Summary
Burn wound infections remain the most important factor limiting survival in burn intensive care units. Large wound surface, impaired immune systems, and broad-spectrum antibiotic therapy contribute to the growth of opportunistic fungal species. Faced with challenging fluid resuscitation, wound excision and cardiopulmonary stabilization, mycosis in burns are likely to be underestimated. Diagnostic performance can sometimes be delayed because clinical signs are unspecific and differentiation between colonization and infection is difficult. Therapeutic measures range from infection prophylaxis over treatment with antifungal agents towards radical amputation of infected limbs. New methods of early and reliable detection of fungal organisms, as well as the use of novel antifungal substances, are promising but require wider establishment to confirm the beneficial effects in burn patients. This review aims to highlight the main important aspects of fungal infections in burns including incidence, infection control, diagnostic and therapeutic approaches, prognosis and outcomes.
Keywords: burns, burn intensive care, fungal infection
Abstract
Les infections de plaies des brûlures restent le facteur le plus important qui limite la survie dans des unités de soins intensifs des brûlures. Une plaie grande, une immunodépression, et une antibiothérapie à large spectre contribuent à la croissance des espèces fongiques opportunistes. Face à la réanimation liquidienne difficile, l’excision de la plaie et la stabilisation cardiorespiratoire, les mycoses des brûlures sont susceptibles d’être sous-estimées. Le rendement diagnostic peut parfois être retardé car des signes cliniques ne sont pas spécifiques et la différenciation entre la colonization et l’infection est difficile. Les mesures thérapeutiques vont de la prévention des infections au traitement avec des agents antifongiques vers amputation radicale des branches infectées. De nouvelles méthodes de détection précoce et fiable d’organismes fongiques, ainsi que l’utilisation de nouvelles substances antifongiques, sont prometteuses mais on a besoin de plus exemples pour confirmer les effets bénéfiques chez les patients brûlés. Cette revue a pour but de mettre en évidence les principaux aspects importants des infections fongiques chez les brûlures, y compris l’incidence, la lutte contre les infections, les approches diagnostiques et thérapeutiques, le pronostic et les résultats.
Introduction
Burn patients are exposed to a high risk of developing fungal infections, compared with other hospitalized patients.1 Although often underestimated, invasive burn wound infections due to Candida spp., Aspergillus spp., and other opportunistic fungi are important emerging causes of late-onset morbidity and mortality in patients with major burns and severely perturbed immune systems.2 Main risk factors that have been identified are an increase in the burned total body surface area (TBSA) and impaired immune defense. The use of broad-spectrum antibiotic substances also leads to an eradication of the natural bacterial flora and promotion of oportunistic species.3-5 Additional predisposing factors are increased age, uncontrolled diabetes, and the presence of central venous catheters.6
Treatment standards and infection prophylaxis after burn center admission
After burn center admission, the patient undergoes primary wound evaluation and stabilization of vital functions. Simultaneously, measures of infection prophylaxis are initiated, including whole body cleaning, shaving, and microbial surveillance. Subsequent placement of wet and aseptic wound covers for 24 hours follows a second wound evaluation to calculate the dimensions of excision and meshgraft transplantation. Surgical excision and grafting is usually performed as soon as the patient’s condition is stabilized. Depending on the depth of the wounds, excision may be tangential until adequate dermal perfusion is visible or epifascial in deep burns. Meshgraft transplantation is typically performed simultaneously, and the grafts are fixed in place with metal clamps or sutures. The grafts and the donor sites are covered with fat gauze and blankets and remain covered for 4-5 days. After another wound evaluation, either healing may be confirmed or further surgery may be planned. Each period of resuscitation, intensive care, and surgery provides a certain risk to acquire infections, including by fungal organisms, whereas the full impact of severe septic complications usually develop in the later course of burn care. Only strict and standardized hygiene regimes may support the efforts to prevent external contamination of the immune-impaired patient.
