Summary
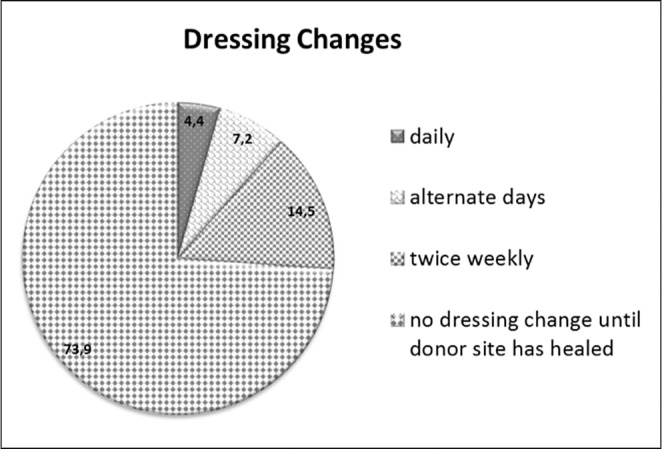
Split skin grafting is a widely used technique for reconstructing skin defects. Although a vast number of different coverage options for donor sites have become available in daily clinical practice, no optimum dressing material has been found to date. For this reason, we conducted a globally-distributed online survey to poll for the properties of such an “ideal” donor site dressing, possibly leading to an improved clinically-driven direction of future wound dressing developments. A total of 69 respondents from 34 countries took part in the questionnaire, resulting in a response rate of 13.8% (69/500) over a 1-month period. The majority of respondents rated the characteristics of an “ideal” donor site dressing to be either “essential” or “desirable” as follows: lack of adhesion to the wound bed (“essential”: 31/69, 44.9%; “desirable”: 30/69, 43.5%); pain-free dressing changes (“essential”: 38/69, 55.1%; “desirable”: 30/69, 43.5%); absorbency (“essential”: 27/69, 39.1%; “desirable”: 33/69, 47.8%); ease of removal (“essential”: 37/69, 53.6%; “desirable”: 27/69, 39.13%). With regard to the desired frequency of dressing changes, respondents preferred “no dressing change until the donor site has healed” (51/69, 73.9%) in the majority of cases, followed by “twice weekly” (10/69, 14.5%), “alternate days” (5/69, 7.2%) and “daily” (3/69, 4.3%). With regard to the design of the dressing material, the majority of participants preferred a one-piece (composite) dressing product (44/69, 63.8%). The majority of respondents also denied the current availability of an “ideal” donor site dressing (49/69, 71%). The strength of this study was the remarkable geographic distribution of responses; all parts of the world were included and participated. We believe that this globally conducted online survey has polled for the properties of the “ideal” donor site dressing and possibly will lead to an improved clinically-driven direction of future wound dressing development.
