Abstract
Background:
Vaccination is one of the most common painful procedures in infants. The irreversible consequences due to pain experiences in infants are enormous. Breast feeding and massage therapy methods are the non-drug methods of pain relief. Therefore, this research aimed to compare the vaccination-related pain in infants who underwent massage therapy or breast feeding during injection.
Materials and Methods:
This study is a randomized clinical trial. Ninety-six infants were allocated randomly and systematically to three groups (breast feeding, massage, and control groups). The study population comprised all infants, accompanied by their mothers, referring to one of the health centers in Isfahan for vaccination of hepatitis B and DPT at 6 months of age and for MMR at 12 months of age. Data gathering was done using questionnaire and checklist [neonatal infant pain scale (NIPS)]. Data analysis was done using descriptive and inferential statistical methods with SPSS software.
Results:
Findings of the study showed that the three groups had no statistically significant difference in terms of demographic characteristics (P > 0/05). The mean pain scores in the breast feeding group, massage therapy, and control group were 3.4, 3.9, and 4.8, respectively (P < 0.05). Then the least significant difference (LSD) post hoc test was performed. Differences between the groups, i.e. massage therapy and breast feeding (P = 0.041), breast feeding group and control (P < 0.001), and massage therapy and control groups (P = 0.002) were statistically significant.
Conclusion:
Considering the results of the study, it seems that breast feeding during vaccination has more analgesic effect than massage therapy. Therefore, it is suggested as a noninvasive, safe, and accessible method without any side effects for reducing vaccination-related pain.
Keywords: Breast feeding, Iran, massage therapy, pain, vaccination
INTRODUCTION
One of the most common painful interventions in infants is vaccination.[1] About 100 million infants are yearly vaccinated.[2] Pain can cause short- and long-term effects in infants. Generally, vaccination complications include an increase in secretion of hormones and substances, experience of a painful event, pain sensitivity, and lower pain threshold,[3] increased behavioral and physiologic responses to pain, increased neural disorders, psychosocial problems, learning disorders, poor adaptive behavior, future fear of injection, and long-term complications in brain development.[4] It was believed in the past that neonates and infants did not feel any pain, while numerous studies showed that they feel more pain compared to children and adults.[5] Researchers believe that human beings are able to feel pain physiologically and anatomically in the fetal period, and infants, contrary to the adults, remember the pain of painful events and manifest a more acute reaction to next vaccinations.[6] Although pain transmission pathways have been thoroughly developed during infancy, pain inhibiting systems do not have adequate growth.[7] On the other hand, limited cognitive abilities, lack of verbal and psychological skills, and constant changes occurring in infants are among the major challenges at this period of life. Therefore, evaluation and reduction of vaccination pain among infants are of great importance. As vaccination is essential for promotion of children's health, the infants have to experience pain in their very early life and inevitably face painful procedure of vaccination which causes them unpleasant mental and psychological effects.[8] Therefore, a method with the lowest number of complications and the highest effect should be used to relieve their pain. Nowadays, major steps have been taken toward pain management, including various medical methods.[3] In the medical methods, medications such as narcotics (morphine), sedatives (acetaminophen), and local analgesics (lidocaine) are used.[9] Some effective non-medical methods to manage pain include cryotherapy, acupressure, distraction, and music therapy.[10] Medical methods are rarely used in infancy due to their side effects like skin rashes and irritations, while non-medical pain relief methods have not only numerous advantages including lack of side effects and interference with vaccination, but a pleasant effect on infants as well.[11] Sujok is one of the non-medical treatment schools. “Su” in Korean means “palm” and “jok” means “sole.” This school of medicine has worked on various methods to activate adaptive palms/soles systems and their effect in the treatment of diseases and pain, based on a comprehensive system of physical and metaphysical mechanisms.[12] In this school of treatment, the palms and soles represent a small mirror image of the human body as a whole. Sujok employs various methods to stimulate pain points,[13] including massaging specific points of palms and soles, which have been used to relieve pain in their related organs in some cultures for hundreds of years.[14] Massage therapy is, in fact, a practical art based on touching which is applied by manual and structured techniques on superficial soft tissue of the skin, muscles, tendons, ligaments, and fascia. Massage increases endorphins and serotonin hormone secretions which lead to a relaxing condition and a pleasant experience in individuals.[15] Abassi et al. (2007) studied the association between the effect of massage and vaccination pain in 60 infants during their vaccination and reported mean pain scores of 3.05 ± 0.13 and 5.03 ± 0.03 in the study and control groups, respectively. Their results revealed that massage therapy reduced vaccination pain.[16] Another non-medical method to manage pain among infants is mothers’ breast feeding which has a pain-relieving effect on repetitive, short, and acutely painful events.[1]
Breast feeding reduces the pain experienced by the infants from painful procedures, as the infants get distracted while sucking and experience a relaxed condition due to their skin-to-skin contact with their mothers.[17,18]
Codipietro et al. (2007) reported that the effect of mothers’ breast feeding on relieving pain experienced due to taking blood sample from infants’ heel was more than the effect of oral sucrose in term infants.[19] Taavoni et al. (2008) also showed that infants’ breast sucking was effective on causing pain relief from vaccination in 2-4 month old infants.[20] Due to the numerous complications of pain in vaccination, which is a painful procedure in infants, and lack of a study on the effect of sujok massage on vaccination pain on the one hand, and application of massage therapy and breast feeding as convenient, noninvasive, and cost-effective methods, on the other, the researcher conducted the present study to compare vaccination pain in these two non-medical methods in 6-12 month old infants, in order to suggest an efficient and complication-free pain management strategy to provide these little infants, suffering from pain, with more emotional psychological and physical health.
