both pre-operatively and at regular follow-up visits (2 and 5 years). Dedicated, experienced joint registry staff assist in the completion of these questionnaires pre-operatively and at the 2- and 5-year time points after joint replacement, including mailed questionnaires and administration during the clinic visit or by telephone. The questionnaire data have been captured electronically since 1993. We included patients in this study if they had undergone a primary or revision TKA during 1993–2005 and had responded to pre-surgery and post-surgery knee questionnaires (2- or 5-year follow-up). The Institutional Review Board (IRB) at the Mayo Clinic approved the study and waived informed consent for this database study.
Demographics (age, gender, etc.), clinical characteristics [American Society of Anaesthesiologists class, BMI, etc.] and medical comorbidity assessed using the validated Deyo–Charlson index [15] based on the presence of International Classification of Diseases, ninth revision, clinical modification (ICD-9-CM) were obtained from the Mayo Clinic Total Joint Registry and linked databases.
Outcomes of interest
Patients answered the following pain question at 2 and 5 years post-TKA: Do you have pain in the knee in which the joint was replaced? The responses were no pain, mild (occasional) (all combined into reference category); stairs only, walking and stairs (set to missing since the severity of pain is unclear with these responses); moderate (occasional), moderate (continuous) and severe categories—combined into the outcome variable moderate to severe pain, based on an a priori decision and as previously [16, 17]. Moderate to severe pain was assessed at 2 and 5 years after primary and revision TKA. This question is similar to the pain question in the KSS, a validated outcome instrument for patients with TKA [7]. In addition, the moderate to severe pain category has been used in previous studies [16–18]. A similar question was also administered pre-operatively that had the same response categories.
Patients self-reported limitations in three key ADLs that specifically assessed index knee function, namely walking, climbing stairs and rising from a chair, on validated questionnaires. The limitations were classified a priori as follows, as previously [19]: (i) distance walked: unlimited or more than 10 blocks = none; 5–10 blocks = mild; <5 blocks = moderate; and housebound, indoors only or unable = severe; (ii) stairs: normal up and down = none; normal up, down with rail = mild; up and down with rail = moderate; and up with rail, down unable or unable = severe and (iii) rising from a chair: able, no arms = none; able, with arms = mild; able with difficulty = moderate; and unable = severe, as previously [19]. Moderate to severe overall activity limitation was defined as moderate or severe limitation in two or more key ADLs (reference, none/mild limitations) to allow an easier interpretation of the study findings, as previously [19, 20].
We defined important improvements a priori as follows: (i) improvement in pain: reduction from moderate or severe pain pre-operatively to mild pain or no pain post-operatively—since occurrence of mild/no pain is deemed as a success for this elective surgery done primarily to improve pain and function and (ii) improvement in ADL limitation: reduction from moderate or severe pre-operative ADL limitation to mild or no post-operative limitation in the respective ADL and in the overall ADL limitation.
Statistical analyses
We assessed the proportion of patients in various categories of pain severity and ADL limitations pre-operatively and 2 and 5 years post-TKA. All analyses were done separately for primary and revision TKA and separately for 2- and 5-year follow-up. Responder and non-responder characteristics were compared using logistic regression analyses. A P-value <0.05 was considered significant.
Role of the funding source
The funding sources (Mayo Clinic Orthopaedic Surgery Department and National Institutes of Health) had no role in study conception, protocol development, data analyses, manuscript preparation or decision to submit. The authors made all the decisions.
Results
Patient characteristics
Demographic and clinical characteristics of primary and revision TKA cohorts at baseline and at 2- and 5-year follow-up are shown in Table 1. For the 2-year primary TKA follow-up cohort, the mean age was 68 years, 44% were men, 19% were ≤60 years of age, 13% had BMI <25 kg/m2 and OA was the underlying diagnosis in 94% (Table 1). Characteristics of pre-operative and 5-year cohorts were similar. The revision TKA cohorts were similar demographically to the primary TKA cohorts and loosening/wear/osteolysis was the underlying diagnosis in 60% (Table 1).
Table 1.