Keywords: donor site, dressing, survey, internet, online
Abstract
Les greffes de peau mince sont largement utilisées pour reconstruire les défauts de la peau. Même si un grand nombre de différentes options de couverture des sites donneurs sont devenus disponibles dans la pratique clinique quotidienne, à ce jour, aucun matériel de pansement optimum n’a été trouvé. Pour cette raison, nous avons mené un sondage en ligne mondialement distribué à scrutin pour les propriétés d’un tel pansement de site donneur «idéal», qui peut conduire à une meilleure direction en ce qui concerne des futurs développements de pansement. Un total de 69 répondants de 34 pays ont été inclus dans le questionnaire, soit un taux de réponse de 13,8% (69/500) sur une période de 1 mois. La majorité des répondants ont évalué les caractéristiques d’un pansement «idéal» pour les sites donneurs d’être «essentiel» ou «souhaitable» comme suit: le manque d’adhérence au lit de la plaie («essentiel»: 31/69, 44,9%; «souhaitable» : 30/69, 43,5%), le changement de pansement sans douleur («essentiel»: 38/69, 55,1%; «souhaitable»: 30/69, 43,5%); l’absorption («essentiel»: 27/69, 39,1% ; «souhaitable»: 33/69, 47,8%), la facilité de retrait («essentiel»: 37/69, 53,6%; «souhaitable»: 27/69, 39.13%), par rapport à la fréquence souhaitée des changements de pansements, les répondants préféraient «aucun changement de pansement jusqu’à ce que le site donneur est guéri» (51/69, 73,9%) dans la majorité des cas, suivi par «deux fois par semaine» (10/69, 14,5%), «deux jours» (5/69 , 7,2%) et «quotidienne» (3/69, 4,3%). En ce qui concerne la conception du matériel de pansement, la majorité des participants ont préféré une seule pièce (composite) (44/69, 63,8%). La majorité des répondants a également nié l’existence actuelle d’un pansement au site donneur «idéal» (49/69, 71%). La force de cette étude est la répartition géographique remarquable de réponses ; toutes les parties du monde ont été inclus et ont participé. Nous croyons que cette enquête en ligne, menée au niveau mondial, concernant les propriétés du pansement «idéal» pour les sites donneurs se traduira, éventuellement, par une amélioration future dans le développement des pansements.
Introduction
Split skin grafting (SSG) has been a widely used technique for reconstructing skin defects (e.g. in burns and chronic or traumatic wounds).1,2 The wound area created during harvest of SSG is called the donor site wound (DSW). Depending on the thickness of the SSG, the DSW should completely re-epithelialize within 7 to 21 days.3 Optimum local care and cover for these DSWs should promote wound healing and be cost-effective, while preventing adverse events or even complications, such as pain, discomfort, infection, and scarring. Pain and discomfort, in particular, have been reported to occur more often in DSWs than in the actual recipient site.3,5 Although a vast number of different coverage options for DSW, including dressings and topical agents, have become available in daily clinical practice, so far no optimum coverage has been found for local wound care.1,2,6,7 Consequently, large variations exist among health care professionals on which kind of wound dressing materials or topical agents to use on DSWs.8,9 The only available evidence-based reports comprise four systematic reviews (SRs), which in turn demonstrate a lack of powerful evidence for the effectiveness of any of the dressing materials used to date for DSWs.1,2,6,7 These SRs tentatively concluded that, as regards wound healing, moist dressing materials were preferable to nonmoist dressings. In the cited SRs, hydrocolloid and films were reported to perform better in comparison to other materials (e.g. alginates, paraffin gauzes, hydrofibers, and foams), as assessed by the parameters of healing and pain.7 Among these other materials, hydrofibers seemed to outperform tulle dressings with regard to wound healing and pain.10,11 Although tulle dressings seemed to be the least suitable for DSWs, recent evidence showed that gauzebased dressings still have a place in wound care.12 Some centers still adhere, or have returned to, these gauze-based dressings.13 Silicone-based dressings have the advantage of being non-adhesive, although they tend to dislocate easily and do not seem to outperform alginates.14 However, scant information exists on characteristics and properties of a wound dressing which would be required in daily clinical practice by wound care specialists worldwide. Therefore, we conducted a globally-distributed online survey to poll for the properties of such an “ideal” donor site dressing, possibly leading to an improved clinically-driven direction of future wound dressing developments.
Materials and methods
In total, 500 specialists in burn care worldwide were invited by email to participate in an open, voluntary internet-based cross-sectional survey. The email invitation was sent with a direct link to the online survey (http://www.abusg.com/index.php/surveys/study-on-donorsites). The survey was generated by the Austria Burn Treatment, Research and Prevention study group (scientific nonprofit medical organization) together with experts among the burn care specialist community. The list of email contacts was compiled from the corresponding addresses found in all publications of the journal of “Burns” (Elsevier Science Ltd. for ISBI) in 2012.