MATERIALS AND METHODS
This was a randomized clinical trial conducted on 96 infants in Navabsafavi Health Care Center in Isfahan during April — July 2011. The study population comprised all infants, accompanied by their mothers, referring to the center for vaccination of hepatitis B and DPT at 6 months of age and for MMR at 12 months of age. The inclusion criteria were: normal weight, breast feeding, and no consumption of any medications except complements by infants, regular and in-time referrals of the mothers for the ongoing and former vaccinations, lack of any diseases, Iranian nationality, and lack of any lesions on infants’ thighs preventing vaccination. If the infant was crying before vaccination and the mother could not calm the infant or the infant had an open wound in his/her palms or soles, the infant was excluded from the study. After obtaining the necessary permissions from the university authorities and consent from the mothers to attend the study, the subjects were randomly assigned to three groups of 32 subjects each. To make the condition equal for the subjects in all groups, vaccination was conducted with the same staff with quite similar equipments and under identical conditions. To omit the confounding factor of staff's haste or rough behavior to some extent, the researcher stayed by the infants, talked to them and touched them. Vaccination was conducted when the infants were hugged by their mothers (hugging position) in all three groups. In the control group, vaccination was conducted in the conventional method with no intervention. In the mother's breast feeding group, the mother started breast feeding the infant and vaccination was conducted during active and constant sucking. In the massage therapy group, the researcher massaged the first knuckle of the middle or ring finger of the infants’ palm or sole of the injection side for 60 sec and finally vaccinated the subject.[13] The massaged point was corresponding with the injection-related leg in the body through sujok correspondence system in which the points are on a miniature map of the body on the palms and soles. Next, neonatal infant pain scale (NIPS) checklist, which is a standard tool to measure pain with its validity and reliability having been confirmed,[1,21] was ticked in all groups by a co-researcher through observing the subjects during the procedure of vaccination. The subjects and the co-researcher who played a key role in data collection did not know about the purpose of the study.
Pain intensity was measured by a behavior scale based on infants’ grimace, cry, respiration pattern, positions of arms and legs, and infants’ consciousness. In this scale, the lowest pain score is zero and the highest is 7, and score 3 shows the existence of pain.[1] It should be indicated that to make vaccination identical in all groups, infantile paralysis vaccine was given after all other vaccines, and in case of some concurrent injections, pain intensity was measured only for the first injection. The type of vaccine to be investigated was randomly selected from 96 envelopes marked as A and B, which the researcher had already made by random number table (zero was ignored; numbers 1, 2, 3 were assigned to the massage group; 4, 5, 6, to the breast feeding group; and 7, 8, 9 to the control group). Envelopes A were assigned to 6-month-old infants and envelopes B to 12-month-old infants.
The envelope was selected and opened based on the age of the qualified subjects who had referred for vaccination, and according to an already recorded method, necessary interventions were conducted. The variables of age and vaccination type of the studied subjects were non-randomly selected before sampling.
Descriptive and inferential statistical methods [chi-square, one-way analysis of variance (ANOVA), and least significant difference (LSD) post hoc test] were adopted to analyze the data in SPSS version 15. All ethical considerations indicated by the related faculty and university research ethical committee were followed in the present study.
