Abstract
Background:
Telenursing includes every nursing and care-giving services conducted remotely. In telenursing, telephone as a device, which is available for most of the people, is being used increasingly. In a telephone-based system, patients are being contacted by health care providers on regular bases and they would be provided with some information about their illness and their treatment method.
This study was conducted to determine the effect of phone-based follow-ups on diabetes patients’ metabolic control in the city of Kerman in Iran.
Materials and Methods:
This is a quasi-experimental study conducted on 50 type II diabetes patients in Kerman during 2011. Data were collected using a demographic questionnaire and also by taking physiological measurement of fasting blood suger (FBS), Glycated Hemoglobin (HbA1c), and postprandial glucose (PPG). Participants’ body mass index (BMI) was calculated by measuring height and weight. Patients completed the questionnaire at the beginning of the study and 12 weeks later. The patients were randomly divided into two groups of experiment and control. Patients in the experimental group received phone calls by the researcher for 12 weeks, and the follow-ups included instructions on self-care and advices to follow their diets, exercise, and insulin titration.
Data analysis was done using descriptive and inferential statistical methods (chi-square, analysis of variance [ANOVA], independent t-test, and paired t-test).
Results:
The decrease of HbA1c and PPG was significantly more in the intervention group compared with the controls (P < 0.001). However, there was no significant difference between the mean of FBS (P = 0.42), and BMI (P = 0.31) in both groups after the intervention.
Conclusions:
According to the results of this study, telenursing was able to improve the metabolic indices of the patients. Therefore, using this method is recommended for patients with type II diabetes.
Keywords: Body mass index, diabetes mellitus Type II, Iran, metabolic control, telenursing
INTRODUCTION
Diabetes mellitus is a metabolic disorder that is characterized by chronic hyperglycemia along with impaired metabolism of proteins, carbohydrates, and fats resulted from defects in insulin secretion or function; it would hurt different organs of the patients and may decrease his/her lifetime.[1] Diabetes is a major and growing problem in all age groups.[2] This disease is the most common endocrine disease and more than 140 million people in the world suffer from it. The prevalence of diabetes in all countries, especially in the developing countries, is increasing, so that it can be called the most important challenge of health care in the 21st century.[3] It is estimated that until 2030, about 366 million people in the world will be suffering from this disease.[4] In Iran, based on the existing statistics, more than 2 million people suffer from diabetes.[3] Growing trend of aging, economical–social transitions, and demographic changes (like the increasing prevalence of obesity) have turned diabetes into a global problem.[5] Therefore, diabetes must be considered as a priority.
Type II diabetes emerges in higher ages (more than 30 years old) and is associated with overweight. This is the most common form of the disease and about 90-95% of patients suffer from this.[3] The chronic nature of this disease and its complications is a big financial burden for patients and their families.[6] Studies have shown that control of blood sugar at the normal rate reduces the progress of microvascular and neuropathic complications to 50% in type II diabetes.[7]
Analysis of the United Kingdom Prospective Diabetes Study (UKPDS) has shown a relationship between hyperglycemia and microvascular complications, so that 1% reduction in HbA1c decreases about 37% incidence of microvascular complications.[8] Considering the high prevalence of diabetes in the world and in Iran and the incidence of short-term and long-term complications and direct and indirect costs of treatment for these complications, it is important to pay attention to various dimensions of care for these patients.[9] Diabetes is not curable, but it is controllable.[10] Most studies have suggested that all patients with diabetes mellitus should participate in an educational program with structured follow-ups to control their metabolism.[11]
Educational program for diabetes patients have various methods. One of the most efficient supportive methods, which effectiveness is proved in solving patients’ problems, is distanced follow-ups, in which the caregiver provides real and correct information for the patients.[12] Nowadays, nurses use telenursing for all processes of nursing including assessment, planning, intervention, and evaluation of the results of their nursing cares.[13] Telenursing includes all kinds of nursing care and services that can be provided from distance and includes a wide range of communication technologies such as phone, fax, email, internet, and video clips to overcome the time and distance obstacles to provide better nursing care.[14] Among these devices, phone calls are frequently used in telenursing as telephone is accessible for majority of people in the society.[15] In calling system, patients receive calls from health care personnel in a periodical basis and get advices on their treatment and educational information[16] and it is especially useful for diabetes patients who have problems of far distance to the health care clinics or need a long time waiting for visiting a doctor.[17]