Clinical and demographic characteristics of primary and revision TKA cohorts
| Primary TKA |
Revision TKA |
|||||
|---|---|---|---|---|---|---|
| Pre-op (n = 7229) | 2-year (n = 7139) | 5-year (n = 4234) | Pre-op (n = 1206) | 2-year (n = 1533) | 5-year (n = 881) | |
| Mean age ± s.d. | 68 ± 10 | 68 ± 10 | 68 ± 10 | 68 ± 10 | 69 ± 10 | 69 ± 10 |
| Men/women, % | 44/56 | 44/56 | 45/55 | 50/50 | 49/51 | 51/49 |
| Age groups, years, % | ||||||
| ≤60 | 19 | 18 | 18 | 22 | 20 | 20 |
| >60–70 | 35 | 35 | 37 | 31 | 29 | 31 |
| >70–80 | 38 | 38 | 38 | 39 | 42 | 41 |
| >80 | 8 | 8 | 7 | 8 | 9 | 8 |
| BMI, %,kg/m2 | ||||||
| <25 | 13 | 13 | 13 | 12 | 13 | 14 |
| 25–29.9 | 35 | 35 | 36 | 35 | 36 | 39 |
| 30–34.9 | 30 | 29 | 43 | 28 | 29 | 27 |
| 35–39.9 | 14 | 14 | 7 | 16 | 14 | 14 |
| ≥40 | 8 | 9 | 7 | 9 | 7 | 5 |
| American Society of Anesthesiologists class, % | ||||||
| Class I | 2 | 2 | 2 | 2 | 2 | 2 |
| Class II | 55 | 56 | 57 | 50 | 48 | 52 |
| Class III | 43 | 42 | 41 | 48 | 49 | 46 |
| Class IV | 1 | 1 | 1 | 1 | 1 | 1 |
| Deyo–Charlson index, mean (s.d.) | 1.3 (2.0) | 1.2 (1.9) | 1.1 (1.9) | 1.0 (1.8) | 1.0 (1.7) | 1.0 ± 1.4 |
| Psychological comorbidity, % | ||||||
| Anxiety | 6 | 6 | 5 | 5 | 5 | 3 |
| Depression | 10 | 10 | 8 | 8 | 8 | 5 |
| Implant fixation, % | ||||||
| Uncemented | 2 | 2 | 1 | 0 | 0 | 0 |
| Cemented/hybrid | 98 | 98 | 99 | 100 | 100 | 100 |
| Diagnosis, % | ||||||
| OA | 94 | 4 | 2 | |||
| Rheumatoid/inflammatory arthritis | 94 | 4 | 2 | |||
| Other | 93 | 5 | 3 | |||
| Loosening/wear or osteolysis, % | 60 | 57 | 61 | |||
| Dislocation, bone or prosthesis fracture, instability, non-union, % | 25 | 22 | 20 | |||
| Failed prior arthroplasty with components removed or infection, % | 15 | 21 | 19 | |||
Characteristics of survey non-responders
Response rates were 65% and 57% at 2 years and 57% and 48% at 5 years for primary and revision TKA, respectively. For primary TKA 2- and 5-year follow-up, men and those with OA were slightly more likely to respond and older age was associated with significantly greater odds of response (Table S1, available at Rheumatology Online). Higher American Society of Anesthesiologists class of 3 or 4 and a higher Deyo–Charlson comorbidity index score were associated with slightly lower odds or response and a distance >500 miles from the Mayo Clinic was associated with a much lower odds of response. Similar patterns were noted for revision TKA patients (Table S1, available at Rheumatology Online).
Prevalence and important improvements in index knee pain after TKA
Moderate or severe index knee pain was reported by 81% and 15% of patients before primary TKA, 7% and 0.5% of patients at 2 years and 8% and 0.8% of patients 5 years after primary TKA, respectively (Fig. 1). For revision TKA, the respective proportions for moderate or severe knee pain were 65% and 9.5% pre-operatively, 21% and 3% at 2 years and 24% and 3% at 5 years (Fig. 1).
Fig. 1.