Environmental risk factors for fungal infections
Thermal injury of the skin considerably impairs the ability to regulate body temperature. Modern burn centers provide special patient rooms, so-called boxes, in which the temperature and humidity can be controlled over a wide range (between 21 and 38°C, humidity up to 60%). There is a difference in air pressure between these boxes and other areas of the burn unit, and the air exchange is at least 10-fold its volume per hour; microbial filters are implemented in these air exchangers. One reason for this technical expenditure is that fungal spores and other microbial species are known to spread by air exchange units.7 In patients with large burns, additional heating lamps may be required to provide normothermia. The combination of external heat, moisturized wound covers and the wounds themselves provide a milieu that increases the risk of microbial colonization and infection, including by fungal organisms. Regular microbial surveillance and the exchange of sensitive parts, e.g., the filter membranes of the air conditioner and water connections, may identify and remove system-dependent weaknesses. Furthermore, an interdisciplinary approach including certified infection control personnel, burns and plastic surgeons, intensivists and microbiologists is required to minimize the risk of environmental contamination of burn patients.8
Patient-related risk factors for fungal infections
Patient-specific risk factors for fungal infections after burn injury include increasing age, >40% burned TBSA, and inhalation injury.3,4 Further contributing factors are neutropenia and uncontrolled Diabetes mellitus.6,9
After burn injuries, ubiquitous Candida colonization of the skin and mucosal membranes of nose, throat and gastrointestinal tract likely represents a latent source of infection, especially in patients with impaired immune resistance. 2,4,10,11 Furthermore, gastric ulcers, either pre-existent or acquired during intensive care, may provide an entrance for systemic fungal organisms.12,13
Prior Candida colonization is an important risk factor for candidaemia, and the risk increases substantially with the number of colonized sites. In a study including 143 Candida-positive patients, 43% of patients colonized at more than three sites (and not receiving antifungal medication) developed candidaemia.4
Treatment-related risk factors for fungal infections
Burns may be complicated by prehospital exposure to contaminated water. Water immersion to extinquish the fire or to cool burn wounds have been described as possible source of invasive bacterial and fungal infections.14
Despite numerous prophylactic efforts, microbial transfer from the hospital environment or staff to burn patients is still a possibility. Incomplete or late burn wound excision increases the risk of infection, whereas too long and extensive surgery may deteriorate the patient’s general condition. 3,15 Moreover, multiple surgical sessions may be required Large blood losses, massive transfusion, vasopressor therapy, sedation, total parenteral nutrition and renal replacement therapy further weaken immune resistance and create circumstances for possible fungal colonization and infection. Additionally, burn surgery may lead to systemic liberation of vasoactive mediators, cytokines and bacteria.16 These stressors influence not only immune resistance but also the ability of wound healing.17-20
The use of fat gauze in wound coverage provides an air-sealed condition, which is another risk factor for possible treatment-related colonization of bacteria and fungi.
Certain bacteria are known to colonize burn wounds.21-25 Staphylococcus aureus, Streptococcus spp and endogenous Enterobacteriacae account for early bacterial wound colonization whereas Klebsiella spp., exogenous Enterobacteriacae (e.g. Enterobacter spp, Serratia spp), Acinetobacter spp. and Pseudomonas spp. (as the most relevant species for burn wound infection) are usually confirmed in a later course of burn intensive care. Fungal colonization may occur due to delayed wound excision or due to suppression of bacterial flora after prolonged prophylactic or therapeutic antibiotic therapy.
The introduction and extensive use of topical antiseptic substances in the 1970s led to a decline in gram-negative bacterial infections in burn centers. Simultaneously, an increase in fungal infections was observed in up to 83% of the patients.21, 26-28 Certain antimicrobial substances, e.g., tazobactam (systemic use) and nystatin (topical application) have been reported to facilitate invasive non-albicans Candida infections.29-31
Patients presenting with simultaneous inhalation injury, prolonged mechanical ventilation predispose to secondary fungal infection.32,33 Furthermore, patients with fungal infections require longer ventilation times and intensive care treatment.4,5
Any catheters inserted into the body of a burn patient, e.g., tracheal tubes, central or peripheral venous catheters, gastric tubes, rectal tubes, and urinary catheters, are possible mediators of fungal colonization or infection. Therefore, their necessity and duration should be re-evaluated frequently.1,9,34
Diagnostic approaches for fungal colonization and infection
Clinical warning signs for fungal infections are unspecific and do not differ from infections of bacterial origin. Due to burn-wound-related permanent inflammation and consequent physiological reactions, common definitions of sepsis are not applicable to burn patients.18,24 Furthermore, laboratory tests may have limited impact. Significant increases and declines in white blood cells and increases in C-reactive protein and interleukin-6 with simultaneous low levels of procacitonin are signs of maximally activated or exhausted immune competence and may be predictors of occult fungal infection or even fungal sepsis.13,18,19 Current diagnostic approaches for an early detection of mycosis are limited and often unreliable.35
Cultures