RESULTS
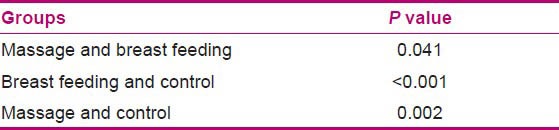
A total of 99 infants entered the study. Three infants were left out due to restlessness and cry before injection. Data analysis was conducted for 96 subjects. Frequency distribution of subjects’ age (age group of 6 months and 12 months) and the type of injection (muscular or subcutaneous) in the massage therapy, breast feeding, and control groups were quite identical (each group 50%). Chi-square test showed no significant difference in the frequency distribution of sex in the three groups of massage therapy, breast feeding, and control (P = 1, χ2 = 0). Frequency distribution of pain intensity showed the percentage of a painful condition in the massage therapy, breast feeding, and control groups as 65.6%, 43.8%, and 87.5%, respectively. Chi-square test also showed that the frequency distribution of a painful condition was not the same in the three groups of massage therapy, breast feeding, and control (P = 0.002, χ2 = 15.04) [Table 1]. Mean (SD) of pain scores in the breast feeding, massage therapy, and control groups were 3.4 (0.83), 3.9 (1.0), and 4.8 (1.1), respectively. One-way ANOVA showed that the mean pain scores were not the same in the three groups (P < 0.001, F = 10.26) [Table 2]. On comparing the mean pain scores of injection among the groups through LSD post hoc, the results showed the LSD value to be P = 0.04 in the massage therapy and breast feeding groups, P < 0.001 in the breast feeding and control groups, and P = 0.002 in the massage therapy and control groups. Mean pain score in the breast feeding group was found to be significantly less than in the massage therapy and control groups. The highest vaccination mean pain score was for the control group [Table 3].
Table 1.
Frequency distribution of NIPS pain intensity in massage therapy, breast feeding, and control groups
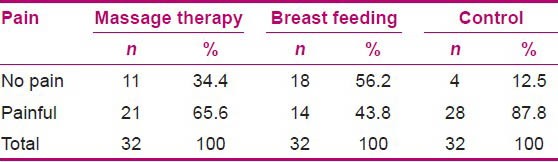
Table 2.
Mean scores of pain in massage therapy, breast feeding, and control groups
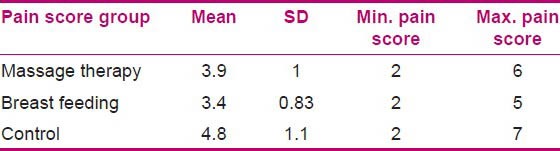
Table 3.
Comparison of pain score through LSD post hoc test among the groups
DISCUSSION
The results of the present study showed that mother's breast feeding during vaccination injection reduced pain more than massage therapy, so the highest pain intensity was observed in the control group. Mothers’ breast feeding is a multisensory experience and employs several concurrent sedation techniques such as mother — infant skin touch, infants’ distraction as a result of sucking, and the feeling of security for the infant. Mother's milk contains carbohydrates and precursors of melatonin (B endorphins release stimulator) which can probably affect pain reduction. Golestan et al. (2006) showed that sweet liquids can reduce vaccination pain in infants.[17,22]
Osinaike et al. also showed that infants’ feeding from their mothers’ breasts leads to a reduction in pain caused due to blood sampling from their heel.[23] Gray et al. (2002) reported that infants’ sucking milk from mothers’ breasts and infant–mother skin touch acted as a strong pain killer during blood sampling from their heels and notably decreased the time of infants’ cry and grimace.[24]
Carbajal et al. (2003) showed that mothers’ breast feeding significantly reduced the length of infants’ cry during blood sampling, compared to placebo group.[25] Shah et al. (2006) in their meta-analysis study showed that mothers’ lactation through breast significantly diminished the length and intensity of infants’ cry, compared to the use of a pacifier or taking glucose or sucrose and/or being hugged.[26]
Efe et al. (2007) conducted a study on the effect of breast feeding on pain relief of infants while crying and measured infants’ O2 saturation and heart rate, and reported that the mean length of cry was less in mothers’ breast feeding group compared to control group (P < 0.01), but infants’ O2 saturation and heart rate showed no difference in the study and control groups.[27] The results of aforementioned studies confirm the effect of mothers’ breast feeding on vaccination pain as observed in the present study.