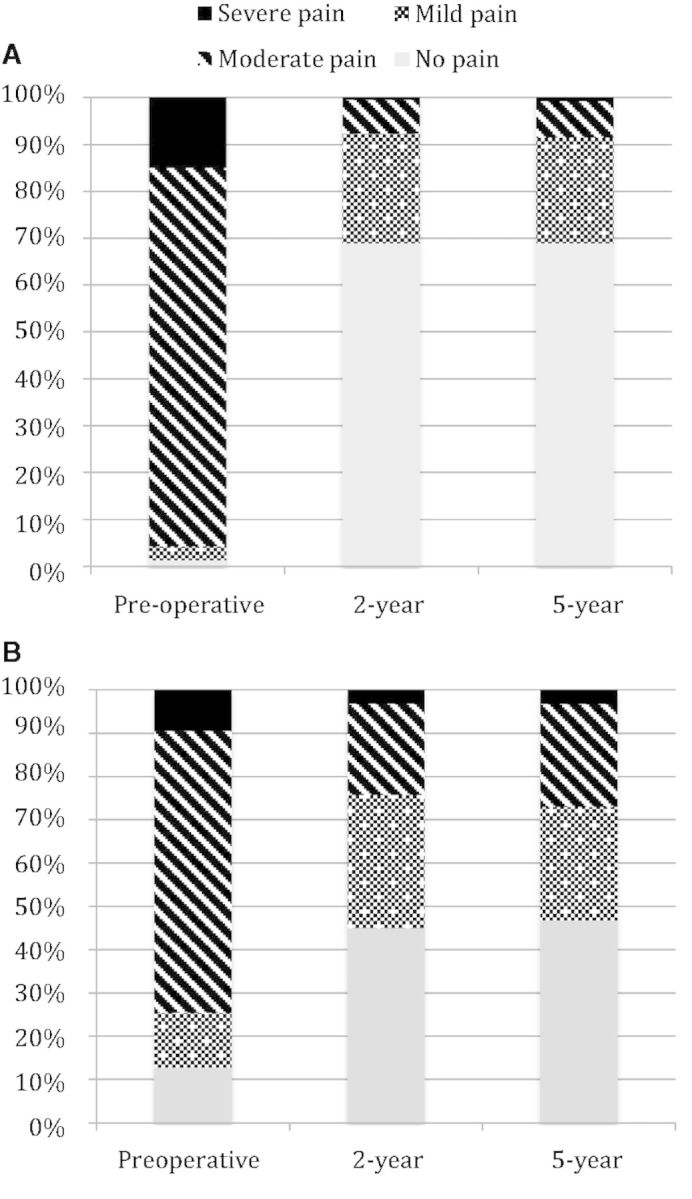
Prevalence of pain pre-operative, 2- and 5-year post primary TKA (A) and revision TKA (B).
Fig. S1, available at Rheumatology Online, shows important improvements in pain after primary and revision TKA at 2 and 5 years. In the primary TKA cohort, 92% of patients with moderate knee pain and 93% with severe knee pain pre-operatively had a substantial reduction in pain severity to mild or no knee pain 2 years after primary TKA. Similarly, 91% of patients with moderate and 91% with severe pre-operative knee pain had substantial improvement to mild or no pain 5 years after primary TKA.
In the revision TKA cohort, 71% with moderate and 66% with severe pre-operative knee pain had substantial improvement to mild or no pain 2 years after revision TKA. while 68% with moderate and 74% with severe knee pain pre-operatively had substantial pain reduction to mild or no pain 5 years after revision TKA.
Prevalence of pre-operative ADL limitations
Pre-operatively, moderate or severe limitations in ADLs were extremely common in patients undergoing primary TKA. We found that 71% had moderate to severe limitation in walking, 86% in stair climbing and 31% in rising from a chair pre-operatively (Table 2). Overall pre-operative activity limitations were moderate or severe (two or more ADLs with moderate to severe limitations) in 70% in the primary TKA cohort.
Table 2.