Direct confirmation of positive fungal cultures from burn wounds is the standard diagnostic approach but it may be associated with certain latency and species-dependent unreliability.35,36 In studies evaluating independent risk factors of invasive Candida infections, the extent of body site colonization due to Candida species was recognized to be associated with consequent invasive disease. The quantification of the colonization was expressed on the Candida colonization index as a clinically relevant score. Furthermore, the Candida score that combines the clinical risk factors preceding surgery, total parenteral nutrition and severe sepsis with Candida multi-site colonization revealed a useful bedside scoring system to identify non-neutropaenic critically ill patients with the risk of invasive candidiasis.4,37
Candida and Aspergillus antigen test
Positive predictive values of some Candida antigen tests may be too low for reliable diagnostic.38,39 In particular, Cand-Tec Candida antigen and the mannan antigen plus anti-mannan antibody measurements may have unacceptably low sensitivity or specificity. However, the (1-->3)- ß-d-glucan and mannan antigen may be superior biomarkers, depending on whether a sensitivity-driven or specificity- driven approach is used.40
Sensitivity of Aspergillus glactomannan immuno assays may also be low (between 0.2 and 0.55), whereas a recently developed point-of-care test for Aspergillus antigen based on lateral flow technology detect an extracellular glycoprotein secreted only during active fungal growth with promising sensitivity and specifity.41,42
Histology
The histological diagnosis of burn wounds after biopsy is a reliable method to confirm fungal colonization and infection. However, due to its invasive character, this method is usually avoided and not routinely performed.43,44
New approaches
New diagnostic methods for an early and non-invasive detection (real-time polymerase chain reaction assays) are known, but they are not available for all fungal organisms and may not be established in every laboratory institution because of high costs.45 These diagnostic limitations may sometimes prevent an early and appropriate antimycotic therapy.46
Incidence and spectrum of fungal organisms
The incidence of fungal contamination and infection in burn patients is reported to be 6.3% to 15%, although there are significant differences between individual burn centers ranging from 0.7% up to 24.1%.3,47 This variation may be the result of different standards in the performance of surveillance cultures and may reflect differences in the frequency, quality and quantity of diagnostic efforts in suspected cases. Earlier studies confirmed much higher incidences of Candida infections in burn centers that performed frequent surveillance protocols compared with other burn centers.25,48 The incidence of fungal infections in patients presenting with >80% TBSA may be lower because of other complications, e.g., uncontrollable hemodynamic instability, septic complications and multiple organ failure, which may occur earlier in the course of burn intensive care and are likely to limit survival.2
There is a domination of Candida albicans mycoses in burn centers.1,3,11,37,41,49-52 However, there are various reports concerning the incidence and virulence of several fungal species.35,48 In certain burn centers, an increasing incidence of invasive infections of non-albicans Candida, Aspergillus and zygomycoses has been reported.8,39,1-58 Zygomycoses in particular, infections of saprophytic molds that typically grow in rotting organic material, may be a serious threat to burn patients. These organisms provide proteolytic enzymes, may invade healthy skin and have an angioinvasive growth pattern that may contribute to severe coagulation disorder and vessel occlusion.59-61
A North American multicenter analysis of 435 positive cultures from 15 burn centers reported Candida species in 85% of them, non-Candida yeast in 21%, Aspergillus in 14%, zygomycetes, including Mucor spp. in 9% and other fungal organisms in 1.4% of the cultures.3
Therapeutic approaches for fungal infections
For the clinical therapy of mycoses, it is important to know whether a fungal colonization or a fungal infection is involved.52,62 In daily practice, this differentiation may be not easy because, as already mentioned, the special pathophysiology of the burn wound provides laboratory characteristics of common inflammatory response and bacteria-related infection, and, furthermore, unreliable diagnostic possibilities.
Systematic risk reduction
The most important goal in burn patients presenting with a high risk of infection is an early achievement of appropriate immune competence. This goal may be facilitated by early enteral nutrition, early and complete burn wound excision and grafting, restrictive use of blood transfusion, early weaning from mechanical ventilation, avoidance of broad spectrum antibiotic prophylaxis, rational antibiotic therapy including de-escalation strategy and frequent re-evaluation, and restrictive use of invasive catheterization.
Antimycotic prophylaxis
Some authors recommend antimycotic prophylaxis for burn patients presenting with a > 50% burned TBSA, inhalation injury and neutropenia, although there is currently no evidence to support this strategy.3,4 The broad and generalized use of antifungal agents in burn patients without a high risk potential may be problematic because of the possible generation of resistances and increasing costs.36,52,63
Antimycotic therapy
Some burn centers use topical applications of antifungal agents, e.g., nystatin, amphomoronal, and silvercontaining agents. These substances may successfully treat local colonization and infection of fungal organisms that contain sterol structures in their cell membrane (Candida albicans) but may also hide manifest infections.11,64-67 Furthermore, certain topical anti-infective agents may have cytotoxic effects. Therefore, their use upon meshgrafts should be restricted to avoid healing complications.