Reviewing the studies conducted on telenursing, it can be concluded that this method has positive effectiveness on the treatment of chronic illnesses but it must be studied more from different dimensions. In recent years, there has been studies on providing care by phone calls in other countries and the results show that this technology has caused less hospitalization and has reduced nursing visits to patients’ houses in chronic diseases such as chronic obstraction pulmonary disease (COPD), diabetes, congestive heart failure (CHF).[18] A few studies have also been conducted in Iran that show the positive effect of follow-ups on the improvement of patient care. In a study by Moqaddam et al., results showed that type II diabetes patients followed their diets better due to nurses’ phone calls.[15] In a study by Sadeqi et al. and Nethari et al., nurses’ follow-ups by phone calls was also effective on the rate of glycosylated hemoglobin and there was a significant difference between the two groups[12,19] and this system also improved the social functioning and self-efficiency and communication with health care staff.[20]
Considering the supportive and care-giving roles of nurses,[9] and the American Diabetes Association's (ADA's) recommendation that all diabetes patients should try to keep their blood sugar in the normal level,[21] it is necessary to follow-up the condition of these patients. Considering the increasing rate of diabetes incidence and the lack of care-giving personnel, it is necessary to develop new methods to make nursing services more effective. It seems that telenursing as a follow-up caring technology[16] can be helpful in achieving this goal. Although there has been studies that have confirmed the positive effect of telenursing, but for turning this method into a standard process, more studies are needed. In contrast, conducting the study in different cultural and geographical areas can discover more facts that are based on local cultures of each area. Therefore it seemed that conducting a study on effectiveness of phone follow-ups on glycemic control and BMI in type II diabetes patients of the city of Kerman would help reaching this goal.
MATERIALS AND METHODS
This is a quasi-experimental study on type II diabetes patients in the city of Kerman in 2011. This study is considered quasi-experimental because it was conducted on human samples and the researchers could not reach all the experimental criteria like those in a laboratory. Entry criteria included having a landline, no talking or hearing disorder, age less than 75 years, HbA1c more than 7%, being able to conduct self monitoring of blood glucose (SMBG), no known psychological disorder or advanced critical illness. Exclusion criteria included severe cardiovascular diseases and uncontrolled high blood pressure and hospitalization during the study. The sample size was calculated to be 40 patients based on the study of Moqaddam et al.; using the following formula:
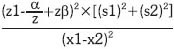
where S1 is the difference between minimum averages of HbA1C in both groups and is equal to 1.87; S2 is the standard deviation of the measured HBA1C and is equal to 7.04; and with 99% confidence and 95% power of the test. However, considering the possibility of drop offs, a total of 50 patients (25 for the experimental group and 25 controls) were selected based on availability.
Data were collected using a demographic questionnaire and also by taking physiological measurement of FBS, HbA1c, and PPG. The questionnaire had two sections, first section included 11 demographic questions and the second section included 12 questions about disease's features, which were completed by patients. Since the questionnaires were as check lists and included completely objective questions, they were considered valid and reliable. Patients completed the questionnaire at the beginning of the study and 12 weeks later using written self-reports; also physiologic measurements were conducted to assess FBS, HbA1c, and PPG. After contacting and registering the participants, they were informed of the study method and the fact that they could leave the study at any time; then an informed written consent was obtained from them.
After they completed the questionnaire, their height was measured using the standard meter and their weight was measured using a digital SECA (Model 769 and accuracy ±100 g) scale to calculate BMI. Their blood samples were collected for FBS and HbA1c tests. Then breakfast was distributed among them and afterward their blood samples were again obtained for PPG test. HbA1c tests in this study were conducted using automatic method of chromatography with a natural limit of 3.6-5.4%. FBS and PPG measurements were conducted using photometric method by a RA1000 device in a laboratory in the city of Kerman. The natural limit of FBS for adults is 70-110 mg/dl.
All volunteers received instructions of self-care for diabetes by an instructor of Gabric Diabetes Association and a professional dietitian and also received educational pamphlets including definition of diabetes, risk factors, treatment regimen, the management and treatment of hypoglycemia, and self-measurement of blood glucose to match the two groups regarding information about the disease. After that, the patients were randomly divided into two groups of experiment and control based on random numbers table. Patients in the experiment group received phone calls by the researcher for 12 weeks, and the follow-ups included instructions on self-care and advices to follow their diets, exercise and insulin titration, taking care of their feet, and advice on SMBG. The calls were regular for two times per week in the first month and then once a week in the second and third months and averagely it was 16 times for every patient during the study. The length of the call was considered 12 minutes per call. The calls and the contents of conversation, number of calls and duration was recorded in a special form. Since criterion for adequate control of blood glucose is HbA1C (when blood sugar increases glucose molecules would attach to red blood cells’ hemoglobin), and its measurement shows the average of blood glucose concentration in a period of 2-3 months; therefore the patients of the intervention group were followed up for 12 weeks. During the intervention, control group received no intervention. The patients in the both groups were called in for repeating the tests and measuring their MBI after 3 months and the above mentioned processes were conducted all over again.