Primary TKA: unadjusted prevalence of functional limitation pre-operative and at the two follow-up periods (2- and 5-year)
| None, % | Mild, % | Moderate, % | Severe, % | ||
|---|---|---|---|---|---|
| Walking limitations | Pre-operative | 13.4 | 15.7 | 57.0 | 13.8 |
| 2-year | 60.2 | 14.1 | 19.7 | 6.1 | |
| 5-year | 52.3 | 13.3 | 25.1 | 9.2 | |
| Stair limitations | Pre-operative | 3.3 | 11.3 | 76.9 | 8.5 |
| 2-year | 36.0 | 23.5 | 37.7 | 2.8 | |
| 5-year | 33.1 | 21.6 | 41.2 | 4.1 | |
| Rise from chair limitations | Pre-operative | 9.4 | 59.7 | 30.3 | 0.6 |
| 2-year | 42.5 | 49.4 | 7.8 | 0.3 | |
| 5-year | 38.7 | 50.3 | 10.4 | 0.5 |
Pre-operative moderate or severe limitations in ADLs were very common in the revision TKA cohort, ranging from 66% for walking limitations to 85% for stair climbing limitations and 38% for rising from a chair (Table 3). Overall pre-operative activity limitations were reported as moderate to severe by 69% of revision TKA patients.
Table 3.
Revision TKA: unadjusted prevalence of functional limitation pre-operative and at the two follow-up periods (2- and 5-year)
| None, % | Mild, % | Moderate, % | Severe, % | ||
|---|---|---|---|---|---|
| Walking limitations | Pre-operative | 21.4 | 12.7 | 45.7 | 20.2 |
| 2-year | 37.8 | 14.0 | 33.9 | 14.3 | |
| 5-year | 33.8 | 12.9 | 33.6 | 19.7 | |
| Stair limitations | Pre-operative | 4.6 | 10.6 | 71.6 | 13.2 |
| 2-year | 17.6 | 19.1 | 52.9 | 10.5 | |
| 5-year | 15.8 | 17.7 | 56.0 | 10.4 | |
| Rise from chair limitations | Pre-operative | 10.2 | 51.3 | 36.3 | 2.1 |
| 2-year | 23.4 | 54.8 | 20.5 | 1.3 | |
| 5-year | 22.1 | 52.8 | 23.4 | 1.8 |
Important improvements in ADL limitations after primary and revision TKA
{start}For walking limitations, 73% of those with moderate and 51% of those with severe pre-operative limitations, achieved mild or no walking limitation 2 years after primary TKA (Table 4). For stairs limitation, 49% with moderate pre-operative and 40% with severe pre-operative limitation achieved mild/no stairs limitation 2 years post-operative. For rising from chair, 88% with moderate pre-operative and 41% with severe pre-operative limitation achieved mild/no limitation 2 years post-operative (Table 4). At 5 years post-primary TKA, similar, but marginally lower improvements were noted (Table 4). Overall moderate-severe ADL limitation 2-year post-primary TKA was 22%.
Table 4.
Change in ADL limitations from pre-operative to 2 and 5 years post-primary TKA
| 2-year post-operative |
5-year post-operative |
|||||||
|---|---|---|---|---|---|---|---|---|
| None, % | Mild, % | Moderate, % | Severe, % | None, % | Mild, % | Moderate, % | Severe, % | |
| Walking limitations | ||||||||
| Pre-op none | 83.8 | 8.8 | 6.6 | 0.8 | 71.8 | 10.5 | 13.4 | 4.3 |
| Pre-op mild | 75.3 | 12.3 | 10.6 | 1.8 | 66.9 | 14.0 | 14.9 | 4.2 |
| Pre-op moderate | 57.9 | 15.4 | 22.1 | 4.6 | 51.1 | 13.1 | 26.5 | 9.4 |
| Pre-op severe | 38.0 | 13.2 | 31.5 | 17.3 | 30.6 | 15.8 | 33.2 | 20.3 |
| Stair limitations | ||||||||
| Pre-op none | 68.4 | 19.6 | 11.4 | 0.6 | 57.3 | 11.7 | 30.1 | 1.0 |
| Pre-op mild | 51.7 | 23.8 | 23.0 | 1.5 | 47.9 | 22.9 | 27.5 | 1.7 |
| Pre-op moderate | 35.3 | 23.8 | 38.9 | 2.0 | 31.7 | 23.0 | 41.9 | 3.5 |
| Pre-op severe | 23.3 | 16.2 | 52.4 | 8.1 | 24.4 | 20.8 | 45.7 | 9.1 |
| Rise from chair limitations | ||||||||
| Pre-op none | 64.6 | 32.7 | 2.7 | 0.0 | 56.8 | 37.6 | 5.2 | 0.3 |
| Pre-op mild | 47.2 | 47.6 | 5.0 | 0.2 | 42.6 | 49.8 | 7.4 | 0.2 |
| Pre-op moderate | 30.3 | 57.4 | 12.1 | 0.2 | 29.3 | 55.8 | 14.1 | 0.8 |
| Pre-op severe | 17.6 | 23.5 | 41.2 | 17.6 | 9.1 | 63.6 | 18.2 | 9.1 |
In the revision TKA cohort, 45% of those with moderate pre-operative walking limitation and 25% with severe pre-operative walking limitation reported mild/no post-operative walking limitation at 2 years (Table 5). Respective numbers were 36% and 20% for stairs limitation and 70% and 57% for rising from chair limitation at 2 years post-revision TKA. At 5 years post-revision TKA, similar but marginally lower improvements were noted (Table 5). Overall moderate-severe ADL limitation 2-years post-revision TKA was 46%.