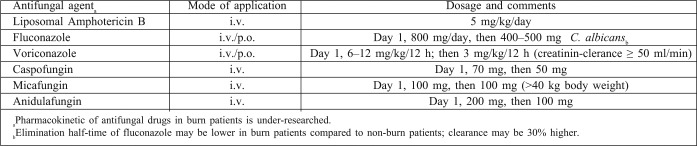
The systemic use of antifungal agents may depend on the general condition of the burn patient, the fungal species and the confirmation of fungemia2-4,39-49 (Table I). Apart from established polyenes and imidazole-based azoles, new triazoles and echinocandins provide higher specificity. Limitations on the use of antifungal agents may be the development of resistances, hepato- and nephrotoxicity, the lack of rapid, reliable and precise diagnostics, insufficient tissue permeability, and limited oral or intravenous applicability.36,38 Species-related gaps may require multiple antifungal substances.46,69 New approaches, such as calcineurin blockers and Candida-secretoric aspartate protease-inhibitors are promising but still have to be clinically investigated and established.70
Table I. Recommendations for antifungal therapy of non-neutropenic patients with Candida infection after burn injury.
Surgical therapy
Invasive fungal infections, typically Aspergillus and zygomycoses, may require additional surgical exploration to limit the extension of infection, including amputation of limbs. An infection requiring surgical therapy is often associated with high mortality.69,71,72
Prognosis of fungal infections
An early and definitive closure of the burn wound was found to be a treatment-related positive predictor of a good outcome, implicating the great impact of thorough burn wound care after surgical therapy.64
In multivariate analyses, 4 parameters predicted increasing mortality due to fungal infections in burn patients: higher age, extensive percentage of burned TBSA, increasing numbers of positive cultures, and confirmation of Aspergillus spp. or zygomycoses.3,73 A contamination with zygomycoses revealed a mortality of 31%, and an infection rate of 81-100%.55,71,72,74 Furthermore, fungal infection of non-burned skin predicted mortality, independent from the extent of burned TBSA.56
Different sub-types of Candida species represent different risks in cases of infection. Compared with Candida albicans, non-albicans Candida infections may be associated with a higher mortality rate and higher resistance rates against antifungal agents, although other burn centers did not reveal these findings.39,52,53,75,76 Recent developments of azole resistance remains a challenge in treating Aspergillus infections, particularly in Europe, while resistence rates are probably even underreported due to incomplete strain analysis. Direct azole resistance detection using molecular biology methods may offer more rapid analysis for clinicians, although the large number of possible resistance mechanisms contributes to very complex interaction processes.42
Conclusions
Fungal infections are rare but severe complications and remain a challenge in burn intensive care. Possible solutions may be the development of clinically practicable diagnostic methods, avoidance of broad spectrum antibiotic prophylaxis, measures to recover immune competence, and the earliest possible definitive burn wound closure. Antifungal agents should be used appropriately and targeted, keeping rising resistance rates in mind.
Key messages
Fungal infections in burns are likely to occur in patients with large wound surfaces, impaired immune resistance, advanced age and broad-spectrum antibiotic therapy.
Discrimination between fungal infection and colonization in burn wounds is difficult; clinical presentation is unspecific and sensitivity of diagnostic results may be unreliable.
Recent studies report an increasing incidence of non-albicans Candida spp., Aspergillus spp., and zygomycoses including Rhizopus in burn units. These organisms provide higher resistance rates to antifungal substances and are associated with poor prognosis.
Antifungal therapy includes infection control using frequent microbial surveillance, early treatment with appropriate antimycotic substances in highrisk patients and earliest possible burn wound closure.