Data analysis was performed by SPSS version 15 using chi-square, Fisher's exact test, independent t–test, and paired t-test statistical tests.
RESULTS
Patients in the both groups of the study were aged from 30 to 75 years, from both sexes (male and female) and they were matched in demographic data (age, sex, BMI, marital status, education, job status, and monthly income) and disease features [Table 1]. There was no significant difference between HbA1c, FBS, and PPG of the both groups (intervention and control) before the intervention [Table 2]. Before the intervention, the mean (SD) of HbA1c was 9.98 (1.34) in the intervention group and 9.38 (1.53) in the control group (P = 0.14). After the intervention, HbA1c level reduced to 8.15 (0.97) in the intervention group and to 9.14 (1.59) in the control group (P < 0.001). Independent t-test showed that there was a significant difference between HbA1c level of both groups before and after the intervention (P < 0.001) [Table 2]. In addition, paired t-test showed that the difference between HbA1c level of the intervention group's patients before and after the intervention was statistically significant (P < 0.001) while this difference was not significant in the control group (P = 0.07). There was no significant difference between FBS (P = 0.37) and PPG (P = 0.64) of both groups before the intervention.
Table 1.
Disease Profile in the two groups of intervention and control before the intervention
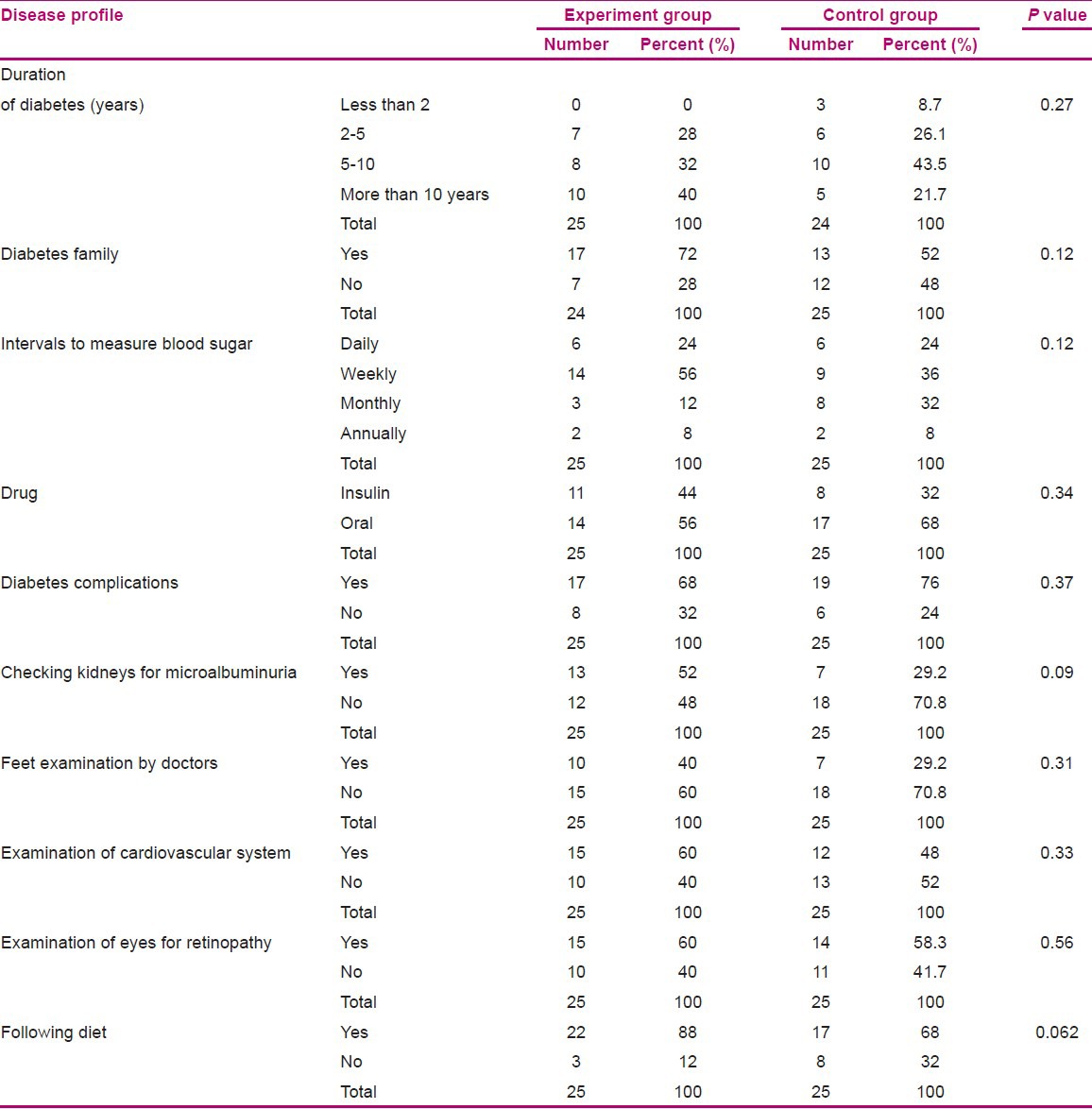
Table 2.