Table 5.
Change in ADL limitation from pre-operative to 2 and 5 years post-revision TKA
| 2-year post-operative |
5-year post-operative |
|||||||
|---|---|---|---|---|---|---|---|---|
| None, % | Mild, % | Moderate, % | Severe, % | None, % | Mild, % | Moderate, % | Severe, % | |
| Walking limitations | ||||||||
| Pre-op none | 63.1 | 19.4 | 15.6 | 1.9 | 52.7 | 21.6 | 21.6 | 4.1 |
| Pre-op mild | 50.0 | 12.8 | 33.0 | 4.3 | 44.2 | 14.0 | 34.9 | 7.0 |
| Pre-op moderate | 29.0 | 16.0 | 42.3 | 12.7 | 35.6 | 11.2 | 36.2 | 17.0 |
| Pre-op severe | 19.5 | 5.7 | 39.8 | 35.0 | 12.5 | 10.9 | 37.5 | 39.1 |
| Stair limitations | ||||||||
| Pre-op none | 51.5 | 15.2 | 33.3 | 0.0 | 37.5 | 25.0 | 31.3 | 6.3 |
| Pre-op mild | 38.6 | 21.4 | 37.1 | 2.9 | 37.5 | 20.0 | 37.5 | 5.0 |
| Pre-op moderate | 14.6 | 20.9 | 57.5 | 7.1 | 14.4 | 19.6 | 61.6 | 4.4 |
| Pre-op severe | 10.7 | 9.5 | 56.0 | 23.8 | 6.1 | 6.1 | 55.1 | 32.7 |
| Rise from chair limitations | ||||||||
| Pre-op none | 40.8 | 50.7 | 8.5 | 0.0 | 38.3 | 51.1 | 10.6 | 0.0 |
| Pre-op mild | 24.3 | 57.8 | 17.6 | 0.3 | 24.6 | 58.7 | 16.8 | 0.0 |
| Pre-op moderate | 18.3 | 52.3 | 28.6 | 0.8 | 13.5 | 57.1 | 27.1 | 2.3 |
| Pre-op severe | 0.0 | 57.1 | 28.6 | 14.3 | 33.3 | 0.0 | 33.3 | 33.3 |
Change in overall ADL limitations after primary and revision TKA
In the primary TKA cohort, 3% with pre-operative no/mild pre-operative and 19% with pre-operative moderate/severe overall limitation had moderate/severe overall activity limitation 2 years post-operative. At 5 years, the respective proportions were 4% and 22%.
In the revision TKA cohort, 3% with pre-operative no/mild pre-operative and 32% with moderate/severe pre-operative severe overall limitation had moderate/severe overall activity limitation 2 years post-operative. At 5 years, the respective proportions were 4% and 34%.
Discussion
In this study, we described the prevalence of various degrees of index TKA pain severity and limitation in three key ADLs in a large cohort of patients with primary or revision TKA. We provided estimates of patient level improvements in patient-reported outcomes at the patient level rather than cohort level, which should be easily understandable and interpretable for patients and policy makers. A more accurate knowledge of expected improvements after TKA can help patients to have realistic expectations and reduce expectation–outcome mismatch, which is independently associated with poorer outcomes after TKA (lower pain, function and activity improvements and patient satisfaction) [21–23]. These data should serve as a resource for surgeons, patients and policy makers and an important educational tool for patients planning to undergo TKA. Several findings in this study deserve further discussion.