References
- 1.Jarvis WR. Epidemiology of nosocomial fungal infections, with emphasis on candida species. Clin Infect Dis. 1995;20:1526–30. doi: 10.1093/clinids/20.6.1526. [DOI] [PubMed] [Google Scholar]
- 2.Church D, Elsayed S, Reid O, et al. Burn wound infections. Clin Microbiol Rev. 2006;19:403–34. doi: 10.1128/CMR.19.2.403-434.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ballard J, Edelman L, Saffle J, et al. Positive fungal cultures in burn patients: a multicenter review. J Burn Care Res. 2008;29:213–21. doi: 10.1097/BCR.0b013e31815f6ecb. [DOI] [PubMed] [Google Scholar]
- 4.Moore EC, Padiglione J, Wasiak XXX, et al. Candida in burns: risk factors and outcomes. J Burn Care Res. 2010;31:257–63. doi: 10.1097/BCR.0b013e3181d0f536. [DOI] [PubMed] [Google Scholar]
- 5.Luo G, Peng Y, Yuan Z, et al. Yeast from burn patients at a major burn centre of China. Burns. 2011;37:299–303. doi: 10.1016/j.burns.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 6.Gore DC, Chinkes D, Heggers J, et al. Association of hyperglycemia with increased mortality after severe burn injury. J Trauma. 2001;51:540–4. doi: 10.1097/00005373-200109000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Vonberg RP, Gastmeier P. Nosocomial aspergillosis in outbreak settings. J Hosp Infect. 2006;63:246–54. doi: 10.1016/j.jhin.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 8.Mousa HA, Al-Bader S, Hassan D. Correlation between fungi isolated from burn wounds and burn care units. Burns. 1999;25:145–7. doi: 10.1016/s0305-4179(98)00148-x. [DOI] [PubMed] [Google Scholar]
- 9.Cochran A, Morris SE, Edelman LS, et al. Systemic candida infections in burn patients: a case-control study of management patterns and outcomes. Surg Infect. 2006;3:367–74. doi: 10.1089/109629602762539580. [DOI] [PubMed] [Google Scholar]
- 10.Zwolinska-Wcislo M, Budak A, Bogdal J, et al. Fungal colonization of gastric mucosa and its clinical relevance. Med Sci Monit. 2001;7:982–8. [PubMed] [Google Scholar]
- 11.Branski LK, Al-Mousawi A, Rivero H, et al. Emerging infections in burns. Surg Infect. 2009;10:389–97. doi: 10.1089/sur.2009.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koh AY, Köhler JR, Coggshall KT, et al. Mucosal damage and neutropenia are required for Candida albicans dissemination. PloS Pathog. 2008;4:35. doi: 10.1371/journal.ppat.0040035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Struck MF, Stiller D, Corterier CC, et al. Fulminant, undetected candida sepsis in a patient with apparently survivable burns. J Burn Care Res. 2009;30:894–7. doi: 10.1097/BCR.0b013e3181b48794. [DOI] [PubMed] [Google Scholar]
- 14.Ribeiro NF, Heath CH, Kierath J, et al. Burn wounds infected by contaminated water: case reports, review of the literature and recommendations for treatment. Burns. 2010;36:9–22. doi: 10.1016/j.burns.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 15.Xiao-Wu W, Herndon DN, Spies M, et al. Effects of delayed wound excision and grafting in severely burned children. Arch Surg. 2002;137:1049–54. doi: 10.1001/archsurg.137.9.1049. [DOI] [PubMed] [Google Scholar]
- 16.Opal SM. Insights into the immune dysfunction associated with thermal injury. Crit Care Med. 2002;30:1651–2. doi: 10.1097/00003246-200207000-00043. [DOI] [PubMed] [Google Scholar]
- 17.Calum H, Moser C, Jensen PØ, et al. Thermal injury induces impaired function in polymorphonuclear neutrophil granulocytes and reduced control of burn wound infection. Clin Exp Immunol. 2009;156:102–10. doi: 10.1111/j.1365-2249.2008.03861.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Greenhalgh DG, Saffle JR, Holmes JH, et al. American Burn Association Consensus Conference to define sepsis and infection in burns. J Burn Care Res. 2007;28:776–90. doi: 10.1097/BCR.0b013e3181599bc9. [DOI] [PubMed] [Google Scholar]
- 19.Bhat S, Milner S. Antimicrobial peptides in burns and wounds. Curr Protein Pept Sci. 2007;8:506–20. doi: 10.2174/138920307782411428. [DOI] [PubMed] [Google Scholar]
- 20.Van de Goot F, Krijnen PA, Bequieneman MP. Acute inflammation is persistent for months locally in burn wounds: a pivotal role for complement and C-reactive protein. J Burn Care Res. 2009;30:74–80. doi: 10.1097/BCR.0b013e318198a252. [DOI] [PubMed] [Google Scholar]