Measured blood indices and BMI before and after intervention in the two groups of experiment and control
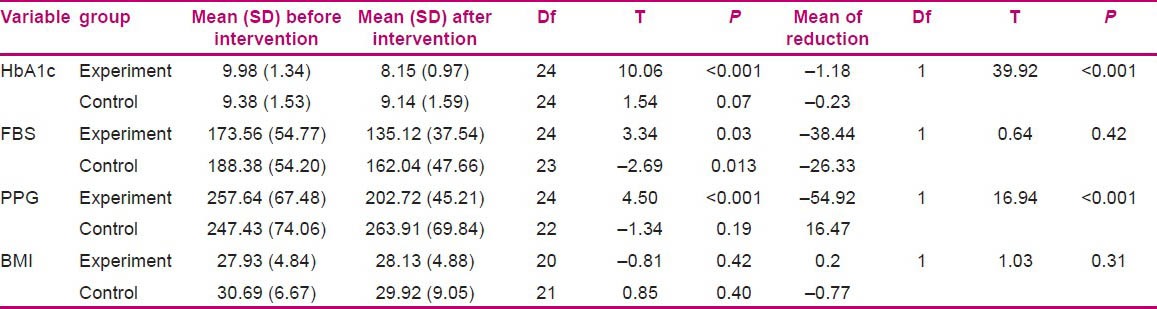
After the phone follow-ups, the mean reduction of FBS was 38.44 mg/dl in the intervention group, which was not significantly different from the mean reduction of FBS in the control group, which was 26.33 mg/dl (P = 0.42). The mean of PPG of the intervention group was 54.92 mg/dl reduced, but in the control group, an increase of 16.47 mg/dl was seen. The difference between the two groups was significant (P = 0.000) [Table 2]. Independent t-test (t = −1.56) showed that there was no significant difference between the BMI of the two groups before the intervention (P = 0.12).
During the 3 month period, the average of BMI in the intervention group had a 0.2 m2/kg increase, but there was a 0.77 m2/kg decrease in the control group; independent t-test showed that there was no significant difference between the average of BMI in both groups after the intervention (t = 1.03, P = 0.31).
DISCUSSION
The results of this study showed that the two groups of control and intervention were matched before the intervention regarding demographic data, disease features, and the main variables of the study, including HbA1C, FBS, PPG, and BMI. After the intervention, metabolism control of the experiment group was significantly improved as compared with the controls. The two groups showed significant difference in HbA1C and PPG, while FBS showed no significant difference between the two groups.