Consistent with the published literature, we found significant improvements in pain severity after TKA, with <1% patients with primary TKA and 3% with revision TKA reporting severe pain post-TKA. Moderate pain was reported by 7% and 8% at 2 and 5 years after primary TKA and 21% and 28% after revision TKA, respectively. Prevalence of moderate to severe index knee pain of 7% at 2 years post-primary TKA is similar to previous studies reporting 7–13% prevalence of poor pain outcome at 1 year [24, 25]. Our study also provided estimates of change in pain severity after primary and revision TKA for each category of pre-operative pain and ADL limitation, which can help address specific questions regarding patient improvements after TKA. For example, a patient with severe pre-operative knee pain can be reassured that 93% patients like him/her will have no/mild knee pain 2 years after primary TKA (Fig. S1, available at Rheumatology Online). Similarly, 66% of patients with severe pain before revision TKA can expect no/mild pain 2 years after revision TKA. Thus, our study provided estimates of change in pain from pre- to post-TKA.
Similarly, we found that important improvements occurred in ADLs in the vast majority of patients with TKA (Fig. S1, Tables S4 and S5, available at Rheumatology Online). Important ADL improvements were more remarkable for primary (vs revision) cohorts. We noted that at 2 years post-primary TKA, 0.3–6.1% patients had severe limitation in three key ADLs; at 5 years, ADL limitation was seen in 0.5–9.2% patients. In those with revision TKA, 1.3–14.3% had severe limitation of each ADL at 2 years and 1.8–19.7% at 5 years. The estimates of each ADL limitation post-operatively within each pre-operative category of ADL limitation should serve as useful resource for both patients and surgeons, especially when improvement in specific key ADL/s is a key goal for the patient undergoing TKA surgery. Detailed studies of functional improvements at the patient level that are meaningful to the patient are needed, since much younger patients now undergo TKA, for whom not only ADLs, but sports and leisure activities are also important [26–28].
An important observation in our study was that the frequency of severe pain and moderate to severe ADL limitation, was similar at 2 vs 5 years post-TKA, in both primary and revision cohorts. For example, among primary TKA patients with pre-operative moderate knee pain, 1% each reported severe index knee pain 2 and 5 years follow-up. Similarly, in primary TKA patients with pre-operative moderate to severe ADL limitation, 19% and 22% reported moderate to severe ADL limitation at 2 and 5 years post-TKA, respectively. This indicates that pain and functional improvements after TKA have maximized by 2 years, and very slight deterioration occurs between 2 and 5 years in these outcomes. Whether this holds true for pain and function outcomes at 10–15 post-TKA needs to be assessed by longer-term studies. Another observation was that a small proportion of patients undergoing primary TKA had mild pain (3%) pre-operatively; 90% of these patients had some activity limitation, which might explain why these patients underwent primary TKA. It is possible that in other settings, such as countries with national health care settings, for example UK, patients may have more pain and activity limitations at the time of undergoing TKA.
Our study has several strengths and limitations. Study strengths include a large cohort, prospective standardized data collection coordinated by dedicated clinical registry staff, analyses of data collected across a 13 year period, categorization of outcomes a priori and presentation of important improvements. Non-response bias may limit our ability to generalize these findings to other populations. Non-responders were more likely to be younger (characteristic associated with poorer pain outcome) [16] and more likely to be female and have higher comorbidity (associated with activity limitation in our previous study) [19]. Thus, non-response biased our estimates towards null, making our estimates conservative and the true differences would at least be as large or larger, had all eligible patients responded. However, the similarity of patient characteristics to those reported in TKA studies previously and our response rate being similar to that reported for large surveys [29] support the representativeness of our study sample. However, the lower response rate for 5-year post-revision TKA indicates that these results should be interpreted with caution. Our study was not designed to assess limitation in sports and leisure activities, important to younger patients, which should be done in future studies.