- 21.Brusselaers N, Monstrey S, Snoeij T, et al. Morbiditi and mortality of bloodstream infections in patients with severe burn injury. Am J Crit Care. 2010;19:81–7. doi: 10.4037/ajcc2010341. [DOI] [PubMed] [Google Scholar]
- 22.de Macedo JL, Santos JB. Bacterial and fungal colonization of burn wounds. Mem Inst Oswaldo Cruz. 2005;100:535–9. doi: 10.1590/s0074-02762005000500014. [DOI] [PubMed] [Google Scholar]
- 23.Gupta N, Haque A, Mukhopadhyay G, et al. Interactions between bacteria and candida in the burn wound. Burns. 2005;31:375–8. doi: 10.1016/j.burns.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 24.Mann-Salinas EA, Baun MM, Meininger JC, et al. Novel predictors of sepsis outperform the American Burn Association sepsis criteria in the burn intensive care unit patient. J Burn Care Res. 2013;34:31–43. doi: 10.1097/BCR.0b013e31826450b5. [DOI] [PubMed] [Google Scholar]
- 25.Trupkovic T, Gille J, Fischer H, et al. Antimicrobial treatment in burn injury patients. Anaesthesist. 2012;61:249–258. doi: 10.1007/s00101-012-1994-4. [DOI] [PubMed] [Google Scholar]
- 26.Law EJ, Kim OJ, Stieritz DD, et al. Experience with systemic candidiasis in the burned patient. J Trauma. 1972;12:543–52. doi: 10.1097/00005373-197207000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Wheeler MS, Mc Ginnis MR, Schell WA, et al. Fusarium infection in burned patients. Am J Clin Pathol. 1981;75:304–11. doi: 10.1093/ajcp/75.3.304. [DOI] [PubMed] [Google Scholar]
- 28.Lin MY, Carmeli Y, Zumsteg J, et al. Prior antimicrobial therapy and risk for hospital-acquired Candida glabrata and Candida krusei fungemia: A case-case-control study. Antimicrob Agents Chemother. 2005;49:455–60. doi: 10.1128/AAC.49.11.4555-4560.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dubé MP, Heseltine PN, Rinaldi MG, et al. Fungemia and colonization with nystatin-resistant Candida rugosa in a burn unit. Clin Inf Dis. 1994;18:77–82. doi: 10.1093/clinids/18.1.77. [DOI] [PubMed] [Google Scholar]
- 30.Desai MH, Rutan RL, Heggers JP, et al. Candida infection with and without nystatin prophylaxis: An 11-year experience with patients with burn injury. Arch Surg. 1992;127:159–62. doi: 10.1001/archsurg.1992.01420020041006. [DOI] [PubMed] [Google Scholar]
- 31.Mayhall CG. The epidemiology of burn wound infections: Then and now. Clin Infect Dis. 2003;37:543–50. doi: 10.1086/376993. [DOI] [PubMed] [Google Scholar]
- 32.Gastmeier P, Weigt O, Sohr D. Comparison of hospital-acquired infection rates in paediatric burn patients. J Hosp Infect. 2002;52:161–5. doi: 10.1053/jhin.2002.1292. [DOI] [PubMed] [Google Scholar]
- 33.O’Mara MS, Reed NL, Palmieri TL, et al. Central venous catheter infection in burn patients with scheduled catheter exchange and replacement. J Surg Res. 2007;142:341–50. doi: 10.1016/j.jss.2007.03.063. [DOI] [PubMed] [Google Scholar]
- 34.Tansho S, Abe S, Ishibashi H, et al. Production of anti-candida antibodies in mice with gut colonization of candida albicans. Mediators Inflamm. 2004;13:189–93. doi: 10.1080/09511920410001713510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rodloff C, Koch D, Schaumann R. Epidemiology and antifungal resistance in invasive candidiasis. Eur J Med Res. 2011;28:187–95. doi: 10.1186/2047-783X-16-4-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schofield CM, Murray CK, Horvath EE, et al. Correlation of culture with histopathology in fungal burn wound colonization and infection. Burns. 2007;33:341–6. doi: 10.1016/j.burns.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 37.Kratzer C, Graninger W, Lassnigg A, et al. Design and use of candida scores at the intensive care unit. Mycoses. 2011;54:467–74. doi: 10.1111/j.1439-0507.2010.01953.x. [DOI] [PubMed] [Google Scholar]
- 38.Kealey GP, Heinle JA, Lewis RW, et al. Value of the candida antigen assay in diagnosis of systemic candidiasis in burn patients. J Trauma. 1992;32:285–8. doi: 10.1097/00005373-199203000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Ha JF, Italiano CM, Heath CH, et al. Candidemia and invasive candidiasis: A review of the literature for the burns surgeon. Burns. 2011;37:181–95. doi: 10.1016/j.burns.2010.01.005. [DOI] [PubMed] [Google Scholar]