The system used, “JQuarks 4 Surveys” (http://www.jquarks.org), guaranteed unique sessions by checking the IP address of the client computer, which filtered and sorted out duplicate entries. Respondents were able to to review a displayed summary of their responses and make changes if they wished. The anonymized responses were automatically logged in a MySQL-Database (http://www.mysql.com). Check-ups for technical difficulties of the website were performed daily. No personal data was collected from respondents and no incentives for survey participation were offered. This procedure was according to our previous paper, which dealt with the ideal burn wound dressing.15
The questionnaire was structured to focus on the characteristics of a preferred/ideal donor site dressing. These characteristics were obtained by using 16 non-compulsory questions featuring answers which could be single choice (as per no.11) or open text (as per no.5). All questions were numbered consecutively and included a clear request for either single or multiple responses. Single choice questions contained either of the two rating scales: (1) “essential”, “desirable”, “neutral”, “seldom required”, and “never required” or (2) “daily”, “alternate days”, “twice weekly”, and “no dressing change until the donor site has healed”. In addition, 4 questions were included to collect general information related to profession (multiple answers), staff grade (multiple answers), and country (open text) and city (open text). The questionnaire was distributed on a single scrolling web-page. The time required for completing the questionnaire was not assessed. In our survey, we followed the CHERRIES (Checklist for Reporting Results of Internet E-Surveys) checklist16,17 and adhered to the SURGE (Survey Reporting Guideline) guidelines18 for assuring reporting quality.
For descriptive data analysis the collected data was exported by “JQuarks 4 surveys” into a comma separated values (CSV) format, which stored tabular data in plaintext form. Fractions for nominal and ordinal data were calculated, with the data represented as percentages of completed answers per question.
Results
A total of 69 respondents from 34 countries submitted completed questionnaires, resulting in a response rate (completion rate) of 13.8% over a 1-month period. Respondents declared their profession as follows: surgeons (68.1%, 47/69); anaesthetists/intensivists (10.2%, 7/69); and others (21.7%, 15/69) - including nursing staff, emergency physicians and physical therapists. The single participating countries are listed in Table I and Fig. 1.
Table I. List of participating countries in alphabetic order.
Fig. 1. Map of participating countries in black (34 countries worldwide).

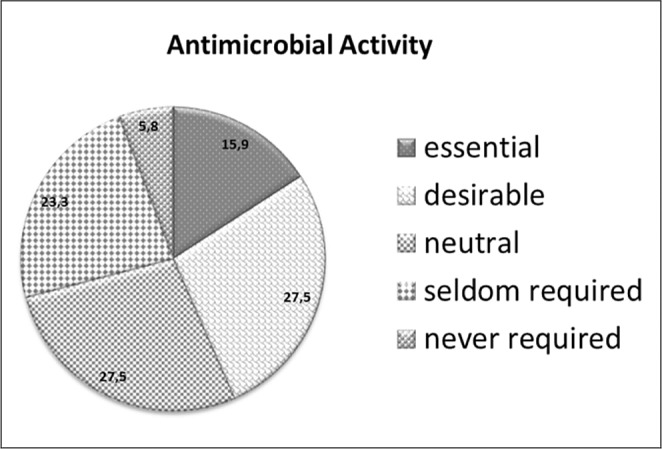
Detailed questionnaire results are provided in Figs. 2-7. The majority of respondents rated the characteristics of an “ideal” donor site dressing to be either “essential” or “desirable” as follows: lack of adhesion to the wound bed (“essential”: 31/69, 44.9%; “desirable”: 30/69, 43.5%); pain-free dressings (“essential”: 38/69, 55.1%; “desirable”: 30/69, 43.5%) (Fig. 2); absorbency (“essential”: 27/69, 39.1%; “desirable”: 33/69, 47.8%); ease of removal (“essential”: 37/69, 53.6%; “desirable”: 27/69, 39.13%) (Fig. 3); different sizes (“essential”: 23/69, 33.3%, “desirable”: 31/69, 44.9%) (Fig. 4); reduction of blood loss („essential“: 20/69, 28.9%, „desirable“: 27/69, 39.1%) (Fig. 5). Antimicrobial activity was rated as either “essential”: 11/69, 15.9%, “desirable”: 19/69, 27.5% or “neutral“: 19/69, 27.5% (Fig. 6).