In relation with the pain relief effects of massage therapy, the studies showed that foot reflexive massage reduced post-cesarean section pain in the study group compared to control (P < 0.001).[28]
The results of another study on comparison of the effect of two methods of reflexology and ibuprofen on girls’ dysmenorrhea showed that reflexology was more effective compared to the ibuprofen.[29] Another study showed that reflexive massage was effective on the management of low back pain. Their results showed that mean pain score decreased by 18 and 11.5 scores in reflexive massage and placebo groups, respectively.[30] These findings support the results obtained in the present study and suggest that massage therapy relives the pain of painful procedures. On the other hand, Golinau et al. (2007) in a study on the effect of non-medical methods such as massage therapy on injection pain in infants observed no significant reduction in the pain intensity of acute pains, and concluded that taking sedative medications is essential in these cases. The reason for the difference can be the massage conducted by someone other than the mother, as infants’ massage done by the mothers can have more effects on pain reduction due to firmer emotional relationship between the mothers and children.[31] Generally, with regard to the obtained results of the present study, mothers’ breast feeding may be more effective on vaccination pain reduction compared to massage therapy due to stimulation of sense of taste.
CONCLUSION
Since less vaccination pain was reported in the massage therapy group compared to the control group, it is suggested to use breast feeding as a natural, efficient, complication-free, noninvasive, convenient, and accessible method to relieve vaccination pain in breast feeding infants. Meanwhile, massage therapy can be used as a replacement method.
ACKNOWLEDGMENTS
The researcher greatly appreciates the Vice-chancellery for Research in Isfahan University of Medical Sciences and the staffs in Navabsafavi Health Care Center who cooperated for this study. This article is derived from MSC thesis No. 390622 in the Isfahan University of Medical Sciences.
Footnotes
Source of Support: Isfahan University of Medical Sciences
Conflict of Interest: Nil.
REFERENCES
- 1.Dilli D, Kucuk IG, Dallar Y. Interventions to reduce pain during vaccination in infancy. J Pediatr. 2009;154:385–90. doi: 10.1016/j.jpeds.2008.08.037. [DOI] [PubMed] [Google Scholar]
- 2.Pickering LK, Baker CJ, Long SS, McMillan JA, editors. Red Book: 2006 Report of the committee on infectious diseases. 27th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2006. American Academy of Pediatrics. Active and passive immunization; pp. 1–9. [Google Scholar]
- 3.Bilgen H, Ozek E, Cebeci D. Comparison of sucrose, expressed breast milk and breastfeeding on the neonatal response to heal prick. J Pain. 2001;2:301–5. doi: 10.1054/jpai.2001.23140. [DOI] [PubMed] [Google Scholar]
- 4.Larsson BA. Pain and pain relief during the neonatal period. Early pain experiences can result in negative late-effects. Lakartidningen. 2001;98:1656–62. [PubMed] [Google Scholar]
- 5.Ramponi DR. Reducing pain in pediatric minor emergency procedures. J Emerg Nurs. 2009;35:379–82. doi: 10.1016/j.jen.2009.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Henry PR, Houbold K, Dobrzykowski TM. Pain in the healthy full- term neonate: Efficacy and safety of interventions. Newborn Infant Nurs Rev. 2004;4:106–13. [Google Scholar]
- 7.Schechter NL, Zempsky WT, Cohen LL, McGrath PJ, McMurtry CM, Bright NS. Pain reduction during pediatric immunizations: Evidence-based review and recommendations. Pediatrics. 2007;119:e1184–98. doi: 10.1542/peds.2006-1107. [DOI] [PubMed] [Google Scholar]
- 8.Puchalski M, Hummel P. The reality of neonatal pain. Adv Neonatal Care. 2002;2:233–47. [PubMed] [Google Scholar]
- 9.Schechter N. Neonatal pain. J Paediatr Child Health. 2006;42:2–3. doi: 10.1111/j.1440-1754.2006.00778.x. [DOI] [PubMed] [Google Scholar]
- 10.Hassett AL, Gevirtz RN. Nonpharmacologic treatment for fibromyalgia: Patient education, cognitive-behavioral therapy, relaxation techniques, and complementary and alternative medicine. Rheum Dis Clin North Am. 2009;35:393–407. doi: 10.1016/j.rdc.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fucs S. 5th ed. St. Louis: Mosby Co; 2000. Mosby's Fundamental and Therapeutic Massage; pp. 15–9. [Google Scholar]