In summary, we studied pain and key ADL limitation at 2 and 5 years after primary and revision TKA in a large cohort. Our estimates of patient level important improvements in pain and ADL limitation should be useful for discussion with patients pre-operatively and help patients set realistic goals. This will allow patients to be well informed during the informed consent process and help them to objectively assess their post-TKA goals. Studies that provide longer-term data for important pain and ADL improvements and address sports and leisure activities are needed to provide the patients with a full spectrum of trajectory of pain and ADL improvement with primary and revision TKA to help them make a well informed decision for undergoing TKA.
Rheumatology key messages.
93% of patients with moderate to severe pre-operative pain have mild or no knee pain up to 5 years after primary total knee arthroplasty.
81% of patients with moderate to severe pre-operative overall limitation to activities of daily living have mild or no limitation 2 years after primary total knee arthroplasty.
70% of patients undergoing revision total knee arthroplasty report important pain reduction up to 5 years post-operatively.
Supplementary Material
Acknowledgements
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government. Study design and protocol: J.A.S.; review of study design: J.A.S., D.G.L.; data analyses: J.A.S.; review of analyses and results: J.A.S., D.G.L.; manuscript draft: J.A.S.; manuscript revision: J.A.S., D.G.L.; submission: J.A.S. This study was supported by resources from and use of facilities at the Birmingham VA Medical Center, Alabama, USA.
Funding: This study received research funding from the Department of Orthopaedic Surgery at the Mayo Clinic.
Disclosure statement: J.A.S. has received research grants from Takeda and Savient and consultant fees from Savient, Takeda, Ardea, Regeneron, Allergan, URL pharmaceuticals and Novartis. J.A.S. is a member of the executive of OMERACT, an organization that develops outcome measures in rheumatology and receives arms-length funding from 36 companies; a member of the American College of Rheumatology's Guidelines Subcommittee of the Quality of Care Committee; and a member of the Veterans Affairs Rheumatology Field Advisory Committee. D.G.L. has received royalties from Zimmer, has been a paid consultant and owns stock in Pipeline Biomedical and Ketai Medical Devices, Ltd. His institution has received research funds from DePuy, Stryker, Biomet and Zimmer.
Supplementary data
Supplementary data are available at Rheumatology online.
References
- 1.Ethgen O, Bruyere O, Richy F, et al. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004 doi: 10.2106/00004623-200405000-00012. 86-A:963–74. [DOI] [PubMed] [Google Scholar]
- 2. HCUP. HCUP. Facts and Figures 2009—Section 3: Inpatient Hospital Stays by Procedure. Exhibit 3.1 Most Frequent All-listed Procedures. http://hcup-us.ahrq.gov/000orts/factsandfigures/2009/pdfs/FF_2009_section3.pdf. In (30 September 2013, data last accessed)
- 3.Biring GS, Masri BA, Greidanus NV, et al. Predictors of quality of life outcomes after revision total hip replacement. J Bone Joint Surg Br. 2007;89:1446–51. doi: 10.1302/0301-620X.89B11.19617. [DOI] [PubMed] [Google Scholar]
- 4.Singh JA, Lewallen D. Predictors of pain and use of pain medications following primary total hip arthroplasty (THA): 5,707 THAs at 2-years and 3,289 THAs at 5-years. BMC Musculoskelet Disord. 2010;11:90. doi: 10.1186/1471-2474-11-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–5. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 6.Beswick AD, Wylde V, Gooberman-Hill R, et al. What proportion of patients report long-term pain after total hip or knee replacement for osteoarthritis? A systematic review of prospective studies in unselected patients. BMJ open. 2012;2:e000435. doi: 10.1136/bmjopen-2011-000435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Insall JN, Dorr LD, Scott RD, et al. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989:13–4. [PubMed] [Google Scholar]
- 8.Ranawat AS, Rossi R, Loreti I, et al. Comparison of the PFC sigma fixed-bearing and rotating-platform total knee arthroplasty in the same patient: short-term results. J Arthroplasty. 2004;19:35–9. doi: 10.1016/j.arth.2003.08.010. [DOI] [PubMed] [Google Scholar]