Fig. 2. Responses to the question: How important are pain-free dressing changes?
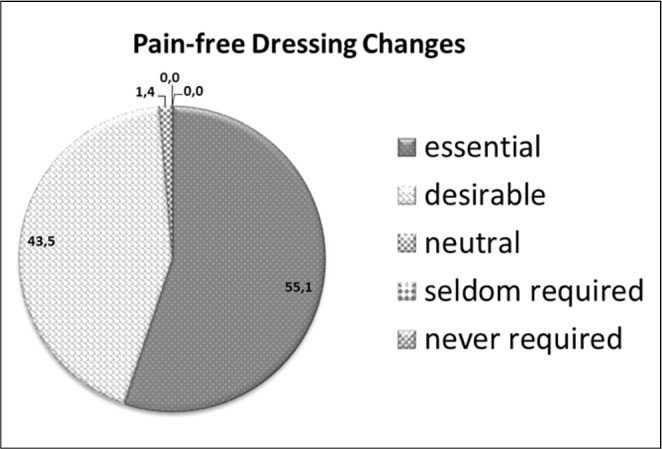
Fig. 3. Responses to the question: How important is ease of removal?
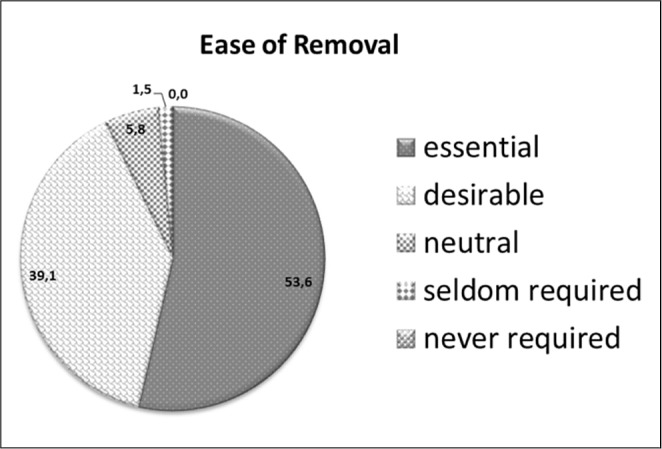
Fig. 4. Responses to the question: How important are different dressing sizes?
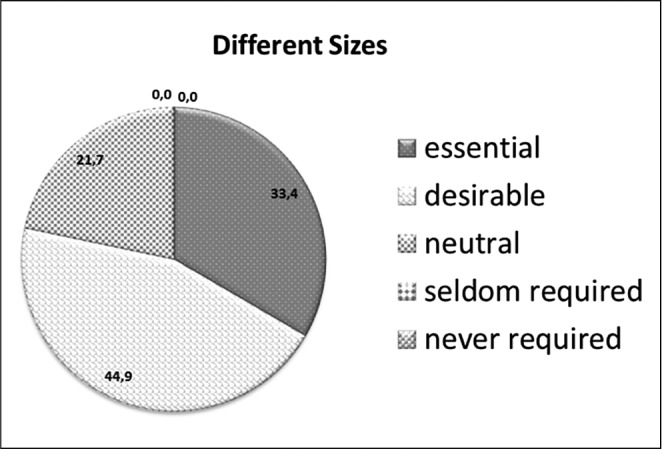
Fig. 5. Responses to the question: How important is reduction of blood loss?