- 40.Held J, Kohlberger I, Rappold E, et al. Comparison of (1->3)-ß-D-Glucan, Mannan/Anti-Mannan Antibodies, and Cand-Tec Candida Antigen as Serum Biomarkers for Candidemia. J Clin Microbiol. 2013;51:1158–64. doi: 10.1128/JCM.02473-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Thornton C, Johnson G, Agrawal S. Detection of invasive pulmonary aspergillosis in haematological malignancy patients by using lateral-flow technology. J Vis Exp. 2012;61:3721. doi: 10.3791/3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hayes GE, Denning DW. Frequency, diagnosis and management of fungal respiratory infections. Curr Opin Pulm Med. 2013;19:259–65. doi: 10.1097/MCP.0b013e32835f1ad1. [DOI] [PubMed] [Google Scholar]
- 43.Hart DW, Wolf SE, Chinkes DL, et al. Determinants of skeletal muscle catabolism after severe burn. Ann Surg. 2000;232:455–65. doi: 10.1097/00000658-200010000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Spebar MJ, Lindberg RB. Fungal infection of the burn wound. Am J Surg. 1979;138:879–82. doi: 10.1016/0002-9610(79)90315-5. [DOI] [PubMed] [Google Scholar]
- 45.McMullan R, Metwally L, Coyle PV, et al. A prospective clinical trial of a real-time polymerase chain reaction assay for the diagnosis of candidemia in non-neutropenic, critically ill adults. Clin Infect Dis. 2008;46:890–6. doi: 10.1086/528690. [DOI] [PubMed] [Google Scholar]
- 46.Enoch DA, Ludlam HA, Brown NM, et al. Invasive fungal infections: A review of epidemiology and management options. J Med Microbiology. 2006;55:809–18. doi: 10.1099/jmm.0.46548-0. [DOI] [PubMed] [Google Scholar]
- 47.Santucci SG, Gobara S, Santos CR, et al. Infections in a burn intensive care unit: experience of seven years. J Hosp Infect. 2003;53:6–13. doi: 10.1053/jhin.2002.1340. [DOI] [PubMed] [Google Scholar]
- 48.Ekenna O, Fader RC. Effect of thermal injury and immunosuppression on the dissemination of candida albicans from the mouse gastrointestinal tract. J Burn Care Rehabil. 1989;10:138–45. doi: 10.1097/00004630-198903000-00007. [DOI] [PubMed] [Google Scholar]
- 49.Mousa HA, al Bader SM. Yeast infection of burns. Mycoses. 2001;44:147–9. doi: 10.1046/j.1439-0507.2001.00627.x. [DOI] [PubMed] [Google Scholar]
- 50.Rosanova MT, Basilico H, Villasboas M, et al. Fungal infections in a pediatric burn care. Arch Argent Pediatr. 2011;109:441–4. doi: 10.5546/aap.2011.441. [DOI] [PubMed] [Google Scholar]
- 51.Pedrosa AF, Rodrigues AG. Candidemia in burn patients: Figures and facts. J Trauma. 2011;70:498–506. doi: 10.1097/TA.0b013e3181f2d4fb. [DOI] [PubMed] [Google Scholar]
- 52.Schaal JV, Leclerc T, Pasquier P, et al. Epidemiology of fungal infection in burns: therapeutic implications. Burns. 2012;38:942–3. doi: 10.1016/j.burns.2012.02.028. [DOI] [PubMed] [Google Scholar]
- 53.Sarabahi S, Tiwari VK, Arora S, et al. Changing pattern of fungal infection in burn patients. Burns. 2012;38:520–8. doi: 10.1016/j.burns.2011.09.013. [DOI] [PubMed] [Google Scholar]
- 54.Gupta N, Haque A, Lattif AA. Epidemiology and molecular typing of candida isolates in burn patients. Mycopathologia. 2004;158:397–405. doi: 10.1007/s11046-004-1820-x. [DOI] [PubMed] [Google Scholar]
- 55.Constantinides J, Misra A, Nassab R, et al. Absidia corymbifera fungal infection in burns: a case report and review of the literature. J Burn Care Res. 2008;29:416–9. doi: 10.1097/BCR.0b013e318166da78. [DOI] [PubMed] [Google Scholar]
- 56.Horvath EE, Murray CK, Vaughan GM, et al. Fungal wound infection (not colonization) is independently associated with mortality in burn patients. Ann Surg. 2007;245:978–85. doi: 10.1097/01.sla.0000256914.16754.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Krcmery V, Barnes AJ. Non-albicans candida spp. causing fungemia: Pathogenicity and antifungal resistance. J Hosp Infect. 2002;50:243–60. doi: 10.1053/jhin.2001.1151. [DOI] [PubMed] [Google Scholar]
- 58.Capoor MR, Gupta S, Sarabahi S, et al. Epidemiological and clinico-mycological profile of fungal wound infection from largest burn centre in Asia. Mycoses. 2012;55:181–8. doi: 10.1111/j.1439-0507.2011.02065.x. [DOI] [PubMed] [Google Scholar]