- 9.Sheng P, Lehto M, Kataja M, et al. Patient outcome following revision total knee arthroplasty: a meta-analysis. Int Orthop. 2004;28:78–81. doi: 10.1007/s00264-003-0526-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singh J, Sloan JA, Johanson NA. Challenges with health-related quality of life assessment in arthroplasty patients: problems and solutions. J Am Acad Orthop Surg. 2010;18:72–82. [PMC free article] [PubMed] [Google Scholar]
- 11.Singh JA, Lewallen DG. Patient-level clinically meaningful improvements in activities of daily living and pain after total hip arthroplasty: data from a large U.S. Institutional registry. Arthritis Res Ther. 2013 doi: 10.1093/rheumatology/kes416. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rand JA, Ilstrup DM. Survivorship analysis of total knee arthroplasty. Cumulative rates of survival of 9200 total knee arthroplasties. J Bone Joint Surg Am. 1991;73:397–409. [PubMed] [Google Scholar]
- 13.Rand JA, Trousdale RT, Ilstrup DM, et al. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. 2003;85-A:259–65. doi: 10.2106/00004623-200302000-00012. [DOI] [PubMed] [Google Scholar]
- 14.McGrory BJ, Morrey BF, Rand JA, et al. Correlation of patient questionnaire responses and physician history in grading clinical outcome following hip and knee arthroplasty. A prospective study of 201 joint arthroplasties. J Arthroplasty. 1996;11:47–57. doi: 10.1016/s0883-5403(96)80160-4. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 16.Singh JA, Gabriel SE, Lewallen DG. Higher body mass index is not associated with worse pain outcomes after primary or revision total knee arthroplasty. J Arthroplasty. 2011;26:366–74. doi: 10.1016/j.arth.2010.02.006. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Singh JA, O'Byrne MM, Colligan RC, et al. Pessimistic explanatory style: A psychological risk factor for poor pain and functional outcomes two years after knee replacement. J Bone Joint Surg Br. 2010;92:799–806. doi: 10.1302/0301-620X.92B6.23114. [DOI] [PubMed] [Google Scholar]
- 18.Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466:2717–23. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Singh JA, O'Byrne MM, Harmsen WS, et al. Predictors of moderate-severe functional limitation 2 and 5 years after revision total knee arthroplasty. J Arthroplasty. 2010;25:1091–5. doi: 10.1016/j.arth.2009.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh JA, O’Byrne M, Harmsen S, et al. Predictors of moderate-severe functional limitation after primary total knee arthroplasty (TKA): 4701 TKAs at 2-years and 2935 TKAs at 5-years. Osteoarthr Cartil. 2010;18:515–21. doi: 10.1016/j.joca.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gonzalez Saenz de Tejada M, Escobar A, Herrera C, et al. Patient expectations and health-related quality of life outcomes following total joint replacement. Value Health. 2010;13:447–54. doi: 10.1111/j.1524-4733.2009.00685.x. [DOI] [PubMed] [Google Scholar]
- 22.Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol. 2002;29:1273–9. [PubMed] [Google Scholar]
- 23.Mancuso CA, Salvati EA, Johanson NA, et al. Patients' expectations and satisfaction with total hip arthroplasty. J Arthroplasty. 1997;12:387–96. doi: 10.1016/s0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- 24.Brander VA, Stulberg SD, Adams AD, et al. Predicting total knee replacement pain: a prospective, observational study. Clin Orthop Relat Res. 2003:27–36. doi: 10.1097/01.blo.0000092983.12414.e9. [DOI] [PubMed] [Google Scholar]
- 25.Elson DW, Brenkel IJ. Predicting pain after total knee arthroplasty. J Arthroplasty. 2006;21:1047–53. doi: 10.1016/j.arth.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 26.McGrory BJ, Stuart MJ, Sim FH. Participation in sports after hip and knee arthroplasty: review of literature and survey of surgeon preferences. Mayo Clin Proc. 1995;70:342–8. doi: 10.4065/70.4.342. [DOI] [PubMed] [Google Scholar]
- 27.Felts E, Parratte S, Pauly V, et al. Function and quality of life following medial unicompartmental knee arthroplasty in patients 60 years of age or younger. Orthop Traumatol Surg Res. 2010;96:861–7. doi: 10.1016/j.otsr.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Williams DH, Greidanus NV, Masri BA, et al. Predictors of participation in sports after hip and knee arthroplasty. Clin Orthop Relat Res. 2012;470:555–61. doi: 10.1007/s11999-011-2198-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50:1129–36. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