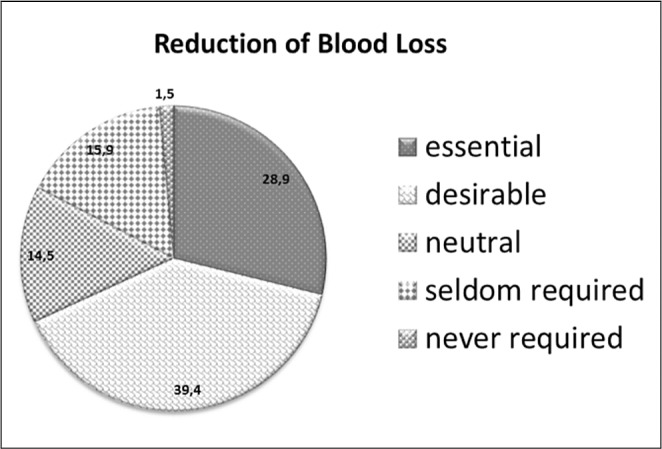
Fig. 6. Responses to the question: How important is antimicrobial activity?
Self-adhesive properties were found to be “essential“ in 11.6% (8/69) of responses, “desirable” in 42.0% (29/69) and “neutral” in 24.6% (17/69) of responses. With regard to the desired frequency of dressing changes, the majority of respondents preferred “no dressing change until the donor site has healed” (51/69, 73.9%), followed by “twice weekly” (10/69, 14.5%), “alternate days” (5/69, 7.2%) and “daily” (3/69, 4.3%) (Fig. 7). With regard to design of the dressing material, the majority of the participants preferred to have a one-piece (composite) dressing product (44/69, 63.8%). The majority of respondents denied the current availability of an “ideal” donor site dressing (49/69, 71%).
Fig. 7. Responses to the question: Ideally, how often should the dressing be changed?
Discussion
In current clinical practice, a relatively standardized wound area like a DSW did not appear to be associated with a uniform dressing choice. Also the systematic reviews of available literature reported a large clinical heterogeneity among the available trials.1,2,6,7 To date, available evidence allowed only for a tentative conclusion in favour of dressing promoting a moist environment over that of gauze-based dressings. The summary was classified as tentative because of poor quality and small sample sizes of available trials. Therefore, most systematic reviews recommended the initiation of new large randomized clinical trials.2,6,7
This globally-distributed online poll among burn care specialists differs from previously published data elaborating on preferences for partial vs. full thickness injuries2,3 in terms of seeking to identify an “ideal” donor site dressing. The main result of our poll is that the “ideal” donor site includes features like non-adhesiveness, absorbency and antimicrobial properties; it should be easily removable, guarantee pain-free dressing changes and, moreover, no dressing change until completed healing of the donor site.
Overall, our findings are partly in agreement with suggestions in the literature defining the key characteristics for donor site dressings.12 However, instead of enumerating all characteristics of an ideal donor site dressing, we aimed to assess the relevant characteristics in the context of its practical relevance as suggested by clinicians. Most of our findings were comparable to the characteristics of the “ideal” burn dressing, but antimicrobial activity, for instance, was identified as less important. This result is not surprising considering that the pathophysiological circumstances in burn wounds incur a high risk of infection, 15,19 as opposed to relatively clean DSWs. As regards absorbency, which was rated as an essential property by most participants, absorbent dressings can manage wound fluids or exudates but there is no evidence to date that they improve wound healing.
Additionally, dressings that are easily removable without causing pain were found to be an essential asset, well noting that intervention-related pain was often undertreated20 and caused patient anxiety.21 This highlights the importance of close to pain-free dressing changes, most certainly supported by easily removable dressings. Given that clinical trials often contain a meagre measurement and reporting of levels of pain, this issue has to be addressed in future to allow adequate evidence-based comparisons.
The majority of respondents preferred a wound dressing that required no dressing change until the donor site has healed in order to improve healing by minimizing wound surface irritation. Avoiding frequent trauma of the regenerating epithelium during dressing change seemed to be pivotal. In addition, the potential to minimize patient discomfort with fewer dressing changes can improve patients ´ compliance, and consequently permit earlier patient discharge, resulting in a reduced length-of-stay with possible financial implications for inpatient care.22 Outpatient care treatment concepts that minimize clinical visits for dressing changes may also lead to reduced costs and improved patient flexibility whilst providing a similar quality of care.