- 59.Kraut EJ, Jordan MH, Steiner CR, et al. Arterial occlusion and progressive gangrene caused by mucormycosis in a patient with burns. J Burn Care Rehabil. 1993;14:552–6. doi: 10.1097/00004630-199309000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Rüchel R, Elsner C, Spreer A. A probable cause of paradoxical thrombosis in zygomycosis. Mycoses. 2004;47:203–7. doi: 10.1111/j.1439-0507.2004.00981.x. [DOI] [PubMed] [Google Scholar]
- 61.Struck MF, Illert T, Stiller D, et al. Basilar artery occlusion after multifactor coagulopathy including rhizopus oryzae infection in burns. J Burn Care Res. 2010;31:955–8. doi: 10.1097/BCR.0b013e3181f93912. [DOI] [PubMed] [Google Scholar]
- 62.Blot S, Vandewoude K, Vogelaers D. Discriminating invasive fungal infection from colonization. Crit Care. 2008;12:412. doi: 10.1186/cc6835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eggimann P, Lamoth F, Marchetti O. On track to limit antifungal overuse. Intensive Care Med. 2009;35:582–4. doi: 10.1007/s00134-009-1432-5. [DOI] [PubMed] [Google Scholar]
- 64.Wright JB, Lam K, Hansen D, et al. Efficacy of topical silver burn wound pathogens. Burns. 1999;27:344–50. doi: 10.1016/s0196-6553(99)70055-6. [DOI] [PubMed] [Google Scholar]
- 65.Eldad A, Icekson M, Zur T. Silver-sulfadiazine eschar pigmentation mimics invasive wound in- fection: A case report. J Burn Care Res. 2003;24:154–7. doi: 10.1097/01.BCR.0000069440.78932.70. [DOI] [PubMed] [Google Scholar]
- 66.Barret JP, Ramzy PI, Heggers JP, et al. Topical nystatin powder in severe burns: A new treatment for angioinvasive fungal infections refractory to other topical and systemic agents. Burns. 1999;25:505–8. doi: 10.1016/s0305-4179(99)00037-6. [DOI] [PubMed] [Google Scholar]
- 67.Acar A, Uygur F, Diktas H. Comparison of silver-coated dressing (Acticoat®), chlorhexidine acetate 0.5% (Bactigrass®) and nystatin for topical antifungal effect in candida albicans-contaminated, full-skin-thickness rat burn wounds. Burns. 2011;37:882–5. doi: 10.1016/j.burns.2011.01.024. [DOI] [PubMed] [Google Scholar]
- 68.Mathew BP, Nath M. Recent approaches to anti-fungal therapy for invasive mycoses. Chem Med Chem. 2009;4:310–23. doi: 10.1002/cmdc.200800353. [DOI] [PubMed] [Google Scholar]
- 69.Murray CK, Loo FL, Hospenthal DR, et al. Incidence of systemic fungal infection and related mortality following severe burns. Burns. 2008;34:1108–12. doi: 10.1016/j.burns.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 70.Gauwerky K, Borelli C, Korting HC. Targeting virulence: a new paradigm for antifungals. Drug Discov Today. 2009;14:224–2. doi: 10.1016/j.drudis.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 71.Ledgard JP, van Hal S, Greenwood JE, et al. Primary cutaneous zygomycosis in a burn patient: a review. J Burn Care Res. 2008;29:286–90. doi: 10.1097/BCR.0b013e31816673b1. [DOI] [PubMed] [Google Scholar]
- 72.Latenser BA. Fusarium infections in burn patients: a case report and review of the literature. J Burn Care Rehabil. 2003;24:285–6. doi: 10.1097/01.BCR.0000085845.20730.AB. [DOI] [PubMed] [Google Scholar]
- 73.Andres LA, Ford RD, Wilcox RM. Necrotizing colitis caused by systemic aspergillosis in a burn patient. J Burn Care Res. 2007;28:918–21. doi: 10.1097/BCR.0b013e318159a3d8. [DOI] [PubMed] [Google Scholar]
- 74.Rees JR, Pinner RW, Hajjeh RA, et al. The epidemiological features of invasive mycotic infections in the San Francisco Bay area, 1992 – 1993: results of population-based laboratory active surveillance. Clin Infect Dis. 1998;28:1138–47. [PubMed] [Google Scholar]
- 75.Me´an M, Marchetti O, Calandra T. Bench to bed-side review: Candida infections in the intensive care unit. Crit Care. 2008;12:204. doi: 10.1186/cc6212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Girão E, Levin AS, Basso M, et al. Seven-year trend analysis of nosocomial candidemia and antifungal (fluconazole and caspofungin) use in intensive care units at a Brazilian university hospital. Med Mycol. 2008;46:581–8. doi: 10.1080/13693780802004996. [DOI] [PubMed] [Google Scholar]