- 12.India; 2005. [Last accessed on 2013 May 30]. Sujok Therapy Center [Internet] Available from: http://www.sujoktherapy.com . [Google Scholar]
- 13.Jafaripour A. Tehran: Bijan Publishes; 2009. Sujok seed therapy; pp. 10–5. [Google Scholar]
- 14.Tsao JC, Evans S, Meldrum M, Altman T, Zeltzer LK. A Review of CAM for Procedural Pain in Infancy: Part II. Other Interventions. Evid Based Complement Alternat Med. 2008;5:399–407. doi: 10.1093/ecam/nem089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tsao JC, Evans S, Meldrum M, Altman T, Zeltzer LK. Review of cam for procedural pain in infancy: Part I. Sucrose and non-nutritive sucking. Evid Based Complement Alternat Med. 2008;5:371–81. doi: 10.1093/ecam/nem084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Abasi Z, Salari A, Rashidi F, Taherpour M. The effect of Massage method on the pain intensity of Vaccination in newborns. J North Khorasan Univ Med Sci. 2011;3:51–6. [Google Scholar]
- 17.Uga E, Candriella M, Perino A, Alloni V, Angilella G, Trada M, et al. Heel lance in newborn during breastfeeding: An evaluation of analgesic effect of this procedure. Ital J Pediatr. 2008;34:3. doi: 10.1186/1824-7288-34-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Academy of Pediatrics. Committee on Psychosocial Aspects of Child and Family Health; Task Force on Pain in Infants, Children, and Adolescents. The assessment and management of acute pain in infants, children, and adolescents. Pediatrics. 2001;108:793–7. doi: 10.1542/peds.108.3.793. [DOI] [PubMed] [Google Scholar]
- 19.Codipietro L, Ceccarelli M, Ponzone A. Breastfeeding or oral sucrose solution in term neonates receiving heel lance: A randomized controlled trial. Pediatrics. 2008;122:716–21. doi: 10.1542/peds.2008-0221. [DOI] [PubMed] [Google Scholar]
- 20.Taavoni S, ShahAli S, Haghani H, Neisani Samani L. Comparison the effect of breast feeding with routine clinical procedure on pain relieving during immunization injection. Arak Univ Med Sci J. 2008;11:33–40. [Google Scholar]
- 21.Razak AA, El-Dein NA. Effect of breastfeeding on pain relief during infant immunization injections. Int J Nurs Pract. 2009;15:99–104. doi: 10.1111/j.1440-172X.2009.01728.x. [DOI] [PubMed] [Google Scholar]
- 22.Golestan M, Sadrebafghi M, Akhavan Karbasi S, Eslami Z, Hashemi A, Mirnaseri F, et al. Comparison Pain relieving effects of glucose and water in neonates. Iran J Pediatr. 2006;16:441–6. [Google Scholar]
- 23.Osinaike BB, Oyedeji AO, Adeoye OT, Dairo MD, Aderinto DA. Effect of breastfeeding during venepuncture in neonates. Ann Trop Paediatr. 2007;27:201–5. doi: 10.1179/146532807X220316. [DOI] [PubMed] [Google Scholar]
- 24.Gray L, Miller LW, Phillipp BL, Blass EM. Breastfeeding is analgesic in healthy newborns. Pediatrics. 2002;109:590–3. doi: 10.1542/peds.109.4.590. [DOI] [PubMed] [Google Scholar]
- 25.Carbajal R, Veerapen S, Couderc S, Jugie M, Ville Y. Analgesic effect of breastfeeding in term neonates: Randomized control trial. BMJ. 2003;326:13–5. doi: 10.1136/bmj.326.7379.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah PS, Aliwalas LL, Shah V. Breastfeeding or breast milk for Procedural Pain in neonates. Cochrane Database Syst Rev. 2006;19:CD004950. doi: 10.1002/14651858.CD004950.pub2. [DOI] [PubMed] [Google Scholar]
- 27.Efe E, Ozer ZC. The use of breastfeeding for pain relief during neonatal immunization injections. Appl Nurs Res. 2007;20:10–6. doi: 10.1016/j.apnr.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 28.Khoshtarash M, Ghanbari A, Yeganeh M, Kazemnajad A, Rezasoltani P. Survey the effect of foot reflexology on pain and physiological parameters after cesarean section in patients referring to Alzahra educational center in Rasht. J Nurs Midwifery Fac Guilan Med Univ. 2011;20:27–33. [Google Scholar]
- 29.Valiani M, Babaie A, Heshmat R, Zare Z. Comparing the effects of reflexology methods and Ibuprofen administration on dysmenorrhea in female students of Isfahan University of Medical Sciences. Iran J Nurs Midwifery Res. 2010;15:371–8. [PMC free article] [PubMed] [Google Scholar]
- 30.Quinn F, Hughes CM, Baxter GD. Reflexology in the management of low back pain: A pilot randomised controlled trial. Complement Ther Med. 2008;16:3–8. doi: 10.1016/j.ctim.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Golinau B, Krane E, Seybold J, Almgren C, Anand KJ. Non-pharmacological techniques for pain management in neonates. Semin Perinatol. 2007;31:318–22. doi: 10.1053/j.semperi.2007.07.007. [DOI] [PubMed] [Google Scholar]