Conclusion
Despite our intention to conduct a representative high quality survey, this study was subject to the inherent limitations of online survey-based data, and thus the relatively low response rate of our survey may implicate a considerable non-response bias. Although some investigators consider a response rate between 60-70% as acceptable,23 our results were in line with the literature, which reveals a wide range of response rates (9-94%),24 and comparable to the response rate of our previous survey. The strength of this study was in the remarkable geographic distribution of the responses, as all parts of the world were included and have participated. Going forward, this should not only lead to optimized clinical trial design for clinicians, but also to clinically-driven product development for the industry, which will play a major role in helping to standardize optimal wound care of DSWs. This study aimed to provide a guide for future developments and to encourage much needed, improved evidence of clinical trials and their respective design in the future.
References
- 1.Rakel BA, Bermel MA, Abbott LI, Baumler SK, Burger MR, Dawson CJ, Heinle JA, Ocheltree IM. Split-thickness skin graft donor site care: A quantitative synthesis of the research. Appl Nurs Res. 1998;11:174–82. doi: 10.1016/s0897-1897(98)80296-6. [DOI] [PubMed] [Google Scholar]
- 2.Wiechula R. The use of moist wound-healing dressings in the management of split-thickness skin graft donor sites: A systematic review. Int J Nurs Pract. 2003;9:9–17. doi: 10.1046/j.1322-7114.2003.00417.x. [DOI] [PubMed] [Google Scholar]
- 3.Ratner D. Skin grafting. Semin Cutan Med Surg. 2003;22:295–305. doi: 10.1016/S1085-5629(03)00079-8. [DOI] [PubMed] [Google Scholar]
- 4.Persson K, Salemark L. How to dress donor sites of split thickness skin grafts: A prospective, randomised study of four dressings. Scand J Plast Reconstr Surg Hand Surg. 2000;34:55–9. doi: 10.1080/02844310050160178. [DOI] [PubMed] [Google Scholar]
- 5.Feldman DL. Which dressing for split-thickness skin graft donor sites? Ann Plast Surg. 1991;27:288–91. doi: 10.1097/00000637-199109000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Voineskos SH, Ayeni OA, McKnight L, Thoma A. Systematic review of skin graft donor-site dressings. Plast Reconstr Surg. 2009;124:298–306. doi: 10.1097/PRS.0b013e3181a8072f. [DOI] [PubMed] [Google Scholar]
- 7.Schreuder SM, Qureshi MA, Vermeulen H, Ubbink DT. Dressings and topical agents for treating donor sites of split-skin grafts: A systematic review [abstract]. EWMA Journal. 2009;9:22. [Google Scholar]
- 8.Geary PM, Tiernan E. Management of split skin graft donor sitesresults of a national survey. J Plast Reconstr Aesthet Surg. 2009;62:1677–83. doi: 10.1016/j.bjps.2008.07.036. [DOI] [PubMed] [Google Scholar]
- 9.Lyall PW, Sinclair SW. Australasian survey of split skin graft donor site dressings. Aust N Z J Surg. 2000;70:114–16. doi: 10.1046/j.1440-1622.2000.01767.x. [DOI] [PubMed] [Google Scholar]
- 10.Barnea Y, Amir A, Leshem D, Zaretski A, Weiss J, Shafir R, Gur E. Clinical comparative study of aquacel and paraffin gauze dressing for split-skin donor site treatment. Ann Plast Surg. 2004;53:132–6. doi: 10.1097/01.sap.0000112349.42549.b3. [DOI] [PubMed] [Google Scholar]