In this study, HbA1C of the experiment group decreased 1.83% after 12 weeks of intervention. In contrast, the decrease in the controls was 0.23%. These findings approve the results of the study of Kim and Oh after 12 weeks of follow-ups with phone calls. In another study, also, that was conducted to find the effectiveness of follow-ups with phone calls on HbA1C of the type II diabetes patients, the decrease of HbA1C was reported as 1.7%.[22] Results of other studies also approve these finding that follow-ups with phone calls can affect the level of HbA1C[12,19] and can also affect following diet.[15] The relationship between HbA1C and risk of micro vascular complications in type II diabetes is proved by UKPDS and it is known that glycemic control reduces the risk of neuropathic and micro vascular complications.[8]
In this study, no significant difference was seen between the FBS of the two groups after the intervention. This finding is in agreement with the results of Kim and Oh. Since the main criteria to control blood sugar for both group of patients was FBS and since the patients are aware of the sampling for FBS one day ahead, both groups further controlled their FBS for the test and it can explain the insignificant difference. Both groups of patients had FBS higher than 120 mg/dl after the intervention, which shows that most patients cannot reach a FBS under this number, which is the goal. Therefore, it is necessary to give care and constant education to such patients.[7]
There was a decrease in the PPG of the experiment group, which was increased in the controls. The difference between PPG of the two groups was significant and this finding was not in agreement with the study in Korea. However, the Korean study reported no significant difference in the mean of PPG decrease, while the PPG of the controls increases to 6.19 mg/dl and in the experiment group decreased to 6.42 mg/dl. The authors provided the following points to explain their results: first, most patients knew nothing about the importance of appropriate control of PPG and second, patients usually measured their FBS in SMBG and at the time of PPG measurement, they were at work.
The increase of PPG is associated with the incidence of macro-vascular and micro-vascular complications. Therefore, in the follow-ups with phone calls, it was tried to explain the importance of this issue for the experiment group and patients got interested to conduct SMBG and report it to researchers. Then according to these reports, they received advices of regulating insulin or following special diets from professional doctors. This may be the reason for the control of PPG. There was an increase in the PPG of controls, which means health care team should educate patients about the importance of proper control of PPG to reduce diabetes complications. Unlike old times when diabetes patients would visit doctors to control their PPG, in this study the patients were educated through phone conversation the importance of PPG and how to measure it and then according to the results, medications were prescribed. Informing and activating patients about their disease were features of this study.
The results of the present study showed that the mean of BMI increased in the intervention group (0.2 kg/m2), while the controls showed a decrease of 0.77 kg/m2. There was no statistically significant difference between the two groups and these results were similar to those of Kim and Oh and Wong et al.[23] It should also be mentioned that to reduce the BMI, more time and care and education about losing weight are needed. However, this study showed that this method has no significant effect on BMI and it is possible that the time considered in the study is not enough for this purpose.
CONCLUSION
The results of this study proved that using telenursing for follow-ups has positive effects on metabolism control and HbA1C and can improve it in 12 weeks.
The results also showed that phone follow-ups can improve the process of self-care and the control of Glycemic index in patients with type II diabetes. It seems that this happens because of the increased roles of the patient in taking care of themselves; the patients have discovered a new kind of relation and training and their motivation for taking care of themselves and contacting with health providers has increased. Therefore telenursing could be programmed as a part of health plan for patients with type II diabetes.
Phone call follow-ups have a good role in clinic centers especially for patients with chronic diseases. This method as compared with other methods of follow-up is easier and more accessible and less costly for patients with type II diabetes who are mostly in the middle age or elderly. Phone call follow-up can decrease the frequency of patients visit to clinics and medical expenses. It can also cover many patients in a wide geographical area with health care they need and therefore, reduces the expenses of human resources and time and energy in health care systems.
In total, just one patient dropped out of the study due to moving to another city.
ACKNOWLEDGMENT
This study was conducted by the support of HSR in the Research Deputy of the Kerman University of Medical Sciences. The authors thank the authorities of the university as well as the staff in the diabetes centers of Shahid Bahonar Hospital in Kerman and the associated laboratory. The authors also thank all the patients who helped them in conducting this study.
Recommendation: Further studies can develop the application of telenursing in providing care for many patients with chronic diseases.
Footnotes
Source of Support: HSR in the Research Deputy of the Kerman University of Medical Sciences
Conflict of Interest: None declared.