- 11.Lohsiriwat V, Chuangsuwanich A. Comparison of the ionic silver-containing hydrofiber and paraffin gauze dressing on splitthickness skin graft donor sites. Ann Plast Surg. 2009;62:421–2. doi: 10.1097/SAP.0b013e31818a65e9. [DOI] [PubMed] [Google Scholar]
- 12.Ubbink DT, Vermeulen H, Goossens A, Kelner RB, Schreuder SM, Lubbers MJ. Occlusive vs gauze dressings for local wound care in surgical patients: A randomized clinical trial. Arch Surg. 2008;143:950–5. doi: 10.1001/archsurg.143.10.950. [DOI] [PubMed] [Google Scholar]
- 13.Malpass KG, Snelling CF, Tron V. Comparison of donor-site healing under Xeroform and Jelonet dressings: Unexpected findings. Plast Reconstr Surg. 2003;112:430–9. doi: 10.1097/01.PRS.0000070408.33700.C7. [DOI] [PubMed] [Google Scholar]
- 14.O’Donoghue JM, O’Sullivan ST, O’Shaughnessy M, O’Connor TP. Effects of a silicone-coated polyamide net dressing and calcium alginate on the healing of split skin graft donor sites: A prospective randomised trial. Acta Chir Plast. 2000;42:3–6. [PubMed] [Google Scholar]
- 15.Selig HF, Lumenta DB, Giretzlehner M, Jeschke MG, Upton D, Kamolz LP. The properties of an “ideal“ burn wound dressing: What do we need in daily clinical practice? Results of a worldwide online survey among burn care specialists. Burns. 2012;38:960–6. doi: 10.1016/j.burns.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 16.Eysenbach G. Correction: Improving the quality of web surveys: The checklist for reporting results of Internet E-surveys (CHERRIES). Journal of Medical Internet Research. 2012;14:8. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of Internet E-surveys (CHERRIES). Journal of Medical Internet Research. 2004;6:34. doi: 10.2196/jmir.6.3.e34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bennet C, Khangura S, Brehaut JC, Graham ID, Moher D, Potter BK, et al. Reporting guidelines for survey research: An analysis of published guidance and reporting practices. PLoS MEdicine. 2010;8:1000–1069. doi: 10.1371/journal.pmed.1001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keck M, Herndon DN, Kamolz LP, Frey M, Jschke MG. Pathophysiology of burns. Wiener Medizinische Wochenschrift. 2009;159:327–36. doi: 10.1007/s10354-009-0651-2. [DOI] [PubMed] [Google Scholar]
- 20.Ashburn MA. Burn pain: The management of procedure-related pain. The Journal of Burn care and Rehabilitation. 1995;16:365–71. doi: 10.1097/00004630-199505001-00006. [DOI] [PubMed] [Google Scholar]
- 21.Weinberg K, Birdsall C, Vail D, Marano MA, Petrone SJ, Mansour EH. Pain and anxiety with burn dressing changes: Patient self-report. The Journal of Burn Care and Rehabilitation. 2000;21:155–6. doi: 10.1097/00004630-200021020-00013. [DOI] [PubMed] [Google Scholar]
- 22.Jansen LA, Hynes SL, Macadam SA, Papp A. Reduced length of stay in hospital for burn patients following a change in practice guidelines: Financial implications. Journal of Burn Care and Rehabilitation. 2012;33:275–9. doi: 10.1097/BCR.0b013e31824d1acb. [DOI] [PubMed] [Google Scholar]
- 23.Burns KE, Duffett M, Kho ME, Meade MO, Adhikari NK, Sinuff, et al. A guide for the design and conduct of self-administered surveys of clinicians. Canadian Medical Association Journal. 2008;179:245–52. doi: 10.1503/cmaj.080372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Braithwaite D, Emery J, De Lusignan S, Sutton S. Using the internet to conduct surveys of health professionals: A valid alternative? Family Practice. 2003;20:545–51. doi: 10.1093/fampra/cmg509. [DOI] [PubMed] [Google Scholar]