REFERENCES
- 1.American Diabetes Association (ADA). Standards of medical care in diabetes V. Diabetes Care. 2008;31(Suppl 1):16–24. [Google Scholar]
- 2.Scottish I. Management of diabetes. Natl Clin Guidel. 2001;82:1–3. [Google Scholar]
- 3.Hadi H. Tehran: Chapkhsh; 2007. Diabetes› treatment. [Google Scholar]
- 4.Fonseca AV, Pendergrass M. London: Current Medicine Group; 2008. Hand book of Diabetes; p. 4. [Google Scholar]
- 5.Peymani M, Tabatabaie A, Pajoohi M. Role of nursing in care of diabetes. Iran J Diabetes Lipid. 2009;9:107–15. [Google Scholar]
- 6.Nagelkerk J, Reick K, Meengs L. Perceived barriers and effective strategies to diabetes self — management. J Adv Nurs. 2006;54:151–8. doi: 10.1111/j.1365-2648.2006.03799.x. [DOI] [PubMed] [Google Scholar]
- 7.Oh JA, Kim H, Yoon K, Choi E. A Telephone-Delivered intervention to improve G Glycemic control in type 2 Diabetic patient. Yonsei Med J. 2003;44:1–8. doi: 10.3349/ymj.2003.44.1.1. [DOI] [PubMed] [Google Scholar]
- 8.United Kingdom Prospective Diabetes Study Group (UKPDS). Intensive blood- glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–53. [PubMed] [Google Scholar]
- 9.Moqaddasian S, Ebrahimi H, Mehdi pour N, Hariryan H. The three dimensions of quality of life of patients referring to Diabetes Center of Tabriz University of Medical Sciences. J Nurs Midwifery. 2008;10:38–44. [Google Scholar]
- 10.Phipps WJ, Monahan FD, Sands JK, Marek JF, Neighbors M. St.Louis: Mosby; 2003. Medical-surgical nursing: Health and illness perspectives. [Google Scholar]
- 11.Braun A, Samann A. Effects of metabolic control, patient education and initiation of insulin therapy on the quality of life of patients with type 2 diabetes mellitus. Patient Educ Couns. 2008;73:50–9. doi: 10.1016/j.pec.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Sadeqi T, Shahabi Nejad M, Derakhshan R, Balaie P. The effectiveness of phone call follow-ups by nurses on the level of HbA1c in diabetic patients. J Rafsanjan Univ Med Sci. 2010;3:175–84. [Google Scholar]
- 13.Health Resources and Services Administration. What is telehealth? [Last accessed on 2007]. Available from: http://www.hrsa.gov/telehealth .
- 14.Jones J, Tschirch P. Nurse leader. Galveston: Mosby; 2006. Nursing and Tele health. [Google Scholar]
- 15.Zakeri Moqaddam M, Basampour S, Rajab A, Faghieh Zade S, Nethari M. Journal of the Faculty of Nursing and Midwifery. Vol. 2. Iran: Tehran University of Medical Sciences (Hayat); 2008. The effectiveness of phone call follow-ups by nurses on diet of patients with type II diabetes; pp. 63–71. [Google Scholar]
- 16.Bellazzi R, Larizza C, Montani S, Riva A, Stefanelli M, d›Annunzio G, et al. A telemedicine support for diabetes management: The T-IDDM project. Comput Methods Programs Biomed. 2002;96:147–61. doi: 10.1016/s0169-2607(02)00038-x. [DOI] [PubMed] [Google Scholar]
- 17.Chumbler N, Neugaard B, Kobb R. An observational study of veterans with diabetes receiving weekly or daily home tele health monitoring. J Telemed Telecare. 2005;11:150–6. doi: 10.1258/1357633053688723. [DOI] [PubMed] [Google Scholar]
- 18.Meyer M, Kobb R, Ryan P. Virtually healthy: Chronic disease management in the home. Dis Manag. 2002;5:87–94. [Google Scholar]
- 19.Nethari M, Zakeri Moqaddam M, Rajab A, Faghieh Zade S, Bassam Pour S, Rahmani M. The effectiveness of phone call follow-ups by nurses on controlling blood sugar and fat in patients with type II diabetes. Iran J Diabetes Lipid. 2008;8:115–22. [Google Scholar]
- 20.Gomez E, Hernando M, Garcia A. Telemedicine as a tool for intensive management of diabetes: The DIABTel experience. Comput Methods Programs Biomed. 2002;69:163–77. doi: 10.1016/s0169-2607(02)00039-1. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Standard of Medical Care for patients with diabetes mellitus care. Diabetes Care. 2007;30:4–41. [Google Scholar]
- 22.Piette JD, Kraemer FB, Weinberger M, McPhee SJ. Impact of automated calls with nurse follow-up on diabetes treatment outcomes in a department of veterans Affairs health care system. Diabetes Care. 2001;24:202–8. doi: 10.2337/diacare.24.2.202. [DOI] [PubMed] [Google Scholar]
- 23.Wong F, Mok M, Chan T, Tsang M. Nurse follow up of patient with diabetes: Randomized controlled trial. J Adv Nurs. 2005;50:391–402. doi: 10.1111/j.1365-2648.2005.03404.x. [DOI] [PubMed] [Google Scholar]


